 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Purpose
Ocular injuries pose a significant threat to performance of military functions by the U.S. service members. To estimate the burden of ocular injuries in service members, administrative health records from the Military Health System were collected and analyzed, inclusive of ocular injuries incurred during deployment, military training, or outside of duty hours.
Methods
Patient encounters which matched the predesignated ICD10 codes for ocular injury and complications were extracted and were longitudinally analyzed to categorize patients into complicated (documentation of surgical procedure performed or ocular condition requiring further treatment) or uncomplicated (documentation of injury only). Comparison of incidence rates between groups was made, and geospatial analysis of the number of patients with ocular injury was conducted.
Results
A total of 61,680 incidences of ocular injuries were identified from 2016 to 2019. The incidence rates for complicated and uncomplicated injuries were 21.3 and 82.3 per 10,000, respectively. The incidence rate of uncomplicated injury declined from 2016 to 2019, while that of complicated injury was relatively stable. For complicated ocular injury, the relative risk of males was 62% higher than that of females. The incidence rates of the Army and the Marines were significantly higher than those of the Air Force. California, Texas, and Virginia ranked top three in the numbers of complicated ocular injury patients. Unintentional injuries and struck were the most frequently coded intention and mechanism.
Conclusion
Our results provide the critical information on trends of ocular injuries in relation to demographics, service branches, and occupations. Categorization of the severity of ocular injuries is important to inform health services operations analysis across the Military Health System to enhance medical readiness and improve outcomes.
Introduction
Injuries suffered by the U.S. service members present a continual challenge to the Military Health System (MHS) and can affect unit readiness and individual retention. This is especially true for ocular injuries, as optimal visual function is required for demanding tasks ranging from effective weapons utilizationCitation1 to aircraft-based flight operations.Citation2 Ocular injuries among service members are associated with a substantial cost in terms of resources, rehabilitation, and training.Citation3
Increasing availability of electronic medical records (EMR) has facilitated the surveillance of ocular injury. Routinely collected health care utilization data are available for the U.S. Armed Forces and are regularly analyzed to inform these efforts.Citation4 EMR data are primarily collected for administrative, billing, or auditing purposes. For secondary uses of research, it is necessary to account for coding inconsistency, and ambiguity.Citation5 Case definitions and analysis methodology have been developed based on multiple medical parameters,Citation6 and validation by chart review.Citation7
Accurate and reproducible capture and categorization of ocular injuries based on EMR is critical to inform prevention measures, to guide outcome analysis, and to provide metrics to health care systems. Ocular injuries can be complex and impact multiple anatomical regions of eyes. Recently, we described a new approach to capture and categorize ocular injury from MHS database.Citation8 In this study, we analyzed the trend of ocular injury surveillance of service members of the U.S. Armed Forces in the period of 2016–2019.
Methods
This report employed a novel approach to categorize ocular injuries for improved accuracy based on encounter data in the Military Health System Management and Analysis Reporting Tool (M2).Citation8 Briefly, records of individuals with a documented ocular injury (defined by a set of 320 ICD-10 codes) were searched for documentation of specific complications (additional set of 332 codes) and/or surgical procedures across 12 months following the initial injury documentation. Records from care provided through military treatment facilities and TRICARE network providers were extracted from M2, in addition to injuries occurring in deployed locations through the Theater Medical Data Store (TMDS) from 2016 to 2020. Individuals with documentation of complications or surgical interventions were categorized as complicated, with the remaining categorized as uncomplicated. Surgical procedure codes, a total of 1,543 inpatient (Current Procedural Terminology or CPT) and outpatient procedure codes (Procedure Coding System or PCS) were adapted from the military ophthalmology Knowledge, Skills and Abilities working group stratification. This stratification was developed to assist with the determination of surgical skills needed for military ophthalmologists to successfully perform under combat and/or austere conditions.
The incidence rates of ocular injuries were estimated by demographics, service branch, occupation, and geographical locations. Available analysis of available external causes of ocular injuries codes through documented external cause codes (ECC), i.e. ICD-10 with prefix V00-Y99. Transitions between different care systems were tracked in the analysis.
Incidence Rules: The year of the first documented ocular injury determined the year of incidence. Uncomplicated injuries were counted separately if they were 60 days apart. Complicated injuries were counted only once during the study period.
Statistical analysis
To calculate incidence rates, denominator data were drawn from the Defense Enrollment Eligibility Reporting System (DEERS) module in M2. Poisson regression model was used to compare the incidence rates between groups.
where θ and p are the incidence and population size, respectively; and a, g, and s are age-group (18–24, 25–34, 35–44, and 45-65), gender (female, male), and service branch (Air Force, Army, Marines, and Navy), respectively. β0 is the intercept.
Geospatial analysis of the number of patients with ocular injury was conducted by geo-reference of zip code of care locations. Intent and mechanisms of injury were categorized using the CDC matrix approach.Citation9
The case classification and statistical analysis were conducted in R. The study was completed after review and approved by the Defense Health Agency (DHA) research ethics committee (DHA Office of Research Protection #935913).
Results
We identified a total of 61,680 incidences of ocular injuries through M2 and the Theater Medical data system (TMDS) from 2016 to 2019. Among them, 49,016 (79.5%) were uncomplicated and 12,664 (20.5%) were complicated injuries. Based on the incidence rule, 1,825 patients had more than one uncomplicated injuries.
With an overall rate of 103.57 per 10,000, the incidence rates for uncomplicated and complicated injuries were 82.3 and 21.3 per 10,000, respectively. There was a significant decrease in incidence rates of uncomplicated injuries during the period of 2016–2019 (). The incidence rate of uncomplicated injury declined from 83.7 in 2016 to 72 per 10,000 in 2019. The declined trend of incidence rates of uncomplicated ocular injury was similar by gender, age groups, and services (). By contrast, the incidence rate of complicated injury was relatively stable from 20.7 in 2016 to 20.0(/10,000) in 2019. Similarly, there were no significant changes in annual incidence rates of complicated ocular injury by gender, age group, and services ().
Figure 1. Annual trend of incidence rates (per 10,000) of ocular injuries in relation to gender, age group, and service branch in service members of the U.S. Armed Force from 2016 to 2019 (error bars are 95% confidence interval).
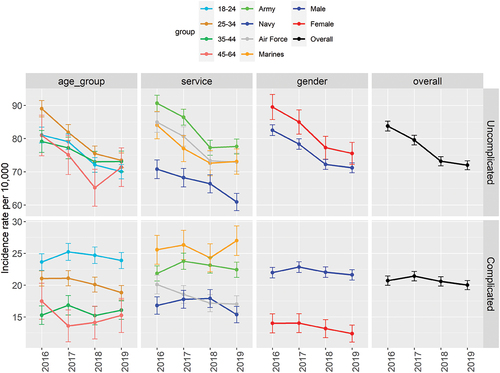
By categories, the highest incidence rate of uncomplicated injury was 86.6 per 10,000 in females in the Air Force, and the highest incidence rate of complicated injury was 26.6 per 10,000 in males in the Marine Corps. The lowest incidence rate of uncomplicated injury was 65.2 per 10,000 in males in the Navy, and the lowest incidence rate of complicated injury was 11.3 per 10,000 in females in the Navy.
For uncomplicated injuries, the most noticeable difference was 15% lower risk in the Navy than the Air Force (p < .001). For complicated ocular injury, it was noted that the estimated relative risk of males was 62% higher than that of females (p < .001). The incidences of age groups of 25–34, 35–44, and 45–64 were lower than that of age group 18–24 by 15% to 39% (p < .001). The estimated incidences of the Army and the Marine Corps were about 20% higher than those of the Air Force (p < .001) ().
Table 1. Estimates of relative risk by multivariate Poisson regression model of incidence rates of ocular injury (the references for gender, age group and service branch are female, age group 18–24, and Air Force, respectively).
Fifty-four percent of complicated injuries and 67% of uncomplicated injuries received care through the direct care system at military treatment facilities (MTF). The percent (22%) of complicated injuries received care from both direct and purchased care which was higher than uncomplicated injury (7%). The percent of patients who received purchase care only was similar for uncomplicated injury (22%) and complicated injury (23%).
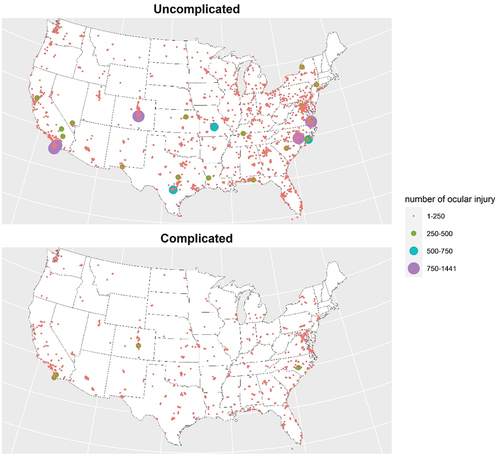
High volumes of ocular injury patients gravitated to a few military medical centers, e.g., Darnall Army Medical Center in Texas and Navy Medical Center San Diego in California (). The top three states in numbers of complicated and uncomplicated injuries were California (1,376 and 4,665), Virginia (939 and 3,534), and North Carolina (919 and 3,480).
Figure 2. Geospatial distribution of the total numbers of ocular injuries in service members of the U.S. Armed Force by zip codes of military treatment facilities in the Continental U.S.
There were substantial numbers (62%) of ocular injury patients with missing values of external cause codes. There were significant differences in compliance of recorded cause code between direct care and purchased care. Patients treated through the direct care system had higher compliance rate in 58% of individuals (53% of uncomplicated injuries, 78% of complicated injuries) than those treated through the purchased care system (32%) (28% of uncomplicated injuries, 44% of complicated injuries). Patients who received treatment through both systems (Dual Care) had ECCs documented in 55% of individuals (44% of uncomplicated injuries, 70% of complicated injuries).
Overall, the compliance of documentation of external causes of ocular injuries was suboptimal. The percentages of ocular injuries with recorded external causes of intention, mechanism, activity, and alcohol use accounted for 37.1%, 39.1%, 14.4%, and 0.3%, respectively. For the documented external causes, unintentional injuries comprised the majority of complicated (85.3%) and uncomplicated injuries (90.8%). Struck by/against was the most frequent occurrence for mechanism causes, in complicated (56.5%) and uncomplicated injuries (45.6%) ().
Table 2. The number of ocular injuries associated with external causes.
Incidence rates of ocular injury varied widely among occupations. Infantry, medical care personnel, supply providers, aircraftmen, law enforcement personnel, and automotive personnel scored high in case number, although the incidence rates of these occupations were not the highest ().
Table 3. Number of ocular injury for occupations (in decreasing order in occurrence) in active duty members of the U.S. Armed Forces during 2016–2019.
Discussion
Ocular injuries continue to pose a threat to the U.S. military. It is a critical function to be able to track injuries with high fidelity to understand the impact on the force. Previous studies had reported incidences of ocular injury in the U.S. service members. The current surveillance program by Armed Forces Health Surveillance Branch (AFHSB) reports ocular injuries in nine group by the impacted anatomic regions or severity of the injuries (Superficial, Lid/Adnexa, Contusion, Posterior Segment, Orbit, High-Risk Blindness, Anterior Segment, Burns, and Optic/Cranial Nerve).Citation10 However, direct comparison of the incidence between these reports is difficult because different case definitions were used and various study designs adopted. For example, the current surveillance by AFHSB adopts a case definition as the matched diagnosis of the first or the initial encounter of ocular injury. Given the difficulties of diagnosis of ocular injury by non-specialists in constrained settings, we categorize ocular injuries by assessing the presence of complications and treatments following the initial diagnosis to improve accuracy of identification of ocular injury. By dichotomizing injuries into complicated versus uncomplicated injury, we provide the critical data of the severity of the injuries for needed advanced medical treatments to improve the readiness of military medical providers.
Uncomplicated injuries showed a significant decrease starting at 2018 and was similar by age groups, gender, and service branches. The underlying reasons of the observed declines are not immediately obvious. Further studies are needed to ascertain factors responsible for this decrease in rates. On the other hand, incidence rates of complicated injuries show no significant change over the time period studied. The different trends between two injury categories might indicate the different driving mechanisms, e.g., preventive efforts might be more effective for curbing certain types of ocular injuries.
Intra-year variability was examined to evaluate for any monthly or seasonal variations of ocular injuries. No significant differences between seasons were noted, although the rate in summer was slightly higher (data not shown). Previous studies have found increased rates of emergency department visits for ocular injuries between May and July, postulating that warmer temperatures and longer daylight hours influenced ocular injury rates.Citation11 Identification of seasonal changes in ocular injuries would inform prevention strategies in military populations, which may have increased exposure of military activities and off duty activities during the warmer seasons.
Geolocation of ocular injuries treatment showed a wide distribution across the continental U.S with a few clusters of higher volumes of both uncomplicated and complicated injuries in areas of military medical centers. The clustered patterns reflects high densities of military personals and the need of military medical centers with advanced experience in treating ocular injuries. Geospatial information could be used to focus prevention efforts and to inform resource allocation.Citation12 From the perspective of medical readiness, it is important to allocate adequate resources to increase effectiveness of treatment based on the estimated volumes of ocular injuries.
The Military Health System provides care for beneficiaries through multiple care pathways. Service members may receive treatment through the direct care system from MTF, the purchased care system (care provided by civilian providers outside of the MTF system), or a combination of both systems. We found that more than half of complicated injuries received cares from MTFs. This information is needed to evaluate mobility of care seeking in and out of the direct care as well as strategic planning for improvement of care in MTFs. Estimation of the relative care burden can provide insight into the availability of ocular trauma cases treated by military providers which is essential to support the capabilities of a ready medical force (providers trained and capable to provide the best available care when deployed in support of missions).
Given the caveat of low compliance of coding of causes and activities, our results provide the useful data for identifying intention/mechanisms associated with ocular injuries and high-risk occupations. Of note, unintentional injuries and struck were predominant intent/mechanism in the documented cases. Ocular injury was predominantly associated with sports/physical training, although only a small proportion of patients had the coded activities. Therefore, prevention measures such as wearing approved eye protection during physically aggressive activities, including sports and physical training, may alleviate ocular injuries among service members. Evaluation of ECC showed the majority of ocular injuries were associated with military activity. Similarly, the extremely low frequency of coded alcohol use might be due to poor compliance of coding. Of note, alcohol involvement appeared more frequent in complicated injuries (0.75%) than in uncomplicated injuries (0.24%). Similar findings have been described previously, with risk behavior and alcohol consumption being independently associated with more severe open-globe injuries.Citation13
There are several limitations. As noted, low compliance of coding circumstances of ocular injuries could bias our findings if undocumented cases were not representative sample. Of note, service members treated in the direct care system had a higher proportion of documented ECCs than the purchased care systems. Guidance is needed to provide adequate coding of intention/mechanism, activity, and ECCs to inform injury surveillance efforts.Citation14 Unlike the current surveillance of AFHSB, which adopts a broad categories of occupations,Citation10 we provide the granular occupations of M2 to highlight the specific occupations associated with the high risk. Precaution should be taken to attribute the differential risks to occupations in observational data like M2 since the data did not reveal circumstances of the injuries, e.g., at home or at work. One survey study of small sample (94 military personnel) showed that most (35%) of ocular injury occurred at home as compared with the work-related (24%).Citation15 Our findings might be useful to select individuals from the identified high-risk groups for survey studies or chart review to reveal the locations (e.g., whether at work or at home) to evaluate the role of occupations in ocular injury.
Ocular injuries present an ongoing challenge to the ability of service members to execute military duties with optimum visual performance. Accurate capture and categorizations of these injuries are essential for ongoing prevention, diagnosis, mitigation, treatment, and rehabilitation. The M2 database contains comprehensive records documenting all clinical encounters of patients. Many of these encounters occurred at primary care or emergency rooms where accurate diagnoses of complex ocular injury were extremely difficult. Categorizing ocular injuries by assessing the longitudinal course of an ocular injury for complications and treatments provides advantages to improving accuracy of identification of ocular injury.Citation8
Injury preventions use the policies of three E approach: education, engineering, and enforcement. It is important to examine potential risk factors and prognostic factors for designing preventive programs and predicting outcomes. Our results provide the data of ocular injuries which require specific surgical procedures to inform health services operations analysis across the MHS to enhance medical readiness and improve outcomes. Our results shed light on high-risk groups for target public health messaging and prevention campaigns. Additionally, this detailed characterization can provide the guidance to prioritize chart review and abstraction of medical encounters in a comprehensive ocular registry (the Defense and Veterans Eye Injury Registry DVEIVR).Citation16
Authorship
M. R. and W. G. contributed in the literature search, study design, data collection, data analysis, data interpretation, and writing of the manuscript.
Disclaimer
The views expressed are solely those of the authors and do not reflect the official policy or position of Defense Health Agency, the Department of Defense, or the US Government.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Hatch BC, Hilber DJ, Elledge JB, Stout JW, Lee RB. The effects of visual acuity on target discrimination and shooting performance. Optom Vis Sci. 2009;86(12):E1359–1367. doi:10.1097/OPX.0b013e3181be9740.
- Tanzer DJ, Brunstetter T, Zeber R, et al. Laser in situ keratomileusis in United States Naval aviators. J Cataract Refract Surg. 2013;39(7):1047–1058. doi:10.1016/j.jcrs.2013.01.046.
- Frick KD, Singman EL. Cost of military eye injury and vision impairment related to traumatic brain injury: 2001-2017. Mil Med. 2019;184(5–6):e338–e343. doi:10.1093/milmed/usy420.
- Brundage JF, Johnson KE, Lange JL, Rubertone MV. Comparing the population health impacts of medical conditions using routinely collected health care utilization data: nature and sources of variability. Mil Med. 2006;171(10):937–942. doi:10.7205/MILMED.171.10.937.
- Valikodath NG, Newman-Casey PA, Lee PP, Musch DC, Niziol LM, Woodward MA. Agreement of ocular symptom reporting between patient-reported outcomes and medical records. JAMA Ophthalmol. 2017;135(3):225–231. doi:10.1001/jamaophthalmol.2016.5551.
- Singla M, Hutfless S, Al Kazzi E, Rodriguez B, Betteridge J, Brant S. Clinical codes combined with procedure codes increase diagnostic accuracy of Crohn’s disease in a US Military health record. BMJ Open Gastroenterol. 2020;7(1):e000378. doi:10.1136/bmjgast-2020-000378.
- Cave AJ, Soos B, Gillies C, Drummond N, Pham ANQ, Williamson T. Validating a case definition for adult asthma in primary care electronic medical records. NPJ Prim Care Respir Med. 2020;30(1):24. doi:10.1038/s41533-020-0181-3.
- Reynolds ME, Gu W. A new approach to categorization of ocular injury among U.S. Armed Forces. MSMR. 2022;29:8–14.
- Annest J, Hedegaard H, Chen L, Warner M, Smalls E. Proposed Framework for Presenting Injury Data Using ICD–10–CM External Cause of Injury Codes. Atlanta, Georgia: Centers for Disease Control and Prevention; 2014.
- Armed Forces Health Surveillance Branch, Program T-SVCaR. US department of defense (DoD) combined active duty eye injury summary calendar year 2019. 2019.
- Ramirez DA, Porco TC, Lietman TM, Keenan JD. Ocular injury in United States emergency departments: seasonality and annual trends estimated from a nationally representative dataset. Am J Ophthalmol. 2018;191:149–155. doi:10.1016/j.ajo.2018.04.020.
- Stewart CL, Acker SN, Pyle L, Smith DS, Bensard DD, Moulton SL. Mapping pediatric injuries to target prevention, education, and outreach. J Pediatr Surg. 2017;52(8):1287–1291. doi:10.1016/j.jpedsurg.2016.12.023.
- Rufer F, Peters A, Klettner A, Treumer F, Roider J. Influence of alcohol consumption on incidence and severity of open-globe eye injuries in adults. Graefes Arch Clin Exp Ophthalmol. 2011;249(12):1765–1770. doi:10.1007/s00417-010-1533-4.
- Canham-Chervak M, Steelman RA, Schuh A, Jones BH. Importance of external cause coding for injury surveillance: lessons from assessment of overexertion injuries among U.S. Army soldiers in 2014. Msmr. 2016;23:10–15.
- Lau JJ, Thach AB, Burden JH, Ward TP, Hshieh PB, Hollifield RD. Eye injuries in the U.S. Armed Forces. Mil Med. 2000;165(9):683–686. doi:10.1093/milmed/165.9.683.
- Colyer MH. Department of defense and eye injury data: shedding new light. Mil Med. 2020;185(11–12):487–488. doi:10.1093/milmed/usaa156.
