ABSTRACT
Purpose: We sought evidence to justify undertaking population-based trachoma surveys in Timor-Leste, believing that in the absence of such evidence, the country could be categorized as not needing interventions to eliminate trachoma.
Methods: We undertook a systematic review of published literature on trachoma in Timor-Leste, with results updated to 28 April 2018. We also undertook a series of clinic- and field-based screening exercises, consisting of: (1) in October 2015, conjunctival examination of all children attending a school in Vila, Atauro Island; (2) from 1 November 2016 to 30 April 2017, examination for trichiasis, by specifically-trained frontline eye workers, of all individuals presenting to the ophthalmic clinics of six referral hospitals and five district eye clinics; and (3) house-to-house case searches in a total of 110 households, drawn from three communities that were reported by investigators from the 2016 Rapid Assessment of Avoidable Blindness (RAAB) to include residents with trachoma.
Results: Three RAABs (2005, 2009–2010, 2016) and two relevant published papers were identified. The 2016 RAAB reported one female subject to have been diagnosed with trachomatous corneal opacity. Re-examination of that individual revealed that she had ankyloblepharon, without evidence of trichiasis or entropion. No children on Atauro Island, no clinic attendees, and no individuals examined in the targeted house-to-house searches had any sign of trachoma.
Conclusion: Trachoma is very unlikely to be a public health problem in Timor-Leste. It would not be appropriate to incur the costs of conducting formal population-based trachoma prevalence surveys here.
KEYWORDS:
Introduction
There is currently no commercially-available vaccine to prevent ocular Chlamydia trachomatis infection.Citation1,Citation2 Prevention of blindness from trachomaCitation3 therefore relies on implementation of the SAFE strategy,Citation4 which involves surgery for trachomatous trichiasis,Citation5 antibiotics to clear C. trachomatis infection,Citation6 and facial cleanlinessCitation7 and environmental improvementCitation8 to reduce its transmission. Whether or not these things should be implemented as public health-level interventions for trachoma is determined by estimating the prevalence of key signs of disease:Citation9,Citation10 trachomatous inflammation—follicular (TF)Citation11 in 1–9-year-olds, and trachomatous trichiasis (TT)Citation11 in ≥ 15-year-olds. Undertaking population-based prevalence surveys to generate such estimates requires resources,Citation12,Citation13 so deciding where to do soCitation14 is an important programmatic step.
Trachoma is prevalent in a number of countries of Southern and South-East Asia, Australia and the Pacific IslandsCitation15–Citation24 (though some aspects of the disease in the Pacific appear to be unusual.Citation25–Citation29) Beyond the Western boundary of the Pacific Ocean, between Indonesia and Australia, lies Timor-Leste, which became a United Nations-recognized sovereign state in 2002. Its estimated 2015 population was 1.2 million people, distributed across the eastern half of the island of Timor, Oecusse (an exclave on Timor Island’s northwestern side), and the island of Atauro. Dili, the national capital, is the largest city, with a 2015 population of 222,000. Atauro had a 2015 population of 9274 people, who are considered to have the lowest socioeconomic status in the country. Jaco, the other island included within Timor-Leste’s territories (and the country’s easternmost land mass) is uninhabited. The national human development index in 2017 was 0.625, which falls in the “medium” range.
Three factors prompted us to review the situation with respect to trachoma in Timor-Leste. First, the country is located close to other trachoma-endemic countries; trachoma clusters at various scales.Citation30–Citation33 Second, its population has relatively poor access to sanitation,Citation34 and poor access to sanitation is associated with increased risk of TF.Citation35 Third, there is a current drive to complete baseline trachoma mapping everywhere that it is justified,Citation36 as efforts ramp up to reach the target of global trachoma elimination.Citation37 We therefore looked for evidence to justify undertaking one or more population-based trachoma prevalence surveys here. We believed that failure to find such evidence after diligent search would mean that Timor-Leste could be categorized as “thought to not require interventions (to eliminate trachoma as a public health problem)” in the World Health Organization’s Global Health Observatory (http://apps.who.int/gho/data/node.main.A1645T).
Methods
Investigations were undertaken from 2015 to 2017. We performed a systematic review plus various activities to screen individuals for trachoma.
For the systematic review, we searched the literature, employing three sources: (1) PubMed (https://www.ncbi.nlm.nih.gov/pubmed/), using the search terms ((“trachoma*” OR “trichiasis”) AND (“Timor” OR “Atauro” OR “Oecusse”)); (2) the authors’ own collections of published papers and grey literature, which are electronically indexed, using the same search terms; and (3) the online repository of rapid assessments of avoidable blindness (RAABs; http://raabdata.info/repository/), using the single search term “Timor”. The literature search was done on 9 October 2016, and updated on 28 April 2018. Results were screened for relevance using articles’ titles and abstracts; where we judged that a paper or report might contain trachoma prevalence data or case reports, we scrutinized the full document and extracted pertinent data. For the most recent RAAB, we were able to draw on the original dataset, which was accessible to our lead author (MC).
De novo trachoma screening consisted of three separate activities. For each of these, the World Health Organization simplified trachoma grading systemCitation11 was generally used as the basis for diagnosis. Where an ophthalmologist was involved, a more comprehensive clinical evaluation of the eyelid and cornea was also undertaken.
First, in October 2015, a visiting ophthalmologist (AJK) systematically examined all available children at a single school in Vila on Atauro Island (), inspecting the everted upper eyelid of both eyes of each child, using a head-mounted 2.5 × magnifying loupe and bright illumination.
Figure 1. Spatial coverage of fieldwork conducted as part of this investigation: school screening by a visiting ophthalmologist; examination by trained eyecare workers of all patients seen for routine clinical care in referral hospital or eye clinic; and house-to-house case searches by ophthalmology registrars, following up results from the 2016 rapid assessment of avoidable blindness (RAAB). The black square shows the capital, Dili. District numbering: 2 = Ainaro (sub-district Maubisse); 3 = Baucau; 4 = Bobonaro (sub-district Maliana); 5 = Covalima; 6 = Dili; 7 = Ermera (sub-district Ermera); 8 = Lautém (sub-district Lospalos); 9 = Liquiça; 11 = Manufahi (sub-district Same); 12 = Oecussi (sub-district Pante Macassar).
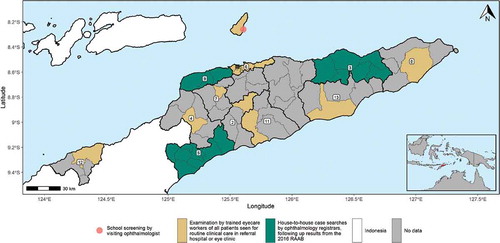
Second, all eyecare workers engaged by the East Timor Eye Program participated in a 1-day training program covering examination for and recognition of trichiasis, delivered by a senior registrar in ophthalmology (VA) in October 2016. Subsequently, from 1 November 2016 to 30 April 2017, those front-line personnel examined for trichiasis all patients seen as part of routine clinical care in the referral hospitals of Baucau, Maliana, Suai, Maubisse, Oecusse and Dili; and the eye clinics of Lospalos (Lautém District); Viqueque (Viqueque District), Same (Manufahi District), Ermera (Ermera District) and Atauro Island (Dili Muncipality) ().
Third, to follow up results from the 2016 RAAB, while undertaking outreach activities to screen for adult cataract, three specific communities in Baucau, Cova Lima and Liquiçá districts () were targeted for focused house-to-house searches for trachoma. Examinations were undertaken by ophthalmology registrars (VA, BMP) from the National Eye Centre. In the three villages, 50, 40 and 20 households, respectively, were visited. The eyelids of all consenting residents of selected households were examined.
Ethical considerations
Screening protocols were approved by the Human Research Ethics Committee, Ministry of Health, Timor-Leste (GEPS/EP/2014/021). Fieldwork was performed only after discussion with and verbal approval by relevant village chiefs, heads of local health clinics and the headmaster of the Atauro Island school. Verbal consent for examination was provided by each subject or, in the case of children, by a parent or guardian. Individuals diagnosed with any eye condition were offered full diagnostic workup and management, in accordance with the standard operating procedures of the East Timor Eye Program.
Results
Systematic review
The PubMed search returned 108 papers. Only one of these contained data on the prevalence of trachoma in Timor-Leste: a peer-reviewed publicationCitation38 describing the methods and results of the 2016 RAAB. Most of this information was also included in the RAAB reportCitation39 itself, and is therefore presented below.
In the authors’ reference collections, one additional study of relevance was located, describing a 2012 study of 293 patients aged 17 years or older presenting to the National Eye Centre, 80% of whom were residents of Dili. No cases of TT or active (inflammatory) trachoma were diagnosed in that series.Citation40
In the RAAB online repository, three RAABs were listed for Timor-Leste, conducted in 2005,Citation41 2009–2010Citation42 and 2016 ().Citation39
Figure 2. Spatial coverage of the three Timor-Leste rapid assessments of avoidable blindness (RAABs) identified, which were conducted in 2005, 2009–2010 and 2016. The black square shows the capital, Dili. District numbering: 1 = Aileu; 2 = Ainaro; 3 = Baucau; 4 = Bobonaro; 5 = Covalima; 6 = Dili; 7 = Ermera; 8 = Lautém; 9 = Liquiça; 10 = Manatuto; 11 = Manufahi; 12 = Oecussi; 13 = Viqueque.
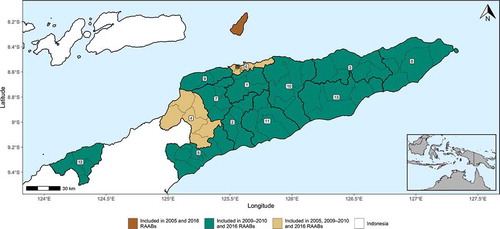
In the 2005 RAAB, 50 villages were selected using a probability-proportional-to-village-population-size methodology, drawn equally from Dili and a single rural district, Bobonaro, 4.5 h by road from Dili. In each village, consecutive households were visited until 30 participants aged ≥ 40 years were enrolled. Presenting visual acuity was measured for each eye of each participant; any eye with visual acuity worse than 6/18 was further examined to ascertain the cause of reduced vision. Amongst 1414 people examined, no cases of trachomatous blindness or low vision were identified.Citation41
In the 2009–2010 RAAB, from a list of all villages in the country’s 12 mainland districts, 50 villages were selected with probability proportional to village population size. Some 87% of the population eligible for selection was rural. In each selected village, consecutive households were enrolled until 45 participants aged ≥ 40 years were enrolled; in all, 2014 people were examined. The examination protocol was the same as that used in 2005. No eyes with trachomatous blindness or low vision were found.Citation42
In the 2016 RAAB, all 13 districts of Timor-Leste were included, and 67 villages were selected with probability proportional to population size.Citation39 Trained teams examined a total of 3253 participants aged ≥ 50 years.Citation38 Four individuals, in Baucau, Cova Lima, and Liquiçá districts, were reported to have trachoma, including one female subject reported to have bilateral trachomatous corneal opacity.Citation38 (During subsequent outreach work, this individual was identified, re-examined and found to have ankyloblepharon, without evidence of trichiasis or entropion.)
De novo trachoma screening
In October 2015, on Atauro, 58 children aged 9–17 years (mean 11 years) were examined. One 13-year-old male had unilateral conjunctival scarring of the right upper lid that had an appearance that would be atypical of trachomatous scarring. There were no corneal changes, and no eyelashes touched the eye. The eyelids of the other 57 children had no signs consistent with trachoma.
Fourteen eyecare workers were trained to recognize trichiasis and asked to do so as part of their day-to-day clinical work. The screening protocol required staff to call the National Eye Centre in Dili if any suspected cases were identified, whereupon one of the visiting Ophthalmology Fellows would be tasked with driving out to visit patients in their homes, in order to verify the diagnosis. No calls were received in the designated 6-month screening period. To ensure that this was not due to front-line eyecare personnel forgetting the screening exercise or being unable to report cases because of pressure of other work, Fellows and the Head of Department of the National Eye Centre periodically called eyecare workers to remind them; on each occasion, assurance was received that trachoma was being searched for, and that no suspected cases had been identified.
In three villages of Baucau, Cova Lima and Liquiçá in which trachoma was reported to have been identified in the 2016 RAAB, no cases of trichiasis, trachomatous conjunctival scarring or active trachoma were found.
Discussion
Though much work remains, tremendous progress is currently being made against trachoma globally.Citation43,Citation44 We undertook the studies described in this manuscript because it was not clear whether trachoma was likely to be a public health problem in Timor-Leste, and we did not want its people to be left behind. We used an approach consistent with the logic used for justifying mapping or not mapping within the Global Trachoma Mapping Project.Citation14 Documenting the methodology and outcome of our work is, we think, important, to avoid duplication of effort and, assuming that others agree with our conclusion, to prevent continuing uncertainty over the possibility of a trachoma elimination program being required here.
With a predominantly rural population—almost two thirds of residents live in areas considered to be remote—and an under-resourced health service, there are multiple barriers to accessing eye care in Timor-Leste.Citation45,Citation46 We could not necessarily assume that individuals suffering from trichiasis would present to clinics requesting assistance for that problem. We therefore systematically searched for evidence of trichiasis in the published literature on Timor-Leste, in individuals attending eye care facilities with any presenting complaint, and in samples drawn from communities believed (on the basis of previous reports) to be at high risk.
In the three RAABs that we identifiedCitation38,Citation41,Citation42 investigators assessed the anterior segment of an examinee’s eye, including for corneal opacity, only if the eye had low vision: the presence of trichiasis in an eye with normal presenting vision would not have been recorded. The previously-published study conducted at the National Eye CentreCitation40 entailed a comprehensive ophthalmic examination of each patient by an eye specialist, but only 57 of 293 subjects included were residents of rural areas, where trachoma is more likely to be found.Citation33,Citation47,Citation48 Our systematic clinic-based screening exercise provided far greater geographical coverage. We visited the culturally-distinct, former prison island of Atauro, where water, sanitation, and other infrastructure are below average national standards, to look for trachoma in the conjunctivae of local schoolchildren. Prompted by reports of trichiasis being found in individuals sampled within the 2016 RAAB, we also undertook active screening of residents of all ages in three purposively-selected rural communities. We found no evidence of trachoma in any individual examined.
These investigations had some weaknesses. First, RAABs do not involve the examination of children and do not include eyelid eversion, even if vision is < 6/18 in the better eye. They therefore have poor sensitivity for determining whether trachoma is present as a public health problem. Second, the de novo screening that we undertook was somewhat limited in scope, concentrating particularly on individuals self-presenting to eye care services, with the only fieldwork undertaken being the visit to Atauro and a follow-up of three communities identified by the 2016 RAAB as possibly having residents with trichiasis. All children examined on Atauro in October 2015 were aged 9 years or above; active trachoma is much more usually found in pre-school-age than older children,Citation49–Citation51 but in areas of intense transmission, conjunctival scarring can be seen in 9–17-year-olds, as examined here.Citation52 Unfortunately, we did not have the human resource capacity to also undertake community-based screening of younger children during the visit to Atauro. Third, no formal standardization (through inter-grader agreement exercises or objective structured clinical examinationCitation53–Citation55) of the graders who participated in our trachoma screening exercises was undertaken. Fourth, house-to-house surveys, as used in three communities in this series of investigations, will result in under-representation of working adults and school-going children. The latter are, however, less likely to have trachoma than 1–9-year-olds examined as part of community-based surveys.Citation56 Finally, some authorities advocate the use of the key informant methodCitation57 as the best method for identifying blinding eye conditions; we did not use this technique.
Despite these limitations, having failed to find a single case of trichiasis amongst all-comers to eye care services nation-wide over a continuous period of observation of 6 months, and having been unable to substantiate previous case reports of trachoma or find others with evidence of disease in the same communities, we suggest that trachoma is very unlikely to represent a current public health problem in Timor-Leste. Given that only 41% of the population accesses improved sanitation facilities,Citation34 continued vigilance for the emergence of trachoma will be necessary until such time as living standards improve.
Disclosure Statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Solomon AW, Mabey DC. Modeling the economic net benefit of a potential vaccination program against ocular infection with Chlamydia trachomatis. Vaccine. 2005;23(46–47):5281–5282. doi:10.1016/j.vaccine.2005.05.042.
- Poston TB, Gottlieb SL, Darville T. Status of vaccine research and development of vaccines for Chlamydia trachomatis infection. Vaccine. 2017. [Epub ahead of print]. doi:10.1016/j.vaccine.2017.01.023.
- Mabey DC, Solomon AW, Foster A. Trachoma. Lancet. 2003;362(9379):223–229. doi:10.1016/S0140-6736(03)13914-1.
- Francis V, Turner V. Achieving Community Support for Trachoma Control (WHO/PBL/93.36). Geneva: World Health Organization; 1993.
- Burton M, Habtamu E, Ho D, Gower EW. Interventions for trachoma trichiasis. Cochrane Database Syst Rev. 2015;11:CD004008.
- Evans JR, Solomon AW. Antibiotics for trachoma. Cochrane Database Syst Rev. 2011;3:CD001860.
- Ejere HO, Alhassan MB, Rabiu M. Face washing promotion for preventing active trachoma. Cochrane Database Syst Rev. 2015;2:CD003659.
- Rabiu M, Alhassan MB, Ejere HO, Evans JR. Environmental sanitary interventions for preventing active trachoma. Cochrane Database Syst Rev. 2012;(2):CD004003. DOI: 10.1002/14651858.CD004003.pub4. Available from: http://tropicaldata.knowledgeowl.com/help/training-system-for-trachoma-prevalence-surveys
- Solomon AW, Zondervan M, Kuper H, Buchan JC, Mabey DCW, Foster A. Trachoma Control: A Guide for Programme Managers. Geneva: World Health Organization; 2006.
- Ngondi J, Reacher M, Matthews F, Brayne C, Emerson P. Trachoma survey methods: a literature review. Bull World Health Organ. 2009;87:143–151.
- Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bull World Health Organ. 1987;65:477–483.
- Trotignon G, Jones E, Engels T, et al. The cost of mapping trachoma: data from the Global Trachoma Mapping Project. PLoS Negl Trop Dis. 2017;11(10):e0006023. doi:10.1371/journal.pntd.0006023.
- Chen C, Cromwell EA, King JD, et al. Incremental cost of conducting population-based prevalence surveys for a neglected tropical disease: the example of trachoma in 8 national programs. PLoS Negl Trop Dis. 2011;5(3):e979. doi:10.1371/journal.pntd.0001370.
- Solomon AW, Willis R, Pavluck AL, et al. Quality assurance and quality control in the Global Trachoma Mapping Project. Am J Trop Med Hyg. 2018; 99(4):858–863. doi:10.4269/ajtmh.18-0082.
- Malhotra S, Vashist P, Gupta N, et al. Prevalence of trachoma in Car-Nicobar Island, India after Three annual rounds of mass drug administration with Azithromycin. PLoS One. 2016;11(7):e0158625. doi:10.1371/journal.pone.0158625.
- Ko R, Macleod C, Pahau D, et al. Population-based trachoma mapping in six evaluation units of Papua New Guinea. Ophthalmic Epidemiol. 2016;23(Sup1):22–31. doi:10.1080/09286586.2016.1235715.
- Meng N, Seiha D, Thorn P, et al. Assessment of trachoma in Cambodia: trachoma is not a public health problem. Ophthalmic Epidemiol. 2016;23(Sup1):3–7. doi:10.1080/09286586.2016.1230223.
- Sokana O, Macleod C, Jack K, et al. Mapping trachoma in the Solomon Islands: results of three baseline population-based prevalence surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(Sup1):15–21. doi:10.1080/09286586.2016.1238946.
- Southisombath K, Sisalermsak S, Chansan P, et al. National trachoma assessment in the Lao people’s democratic republic in 2013-2014. Ophthalmic Epidemiol. 2016;23(Sup1):8–14. doi:10.1080/09286586.2016.1236973.
- Cama A, Müller A, Taoaba R, et al. Prevalence of signs of trachoma, ocular Chlamydia trachomatis infection and antibodies to Pgp3 in residents of Kiritimati Island, Kiribati. PLoS Negl Trop Dis. 2017;11(9):e0005863. doi:10.1371/journal.pntd.0005863.
- Taleo F, Macleod CK, Marks M, et al. Integrated mapping of Yaws and Trachoma in the five Northern-most provinces of Vanuatu. PLoS Negl Trop Dis. 2017;11(1):e0005267. doi:10.1371/journal.pntd.0005267.
- Hiep NX, Ngondi JM, Anh VT, et al. Trachoma in Viet Nam: results of 11 surveillance surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018. In press
- Macleod CK, Butcher R, Mudaliar U, et al. Low prevalence of ocular chlamydia trachomatis infection and active trachoma in the Western Division of Fiji. PLoS Negl Trop Dis. 2016;10(7):e0004798. doi:10.1371/journal.pntd.0004798.
- Dirani M, Keel S, Foreman J, van Wijngaarden P, Taylor HR. Prevalence of trachomatous trichiasis in Australia: the National Eye Health Survey. Clin Exp Ophthalmol. 2017;46(1):13–17. doi:10.1111/ceo.13003.
- Butcher RM, Sokana O, Jack K, et al. Low prevalence of conjunctival infection with chlamydia trachomatis in a treatment-naive trachoma-endemic region of the Solomon Islands. PLoS Negl Trop Dis. 2016;10(9):e0004863. doi:10.1371/journal.pntd.0004863.
- Cocks N, Rainima-Qaniuci M, Yalen C, et al. Community seroprevalence survey for yaws and trachoma in the Western Division of Fiji. Trans R Soc Trop Med Hyg. 2016;110(10):582–587. doi:10.1093/trstmh/trw069.
- Macleod C, Yalen C, Butcher R, et al. Eyelash epilation in the absence of trichiasis: results of a population-based prevalence Survey in the Western Division of Fiji. PLoS Negl Trop Dis. 2017;11(1):e0005277. doi:10.1371/journal.pntd.0005277.
- Butcher R, Sokana O, Jack K, et al. Clinical signs of trachoma are prevalent among Solomon Islanders who have no persistent markers of prior infection with Chlamydia trachomatis. Wellcome Open Res. 2018;3:14. doi:10.12688/wellcomeopenres.13423.2.
- Butcher RMR, Sokana O, Jack K, et al. Active trachoma cases in the Solomon Islands have varied polymicrobial community structures but do not associate with individual non-chlamydial pathogens of the eye. Front Med. 2018;4:251. doi:10.3389/fmed.2017.00251.
- Polack SR, Solomon AW, Alexander ND, et al. The household distribution of trachoma in a Tanzanian village: an application of GIS to the study of trachoma. Trans R Soc Trop Med Hyg. 2005;99(3):218–225. doi:10.1016/j.trstmh.2004.06.010.
- Bailey R, Osmond C, Mabey DC, Whittle HC, Ward ME. Analysis of the household distribution of trachoma in a Gambian village using a Monte Carlo simulation procedure. Int J Epidemiol. 1989;18:944–951.
- Smith JL, Flueckiger RM, Hooper PJ, et al. The geographical distribution and burden of trachoma in Africa. PLoS Negl Trop Dis. 2013;7(8):e2359. doi:10.1371/journal.pntd.0002359.
- Smith JL, Sivasubramaniam S, Rabiu MM, Kyari F, Solomon AW, Gilbert C. Multilevel analysis of trachomatous trichiasis and corneal opacity in Nigeria: the role of environmental and climatic risk factors on the distribution of disease. PLoS Negl Trop Dis. 2015;9(7):e0003826. doi:10.1371/journal.pntd.0003826.
- UNICEF, World Health Organization. Progress on Sanitation and Drinking Water: 2015 Update and MDG Assessment. Geneva: UNICEF and World Health Organization; 2015.
- Garn JV, Boisson S, Willis R, et al. Sanitation and water supply coverage thresholds associated with active trachoma: modeling cross-sectional data from 13 countries. PLoS Negl Trop Dis. 2018;12(1):e0006110. doi:10.1371/journal.pntd.0006110.
- Solomon AW, Kurylo E. The global trachoma mapping project. Community Eye Health. 2014;27:18.
- World Health Assembly. Global Elimination of Blinding Trachoma. 51st World Health Assembly, Geneva, 16 May 1998, Resolution WHA51.11. Geneva: World Health Organization; 1998.
- Correia M, Das T, Magno J, et al. Prevalence and causes of blindness, visual impairment, and cataract surgery in Timor-Leste. Clin Ophthalmol. 2017;11:2125–2131. doi:10.2147/OPTH.S146901.
- Ministry of Health. Summary Report: Rapid Assessment of Avoidable Blindness, Timor-Leste. Dili: Ministry of Health, Timor-Leste; 2017; 2016.
- Sugnanam KK, Ma S, Kreis A, Correia M, Verma N, Dirani M. Prospective study of eye disease in Timor-Leste: the east timor eye program. Asia Pac J Ophthalmol (Phila). 2016;5(5):349–353. doi:10.1097/APO.0000000000000164.
- Ramke J, Palagyi A, Naduvilath T, et al., Prevalence and causes of blindness and low vision in Timor-Leste. Br J Ophthalmol. 2007;91(9):1117–1121. doi:10.1136/bjo.2006.106559.
- Ramke J, Brian G, Naduvilath T, Lee L, Qoqonokana MQ. Prevalence and causes of blindness and low vision revisited after 5 years of eye care in Timor-Leste. Ophthalmic Epidemiol. 2012;19(2):52–57. doi:10.3109/09286586.2011.645108.
- World Health Organization. WHO alliance for the global elimination of trachoma by 2020: progress report on elimination of trachoma, 2014-2016. Wkly Epidemiol Rec. 2017;92(26): 359–368.
- Solomon AW, Emerson PM, Resnikoff S. Trachoma then and now: update on mapping and control. Community Eye Health. 2017;30:90–91.
- Lee L, Ramke J, Blignault I, Casson RJ. Changing barriers to use of eye care services in Timor-Leste: 2005 to 2010. Ophthalmic Epidemiol. 2013;20(1):45–51. doi:10.3109/09286586.2012.742551.
- Palagyi A, Ramke J, du Toit R, et al., Eye care in Timor-Leste: a population-based study of utilization and barriers. Clin Exp Ophthalmol. 2008;36(1):47–53. doi:10.1111/j.1442-9071.2007.01645.x.
- Sallam TA, Raja’a YA, Al-Zubiery TK, et al. Chlamydia trachomatis infections among Yemeni school pupils in relation to environmental conditions. Saudi Med J. 2003;24(1):84–87.
- Berhane Y, Worku A, Bejiga A, et al. Prevalence of trachoma in Ethiopia. Ethiop J Health Dev. 2007;21(3):211–215.
- Bero B, Macleod C, Alemayehu W, et al. Prevalence of and risk factors for trachoma in Oromia regional state of Ethiopia: results of 79 population-based prevalence surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(6):392–405. doi:10.1080/09286586.2016.1243717.
- Elshafie BE, Osman KH, Macleod C, et al. The epidemiology of trachoma in Darfur states and Khartoum state, Sudan: results of 32 population-based prevalence surveys. Ophthalmic Epidemiol. 2016;23(6):381–391. doi:10.1080/09286586.2016.1243718.
- Adera TH, Macleod C, Endriyas M, et al. Prevalence of and risk factors for trachoma in Southern Nations, nationalities, and peoples’ region, Ethiopia: results of 40 Population-based prevalence surveys carried out with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(Sup1):84–93. doi:10.1080/09286586.2016.1247876.
- West SK, Munoz B, Mkocha H, Hsieh YH, Lynch MC. Progression of active trachoma to scarring in a cohort of Tanzanian children. Ophthalmic Epidemiol. 2001;8:137–144.
- Courtright P, MacArthur C, Macleod C, et al. Tropical data: training system for trachoma prevalence surveys (version 1). London: International Coalition for Trachoma Control; 2016. http://tropicaldata.knowledgeowl.com/help/training-system-for-trachoma-prevalence-surveys, Accessed August 30, 2017.
- Solomon AW, Pavluck A, Courtright P, et al. The Global Trachoma Mapping Project: methodology of a 34-country population-based study. Ophthalmic Epidemiol. 2015;22(3):214–225. doi:10.3109/09286586.2015.1037401.
- World Health Organization Strategic and Technical Advisory Group on Neglected Tropical Diseases. Design and Validation of a Trachomatous Trichiasis-Only Survey (WHO/HTM/NTD/PCT/2017.08). Geneva: World Health Organization; 2018.
- King JD, Odermatt P, Utzinger J, et al. Trachoma among children in community surveys from four African countries and implications of using school surveys for evaluating prevalence. Int Health. 2013;5(4):280–287. doi:10.1093/inthealth/iht027.
- Muhit MA, Shah SP, Gilbert CE, Hartley SD, Foster A. The key informant method: a novel means of ascertaining blind children in Bangladesh. Br J Ophthalmol. 2007;91(8):995–999. doi:10.1136/bjo.2006.108027.
