ABSTRACT
Background
In baseline trachoma prevalence surveys, six districts in two governorates of Yemen were identified as requiring interventions. We set out to estimate the prevalence of trachoma 6−12 months after one round of antibiotic mass drug administration (MDA) and implementation of measures to encourage facial cleanliness.
Methods
A population-based prevalence survey was conducted in each of the four evaluation units in October 2019. Contemporary World Health Organization recommendations for trachoma surveys were followed. Participants were selected using a two-stage cluster sampling process. The prevalence of inflammatory and late-stage trachoma was measured through eye examination. Water, sanitation, and hygiene facility access among visited households was estimated.
Results
The prevalence of trachomatous inflammation—,follicular (TF) in 1–9-year-olds per EU was <5.0% in three EUs (Al Mighlaf, Al Munirah, and As Salif; Az Zaydiyah; and Mudhaykhirah districts) and 5.0–9.9% in one EU (Far Al Udayn District). The prevalence of TT unknown to the health system in ≥15-year-olds per EU was <0.2% in all four EUs. Per EU, the proportion of households with an improved drinking water source ranged from 40% to 100%; access to an improved drinking water source within 30-minute return journey of the household ranged from 45% to 100%; and with an improved latrine ranged from 32% to 83%.
Conclusion
An additional round of antibiotic MDA should be administered in Far Al Udayn district before it is resurveyed. In the other surveyed districts, pre-validation surveillance surveys should be conducted in 2 years’ time to determine if the TF prevalence <5% has been maintained.
Introduction
Trachoma, caused by ocular infection with Chlamydia trachomatis, is the leading infectious cause of blindness globally.Citation1 The infection is thought to spread through contact with eye and nose discharge from an infected person, transmitted on fingers, fomites, and eye-seeking flies.Citation2–4 After years of repeated infection, the inside of the eyelid may become scarred, and this can cause distortion of the eyelid, resulting in eyelashes rubbing on the eyeball. The presence of one or more eyelashes touching the eyeball or evidence of recent eyelash epilation, is known as trachomatous trichiasis (TT).Citation5 (The TT definition was amended in November 2018 to exclude trichiasis that affects only the lower eyelid.Citation6) TT is very painful and, if untreated, can lead to the formation of corneal opacity and subsequently to irreversible blindness.Citation7
The World Health Organization (WHO)-endorsed SAFE (Surgery, Antibiotics, Facial cleanliness, and Environmental improvement) strategy for trachoma elimination has been implemented in over 40 trachoma-endemic countries worldwide.Citation8,Citation9 Eyelid surgery corrects the misdirected eyelashes to prevent them from rubbing on the eyeball. Mass drug administration (MDA) of antibiotics is indicated in evaluation units (EUs, defined as the local administrative unit for healthcare management, generally having a population of 100,000–250,000Citation10) where the trachomatous inflammation—follicular (TF) prevalence in 1–9-year-olds is ≥5%. The recommended strategy involves delivering oral azithromycin (or 1% tetracycline eye ointment if azithromycin is unavailable or contra-indicated) to all EU residents, with a minimum acceptable coverage target of 80%. Promotion of facial cleanliness and environmental improvement are intended to facilitate sustained reductions in transmission of the pathogen.Citation11 The implementation of SAFE in order to eliminate trachoma as a public health problem is guided by the EU-level prevalence of trachoma assessed by population-based prevalence surveys before MDA (baseline surveys), 6–12 months after the last recommended MDA round (impact surveys) and 2 years after the last impact survey resulted in a TF prevalence <5% (surveillance survey). Whereas A, F, and E interventions are recommended when the prevalence of TF in 1–9-year-olds is ≥5%, community-level S services are needed when the prevalence of TT unknown to the health system in ≥15-year-olds is ≥0.2%.Citation11,Citation12
Trachoma is endemic in Yemen.Citation13–15 Baseline mapping took place in two phases from 2013−2015 as part of the Global Trachoma Mapping Project (GTMP). The first phase of population-based surveys for trachoma was conducted in 2013 and covered four governorates, namely Hodeidah, Ibb, Mareb, and Al-Jawf. Six EUs (covering 25 districts) of the 15 surveyed had a TF prevalence ≥5%; two EUs (6 districts) required three annual MDA rounds and four EUs (19 districts) needed one MDA round.Citation14,Citation15 The highest prevalence of 12.6% was found in the EU covering As Sabrah, As Sayyani, and Dhi As Sufal districts of Ibb governorate.Citation14,Citation15 The second phase of baseline surveys took place between 2013 and 2015 and identified two further EUs (covering five districts of the Hajjah governorate) in need of MDA.Citation14 In May 2018, one round of MDA was conducted in six districts in Hodeidah and Ibb governorates based on the results of the baseline surveys. More districts were eligible for MDA but for funding and security reasons, the program decided to select these six for the first phase of MDA. Hygiene kits (containing soap and a cloth) were distributed to all families with children alongside health promotional activities to help encourage facial cleanliness in the community. Health promotion activities included the distribution of brochures promoting regular, effective face washing and broadcast of health promotion messages on radio spots, from megaphones in cars and from mosques. Interventions were focused on changing behaviour: no water, sanitation, and hygiene (WASH) infrastructure improvement projects were carried out for the purposes of trachoma elimination between the baseline and impact surveys. The six districts in which elimination measures were implemented correspond to two of the eight EUs with a TF prevalence ≥5% during baseline mapping. They included all four districts from one pre-MDA EU in Hodeidah governorate and two of the three districts from another pre-MDA EU in Ibb governorate.
Here, we aimed to estimate the prevalence of TF in 1–9-year-olds and of TT in ≥15-year-olds in four EUs covering the six districts treated in May 2018, 6 months after receiving the recommended single MDA round. The purpose of estimating prevalence was to determine if the elimination thresholds had been met, or whether further trachoma elimination activities were required.
Methods
Study ethics and consent
These surveys were approved by the Ethical Committee of Sana’a University (November 2018). Tropical Data survey support for trachoma surveys was approved by the London School of Hygiene & Tropical Medicine Observational Ethics Committee (16105).
Communities were contacted in advance of the teams’ arrival. The teams were accompanied by a village guide familiar with the local community. The teams sought verbal consent from household heads to enroll households in the study. All participants aged ≥18 years were required to provide verbal consent before they could take part. Verbal consent from a parent or guardian was required before people aged <18 years could take part in the surveys.
Standard quality control and quality assurance mechanisms for trachoma surveysCitation16 were implemented throughout.
Survey design and participant selection
The surveys were designed to meet WHO standards for population-based prevalence surveys for trachoma.Citation17 EUs for the survey were defined according to the WHO definition of a health district for trachoma elimination purposes. The three districts had an estimated population of 100,000–250,000 and were each allocated to their own EU. There were three other districts in Al Hodeidah governorate with a population <100,000 and which were merged into a single EU ().
Table 1. Population enumerated, examined, and reasons for nonparticipation during trachoma impact surveys in two governates of Yemen, October 2019.
Because the country is under conflict, there were security issues throughout these surveys. These were managed as diplomatically as possible to enable the surveys to continue. People carrying mobile phones could be arrested at the time of the surveys: for this reason, paper-based data collection forms were used rather than mobile-based forms. Survey schedulers kept security at the forefront of their planning and, as in similarly insecure environments,Citation18,Citation19 communicated closely with district-level health authorities before and during surveys to ensure teams were working in the safest possible way.
In each EU, we planned to recruit enough children to estimate a TF prevalence of 4% in 1–9-year-olds with a precision of 2% at the 95% confidence level. After inflating by a design effect of 2.63 to account for disease clusteringCitation20 and by a non-response rate inflation factor of 1.2 to account for enumerated people not taking part, we determined that sufficient households to yield 1,164 children should be visited in each EU. A two-stage cluster sampling approach was taken to recruit survey participants. The primary sampling unit was the village, and the secondary sampling unit was the household. We estimated there would be 2.03 children aged 1–9 years per household in these governorates and that 30 households could reasonably be visited per village per day by a field team. Consequently, 20 villages per EU were needed to meet our sample size. All residents of the selected households aged 1 year and above were eligible to be enrolled in the survey.
Training of graders and recorders
The training of trachoma graders and recorders followed the training system outlined in the 2017 Tropical Data Training Manual.Citation21 The grader trainees were general medical practitioners. The recorder trainees were university or college graduates who had experience using Smartphones and other electronic devices. Where possible, those who participated in the previous baseline surveys were preferentially selected to take part in training. Both the grader and recorder trainees were selected based on their knowledge of the local culture, traditions, and language, and on their ability to build good relationships and demonstrate a respectful attitude when challenged by individual or community beliefs and values.
To be qualified to work as trachoma graders, selected grader trainees were required to attend a standardised four-day training course and score a kappa of ≥0.7 in grading a set of 50 images compared with a consensus grade of international trachoma grading experts, and again in grading 50 school children compared to a certified grader trainer. Recorder trainees were required to attend a standardised training course, which included training for the classification of water sources and sanitation facilities, and pass a competency assessment to work as recorders in the surveys.
After the standard Tropical Data training, both graders and recorders attended an additional training session on the use of paper data collection forms and transcription to the Tropical Data data collection tool.
Household and clinical data collection
Upon arrival at the household, the recorder collected data on the household access to WASH facilities. Questions were taken from a version of the WHO/United Nations Children’s’ Fund (UNICEF) Joint Monitoring Programme (JMP) household questionnaire modified for trachoma surveys.Citation22,Citation23 Recorders visited water sources and toilet facilities to determine what type they were, whether toilets had a handwash facility (this was only assessed where a household had a latrine) and whether water and soap were available at the handwash station. Latrines flushing to open drains were considered unimproved.
Consenting participants had both eyes examined for TT, TF, trachomatous inflammation—intense (TI) according to the WHO's simplified trachoma grading system.Citation5 The grader used 2.5× binocular loupes and sun- or torch-light. Eyes with TT (using the then-current TT definition, which did not exclude lower eyelid trichiasis) were additionally examined for trachomatous scarring (TS); the eyelid (upper or lower) from which any misdirected eyelash originated was not recorded. Participants with TT were asked whether they had been offered surgery or epilation for their TT, and whether they had accepted. Participants who had not or could not recall being offered either intervention in the eye with TT were classified as having TT ‘unknown to the health system’.
Households in which children aged 1–9 years were absent at the time of the team’s first visit were re-visited once before the end of the day to maximise recruitment.
Household and individual data were collected onto paper versions of the Tropical Data data collection tool. Data were then transcribed into a smartphone-based version of the Tropical Data app at the end of each day by two separate recorders. Data were submitted to Tropical Data-administered servers as soon as possible once a data connection was available. The duplicate submissions were compared by a data manager, and discrepancies between the two entries were identified. Discrepancies were sent back to the data entry personnel, who checked the paper forms to confirm the correct response.
Data analysis
EU prevalence was determined by taking the mean of the age-adjusted (TF) and age- and gender-adjusted (TT) village-level disease proportions, as previously described.Citation22 Confidence intervals were generated by computationally resampling adjusted village-level proportions, with replacement, 10,000 times and taking the 2.5th and 97.5th centile of the resulting distribution.
Association between TF and individual and household variables was conducted using mixed effects binomial regression, with village of residence included as a random-effects variable in all models. We tested whether the addition of variables to the null model improved the model fit using likelihood ratio tests. Only one variable was significant in univariable testing, so no multivariable testing was conducted. The association between TT and individual and household variables was not tested because there were too few cases of TT.
Results
Participant characteristics
Fieldwork for all four surveys was completed in October 2019. A total of 11,682 people aged ≥1 year were enumerated across four EUs (range: 2,747–3,147 per EU). A total of 11,118 (95%) of those enumerated were examined, with the proportion examined ranging from 93 to 97% by EU (). Overall, 289 (2%) were absent at the time of the teams’ visit, 217 (2%) refused to take part and 58 (<1%) had another, unspecified reason for not taking part. Notably, 212/217 (98%) of those who refused to take part in the study were female. Of the people examined, 3,811 (34%) were aged 1−9 years and 5,586 (50%) were aged ≥15 years.
Signs of trachoma
A total of 358 individuals were identified with TF in at least one eye, of whom 171 were aged 1−9 years (). There were 16 people with TI in at least one eye, of whom 6 were aged 1−9 years. Just over half (94/171) of TF cases in 1−9-year-olds were bilateral. The EU-level prevalence of TF in 1−9-year-olds ranged from 2.3 to 7.9%. The TF prevalence was <5% in three of the four surveyed EUs and 5.0−9.9% in one EU (, ). Three post-MDA EUs had a lower point prevalence of TF in 1−9-year-olds than that of the EU they were surveyed as previously; one had a higher prevalence ().
Figure 1. Prevalence of trachomatous inflammation—follicular (TF) in 1−9-year-olds in trachoma impact surveys of four evaluation units of Yemen, October 2019. The prevalence of trachomatous trichiasis (TT) unknown to the health system in ≥15-year-olds was <0.2% in all EUs surveyed. The boundaries and names shown and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the authors, or the institutions with which they are affiliated, concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries.
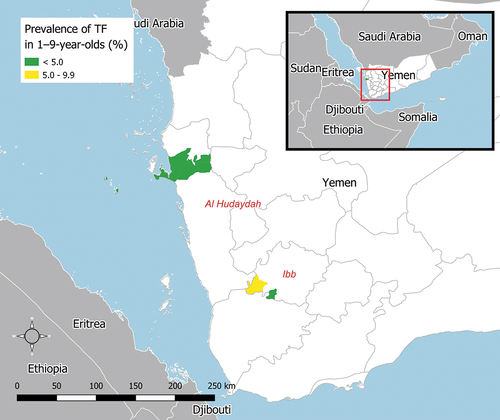
Figure 2. Change in prevalence of trachomatous inflammation—follicular (TF) in 1−9-year-olds following one round of antibiotic mass drug administration. X-axis coordinates have been artificially adjusted to prevent overlap and allow confidence intervals to be seen more clearly. Pre-MDA prevalence estimates are taken from Thabit et al., 201814. Pre-MDA prevalence estimates in Al Hodeidah governate are from four districts surveyed as a single EU: Al Mighlaf, Al Munirah, As Salif and Az Zaydiyah. Prevalence estimates from Ibb governate are from three districts surveyed as a single EU, one of which was not re-surveyed in this series: Al Udayn (not resurveyed), Far Al Udayn and Mudhaykhirah. Because the pre-MDA and post-MDA EU boundaries are not identical, potential changes in prevalence between time points are not interpretable.
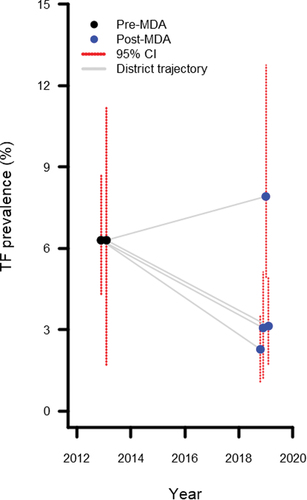
Table 2. Prevalence of trachomatous inflammation—follicular (TF) in children aged 1−9 years in trachoma impact surveys of two governates of Yemen, October 2019.
There were nine people with TT identified among 5,586 people aged ≥15 years examined (). Four of those individuals with TT were women. Three of the nine individuals were affected in both eyes. Of the nine people with TT, seven also had TS and eight reported not being offered or not remembering being offered epilation or surgery. The prevalence of TT unknown to the health system was <0.2% in all EUs surveyed ().
Table 3. Prevalence of trachomatous trichiasis (TT) in people aged ≥15 years in trachoma impact surveys, two governates of Yemen, October 2019.
Water, sanitation, and hygiene access
A total of 2,417 households were visited across the four EUs. Overall, 1,884 (78%) had an improved drinking water source, 1,851 (77%) had a drinking water source within a 30-minute return journey of the house, and 1,321 (55%) had an improved latrine. The EU-level findings are presented in . The coverage of improved water sources and water sources <30 minutes from the household was noticeably lower in Far Al Udayn compared with the other EUs. Overall, 470 (19%) households practiced open defecation. Among households with a latrine (n = 1,947), 422 (22%) had a handwash station of which 323 (77%) had water and soap available at the time of the teams’ visit. TF was more common in households with an unimproved or surface washing water source compared with an improved washing water source (odds ratio: 2.1, 95% confidence interval: 1.1−3.8; p=0.026; Supplementary Table 1).
Table 4. Household water, sanitation and hygiene access, trachoma impact surveys, two governates of Yemen, October 2019.
Discussion
Interventions to reduce the prevalence of trachoma have been implemented in a number of districts of Yemen following surveys throughout the country undertaken from 2013 to 2015.Citation14 Here, we report TF prevalence in the first of these districts to be resurveyed post-MDA. Three of the four EUs surveyed here, covering five districts with a collective population estimate of almost 380,000 people, have now recorded a TF prevalence of <5%, indicating MDA can be stopped and surveillance surveys conducted after 2 further years. One EU (Far Al Udayn, with an estimated population of approximately 125,000 people) had a TF prevalence of 7.9%, suggesting one additional round of MDA is needed before a repeat impact survey is conducted.Citation25,Citation26
, which presents a change in TF prevalence following one MDA round, may be interpreted as suggesting that TF prevalence increased following MDA in one district and decreased in the others. The evidence here is insufficient to make either claim, as EU boundaries changed between pre- and post-MDA surveys. We do not feel that to be a limitation of this paper, as the primary intention of the surveys was to help programmatic planning going forward, rather than to compare with previous trachoma estimates.
The prevalence of TT unknown to the health system in ≥15-year-olds was <0.2% in all four EUs surveyed. However, WHO recommendations on TT prevalence surveys suggest that a minimum sample of 2,818 people or 30 primary-stage clusters per EU is required to estimate TT prevalence with enough precision to claim the elimination target has been achieved.Citation27 We did not meet that minimum sample size in these surveys, so must assume the prevalence estimates are imprecise. Indeed, the upper bound of the confidence intervals around our prevalence estimates in the two EUs where TT cases were identified exceeded 0.2%. Geostatistical modelling, as recently applied to TT prevalence data from Ethiopia,Citation28 may allow us to derive sufficient precision from the existing data presented here. In the meantime, active TT case findings should continue in the surveyed areas. A sustainable strategy to identify and manage incident cases in the longer term should also be developed to ensure those exposed to ocular C. trachomatis infection during their childhood can be effectively treated. This is also one of the criteria to achieve elimination of trachoma as a public health problem.Citation29
Access to WASH facilities in the areas surveyed was variable. There was some evidence of a relationship between TF and living in a household without an improved washing water source. It is also interesting to note that coverage of drinking water access was lowest in the EU with the highest TF prevalence. However, the relationship between trachoma and water use is likely to be much more complex than could be captured in a survey like this, and a linear relationship between distance to water source and trachoma prevalence is unlikely.Citation30–32 Lower coverage of easy access to improved water facilities is likely to be a general indication of a comparatively less economically developed area. Trachoma elimination activities in Yemen have, to date, focused on encouraging behaviour change. These should continue to be implemented in these regions to maintain the gains made by interventions so far. Targeted WASH infrastructure improvement may enable more regular face washing and may have additional health and socioeconomic benefits. This should be considered as a component of future trachoma elimination measures.
The findings here are somewhat different from findings from other contemporary reports on access to WASH infrastructure in Yemen. For example, a report from the Yemen WASH Cluster estimated <20% of the population to have access to improved water sources in Al Hodeidah governorate,Citation33 whereas we found >80% of households to have an improved water source. There is heterogeneity in the methods used to estimate WASH infrastructure coverage, which could explain this difference. Moving towards integration of data collection or at least ensuring methodological standardisation is important for monitoring progress of the E component of SAFE and is likely to have benefits for other sectors, too.Citation24,Citation34,Citation35
These surveys were affected by security challenges, for example, there were many road checkpoints during the fieldwork. In addition, paper-based data collection had to be used rather than mobile-based forms. Both of these factors increased survey time, with budget implications. The advantages of electronic data collection have been previously outlined,Citation22,Citation36 but it was not possible to employ this methodology for this survey series due to insecurity. The use of paper forms resulted in additional personnel costs in order to conduct double data entry and resolve discrepancies, and delays from data collection to having clean data available for analysis. This limited our ability to provide data-related feedback to teams whilst they were still in the field, and meant teams were unable to proceed with the fieldwork schedule as they waited for data entry from the previous EU to be completed. There were other limitations to these findings: our survey sample size target was not met in two EUs (covering Al Mighlaf, Al Munirah and As Salif, and Az Zaydiyah). This would have resulted in a slightly reduced precision in the TF prevalence estimate compared to what we planned. We also did not survey enough villages per EU to make a TT estimate with the precision to declare the elimination threshold to have decisively been reached, as described above.
Looking forward, the programme plans to continue with impact surveys in the remaining EUs, which have received the requisite number of MDA rounds. This should include Al Udayn district, which was included in the GTMP Ibb governorate at baseline but not included in the impact surveys presented here. Surveillance surveys should be planned in the districts of Ibb and Al Hodeidah, which have now met the elimination targets, whilst taking into account security challenges, which will likely disrupt programme planning and implementation in some parts of the country. Shabwah and Amran governorates were too insecure for survey activities during the GTMP: baseline surveys are still needed there.
Conclusion
The reduction of TF below the elimination target in three of four surveyed EUs is a promising step in Yemen’s progress towards elimination of trachoma as a public health problem. Future impact surveys conducted following antibiotic MDA will determine the need for additional MDA rounds. Surgical services, facial cleanliness, and environmental improvement should all continue to be implemented to ensure the sustainability of trachoma elimination.
Disclaimer
The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated, USAID or the United States Government.
Supplemental Material
Download MS Word (16.2 KB)Acknowledgments
We acknowledge MedVeritas for providing technical support to the impact surveys under the supervision of the Trachoma Control Program, Ministry of Public Health and Population, Yemen.
Disclosure statement
AB and SB are employed by the International Trachoma Initiative at The Task Force for Global Health, which receives an operating budget and research funds from Pfizer Inc., the manufacturers of Zithromax® (azithromycin). EMHE receives salary support from the International Trachoma Initiative.
The other authors declare no conflicts of interest.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/09286586.2023.2180805
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e1234.doi:10.1016/S2214-109X(17)30393-5.
- Last A, Versteeg B, Abdurahman OS, et al. Detecting extra-ocular chlamydia trachomatis in a trachoma-endemic community in Ethiopia: identifying potential routes of transmission. PLoS Negl Trop Dis. 2020;14(3):18–32.doi:10.1371/journal.pntd.0008120.
- Versteeg B, Vasileva H, Houghton J, et al. Viability PCR shows that non-ocular surfaces could contribute to transmission of chlamydia trachomatis infection in trachoma. PLoS Negl Trop Dis. 2020;14(7):1–12.doi:10.1371/journal.pntd.0008449.
- Miller K, Pakpour N, Yi E, et al. Pesky trachoma suspect finally caught. Br J Ophthalmol. 2004;88(6):750–751.doi:10.1136/bjo.2003.038661.
- Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bull World Health Organ. 1987;65:477–483.
- Solomon AW, Kello AB, Bangert M, et al. The simplified trachoma grading system, amended. Bull World Health Organ. 2020;98(10):645–724. doi:10.2471/BLT.19.248708.
- Taylor HR. Trachoma: A Blinding Scourge from the Bronze Age to the Twenty-First Century. East Melbourne: Centre for Eye Research, Australia; 2008.
- World Health Organization. WHO alliance for the global elimination of trachoma by 2020: progress report on elimination of trachoma. Wkly Epidemiol Rec. 2020;2021(31): 353–364.
- Francis V, Turner V. Achieving Community Support for Trachoma Control: A Guide for District Health Work (WHO/PBL/93.36). Geneva, Switzerland: World Health Organization; 1993.
- World Health Organization. Report of the 3rd Global Scientific Meeting on Trachoma. 2010;19-20 July . Johns Hopkins University, Baltimore, MA; WHO/PBD/2.10 Geneva, Switzerland.
- Solomon A, Zondervan M, Kuper H, Buchan J, Mabey D, Foster A. Trachoma Control: A Guide for Program Managers. Geneva, Switzerland: World Health Organization: World Health Organization; 2006.
- International Coalition for Trachoma Control. Transition planning for trichiasis management services. London, UK; 2019. https://www.ICTC_TransitionPlanningTrichiasis_041819_FINALonline_0.pdf (trachomacoalition.org).
- Al-Khatib TK, Hamid AS, Al-Kuhlany AM, Al-Jabal MH, Raja’a YA. Rapid assessment of trachoma in 9 governorates and Socotra Island in Yemen. East Mediterr Heal J. 2006;12:566–572.
- Ali Thabit A, Al-Khatib T, Hail WHM, et al. Prevalence of trachoma in Yemen: results of population-based prevalence surveys of 42 evaluation units in nine governorates. Ophthalmic Epidemiol. 2018;25(sup1):62–69.doi:10.1080/09286586.2018.1441426.
- Ali Thabit A, Al-Khatib T. Prevalence of trachoma in 4 governorates in Yemen. Sana’a Univ J Med Sci. 2017;11:1–6.
- Solomon AW, Willis R, Pavluck AL, et al. Quality assurance and quality control in the global trachoma mapping project. Am J Trop Med Hyg. 2018;99(4):858–863.doi:10.4269/ajtmh.18-0082.
- World Health Organization. Design Parameters for Population-Based Trachoma Prevalence Survey (WHO/HTM/NTD/PCT/2018.07). Geneva, Switzerland: World Health Organization; 2018.
- Elshafie BE, Osman KH, Macleod C, et al. The epidemiology of trachoma in Darfur States and Khartoum State, Sudan: results of 32 population-based prevalence surveys. Ophthalmic Epidemiol. 2016;23(6):381–391. https://www.tandfonline.com/doi/full/10.1080/09286586.2016.1243718.
- Yaya G. Lessons learned in the implementation of programmes to eliminate trachoma within conflict zones. Trans R Soc Trop Med Hyg. 2022;116(11):979–980. doi:10.1093/trstmh/trac061.
- Macleod CK, Bailey RL, Dejene M, et al. Estimating the intracluster correlation coefficient for the clinical sign “trachomatous inflammation—follicular” in population-based trachoma prevalence surveys: results from a meta-regression analysis of 261 standardized preintervention surveys carried O. Am J Epidemiol. 2019;1–9. doi:10.1093/aje/kwz196.
- Courtright P, Flueckiger R, Harding-Esch E, Lewallen S, Solomon A. Tropical Data: Training Manual for Trachomatous Trichiasis Population-Based Prevalence Surveys (Version 1). 1st. London: International Coalition for Trachoma Control; 2017.
- Solomon AW, Pavluck AL, Courtright P, et al. The global trachoma mapping project: methodology of a 34-country population-based study. Ophthalmic Epidemiol. 2015;22(3):214–225. doi:10.3109/09286586.2015.1037401.
- World Health Organisation(WHO)/UNICEF. Improved and unimproved water sources and sanitation facilities. WHO/UNICEF Joint Monitoring Programme(JMP) for Water Supply and Sanitation.
- World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals. A Global Strategy on Water, Sanitation and Hygiene to Combat Neglected Tropical Diseases 2021–2030. Geneva: Switzerland; 2021.
- Kalua K, Chisambi A, Chinyanya D, et al. One round of azithromycin MDA adequate to interrupt transmission in districts with prevalence of trachomatous inflammation—follicular of 5.0-9.9%: evidence from Malawi. PLoS Negl Trop Dis. 2018;12(6):1–11.doi:10.1371/journal.pntd.0006543.
- Elshafie BE, Elsanosi MSA, El Amin A, et al. Trachoma prevalence in four localities of Darfur region, Sudan, following one round of antibiotic mass drug administration. Ophthalmic Epidemiol. 2021;:1–9.doi:10.1080/09286586.2021.1953538.
- World Health Organization Strategic and Technical Advisory Group for Neglected Tropical Diseases., Working Group on Monitoring and Evaluation. Design and Validation of a Trachomatous Trichiasis-Only Survey (WHO/HTM/NTD/PCT/2017.08). Geneva, Switzerland: World Health Organization; 2017.
- Amoah B, Fronterre C, Johnson O, et al. Model-based geostatistics enables more precise estimates of neglected tropical-disease prevalence in elimination settings: mapping trachoma prevalence in Ethiopia. Int J Epidemiol. 2022;51(2):468–478. doi:10.1093/ije/dyab227.
- World Health Organization. Validation of Elimination of Trachoma as a Public Health Problem (WHO/HTM/NTD/2016.8). Geneva, Switzerland: World Health Organization; 2016.
- West S, Muñoz B, Lynch M, et al. Impact of face-washing on trachoma in Kongwa, Tanzania. Lancet. 1995;345(8943):155–158.doi:10.1016/s0140-6736(95.
- Bailey R, Downes B, Downes R, Mabey D. Trachoma and water use; a case control study in a Gambian village. Trans R Soc Trop Med Hyg. 1991;85(6):824–828. doi:10.1016/0035-9203(91)90470-J.
- Dodson S, Heggen A, Solomon AW, Sarah V, Woods G, Wohlgemuth L. Behavioural change interventions for sustained trachoma elimination. Bull World Health Organ. 2018;96(10):723–725. doi:10.2471/BLT.18.212514.
- Yemen WASH Cluster, REACH Initiative, ACAPS. Yemen water, sanitation and hygiene secondary desk revie. https://www.impact-repository.org/document/reach/56ce7aaa/REACH_YEM_Report_WASH-Secondary-Desk-Review_May-2020.pdf. Published 2020.
- World Health Organization. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030. Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/neglected_diseases/Revised-Draft-NTD-Roadmap-23Apr2020.pdf?ua=1.
- Boisson S, Wohlgemuth L, Yajima A, et al. Building on a decade of progress in water, sanitation and hygiene to control, eliminate and eradicate neglected tropical diseases. Trans R Soc Trop Med Hyg. 2021;115(2):185–187.doi:10.1093/trstmh/trab001.
- Pavluck A, Chu B, Mann Flueckiger R, Ottesen E, Brooker S. Electronic Data Capture tools for global health programs: evolution of LINKS, an Android-, web-based system. PLoS Negl Trop Dis. 2014;8(4):e2654. doi:10.1371/journal.pntd.0002654.
