ABSTRACT
Children with Disruptive Mood Dysregulation Disorder (DMDD) or Oppositional Defiant Disorder (ODD) are characterized by irritability and social difficulties. However, the mechanisms underlying these disorders could be different. This study explores differences in social cognition and executive function (EF) across DMDD and ODD and the influence of these factors and their interaction on social problems in both groups. Children with DMDD (n = 53, Mage = 9.3) or ODD (n = 39, Mage = 9.6) completed neuropsychological tasks measuring social cognition (Theory of Mind and Face-Emotion Recognition) and EF (cognitive flexibility, inhibition, and working memory). Parents reported social problems. More than one-third of the children with DMDD and almost two-thirds of those with ODD showed clear difficulties with Theory of Mind. Most children with DMDD (51–64%) or ODD (67–83%) showed difficulties with EF. In children with DMDD, worse EF (β = –.36) was associated with more social problems, whereas in children with ODD, better EF (β = .44) was associated with more social problems. In those with ODD, but not in those with DMDD, the interaction between social cognition and EF contributed to the explained variance of social problems (β = –1.97). Based on the observed interaction pattern, enhanced EF may lead to increased social problems among children with ODD who also exhibit social cognition difficulties. This study suggests the existence of distinct neuropsychological mechanisms underlying the social issues observed in children with DMDD versus those with ODD.
Children diagnosed with Disruptive Mood Dysregulation Disorder (DMDD) or Oppositional Defiant Disorder (ODD) often display social difficulties (Freeman et al., Citation2016; Greene et al., Citation2002; Lin et al., Citation2021; W. Copeland et al., Citation2013). The diagnostic criteria for DMDD include irritable mood for at least one year and frequent temper outbursts. ODD requires argumentative or defiant behavior, vindictiveness, or irritable mood for at least six months (APA, Citation2013). Our understanding of the types and causes of these social difficulties within each diagnostic group is complicated because past research on ODD often combined ODD with conduct disorders or did not exclude children with DMDD (since DMDD was not a diagnosis until 2013). The fact that there might be different mechanisms associated with these disorders is reflected in the understanding of DMDD as an affective disorder and ODD as a disruptive behavior disorder in the DSM-5. However, recognizing these disorders as separable entities is still controversial (Lochman et al., Citation2015). Thus, a more careful examination of the neuropsychological correlates and interactions of social difficulties in each of these groups is warranted. This study focuses on two related factors in children’s social functioning: social cognition and executive functions (EF). This will be the first study to examine how the social problems observed in children with DMDD or ODD might differ in their interactional neuropsychological mechanisms.
Social cognition
Social cognition refers to the cognitive systems involved in mediating responses in interpersonal settings and was recently recognized as one of the six core neuropsychological domains important for understanding mental disorders (Insel et al., Citation2010). This highlights the need for clinical investigation of cognitive abilities involved in social functioning to understand mental illness. Two fundamental components of social cognition are the ability to understand and attribute mental states to oneself and others, named Theory of Mind (ToM; Premack & Woodruff, Citation1978), and the ability to distinguish and label different emotional facial expressions adequately, referred to as Face-Emotion Recognition (FER; e.g., Philippot & Feldman, Citation1990). These abilities are crucial in the interpretation and adaptation to other people’s behavior and reactions and are thus critical components of social interaction (for a review on ToM, see (Hughes & Leekam, Citation2004), and for FER, see (Lemerise & Arsenio, Citation2000; Leppänen & Hietanen, Citation2003; Philippot & Feldman, Citation1990)). Generally, previous studies found that children with behavior problems display a broad pattern of deficits and biases in social cognition (for a meta-analytic review, see (Yoon et al., Citation1999)). For example, children with aggressive behavior tend to interpret others’ intentions as hostile in ambiguous social situations (De Castro et al., Citation2002), interpret facial expressions more negatively (Mellentin et al., Citation2015), and allocate attention toward social threats (Miller & Johnston, Citation2019).
A recent study reported that children with DMDD have social cognition difficulties and poor social awareness similar to children with autism spectrum disorders (Sturm et al., Citation2018). Furthermore, another study found that they have difficulties identifying emotional prosody, which is the emotional intonation of speech (Deveney, Brotman, et al., Citation2012). These results lead one to question whether children with DMDD could have general difficulties with understanding the mental states of others (i.e., ToM). Indeed, this could make social interactions challenging because of misinterpretations and violation of social expectations, which could lead to frustration and temper outbursts as observed in children with DMDD. However, to our knowledge, ToM has never been tested in children with DMDD.
There has been an interest in FER related to emotional dysregulation. This originates from attempts to distinguish chronic from episodic irritability, as chronic irritability was previously (mis)understood as a child version of bipolar disorder (Rao, Citation2014) and in which FER difficulties were demonstrated (McClure et al., Citation2005; Rich et al., Citation2006). Although FER has been investigated in DMDD, this line of research provides inconsistent evidence (Guyer et al., Citation2007; Kim et al., Citation2013; Rich et al., Citation2008; Thomas et al., Citation2012, Citation2014; Tseng et al., Citation2016). This may be due to diagnostic criteria similar (but not identical) to DMDD (Brænden et al., Citation2022; Meyers et al., Citation2017).
A recent study comparing children with ODD with healthy controls indicated (although presenting a small effect size) that children with ODD have impaired recognition of anger but not impaired recognition of other emotions (Deters et al., Citation2020). Another study showed that, compared with typically developing children, children with ODD do not have relative impairments in emotion perception, emotion perspective-taking, and in the ability to appreciate mixed emotions (O´Kearny et al., Citation2017). When thinking about the possible causes for anger, children with ODD provided fewer reasons than typically developing children. Thus, although there is mixed evidence on the perception of anger in children with ODD (Deters et al., Citation2020; O´Kearny et al., Citation2017), research otherwise suggests that these children have intact emotional recognition and understanding of the mental states of others (O´Kearny et al., Citation2017).
Executive function
Individual differences in social cognition are closely related to functions underlying flexible goal-directed behavior (Carlson & Moses, Citation2001; Hughes, Citation1998; Russell, Citation1997). EF is an umbrella term for distinct but interacting cognitive functions such as inhibition, cognitive flexibility (CF), and working memory (WM) (Miyake et al., Citation2000). These functions enable the regulation of behavior, thoughts, and emotions adaptively and flexibly in different situations and demands, including in social contexts. ToM and EF are moderately correlated (e.g., Carlson & Moses, Citation2001; Müller et al., Citation2005) and are important for children’s social competence (Capage & Watson, Citation2001).
Research comparing children with DMDD with healthy controls using performance-based behavior tasks suggests that DMDD is characterized by impaired CF and normal motor inhibition abilities, but the results are equivocal (Adleman et al., Citation2011; Deveney, Connolly, et al., Citation2012; Dickstein et al., Citation2007, Citation2010; Uran & Kilic, Citation2015). For example, in two of the three studies indicating that children with DMDD have cognitive inflexibility (Adleman et al., Citation2011; Dickstein et al., Citation2010; Uran & Kilic, Citation2015), the children were not significantly (but only descriptively) worse than healthy controls (Dickstein et al., Citation2010; Uran & Kilic, Citation2015), although the associated effect size (d = .74) could indicate a type II error (Dickstein et al., Citation2010). Furthermore, because social and emotional cues and situations are constantly changing, the ability to adaptably shift between or among mental sets or operations, i.e., CF (Miyake et al., Citation2000), could be especially important in social functioning.
The diagnostic criteria for ODD imply that these children execute behavior in accordance with their will (APA, Citation2013). This raises the question of whether children who meet these diagnostic criteria will exhibit greater ability to plan and execute behavior in a goal-directed manner. The criteria include “often actively […] refuses to comply with requests from authority figures or with rules” and “often deliberately annoys others.” Indeed, although evidence is ambiguous (often because ODD is pooled together with conduct disorder in research), it suggests that children with ODD may not experience difficulties with EF (e.g., Ezpeleta & Granero, Citation2015; Van Goozen et al., Citation2004).
In summary, current evidence indicates that children with DMDD could have ToM difficulties and EF difficulties that compromise their ability to adapt flexibly to changing situations. By contrast, children with ODD may have intact EF and social cognition. These factors may be differently associated with the social difficulties experienced by these children.
Present study
Here, we first explore the everyday social problems that parents report in children with DMDD or ODD in a Norwegian clinical sample. Then, we compare social cognition and EF in children with DMDD with those with ODD based on neuropsychological tasks on FER, ToM, inhibition, CF, and WM. Third, we explore how social cognition (FER and ToM combined) and EF (inhibition, CF, and WM combined) are associated with social problems in each group.
Based on the reviewed literature, we expect both groups to have social problems. As the literature on FER is ambiguous, we made no hypothesis on whether children with DMDD or ODD would have such difficulties. Taking into account the study by Sturm and colleagues (2018), we expect children with DMDD to display ToM difficulties. We further expect that children with DMDD will have difficulties with CF, whereas no hypothesis was made concerning inhibition and WM due to limited knowledge. Furthermore, we hypothesize that the social problems of children with DMDD will be related to ToM problems and worse EF, assuming that difficulties with CF will influence the overall EF of these children. As it is not clear from the reviewed literature if children with ODD have any difficulties with ToM or EF, we do not expect children with ODD to have such difficulties or that their social problems will be related to social ToM or EF.
Methods
Participants
This study includes a treatment-seeking sample of 6–12-year-old children. These children did not receive psychiatric treatment or medication during inclusion and study participation. Participants were recruited from outpatient child psychiatry departments at Oslo University Hospital and Nic Waals Institute between September 2019 and August 2021. Thus, part of the recruitment and participation occurred during the COVID-19 pandemic. This did not change recruitment or consenting procedures. However, it resulted in some neuropsychological test appointments being canceled for a number of reasons, such as complete social isolation or covid-related sick leave. Informed oral and written consent was attained from parents. The Regional Committees for Medical and Health Research Ethics (#2017/135) approved the study which is part of a registered study protocol (NCT05049356). Inclusion criteria included children between 6 and 12 years of age, IQ ≥ 70, and sufficient Norwegian language skills to respond to questionnaires and a semi-structured clinical interview. The recruitment and selection process is detailed in .
Measures
Measures were completed as part of each child’s clinical assessment before starting treatment. In two different sessions (occurring simultaneously or different in time) parents were interviewed and the children completed neuropsychological testing.
Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version (K-SADS-PL-5; Kaufman et al., Citation1997), the 2016 version, was used for the psychiatric diagnoses following the DSM-5 criteria. Of note, the DSM-5 specifies that DMDD takes precedence over ODD. Thirteen clinical psychologists and final-year clinical psychology students administered the Norwegian version of K-SADS-PL-5 to parents. Reliability was established in three ways: First, interviewers were thoroughly trained in the administration of K-SADS-PL-5 before they contributed to the data collection. Second, cases were discussed with other clinicians. Third, 8.3% (18 of the 218 in NCT05049356) of the interviews were scored independently by two different clinicians demonstrating a substantial agreement between the interviewers’ diagnostic evaluations, Cohen’s к = .90 for DMDD and .88 for ODD.
The Achenbach System of Empirically Based Assessment (Achenbach & Rescorla, Citation2001) was used to measure social problems. Parents completed the Child Behavior Check List (CBCL) including a Social Problems scale. Items are rated on a 3-point Likert scale (not true, sometimes true, often true). The CBCL Social Problems scale consists of 11 items: (I) clings to adults or is too dependent, (II) complains of loneliness, (III) doesn’t get along with other kids, (IV) easily jealous, (V) feels others are out to get her/him, (VI) gets hurt a lot, accident-prone, (VII) gets teased a lot, (VIII) not liked by other kids, (IX) poorly coordinated or clumsy, (X) prefers being with younger kids, and (XI) speech problem. The score range is 0 (none) to 22 (high). Psychometric support for the scales is provided in various studies (e.g., Achenbach & Rescorla, Citation2001; Novik, Citation1999; Schmeck et al., Citation2001). Raw scores were used in the statistical analyses and T-scores to examine whether the group’s scores were within the normal or clinical range compared with standardized norm values. T-scores ≥ 65 are indicative of social problems.
In the CBCL, parents also reported the child’s number of close friends (none (0), 1 (1), 2 or more (2)), times per week the child is with friends outside school (fewer than 1 (0), 1 or more (1)), and to which degree (worse (0), average (1), better (2)) the child gets along with other kids compared with others of the same age.
NEPSY Second edition (NEPSY-2; Korkman et al., Citation1998, Citation2007b) is a comprehensive performance-based neuropsychological assessment tool. The NEPSY-2 manual (Korkman et al., Citation2007a) provides evidence of content, construct, concurrent, clinical validity, and internal and test-retest reliability (Brooks et al., Citation2009). Participants completed the two subtests developed for measuring social cognition in 6–12-year-old children: (1) affect recognition and (2) ToM. In affect recognition, also referred to as FER, the child is asked to identify the correct face-emotion of children in pictures. Some pictures are displayed for only five seconds, whereas others have no time limit. In ToM, the child is presented with pictures or stories of different social situations and must decide the characters’ beliefs, thoughts, or intentions in the picture or story. Raw scores were used in the statistical analyses and scaled scores or percentile ranks to examine whether the group’s scores were within the normal or clinical range compared with American standardized norm values. Higher raw scores indicate better performance. Scaled scores have a mean of 10 and a standard deviation of 3; scaled scores < 8 indicate clinical scores. Percentile ranks < 26% indicate clinical scores (Korkman et al., Citation2007b). We also used percentile ranks to categorize ToM scores into groups within or below clinical levels. To be used in the regression models, raw scores were transformed into z scores. Considering the sample size and the need to represent a common social cognition factor capturing emotion perception and the ability to infer the beliefs, feelings, and intentions of others, which is often included in models of social cognition (Adolphs, Citation2010; McDonald, Citation2013), a Social Cognition Composite score was made by adding the z scores of FER and ToM and dividing by two (number of subcomponents).
Participants also completed three NEPSY-2 subtests of EF, that is, CF, inhibition, and WM: (1) Design Fluency (for children between 5 and 12 years), i.e., cognitive flexibility (CF), assessing behavioral productivity and the child’s ability to generate unique designs by connecting five dots, presented in a structured and random way, (2) Inhibition (INH) measuring the ability to inhibit automatic responses (5–16 years) and to switch between response styles (7–16 years), and (3) Word List Interference (7–16 years) assessing verbal WM. Higher raw scores indicate better performance, except for INH completion time. However, the completion time is accounted for in the INH scaled scores used in this study. Scaled scores have a mean of 10 and a standard deviation of 3; and scaled scores<8 indicate clinical scores (Korkman et al., Citation2007b). The design fluency raw score, the inhibition condition scaled score (accounting for the number of faults and time passed), and the world list interference scaled contrast score (accounting for the effect of correct repetitions on recalling) were transformed into z scores. These z scores were added and divided by three (number of subcomponents), creating an EF composite score to be used in the regression models to represent common EF (Miyake et al., Citation2000).
Statistical procedures
Analyses were carried out using IBM SPSS Statistics Version 28.0.0.0 (190) and R version 4.2.0 (Team, Citation2022) including the QuantPsyc package (Fletcher, Citation2022). Alpha level was set to .05. Effect sizes were measured using Cohen’s d with values of .20, .50, and .80, and partial eta squared with values of .01, .06, and .14, interpreted as small, medium, and large effects, respectively (Cohen, Citation1969; Richardson, Citation2011).
Participant characteristics across diagnostic groups were analyzed using the chi-square tests or independent sample t-tests. In addition, the effects of sex and age on social problems, social cognition, and EFs were examined using chi-square tests or Pearson’s correlation analysis.
To examine differences in social problems, social cognition, and EF between diagnostic groups, independent sample t-tests or analysis of covariance were conducted. Pearson’s correlation analyses were performed for DMDD and ODD to explore associations between each group’s predictors and dependent variables. Multiple regression analyses were conducted first in children with DMDD and then in children with ODD to investigate the explained variance of social cognition and EF and their interaction with social problems. Because of COVID-19 lockdown, we expected missing responses, especially on NEPSY-2 subtests. To be used in the regression analyses, data were imputed to compensate for the missing responses (see Supplementary Material I: Multiple Imputation). Ensuring that accurate interpretations could be drawn from the study, the regression analyses were performed using (I) raw (i.e., non-imputed) data, (II) imputed data, and (III) raw data with an EF composite excluding WM (as children < 7 years of age (n = 8) could not complete the WM tasks cf. NEPSY-2 and were thus excluded from regression analyses I and II).
Results
Participant characteristics
Participant characteristics are presented in showing no significant differences between groups on demographic variables except for family income. Fifty-three children were diagnosed with DMDD (Mage = 9.33, SD = 1.91) and 39 with ODD (Mage = 9.61, SD = 1.81). Among those with DMDD, 43 children could have also met the ODD criteria if not following the DSM-5 rule (DMDD takes precedence over ODD). Seventy-seven percent of the children with DMDD and 64% of those with ODD were boys. There were no significant sex differences on any measures. Levene’s test indicated that equal variances could be assumed across diagnostic groups on all measures (p’s > .05). Age correlated significantly with FER (.41, p < .001), ToM (.46, p < .001), and design fluency (.50, p < .001) in the total sample.
Table 1. Participant characteristics.
Social problems
Fifteen (33%) children with DMDD and 14 (38%) with ODD had T-scores ≥ 65 on CBCL Social Problems, with no difference between groups (see ). The distributions of scores are presented in Supplementary Material II. In children with DMDD (n = 31), parents reported that 45% (n = 14) were worse in getting along with other kids, 52% (n = 16) were roughly equal, and 3% (n = 1) were better compared with other children of the same age. In children with ODD (n = 24), parents reported that 38% (n = 9) were worse in getting along with other kids, 54% (n = 13) were roughly equal, and 8% (n = 2) were better compared with other children of the same age. There were no differences in the frequency distribution between children with DMDD and those with ODD, χ2(2, N = 55)=.85, p = .65.
Table 2. Test statistics of the measures across DMDD and ODD.
Social cognition
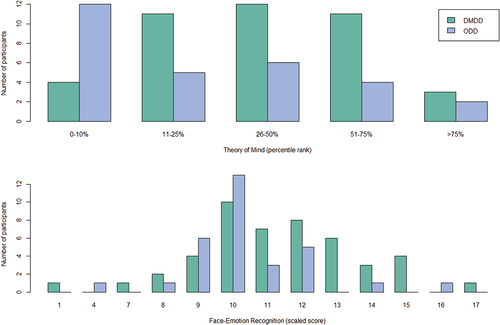
Children with DMDD (n = 47, Scaled Score M = 11.28, SD = 2.62) or ODD (n = 31, Scaled Score M = 10.29, SD = 1.99) scored within a normal level on FER, and there was no significant difference between groups (see ). Two children (4%) with DMDD and one child (3%) with ODD scored below the clinical cutoff score (based on non-imputed data). On ToM, a relatively greater proportion of children with ODD (58%) scored below the clinical cutoff compared with children with DMDD (33%), χ2(1, N = 77) = 4.90, p < .05, although there was no significant difference in mean scores. The distributions of scores on FER and ToM are presented in .
Executive function
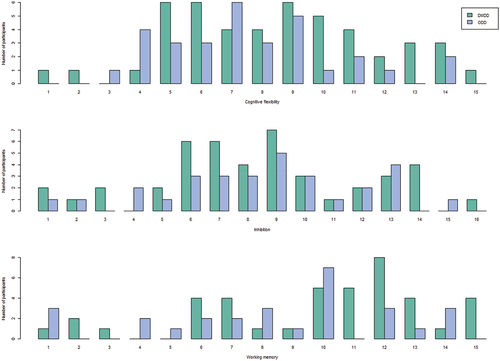
On a group level, children with DMDD or ODD scored below the normed average but above the clinical cutoff on INH and WM (see ). There were no significant differences in mean scores on any EF measure. On CF, children with DMDD scored (on a group level) below the normed average but above the clinical cutoff (Scaled Score M = 8.53, SD = 3.28), whereas those with ODD scored below the clinical cutoff (Scaled Score M = 7.58, SD = 2.85). The proportion of children with DMDD scoring below the clinical cutoff on CF was 53%, and 81% for those with ODD. On INH, 64% of those with DMDD and 67% with ODD scored below the clinical cutoff. Furthermore, 59% of those with DMDD and 81% with ODD scored below the clinical cutoff on WM. The distributions of EF scores are illustrated in .
Regression models
The bivariate relations between variables in DMDD and ODD are presented in . Across groups, CF correlated moderately with FER and ToM (r > .34) and WM correlated moderately with ToM (r > .32). FER and WM correlated moderately in children with DMDD (r > .29), but this correlation was not significant using raw data. INH did not significantly correlate with FER or ToM in either group. In children with DMDD but not in those with ODD, a strong significant correlation was found between FER and ToM (r = .77).
Table 3. Correlations between variables in DMDD and ODD.
The regression models predicting social problems are presented in . In children with DMDD, the EF composite contributed significantly to explaining social problems in the analysis using imputed data (β = –.39, p < .05) and showed a similar tendency when using raw data (β = –.36, p = .0575). In none of the analyses the social cognition composite or the interaction between the EF and social cognition composite influenced social problems significantly. Only when using imputed data (and not raw data), the model significantly contributed to explaining social problems, explaining 19% of the variance in social problems. The regression model is illustrated in . A supplementary analysis indicated that the presented effects are not driven only by the children with DMDD who did not also fulfill the ODD criteria when ignoring the DSM-5 rule (see Supplementary Material III). In children with ODD, the EF composite contributed significantly to explaining social problems using the imputed data (β = .38, p < .05) and the raw data (β = .44, p < .05), with an opposite effect on social problems than in those with DMDD. In the analysis using raw data, but not in the analysis using imputed data, the interaction between the EF composite and the social cognition composite significantly affected social problems (β = –4.40, p < .01). The interaction effect is plotted in . Using raw data, the model significantly explained social problems (p < .01), explaining 48% of the variance. A similar tendency was present when using the imputed data (R2 = .23, p = .055). The regression model is illustrated in .
Figure 4. Regression model in children with DMDD with coefficients.
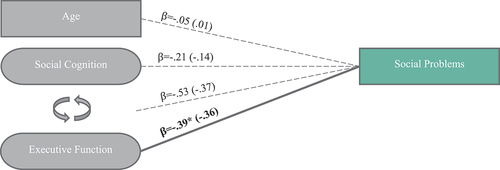
Figure 5. Interaction effect of executive function and social cognition on social problems in children with ODD.
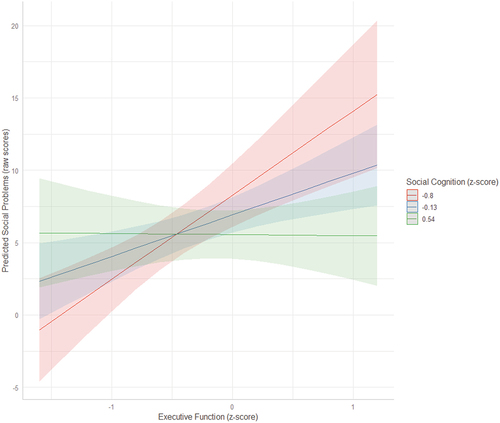
Figure 6. Regression model in children with ODD with coefficients.
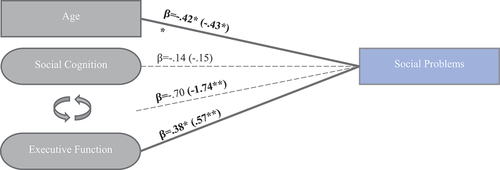
Table 4. Regression analyses predicting CBCL social problems.
Discussion
Although DMDD and ODD are recognized as different disorders (APA, Citation2013), implying that different mechanisms could be associated with these disorders, this is controversial (Lochman et al., Citation2015) and needs clarification. This study compares social cognition and EF in children with DMDD or ODD and how these neuropsychological mechanisms could be linked to their social difficulties (Freeman et al., Citation2016; Greene et al., Citation2002; Lin et al., Citation2021; W. Copeland et al., Citation2013). Determining whether there are different mechanisms is important not only to inform the ongoing diagnostic controversy but also because treatment recommendations could differ based on our understanding of the mechanisms of these disorders. In the following, we discuss the present study’s findings and the possible distinct social-cognitive mechanisms in children with DMDD versus ODD.
Social problems
In line with existing research (Freeman et al., Citation2016; Greene et al., Citation2002; Lin et al., Citation2021; W. Copeland et al., Citation2013), this study found that children with DMDD or ODD have more social impairment than the general population. However, there was a substantial degree of variability in their scores, such that 60–70% did not appear to be socially impaired, that is, not crossing the clinical cutoff. Of note, some researchers have recommended a lower clinical cutoff for the CBCL Social Problems scale (e.g., Leung et al., Citation2006; Schmeck et al., Citation2001) and cross-culturally Norway is characterized as a low-scoring country (Jozefiak et al., Citation2012; Rescorla et al., Citation2007). By lowering the clinical cutoff or applying Norwegian norms, an increased proportion of the children in this study could thus have been categorized as having social problems.
Social cognition
ToM
In our study, more than one-third of the children with DMDD and almost two-thirds of those with ODD showed clear ToM difficulties, crossing the clinical cutoff. This may support and extend previous findings, indicating that children with DMDD, on a group level, have poor social awareness and cognition, as reported by parents (Sturm et al., Citation2018). Contrary to our hypothesis and previous research (O´Kearny et al., Citation2017), this study found that ToM was significantly associated with ODD, suggesting that it may be a mechanism worthy of additional study. For those with ToM difficulties, independent of diagnoses, this might prohibit reflection on the potential harm caused by their behavior and thus (re)learning. It could be that these children rely on premature or underdeveloped assumptions about others’ mental states. By contrast, children with intact abilities to understand the mental states and feelings of others might be able to reflect upon the potential harm inflicted by their behavior or temper outbursts. Combined with an experience of being unable to control or stop one’s temper outbursts, as in those with DMDD, this could lead to a downward spiral, increasing both negative emotions or frustration (i.e., irritability) and negative self-experience or regard. This could then contribute to an understanding of why children with DMDD are at risk of developing depression and anxiety disorders in long term (W. E. Copeland et al., Citation2014). It is worth noting that there was variability in ToM abilities within each diagnosis. Although a relatively higher proportion of children with ODD had severe ToM difficulties, such difficulties were present in both groups. Therefore, they can not be used alone to differentiate DMDD from ODD.
FER
In our study, most children with DMDD or ODD accurately identified facial emotions. Although this contrasts with some studies showing FER difficulties in children with severe mood dysregulation (Guyer et al., Citation2007; Kim et al., Citation2013; Rich et al., Citation2008), our findings align with more recent studies indicating intact face-emotion labeling by task performance in these children (Thomas et al., Citation2012, Citation2014; Tseng et al., Citation2016). Of note, some studies have tested recognition tendencies of specific emotions such as anger, indicating that children with DMDD tend to interpret others’ intentions as threatening, that is, aberrant threat processing (Brotman et al., Citation2010; Hommer et al., Citation2014). One study suggests a similar tendency in those with ODD, namely impaired anger recognition, but not impaired recognition of other emotions (Deters et al., Citation2020). However, our result of intact FER in children with ODD aligns with studies indicating that most children do not have impairments in emotion perception (O´Kearny et al., Citation2017). ODD symptoms are not associated with recognizing negative facial emotions (Acland et al., Citation2021). Acland et al. (Citation2021) disentangled ODD symptoms from overt aggression and found that poor recognition of negative emotion is associated with overt aggression, explained by more difficulties with accurately identifying the type of negative emotion (sad, anger, fear) and by a reduced sensitivity to negative emotions. Our study did not consider specific emotion identification abilities or sensitivity to emotions. Nevertheless, children with ODD or DMDD might not have general problems accurately identifying facial emotions.
An interesting observation is the difference in the degree and significance of the correlation between ToM and FER in each group. Our results suggest a greater coherence between the ability to interpret and understand the mental states and emotions of others and the ability to adequately perceive facial emotions in children with DMDD than in those with ODD. Further conceptualization is needed to understand how ToM difficulties combined with a relatively intact ability to discriminate facial emotions could be connected to oppositionality.
Social cognition did not explain the variance in social problems in DMDD or ODD. Indeed, there is evidence of ToM (and EF, which we discuss below) being related to physical aggression but not relational aggression or peer acceptance (O’Toole et al., Citation2016). One might expect that since social cognition is considered essential for social functioning (Beauchamp & Anderson, Citation2010; Yeates et al., Citation2007), social cognition would be related to social problems in any case. However, this study’s measures of social problems and social cognition might not be sensitive to the specific interpersonal difficulties of children with DMDD (e.g., self-regulation and emotion control in interpersonal contexts). EF, related to self-regulation, could be more important in explaining these children’s social problems than social cognition.
EF
Between 53% and 80% of children in our study showed difficulties with INH, CF, and/or WM, that is, more problems with EF than the general population. Similar to the social cognition tests, there was considerable variability in the test scores, suggesting that many but not all children with DMDD or ODD will show executive dysfunction. The (closer) investigation of EF variability in the present study shed new light on previous work where the clinical cutoffs, but not the degree of variability, were considered (Brænden et al., Citation2023). This means that, based on parent reports (Brænden et al., Citation2023) and task performance, most children with DMDD might have EF difficulties. This is consistent with findings indicating that children with DMDD have cognitive inflexibility (Adleman et al., Citation2011; Dickstein et al., Citation2007) but challenges previous findings of intact INH abilities (on a group level) in children with severe mood dysregulation (Deveney, Connolly, et al., Citation2012). In the present study, we did not take ADHD symptoms into account. In a previous study using the same sample, only those with DMDD+ADHD (and not those with DMDD without ADHD) showed WM difficulties based on parent reports (Brænden et al., Citation2023). Presumably, WM problems in children with DMDD could be attributed to ADHD comorbidity. Given that 81% of the children with ODD displayed WM difficulties, it may be worth investigating how WM skills are associated with ODD versus ADHD in an additional study. As diagnostic comorbidity is common in clinical populations, and due to the great variability in the EF scores within both DMDD and ODD, it is important to consider individual differences in EF.
Our results suggest that in children with DMDD, worse EF is associated with more social problems and is more influential on their social problems than social cognition. As EF influences whether a child manages to reflect on different behavioral responses (Verhoef et al., Citation2022), our findings imply that worse EF could increase social problems by prohibiting children with DMDD from remaining in reflective processing (e.g., reconsidering if their anger is justified). In children with ODD, a reversed tendency was demonstrated; better EF was linked to more social problems. Furthermore, the interaction between EF and social cognition significantly influenced the social problems of children with ODD. The results indicate that when social cognition abilities are high, the effect of EF on social problems is almost negligible, but as the social cognition abilities decrease, the effect of EF on social problems becomes more pronounced. Thus, the social problems of those with ODD only seem relatively more goal-directed when they also have clear difficulties with understanding the mental states and emotions of others. Whether one recognizes the interpersonal behavior of children with ODD as “willful” or intentional (APA, Citation2013; El Ouardani, Citation2016) must thus be considered in the light that most children with ODD (in our sample) show difficulties in EF and ToM compared with the general population.
In those with DMDD, we did not find any evidence of an interaction effect. Of note, with the present sample size, we could not examine the associations between EF, social cognition, and social difficulties at a subcomponent level. Furthermore, as we did not use empirically derived composite scores (e.g., from factor analysis), we cannot exclude the possibility of a common “performance” factor influencing our results (e.g., an overall performance skill captured by the EF composite, suppressing a possible social cognition effect). This might also have limited our ability to disentangle the influence of emotional-based EF (i.e., the perception of emotions and understanding of others’ emotions) versus cognitive (nonemotional) EF on social problems. Future studies should allow for investigations at the subcomponent level using empirically derived composites and improved measures of interpersonal problems.
As apparent from the present and previous studies (Freeman et al., Citation2016; W. Copeland et al., Citation2013), many children with DMDD also fulfill the diagnostic criteria for ODD. Thus, how can one understand the different neuropsychological mechanisms across the groups? One possibility is that DMDD and ODD differ in the intensity and duration of emotions. Presumably, after the inclusion of DMDD in the DSM-5, children with the highest levels of irritability and anger for the longest period are diagnosed with DMDD and not ODD. To be diagnosed with ODD, a child needs to exhibit argumentative or defiant behavior, or vindictiveness, and not necessarily irritable mood. Compared with those with DMDD, children with ODD might therefore be relatively less irritable and angry. The social difficulties of those with DMDD could thus be more strongly linked to high emotional arousal. By contrast, the social problems of children with ODD could be better characterized as proactive or goal-directed. This explanation would fit the present results and could be understood in line with the DSM-5’s categorization of DMDD as an affective disorder and the diagnostic criteria of ODD focused on argumentative or defiant behavior or vindictiveness (APA, Citation2013). An opportunity for future studies is to test how (irritable) mood or emotional intensity interacts with EF and influences social problems in children with DMDD versus ODD. This could help refine our understanding of these disorders and may help inform the development of diagnostic criteria.
Strengths and limitations
A strength of our study is that it links neuropsychological function as measured by behavioral tasks to reports of everyday social problems. We also tested differences across groups with similar symptom expressions but with assumed different underlying or inherent phenomena as defined in the DSM-5, i.e., emotional dysregulation versus oppositionality or intentionality. However, our study has several limitations. First, in real-life situations, social cognition and EF may interact in a manner that is not detectable by separating these variables in different contexts, i.e., in everyday situations versus laboratory settings, and by different informants, i.e., the parent versus the child. Future studies should link these variables to context and measure interactional processes between them. Second, due to the correlational nature of our study, we cannot assume a causative relationship between the variables. This means it is yet to be determined if treatments targeting EF or ToM would have an effect. Third, although we do not assume that each disorder is a completely discrete entity (APA, Citation2013), we explored differences between groups. Our results indicate individual differences and variability in social cognition and EF abilities within each diagnosis. Fourth, our sample sizes are relatively small (e.g., prohibiting the use of subcomponent-level scores in the regression analyses), and fifth, consequences of the COVID-19 pandemic (e.g., social restrictions, contagion, and disease in the family) may have influenced the social problems reported in our study. Finally, the NEPSY-2 reference data used for the clinical cutoffs may be nonrepresentative of our sample. As there is a lack of Norwegian norms for NEPSY-2, future studies should include a healthy control group. Given the limitations of this study, future studies should use larger samples (including nonclinical cases) and improved measures (including non-categorical/nondiagnostic measures) to further understand the different kinds of relationships between social-neurocognitive mechanisms and social difficulties in children struggling with mood dysregulation or oppositional or defiant behavior.
Conclusion
Our study indicates that the neuropsychological mechanisms of DMDD and ODD could be different. Children with ODD may struggle with understanding the mental states or emotions of others, which when combined with better EF skills may result in more social problems. By contrast, in children with DMDD, worse EF could result directly in more social problems, regardless of their ability to understand the mental states or emotions of others. Although more children with ODD showed ToM difficulties, few differences in the social-cognitive correlates of DMDD versus ODD were found when not considering the effect of these mechanisms on social problems. This highlights the importance of considering the interactive processes between social-cognitive functions and daily-life functioning for understanding mental illness. Although our findings need to be replicated, our study suggests different neuropsychological mechanisms related to the social problems of children struggling with DMDD versus ODD, which may require different treatment interventions.
CNY-OA_22-148-File003.docx
Download MS Word (37.3 KB)Acknowledgments
We are very grateful to the children and their parents participating in this study, as well as our colleagues at the Child and Adolescent Mental Health Clinics. We would also like to thank the reviewers for their constructive feedback and valuable suggestions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed at https://doi.org/10.1080/09297049.2023.2205632.
Additional information
Funding
References
- Achenbach, T. M. and Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6-18, teacher’s report form, youth self-report: An integrated system of multi-informant assessment. University of Vermont, research center for children youth & families.
- Acland, E. L., Jambon, M., & Malti, T. (2021). Children’s emotion recognition and aggression: A multi‐cohort longitudinal study. Aggressive Behavior, 47(6), 646–658. https://doi.org/10.1002/ab.21989
- Adleman, N. E., Kayser, R., Dickstein, D., Blair, R. J. R., Pine, D., & Leibenluft, E. (2011). Neural correlates of reversal learning in severe mood dysregulation and pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50(11), 1173–1185.e2. https://doi.org/10.1016/j.jaac.2011.07.011
- Adolphs, R. (2010). Conceptual challenges and directions for social neuroscience. Neuron, 65(6), 752–767. https://doi.org/10.1016/j.neuron.2010.03.006
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Beauchamp, M. H., & Anderson, V. (2010). SOCIAL: An integrative framework for the development of social skills. Psychological Bulletin, 136(1), 39–64. https://doi.org/10.1037/a0017768
- Brænden, A., Coldevin M, Zeiner P, Stubberud J, & Melinder A. (2023). Executive function in children with disruptive mood dysregulation disorder compared to attention-deficit/hyperactivity disorder and oppositional defiant disorder, and in children with different irritability levels. European Child & Adolescent Psychiatry.
- Brænden, A., Zeiner, P., Coldevin, M., Stubberud, J., & Melinder, A. (2022). Underlying mechanisms of disruptive mood dysregulation disorder in children: A systematic review by means of research domain criteria. Journal of Child Psychology and Psychiatry Advances, 2(1). https://doi.org/10.1002/jcv2.12060
- Brooks, B. L., Sherman, E. M. S., & Strauss, E. (2009). NEPSY-II: A developmental neuropsychological assessment, second edition. Child Neuropsychology, 16(1), 80–101. https://doi.org/10.1080/09297040903146966
- Brotman, M. A., Rich, B. A., Guyer, A. E., Lunsford, J. R., Horsey, S. E., Reising, M. M., Thomas, L. A., Fromm, S. J., Towbin, K., Pine, D. S., & Leibenluft, E. (2010). Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder. The American Journal of Psychiatry, 167(1), 61–69. https://doi.org/10.1176/appi.ajp.2009.09010043
- Capage, L., & Watson, A. C. (2001). Individual differences in theory of mind, aggressive behavior, and social skills in young children. Early Education and Development, 12(4), 613–628. https://doi.org/10.1207/s15566935eed1204_7
- Carlson, S., & Moses, L. (2001). Individual differences in inhibitory control and children’s theory of mind. Child Development, 72(4), 1032–1053. https://doi.org/10.1111/1467-8624.00333
- Cohen, J. (1969). Statistical power analysis for the behavioural sciences. Academic Press.
- Copeland, W., Angold, A., Costello, E. J., & Egger, H. (2013). Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. The American Journal of Psychiatry, 170(2), 173–179. https://doi.org/10.1176/appi.ajp.2012.12010132
- Copeland, W. E., Shanahan, L., Egger, H., Angold, A., & Costello, E. J. (2014). Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. The American Journal of Psychiatry, 171(6), 668–674. https://doi.org/10.1176/appi.ajp.2014.13091213
- De Castro, B., Veerman, J. W., Koops, W., Bosch, J. D., & Monshouwer, H. J. (2002). Attribution of intent and aggressive behavior: A meta-analysis. Child Development, 73(3), 916–934. https://doi.org/10.1111/1467-8624.00447
- Deters, R. K., Naaijen, J., Rosa, M., Aggensteiner, P. M., Banaschewski, T., Saam, M. C., Schulze, U. M. E., Sethi, A., Craig, M. C., Sagar-Ouriaghli, I., Santosh, P., Castro-Fornieles, J., Penzol, M. J., Arango, C., Werhahn, J. E., Brandeis, D., Franke, B., Glennon, J., Buitelaar, J. K. … Dietrich, A. (2020). Executive functioning and emotion recognition in youth with oppositional defiant disorder and/or conduct disorder. The World Journal of Biological Psychiatry, 21(7), 539–551. https://doi.org/10.1080/15622975.2020.1747114
- Deveney, C. M., Brotman, M. A., Decker, A. M., Pine, D. S., & Leibenluft, E. (2012). Affective prosody labeling in youths with bipolar disorder or severe mood dysregulation. Journal of Child Psychology and Psychiatry, 53(3), 262–270. https://doi.org/10.1111/j.1469-7610.2011.02482.x
- Deveney, C. M., Connolly, M. E., Jenkins, S. E., Kim, P., Fromm, S. J., Pine, D. S., & Leibenluft, E. (2012). Neural recruitment during failed motor inhibition differentiates youths with bipolar disorder and severe mood dysregulation. Biological Psychology, 89(1), 148–155. https://doi.org/10.1016/j.biopsycho.2011.10.003
- Dickstein, D. P., Finger, E. C., Brotman, M. A., Rich, B. A., Pine, D. S., Blair, J. R., & Leibenluft, E. (2010). Impaired probabilistic reversal learning in youths with mood and anxiety disorders. Psychological Medicine, 40(7), 1089–1100. https://doi.org/10.1017/S0033291709991462
- Dickstein, D. P., Nelson, E. E., McClure, E. B., Grimley, M. E., Knopf, L., Brotman, M. A., Rich, B. A., Pine, D. S., Leibenluft, E. (2007). Cognitive flexibility in phenotypes of pediatric bipolar disorder. The Journal of the American Academy of Child & Adolescent Psychiatry, 46(3), 341–355. https://doi.org/10.1097/chi.0b013e31802d0b3d
- El Ouardani, C. N. (2016). Innocent or intentional?: Interpreting oppositional defiant disorder in a preschool mental health clinic. Culture, Medicine and Psychiatry, 41, 94–110. https://doi.org/10.1007/s11013-016-9506-7
- Ezpeleta, L., & Granero, R. (2015). Executive functions in preschoolers with ADHD, ODD, and comorbid ADHD-ODD: Evidence from ecological and performance-based measures. Journal of Neuropsychology, 9(2), 258–270. https://doi.org/10.1111/jnp.12049
- Fletcher, T. D. (2022). _quantpsyc: Quantitative psychology tools_. R Package Version 1.6.
- Freeman, A. J., Youngstrom, E. A., Youngstrom, J. K., & Findling, R. L. (2016). Disruptive mood dysregulation disorder in a community mental health clinic: Prevalence, comorbidity and correlates. Journal of Child and Adolescent Psychopharmacology, 26(2), 123–130. https://doi.org/10.1089/cap.2015.0061
- Greene, R. W., Biederman, J., Zerwas, S., Monuteaux, M. C., Goring, J. C., & Faraone, S. V. (2002). Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. The American Journal of Psychiatry, 159(7), 1214–1224. https://doi.org/10.1176/appi.ajp.159.7.1214
- Guyer, A. E., McClure, E. B., Adler, A. D., Brotman, M. A., Rich, B. A., Kimes, A. S., Pine, D. S., Ernst, M., & Leibenluft, E. (2007). Specificity of facial expression labeling deficits in childhood psychopathology. Journal of Child Psychology and Psychiatry, 48(9), 863–871. https://doi.org/10.1111/j.1469-7610.2007.01758.x
- Hommer, R. E., Meyer, A., Stoddard, J., Connolly, M. E., Mogg, K., Bradley, B. P., Pine, D. S., Leibenluft, E., & Brotman, M. A. (2014). Attention bias to threat faces in severe mood dysregulation. Depression and Anxiety, 31(7), 559–565. https://doi.org/10.1002/da.22145
- Hughes, C. (1998). Finding your marbles: Does preschoolers’ strategic behaviour predict later understanding of mind? Developmental Psychology, 34(6), 1326–1339. https://doi.org/10.1037/0012-1649.34.6.1326
- Hughes, C., & Leekam, S. (2004). What are the links between theory of mind and social relations? Review, reflections and new directions for studies of typical and atypical development. Social Development, 13(4), 590–619. https://doi.org/10.1111/j.1467-9507.2004.00285.x
- Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., Sanislow, C., & Wang, P. (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. The American Journal of Psychiatry, 167(7), 167. https://doi.org/10.1176/appi.ajp.2010.09091379
- Jozefiak, T., Larsson, B., Wichstrøm, L., & Rimehaug, T. (2012). Competence and emotional/behavioural problems in 7–16-year-old Norwegian school children as reported by parents. Nordic Journal of Psychiatry, 66(5), 311–319. https://doi.org/10.3109/08039488.2011.638934
- Kaufman, J., Birmaher, B., Brent, D., RAO, U., Flynn, C., Moreci, P., Williamson, D., & Ryan, N. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. https://doi.org/10.1097/00004583-199707000-00021
- Kim, P., Arizpe, J., Rosen, B., Razdan, V., Haring, C., Jenkins, S., Deveney, C., Brotman, M., Blair, J., Pine, D., Baker, C., & Leibenluft, E. (2013). Impaired fixation to eyes during facial emotion labelling in children with bipolar disorder or severe mood dysregulation. Journal of Psychiatry & Neuroscience, 38(6), 406–416. https://doi.org/10.1503/jpn.120232
- Korkman, M., Kirk, U., & Kemp, S. (1998). NESPY: A developmental neuropsychological assessment. The Psychological Corporation.
- Korkman, M., Kirk, U., & Kemp, S. (2007a). NEPSY-II manual norsk versjon. Harcourt Assessment, PsychCorp.
- Korkman, M., Kirk, U., & Kemp, S. (2007b). NEPSY-II second edition clinical and interpretive manual. Pearson.
- Lemerise, E. A., & Arsenio, W. F. (2000). An integrated model of emotion processes and cognition in social information processing. Child Development, 71(1), 107–118. https://doi.org/10.1111/1467-8624.00124
- Leppänen, J. M., & Hietanen, J. K. (2003). Emotion recognition and social adjustment in school–aged girls and boys. Scandinavian Journal of Psychology, 42(5), 429–435. https://doi.org/10.1111/1467-9450.00255
- Leung, P., Kwong, S. L., Tang, C. P., Ho, T. P., Hung, S. F., Lee, C. C., Hong, S. L., Chiu, C. M., & Liu, W. S. (2006). Test–retest reliability and criterion validity of the Chinese version of CBCL, TRF, and YSR. Journal of Child Psychology and Psychiatry, 47(9), 970–973. https://doi.org/10.1111/j.1469-7610.2005.01570.x
- Lin, Y., Tseng, W., & Gau, S. S. (2021). Psychiatric comorbidity and social adjustment difficulties in children with disruptive mood dysregulation disorder: A national epidemiological study. Journal of Affective Disorders, 281(15), 485–492. https://doi.org/10.1016/j.jad.2020.12.039
- Lochman, J. E., Evans SC, Burke JD, Roberts MC, Fite PJ, Reed GM, De la Peña FR, Matthys W, Ezpeleta L, Siddiqui S, & Garralda ME. (2015). An empirically based alternative to DSM-5’s disruptive mood dysregulation disorder for ICD-11. World Psychiatry, 14(1), 30. https://doi.org/10.1002/wps.20176
- McClure, E. B., Treland, J. E., Snow, J., Schmajuk, M., Dickstein, D. P., Towbin, K. E., Charney, D. S., Pine, D. S., & Leibenluft, E. (2005). Deficits in social cognition and response flexibility in pediatric bipolar disorder. The American Journal of Psychiatry, 162(9), 1644–1651. https://doi.org/10.1176/appi.ajp.162.9.1644
- McDonald, S. (2013). Impairments in social cognition following severe traumatic brain injury. Journal of the International Neuropsychological Society, 19, 3. https://doi.org/10.1017/S1355617712001506
- Mellentin, A. I., Dervisevic, A., Stenager, E., Pilegaard, M., & Kirk, U. (2015). Seeing enemies? A systematic review of anger bias in the perception of facial expressions among anger-prone and aggressive populations. Aggression and Violent Behavior, 25, 373–383. https://doi.org/10.1016/j.avb.2015.09.001
- Meyers, E., DeSerisy, M., & Roy, A. K. (2017). Disruptive mood dysregulation disorder (DMDD): An RDoC. Journal of Affective Disorders, 216, 117–122. https://doi.org/10.1016/j.jad.2016.08.007
- Miller, N. V., & Johnston, C. (2019). Social threat attentional bias in childhood: Relations to aggression and hostile intent attributions. Aggressive Behavior, 45(3), 245–254. https://doi.org/10.1002/ab.21813
- Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex “Frontal lobe” tasks: A latent variable analysis. Cognitive Psychology, 41(1), 49–100. https://doi.org/10.1006/cogp.1999.0734
- Müller, U., Zelazo, P. D., & Imrisek, S. (2005). Executive function and children’s understanding of false belief: How specific is the relation? Cognitive Development, 20(2), 173–189. https://doi.org/10.1016/j.cogdev.2004.12.004
- Novik, T. S. (1999). Validity of the child behaviour checklist in a Norwegian sample. European Child & Adolescent Psychiatry, 8(4), 247–254. https://doi.org/10.1007/s007870050098
- O´Kearny, R., Salmon K, Liwag M, Fortune CA, & Dawel A. (2017). Emotional abilities in children with oppositional defiant disorder (ODD): Impairments in perspective-taking and understanding mixed emotions are associated with high callous–unemotional traits. Child Psychiatry & Human Development, 48, 346–357. https://doi.org/10.1007/s10578-016-0645-4
- O’Toole, S. E., Monks, C. P., & Tsermentseli, S. (2016). Executive function and theory of mind as predictors of aggressive and prosocial behavior and peer acceptance in early childhood. Social Development, 26(4), 907–920. https://doi.org/10.1111/sode.12231
- Philippot, P., & Feldman, R. S. (1990). Age and social competence in preschoolers’ decoding of facial expression. British Journal of Social Psychology, 29(1), 43–54. https://doi.org/10.1111/j.2044-8309.1990.tb00885.x
- Premack, D., & Woodruff, G. (1978). Does the chimpanzee have a theory of mind? The Behavioral and Brain Sciences, 1(4), 515–526. https://doi.org/10.1017/S0140525X00076512
- Rao, U. (2014). DSM-5: Disruptive mood dysregulation disorder. Asian Journal of Psychiatry, 11, 119–123. https://doi.org/10.1016/j.ajp.2014.03.002
- Rescorla, L., Achenbach, T., Ivanova, M. Y., Dumenci, L., Almqvist, F., Bilenberg, N., Bird, H., Chen, W., Dobrean, A., Döpfner, M., Erol, N., Fombonne, E., Fonseca, A., Frigerio, A., Grietens, H., Hannesdottir, H., Kanbayashi, Y., Lambert, M., Larsson, B. O. … Verhulst, F. (2007). Behavioral and emotional problems reported by parents of children ages 6 to 16 in 31 societies. Journal of Emotional and Behavioral Disorders, 15(3), 130–142. https://doi.org/10.1177/10634266070150030101
- Richardson, J. T. E. (2011). Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review, 6(2), 135–147. https://doi.org/10.1016/j.edurev.2010.12.001
- Rich, B. A., Grimley, M. E., Schmajuk, M., Blair, K. S., Blair, R. J. R., & Leibenluft, E. (2008). Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Development and Psychopathology, 20(2), 529–546. https://doi.org/10.1017/S0954579408000266
- Rich, B. A., Vinton, D. T., Roberson-Nay, R., Hommer, R. E., Berghorst, L. H., McClure, E. B., Fromm, S. J., Pine, D. S., & Leibenluft, E. (2006). Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. Proceedings of the National Academy of Sciences, 103(23), 8900–8905. https://doi.org/10.1073/pnas.0603246103
- Russell, J. (1997). How executive disorders can bring about an inadequate ‘theory of mind’. In J. Russell (Ed.), In Autism as an executive disorder (pp. 256–304). Oxford University Press.
- Schmeck, K., Poustka, F., Döpfner, M., Plück, J., Berner, W., Lehmkuhl, G., Fegert, J. M., Lenz, K., Huss, M., & Lehmkuhl, U. (2001). Discriminant validity of the child behaviour checklist CBCL-4/18 in German samples. European Child & Adolescent Psychiatry, 10(4), 240–247. https://doi.org/10.1007/s007870170013
- Sturm, A., Rozenman, M., Chang, S., McGough, J. J., McCracken, J. T., & Piacentini, J. C. (2018). Are the components of social reciprocity transdiagnostic across pediatric neurodevelopmental disorders? Evidence for common and disorder-specific social impairments. Psychiatry Research, 264, 119–123. https://doi.org/10.1016/j.psychres.2018.03.063
- Team, R. C. (2022). R: a language and environment for statistical computing. R foundation for statistical computing.
- Thomas, L. A., Brotman, M. A., Bones, B. L., Chen, G., Rosen, B. H., Pine, D. S., & Leibenluft, E. (2014). Neural circuitry of masked emotional face processing in youth with bipolar disorder, severe mood dysregulation, and healthy volunteers. Developmental Cognitive Neuroscience, 8, 110–120. https://doi.org/10.1016/j.dcn.2013.09.007
- Thomas, L. A., Brotman, M. A., Muhrer, E. J., Rosen, B. H., Bones, B. L., Reynolds, R. C., Deveney, C. M., Pine, D. S., & Leibenluft, E. (2012). Parametric modulation of neural activity by emotion in youth with bipolar disorder, youth with severe mood dysregulation, and healthy volunteers. Archives of General Psychiatry, 69(12), 1257–1266. https://doi.org/10.1001/archgenpsychiatry.2012.913
- Tseng, W. -L., Thomas, L. A., Harkins, E., Pine, D. S., Leibenluft, E., & Brotman, M. A. (2016). Neural correlates of masked and unmasked face. Social Cognitive and Affective Neuroscience, 11(1), 78–88. https://doi.org/10.1093/scan/nsv087
- Uran, P., & Kilic, B. G. (2015). Comparison of neuropsychological performances and behavioral patterns of children with attention deficit hyperactivity disorder and severe mood dysregulation. European Child & Adolescent Psychiatry, 24(1), 21–30. https://doi.org/10.1007/s00787-014-0529-8
- Van Goozen, S. H. M., Cohen-Kettenis, P. T., Snoek, H., Matthys, W., Swaab-Barneveld, H., & van Engeland, H. (2004). Executive functioning in children: A comparison of hospitalised ODD and ODD/ADHD children and normal controls. Journal of Child Psychology and Psychiatry, 45(2), 284–292. https://doi.org/10.1111/j.1469-7610.2004.00220.x
- Verhoef, R. E. J., van Dijk, A., & de Castro, B. O. (2022). A dual-mode social-information-processing model to explain individual differences in children’s aggressive behavior. Clinical Psychological Science, 10(1), 41–57. https://doi.org/10.1177/21677026211016396
- Yeates, K. O., Bigler, E. D., Dennis, M., Gerhardt, C. A., Rubin, K. H., Stancin, T., Taylor, H. G., & Vannatta, K. (2007). Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin, 133(3), 535–556. https://doi.org/10.1037/0033-2909.133.3.535
- Yoon, J., Hughes, J., Gaur, A., & Thompson, B. (1999). Social cognition in aggressive children: A metaanalytic review. Cognitive and Behavioral Practice, 6(4), 320–331. https://doi.org/10.1016/S1077-7229(99)80051-0