ABSTRACT
That pathology and normality exist on a complex spectrum of bodily manifestation is an enduring problem at the heart of the philosophy, anthropology and history of medicine. As the primary locus for the reproduction of medicine, medical schools are important sites for cultivating knowledge of what is normal and what is not. Here students come to engage with the slippery concepts of normality and pathology in collaboration with a wide range of educational technologies – the cadavers, plastic models, illustrations and diagnostic tools which corral student knowledge of the body in both health and disease. These technologies are not universally employed across medical faculties, and variations in their use contributes to various constructions of pathology and normality. Ethnographic observation and historical research in medical faculties in Hungary, the Netherlands and Ghana, shows that educational practices are shaped by the epistemic traditions which manifest in the material environment of the medical school, and that these different sociomaterial settings contribute to inconsistent notions of normalcy. Although educational technologies often tend towards fixity in their representations of the body in health and disease, medical school practice in the north of Ghana resists the imposition of the often alien standards typically found in teaching materials imported from Europe or North America. By teaching around and beyond these materials, Ghanaian educators also challenge their assuredness and the intellectual history of contemporary medicine.
Introduction
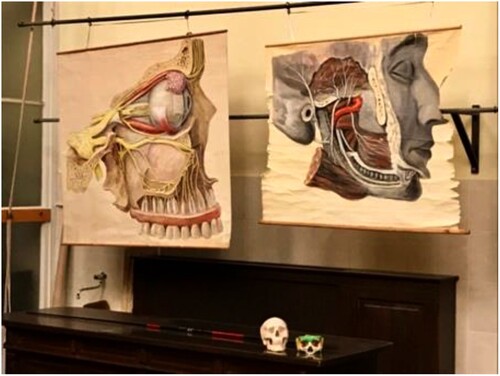
Alongside its windmills and canals, the picturesque Dutch city of Leiden is home to both the oldest medical school in the Netherlands and, in the Rijksmuseum Boerhaave, one of the most celebrated medical museums in Europe. In its vast, off-site storerooms, if you are lucky enough to have a guide, you can find an early simulator used in the study of ophthalmology. This particular ophthalmological ‘phantom’ is from the late nineteenth century and consists of a hollow, artificial eye mounted on a metal frame (). On one side of the eye is a glass lens and, on the other, a removable backing which can hold one of a dozen hand-painted funduses, depicting a range of normal presentations, as well as various pathologies ().Footnote1 By the late nineteenth century, and partly due to the development of the ophthalmoscope, physicians had come to realise ‘that many serious general diseases may first be detected by changes taking place in the fundus’ (Hartridge, Citation1907, p. vii). There was, however, a problem:
wthe acquirement of even a moderate degree of knowledge respecting diseases of the eye – especially those requiring the use of the ophthalmoscope – necessitates considerable study and frequent chances for observation. The everyday routine of [general] practice affords neither opportunities for the one nor time for the other. (Wood, Citation1891, p. 1)
Figure 1. An ophthalmological phantom, c. 1925 (Collin et Cie, Citation1925, p. 45).
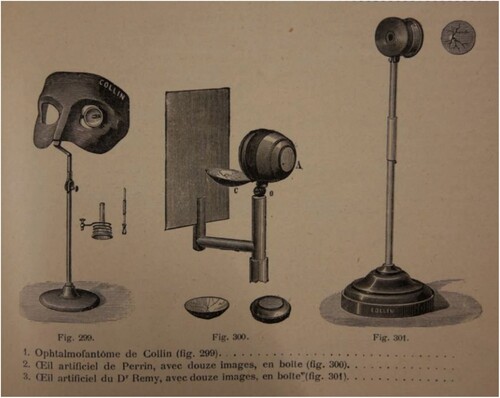
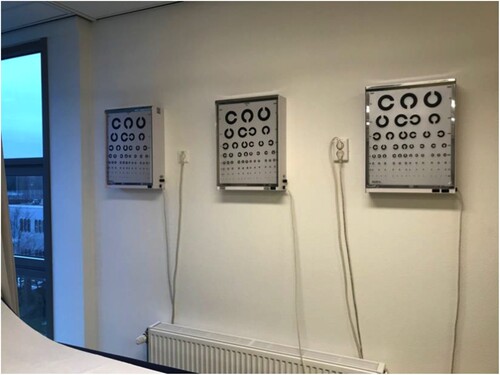
Figure 2. A painted textbook comparison of the fundus as seen through an ophthalmoscope, patient with a fair complexion (top) and albinism (bottom), c. 1907 (Hartridge, Citation1907).
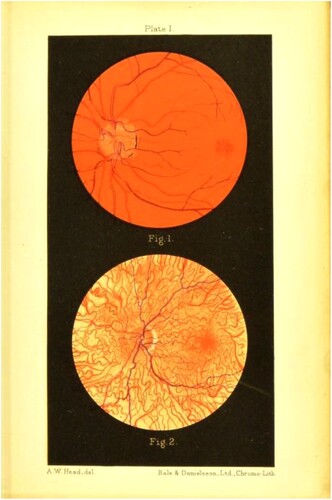
The development of the ophthalmological phantom provided something of a solution, offering a means to practice eye examinations, as well a material reference for what was then considered normal, and what was not. In other words, the phantom simultaneously provided a means to practice seeing and a guide to what should be seen. Advances in diagnostic and clinical technologies – such as the ophthalmoscope – have long been held responsible for the progressive pathologisation of the body within biomedical frameworks, and for the broader construction of disease (Rosenberg, Citation1989; Latour, Citation2000). In this article, however, we are concerned with an altogether less visible network of technologies and sociomaterial practices which, like the ophthalmological phantom, contribute to the reproduction of particular understandings of disease.
As the primary locus for the teaching and learning of medicine, medical schools are an important site for the reproduction of medical practices and epistemologies. Learning the physiological bounds and conceptual vagaries of what is normal and what is not – by viewing, touching, listening to, and working with educational materials – is central to the medical school experience. Despite the necessity of a host of technologies, there has been no comparative analysis of the various material cultures of medical education. Nor has there been any concerted analysis of the material manifestations of normality and pathology within teaching materials, in objects like the eye model in the Boerhaave, or in cadavers, simulations, medical photographs and film. These are objects which we refer to as educational technologies. These technologies are made and used in place, as part of individual constellations of material influences over medical knowledge, and as part of an embodied, practical choreography of learning. In pusuit of such comparision, the three places which we consider here are Semmelweis University in Budapest, Hungary; Maastricht University in Maastricht, in the south of the Netherlands; and the University for Development Studies (UDS) in Tamale, in the north of Ghana. As we will see, through ethnographic vignettes and their historical implosion, each of these schools is materially distinct, products of their unique histories. Building out of this observation, this article asks how do these material distinctions contribute to variations in the construction of pathology and normality in each of our three schools?
Normality, pathology, and the material history of medical education
In the 1940s, the French philosopher of science, Georges Canguillem (Citation2007, Citation2008), posed an enduring question: when we think about the body, where does normality end and pathology begin? The persistence of this problem derives from a fundamental tension in the conceptualisation of normality (Hacking, Citation1990, p. 160–169; Bowker and Star, Citation2000; Daston and Galison, Citation2010; Cryle and Stephens, Citation2017). This, as Ian Hacking later explained, is that ‘the normal stands indifferently for what is typical, the unenthusiastic objective average, but it also stands for what has been, good health, and for what shall be, our chosen destiny’ (Hacking, Citation1990, p. 169). Reproducing such an ephemeral concept has proved extremely difficult within a scientific framework unsuited to ephemerality. As a result, the materials which are used in medical education tend towards assuredness and fixity in their representations of the body in both health and disease. However, insights from STS and medical anthropology suggest that any such material reproductions of either normality or pathology are bound to be inadequate, because the body does not exist as a single entity but as something which is enacted in many ways, and in various spaces and times, through ‘practices which make bodies visible, audible, tangible and knowable’ (Mol, Citation2002, p. 33). Drawing from these contradictions, the article investigates the role of educational technologies in the reproduction of medical epistimiologies and practices.
Closer attention to the matter of medical education – be it textbooks, models, blackboard drawings or digital simulations – is necessary for understanding the cultivation and disciplining of medical knowledge, as well as the sensory attention and practical skills necessary for diagnosis and care. Since the 1960s, there has been a rich stream of anthropological and sociological research into the practices and settings of medical education (e.g. Becker et al. Citation1961; Fox Citation1989; Cassell, Citation1991, Citation1998; Hirschauer, Citation1991; Good and DelVecchio Good, Citation1993; Atkinson and Pugsley Citation2005; Pope Citation2005; Holmes et al., Citation2011). More recent ethnographies have focussed on surgical educators (Prentice, Citation2013), patient simulations (Taylor, Citation2014), obstetric simulators (Johnson, Citation2005, Citation2008), stethoscopes (Rice, Citation2013) and gynaecological teaching associates (Underman, Citation2020). These studies have addressed the sociomaterial conditions of learning in medicine more directly (Fenwick, Citation2014), highlighting the role of technologies in the formation of medical knowledge. Although often addressing issues of pathology in their analysis, these studies have not focused explicitly on the material construction of pathology and normality. They also tend to draw from lone-ethnographer studies, a tradition in which a single anthropologist navigates the terrain of one or more medical schools, often in North America. We also differ in this regard, by drawing insight from across a diversity of spaces – Central and Western Europe, and West Africa – while also considering the histories which contributes to these different sociomaterial contexts.
Despite their importance within the history and ongoing practice of medicine, educational technologies have been largely overlooked as drivers of the universalist assumptions which underpin biomedical discourses and their global hegemony (Lock and Nguyen, Citation2010). Building from STS approaches to the study of technology, we suggest that such technologies must be seen as agential actors in the history of medicine and that they are, by their nature, evangelists for specific epistemologies (Haraway, Citation1991; Barad, Citation2007). Unlike more ‘fluid’ technologies (de Laet and Mol, Citation2000), which change according to context and the agency of users, educational tools purport to reproduce ideas and standards and have more in common with Bruno Latour’s (Citation1990) conceptualisation of ‘immutable mobiles.’ As with printed text – Latour’s initial example and the foundational technology of modern education – educational technologies, by and large, proffer ‘translation without corruption’ (Latour, Citation1990, p. 7). In this respect, and as with clinical or research technologies in medicine, such as X-Rays or MRIs, educational technologies inculcate specific modes of seeing the body (see Burri and Dumit, Citation2008). Such material variations contribute, in turn, to a degree of ontological and epistemic instability within contemporary medicine. Those few instances where the translation of educative technologies has been studied in this regard have all highlighted these issues (Hirschauer, Citation1991; Johnson, Citation2008; Prentice, Citation2013; Nott and Harris, Citation2020, Citation2022).
The immutable nature of educative technologies – and their enduring epistemic affect – contributes to the reproduction of historically- and spatially-specific assumptions of what is normal and what is not. Our material history, across a range of medical schools, illustrates the unevenness of the ‘epistemic virtues’ reproduced in educational technologies (Daston and Galison, Citation2010). It also details the persistence of the various historical ideals which remain present within the modern medical school. In order to show this, we adopt Joseph Dumit (Citation2014) and Donna Haraway’s (Citation1997) ‘implosion’ methodology. This method involves breaking apart indivdual objects, and unravelling the historic, mythic or economic threads which pull at their contemporary use. It is a method which we have found particularly relevant to ethnographic-historic collaboration (Nott and Harris, Citation2020). Here, our starting point is ethnographic. That is, we began with the observations of three ethnographers, Author 2 being one of them, and shaped a historical implosion around that. The three ethnographers had spent one academic year in the above mentioned medical schools, collecting fieldnotes, photographs and materials. Author 1 joined the team a year later, using these ethnographic materials as his starting point, and finding his own way in the fieldsites, and their related archives and museums.
The implosion of teaching materials became a productive and insightful way to tie together the methodological practices of history and anthropologywhich have been employed in our collaborative project. While there were many material elements of confluence and contrast across the three field sites, ophthalmology and the eye offered a particularly rich starting point for reflection, comparison and analysis. Each ethnographer had meaningful experiences during classes which focused on the eye, and were struck by the materials which assisted the teaching. As it turns out, these objects also offered rich histories to unpack. In this article, we implode the teaching materials which facilitate teaching about the eye, which are initially described in vignettes, and work backwards through their material and conceptual histories. The vignettes are taken from fieldnotes recorded during Author 2’s research at Maastricht and also generously provided by Rachel Vaden Allison and Andrea Wojcik, who conducted ethnographic fieldwork at Semmelweis and UDS respectively. We then pull at the historic threads of present practice. This comes through Author 1’s oral histories, archival research, and time well-spent in museum collections and hospital storerooms across two continents. Following these sticky historical threads opens up broader questions concerning how pathologies are reproduced in the construction of educational technologies and as part of a medical school’s unique material setting. In doing so, our article builds on the assumption that the pull of past practice can affect, direct and misdirect medicine in the present (Nott and Harris, Citation2020).
These methods also help build the central claim made in this article: that material approaches to medical education are shaped by histories of knowledge production particular to each of our three universities. Semmelweis offers what might be described as a ‘traditional’ form of medical education. A hallmark of this approach is the thorough introduction to anatomy, taught in conjunction with extensive cadaveric dissection, which has formed the basis of Semmelweis’ approach since the university moved to its current site in the late-nineteenth century. Maastricht opened in the mid-1970s as a provincial university, and something of a reaction to the dominant, didactic tradition apparent at older universities, such as Semmelweis. A pioneer of Problem-Based Learning (PBL), a pedagogy which encourages learning from small-group, hands-on approaches to real-life scenarios, students at Maastricht are encouraged to develop clinical skill in conjunction with scientific knowledge. Skills training takes place in a purpose-built ‘skills laboratory,’ or Skillslab. Here, students practice on themselves and their classmates, on specially trained ‘standardised patients’ and, most importantly for our analysis, on a wide variety of models and material simulations.
UDS is another adherent of the PBL approach and has close institutional ties with Maastricht. Opened in the 1990s in order to address the longstanding shortage of medical practitioners in the north of Ghana, UDS has also adopted the Skillslab approach and, along with it, a considerable number of imported, European models and mannequins. However, the application of a skills-heavy pedagogy vies with the university’s relative lack of funding, and attendant constraints on the material resources necessary for the maintenance, repair and replacement of these objects. Visiting each of these sites in turn – from oldest to newest – we show that contemporary approaches to medical education are shaped by the various epistemic traditions which are manifest in the materials used in teaching. Although educational practice is affected by sector-wide shifts in discourse and pedagogy, the material culture of the medical school does not always acquiesce to such subtle change. Instead, the specific, historied constellations of educational technologies encountered at each school contributes to a distinct material culture of education and, by extension, to various epistemiologies and ontologies in each of our three sites.
Prototypes, archetypes and beautiful specimens
Built in 1898, Semmelweis University’s Department of Anatomy, Histology, and Embryology is an appropriate material witness to the conceptual development of normality in Europe. Born initially out of comparative anatomy, the concept of the normal bears, as Ian Hacking has argued, ‘the stamp of the nineteenth century and its conception of progress’ (Hacking, Citation1990, p. 161). Over the course of a century the ‘normal ceased to be the ordinary healthy state; it became the purified state to which we should strive’ (Hacking, Citation1990, p. 168). Both Canguilhem and Foucault have traced the history of normality alongside the process of normalisation and the disciplinary technologies which fostered the development of biopolitics into the twentieth century (Foucault, Citation2003; Canguilhem, Citation2007; Cryle and Stephens, Citation2017). The affective weight of Semmelweis’ material history lends these theoretical approaches a degree of substance which seems appropriate here, in a school which celebrates an ‘old world’ approach to medicine, rooted in dissection and student study of post-vital tissue (Schuetze, Citation2013). These are the kind of practices which facilitated ‘the birth of the clinic’ and the shifting conceptualisation of disease away from symptom-based nosology and towards its contemporary basis in pathological anatomy (Foucault, Citation2003). Semmelweis’ epistemic technologies – its cadavers, persevered specimens and hand-painted illustrations – still seem to claim an objective, archetypal form of ‘the body,’ one which is faithfully preserved in formalin. In its exhaustive focus on anatomy for first- and second-year students, Semmelweis’ guiding principle remains that, in order to understand what is pathological, students have to first know an anatomical normal.
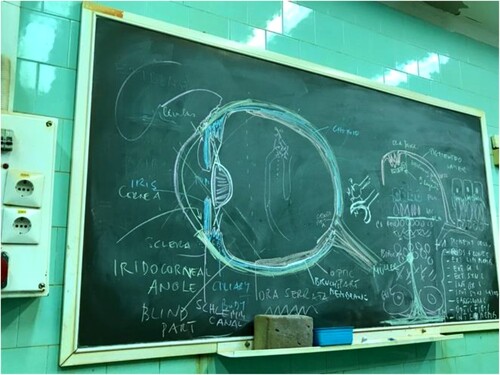
A challenge which educators at Semmelweis face when teaching the anatomy of the eye is that these are relatively small organs, too small and too finite for the sort of gross dissection which is routinely employed to introduce larger anatomic structures. Teachers instead rely on various representations of the eye, all of which are used in combination in these classes. They make detailed drawings on chalkboards in imposing lecture theatres lined with wooden seats. Large, hand-painted posters are brought out; hung up by assistants, they dramatically flank the chalkboard during lectures. Yet, as Rachel Vaden Allison noted in fieldnotes from the winter of 2017, and as is often the case at Semmelweis, the dissection room plays host to students’ most affecting introduction to the eye:
The teacher begins an afternoon lesson holding a model of the human eye. The eyeball is roughly the size of two clenched fists and can be broken apart into five pieces. She unpacks the model eye onto a green tea towel that she has laid on the metal gurney and starts describing the eye and some of its functions whilst holding pieces of the model and pointing to the corresponding structures. Soon she walks to the chalkboard to make a drawing of the eye. This starts out relatively simple, just an outline, but she comes back to it throughout the rest of the class, adding layers and structures, until it becomes a complex layering of chalk.
After these introductions, animal and human models are added into the lesson. The teacher leaves the room and returns with an eyeball in her hand. Some students speculated that it was from a cow. The students lay a tray on the first gurney and the teacher places the eye on to it. She then gets a small surgical saw and cuts the eye in half vertically, between the lens and the retina. … The lens is passed around and everyone feels and, in one case, smells all of the structures previously introduced. After some time, while the teacher talks from the chalkboard, one of the students picks up one half of the now abandoned eye and holds it in his hand. He looks back and forth between the eye in his palm and the chalk drawing.
The class now moves onto the cadaver. The teacher says that they are now going to try to ‘free’ the eye, then begins to chisel at the cranium right above the eye socket. It is silent for a minute or so. She then breaks the silence saying, ‘this is the funnest bit of class, isn’t it?'
The thrill of dissection is a common experience in medical school ethnographies, one which seems to derive from the nature of the material under consideration. While medicalised interactions with the living bodies of patients and classmates is also seen to challenge student understandings of the body, it is commonly suggested that dissection is the most transformative element of the medical school experience (Hirschauer, Citation1991; Good, Citation1994).Footnote2 Byron Good’s study of Harvard medical school, for instance, poses dissection as a literal analogue to the broader objectification (and depersonalisation) of the biomedical body (Good, Citation1994, p. 74). But our professor’s excitement cannot be taken as some transgressive thrill. Instead, her enthusiasm for dissection is indicative of a faith which is shared by most of Semmelweis’ faculty, a belief that human dissection is the surest means to understanding the body ().
Figure 4. Eye models used in the dissection laboratory in Budapest, 2019. Courtesy of Rachel Vaden Allison.

Figure 5. Chalk drawings used in the dissection laboratory in Budapest, 2019. Courtesy of Rachel Vaden Allison.
As an educational technology, the cadaver seems to promise absolute fidelity, and it is the objective clarity of human remains which ties Semmelweis’ pedagogy to the logics of nineteenth-century science. Alongside colleagues in Paris, the pioneering French anatomist Xavier Bichat sought to explain that material changes seen inside the body offered insight into the cause of disease. ‘Open up a few corpses,’ wrote Bichat in 1801, ‘you will dissipate at once the darkness that observation alone could not’ (quoted in, Foucault, Citation2003, p. 146). It is worth noting that a number of corpses is required. Indeed, in their recent ‘genealogy of normality,’ Cryle and Stephens (Citation2017) suggest that, throughout the nineteenth century and well into the twentieth, the medical profession, recognising that variability was the rule, were wary of any suggestion that the normal could be understood as a quantifiable average.
Anatomy professors at Semmelweis remain well aware of this problem but, in the absence of the countless cadavers required to properly illustrate the ‘normality’ of variance, supplementary educational materials deviate towards the aesthetic distinction of the archetype, as is evident in the beautifully painted posters and oversized models. This is similar to the selective portrayal of the ideal type, as seen in anatomical atlases throughout the nineteenth century, or what Daston and Galison (Citation2010) have described as a process of bringing ‘truth-to-nature.’ During the nineteenth century this was partly due to the technologies of production – pencil, charcoal and paint – and reproduction – engraving, mezzotint and lithography. Varying levels of art and artifice allowed anatomists to show what ‘was not always visible to the eye, and [was] almost never to be discovered in the individual specimen’ (Daston and Galison, Citation2010, p. 104).
In their continued employment of a departmental artist, and in the continued use of artistic representation in the adornment of lecture theatres and in the Department’s own anatomy textbooks, Semmelweis proudly continues in this tradition. The eye model in Rachel’s fieldnotes offers an obvious (and more modern) archetype of the anatomical eye. The chalkboard drawing – seemingly spontaneous but actually deriving from years of experience and practice – also offers students an ideal, an elegant rendering that unfolds in a less piecemeal way than the plastic model. The chalkboard, in this respect, complements the material limitations of the cadaver. An ‘immobilised mutable’ (Barany and MacKenzie, Citation2014), and ephemeral almost to the point of immateriality, chalk drawings are used to help bring truth to the natural but imperfect forms which are under dissection.
There is also an important distinction between student’s dissections – which allow for exploratory understandings of the body – and those which are professionally dissected, then stored or preserved. Tutors may explain that something cannot be seen on a particular cadaver due to age or a history of ill-health, and they will instead refer to another cadaver, to a preserved dissection, or to their chalk drawing. Although students are expected to know that variation is the norm, they are also expected to see beyond it and to recognise what ought to be.
In this respect, the weight of nineteenth-century philosophies of science have retained their epistemic influence at Semmelweis. Teachers and technicians often laud the beauty of a particular specimen and the skill which was required to expose its fine anatomic details. Indeed, the memorial plaque for Professor János Szentágothai (1912–1994) states that
Anatomy, for me, is not merely the unalienable foundation of the totality of medical thought and action. It is also one of the highest order manifestations of the eternal beauty and harmony of matter and existence. (Hargittai and Hargittai, Citation2015, p. 121)
Here beauty does not always suggest normality but is, rather, the clear isolation of something archetypical (Rice, Citation2008). Properly presented, the post-vital body offers the objective clarity of taxonomic distinction and helps to materialise what can otherwise only be seen in chalk or paint. But when, as is the often the case at Semmelweis, the archetype is conflated with what is normal, it can be considered ‘prototypical and no longer simply archetypal’ (Canguilhem, Citation2008, p. 127). When the prototypical body becomes the norm, the disciplinary potential of biomedicine also becomes much more apparent. In this respect, the educational technologies employed at Semmelweis bridge contemporary practices with nineteenth-century epistemologies, enlivening, reproducing and further necessitating historical analyses from the likes of Canguilhem and Foucault. This constellation of technologies privileges an abstract, universal idea of what the eye should be, rather than promoting a reflective uncertainty, or responsiveness to contextual influence.
Simulating a spectrum of normality
In Budapest’s Semmelweis Museum of Medical History there is a very similar ophthalmological phantom to that which is kept in Leiden’s Boerhaave Museum (). Unlike in the study of singular specimens or archetypical reproductions, material simulations of the body allow greater insight into a spectrum of bodily presentations. Until fairly recently, the use of simulations was something of a novelty in Semmelweis and the older medical schools and teaching hospitals in Amsterdam, Leiden and Utrecht. Further to the south, however, in Limburg, a historically peripheral part of the country, Maastricht University developed as a determined break from these traditions (Klijn Citation2016). Founded only 40 years ago, Maastricht embraced simulation and, today, when rifling through the cupboards of the university’s Skillslab, you can find a more modern iteration of an ophthalmological phantom (). The pedagogy of Problem-Based Learning (PBL), partially developed here, encourages hands-on, clinical skills training, with students often using their own bodies as a material simulation of their future patients (Wachelder, Citation1992; Servant Citation2016). In doing so, the Maastricht approach has meant that students are confronted, early in their medical education, with the blurred boundaries and muddled spectra that trouble the concepts of pathology and normality.
In Maastricht's Skillslab, abnormalities are introduced in simulated clinics populated by patient simulations. Here, in rooms designed to closely resemble hospital clinics and doctors’ surgeries, medical students experiment on material simulations, on each other and on themselves. The building is large enough for individual rooms to be divided up by specialism and a room on the top floor is reserved for the training of eye examinations. The room looks like all the others, except that its walls are adorned with eye charts and its cupboards are filled with eye examination equipment, including an updated ophthalmological phantom. As Author 2 observed in her fieldnotes, student introduction to the eye begins with the clinical ‘problem’ of eye examination:
Two students are examining one another, a female student who was wearing glasses and a male who was not. When the teacher asked if they had had eye examinations before, the female student said that she had had lots, but the male student had not had any. The teacher then flicks a switch below the three light boxes in the room, and they splutter into life. The lightbox illuminates charts that show rows of the letter C, presented in decreasing size from the top of the chart to the bottom. The gap in the C points randomly in four different directions – to the right, left, up and down.
In the eerie light of the charts, students are instructed on how to instruct the patient. Students practice instructing a patient on where to stand, how to cover one eye and how to read the chart. They need to tap on the lightbox, so it is clear which letter they are pointing to. They need to check that the patient is not straining an eye too hard. They need to travel from the patient’s left to their right. And they need to find ways to change their patterns, so that the patient does not ‘learn’ the chart and thus fake the test. For those who cannot even read the chart, students are taught to hold up two fingers.
But these two students are not listening too well – they just want to have a go at reading the letters. The male student volunteers first. He bounds up for his role as a patient. He obviously wants to excel at this, he wants to show not only that he is he normal but that he exceeds the standard.
In these notes, we see medical students learning clinical examination skills with an instrument straight from the doctor’s office. The standard which is materialised in this eye chart is commonly referred to as 20/20 vision, at least in the Anglophone world, and the eager student represents what Canguilhem would describe as ‘more than normal’ (Canguilhem, Citation2008, p. 132). A defiant vestige of the imperial system of measurement, persons with 20/20 vision are able to read a specific line of a given chart from twenty feet away. Twenty feet from the same chart, someone with 20/30 vision would only be able to make out the letters a ‘normal’ person could see from thirty feet. Although eye charts accommodate the measurement of sharper eyes – and population-level studies suggest that 20/20 has never been a measurable average (Elliot et al., Citation1995; Colenbrander, Citation2008) – this is the standard which physicians and allied health professionals work to in diagnoses and correct to with glasses, contact lenses or surgeries. The 20/20 paradigm provides a biomedical norm which is taken to be both the average and the ideal. Developed in the late nineteenth century, this chart, the Landolt C (), as well as its more famous Dutch predecessor, the Snellen chart, can be seen as part of a Foucauldian history of normalisation in biomedicine.
These tools were not, however, designed for this purpose. In his history of the eye chart, William Germano explains that ‘the eye chart depends on uncertainty, the presence of the border … it’s the edge that the eye chart tests for’ (Germano, Citation2017, p. 9). Herman Snellen, Edmund Landolt and other nineteenth century ophthalmologists designed these charts in order to identify ‘a standard metric, not offer a scientific judgment on normal or abnormal vision’ (Germano, Citation2017, p. 60). Yet what the students in the Skillslab show is that, in the course of learning with and through instruments of measurement, eye charts contribute to the enactment of precisely these judgments. Clearly, the uncritical use of diagnostic tools in medical education has the potential to reproduce the conflation of the norm and normal, the statistical and the ideal. As technologies which objectify the subjective experience of sight, eye charts oversee the creation, crafting and quantification of the seeing body.
At other times, however, such educational tools offers students a means to challenge this narrow construction of normalcy. The Skillslab’s pedagogic focus on the students’ own bodies, for instance, allows for routine confrontation with their own, unique biologies. While the student with glasses would probably not consider herself pathological this is, perhaps, because of the nature of the lesson and the robustness of medical infrastructure in Western Europe. If health is ‘life lived in the silence of organs’ (Canguilhem, Citation2007, p. 91), our student’s glasses mediate what, in another place or another time, might have been profoundly pathological into something which is little more than a habitual inconvenience.Footnote3 As with many lessons in the Skillslab, this approach helps to show students that variation is, in fact, the norm and that deviation from the standard does not necessarily correlate with illness. Elsewhere, in classes which focus on physical examination, or the laboratory analysis of students’ own tissue samples, students routinely find anatomic oddities in themselves and their classmates and protocols exist for the reporting of any more troubling findings. This does not mean that the social stigma of disease has been eroded but that students are forced to confront their own potential for pathology.
These confrontations are a central part of Maastricht’s concious break from epistemic tradition and have been a considered element of the PBL and Skillslab approaches since the 1970s (Wachelder, Citation1992; Servant, Citation2016). Here, use of the student body as a teaching tool was intended to contribute to a more porous boundary between practitioner and patient. Into the 1970s, one of the medical faculty’s orienting principles was an emphasis on pathology rather than normal anatomical function (Wachelder, Citation1992, p. 250).
As at Semmelweis, Maastricht’s intellectual history influences which teaching materials it employs. Unlike in Budapest, however, the Skillslab’s educational technologies, and the ways that they are used, attempts to eschew a nineteenth-century, idealised form of normality. They are, instead, more reflective of twentieth-century ideas. Since its inception, Maastricht has, for instance, engaged heavily with film, and the intimate realities and uncertainties which it purports to show (Audiovisuele Dienst Rijksuniversiteit Limburg, Citation1975, Citation1980). As Lukas Engelmann (Citation2019, p. 23) has recently argued, moving the camera away from the visible manifestations of disease – as in the Skillslab’s filmed re-enactments of encounters with patients – ‘renders objects and bodies uncertain, and thus crafts the conditions under which the investigation of a pathology can commence.’ Yet these technologies coexist with others which actively work to fix the body. Open cupboards in the Skillslab, and you find ophthalmological phantoms and dolls designed to allow students to diagnose strabismus and nystagmus eyes (), conditions which they are unlikely to see in their classmates. These dolls, as with all material simulations of the biomedical body, struggle to offer students genuine insight into the ontological uncertainties of disease in place (Mol, Citation2002). As Erika Johnson (Citation2008) has shown with reference to obstetric phantoms travelling between producers in the United States and consumers in Swedish universities, variations in the enactment of obstetrics are reflected in the material construction of obstetric simulators and can jar with localised practices.
Neither archetypes nor prototypes, the bodies which are present in the Skillslab (student’s own, other students,’ and those of the phantoms) introduce a conceptual spectrum of normality and pathology. The pedagogic value of the eye exam lies in its illustration of uncertainty; inviting students to use their own bodies broadens what can be considered normal or pathological. But while a spectrum of normality and pathology may be considered universal, there is no universal spectrum. As with ophthalmological or obstetric phantoms, the eye chart provides students a spectrum of normality which reflects the history of the materials themselves. As such, and as at Semmelweis, normality and pathology are learned in relation to the teaching materials and material subjectivities which are present in the classroom.
Absent pathologies
In Maastricht, learning physical examination – including some skills which are unlikely to be used in clinical practice – is justified in various ways. One of these is the possibility that students may find themselves in situations where they do not have diagnostic technologies, where they are left with their body alone and maybe a few simple tools. This place is often imagined as ‘Africa.’ In other classes, this generalised Africa is also imagined as a place in which students might encounter ‘tropical’ diseases which are absent from the Netherlands. Although in Dutch universities Africa is expressly removed – in terms of both practice and pathology – from the Netherlands, Ghana’s University for Development Studies’ skills curriculum builds from the Maastricht model. Ghanaian universities are often beholden to teaching tools and textbooks that promote Western medicine as the ultimate telos of ‘global health’ and in which African science is determinedly peripheral (Nott, Citationforthcoming). Most of the models used in skills training at UDS were, for instance, obtained with Dutch assistance and from European manufacturers. These simulations – partial reproductions of human anatomies which allow students to practice more invasive physical examinations and procedures – also reproduce particular constructions of normal and pathological bodies. Lumps on model breasts and growths on model prostates offer an embodied, sensory introduction to ostensibly universal pathology, but one developed with a European patient public in mind. These are tools which speak to the spaces and times in which they were developed, as well as to unproved assumptions of universality in epidemiological change (Adjaye-Gbewonyo and Vaughan, Citation2019). When technologies encourage students to feel for specific pathologies, students also feel the histories, philosophies and subjectivities which have gone into their construction (Johnson, Citation2005; Nott and Harris, Citation2020).
Educators in Ghana are, of course, well aware of this problem and have long endeavoured to better localise both practice and pathology. One of the ways in which this might be done is through the local construction of teaching tools, but such efforts are often limited by structural and economic constraints (Kumoji and Nott, Citation2022; Nott, Citationforthcoming). Another is to move learning away from the materials in the classroom altogether. Although interaction with patients is a universally affecting element of medical education, at UDS the clinic introduces forms of pathology and normality which tend to be absent from the imported educational technologies commonly found in the pre-clinical environment.
As in Maastricht, students at UDS come to understand the eye via the clinical ‘problem’ of the eye exam. As also in Maastricht, a standard eye exam is introduced in a Skillslab. At UDS, however, these international standards are immediately challenged as students move into hospital clinics. When Andrea Wojcik arrived at the clinic at the university’s teaching hospital, she was met by patients lined up on benches, some with patches and bandages covering their eyes. In another room, students gathered with a doctor and nurse:
The assessment room consists of a desk, a curtained area, a fridge, two chairs and two eye charts which have only the letter ‘E,’ facing in one of four directions, hanging from the wall. The practice nurse proceeds with an extensive explanation of how to conduct the sight test. Much of this concerns what to do if the patient could not see the eye chart at all. They should, first, hold up two fingers from six meters, then five, four, three, two, one and, if the patient still cannot see the doctor’s hand, they then test to see if they can detect movement by waving in front of their eyes. If the patient cannot see this, students are instructed to test if they can perceive light, using a pen torch.
Following this detailed explanation, the nurse noted that rather than going step by step through the protocol, he often simply observes the patient and, depending on their behaviour, starts somewhere in the middle of the test. In fact, when the first patient enters, he skips the eye chart altogether, immediately putting up two fingers.
Throughout the clinic, as patients come and go, students try to navigate the eye exam per the protocol, while the nurses improvise regularly, sometimes starting with their fingers, then moving to the chart. All of this happens in a buzz of translation, between words, letters, signs, fingers.
Given that UDS students are often poorly served by educational technologies, the clinic offers unique insight. Here they are introduced to the localised forms of normality and pathology which are absent from the commercial teaching materials that populate the university.
The medical school at the University for Development Studies was established in the 1990s, in order to train doctors to practice in Ghana’s historically underdeveloped northern savannah (Bening, Citation2005). Here, and unlike in Maastricht, students are offered much more detail on what to do if a patient is unable to see the largest letter on the chart, a metric often as the legal standard for blindness. Tamale’s peripherality, relative to both national and international centres of medicine, echoes the long history of economic and medical neglect which has allowed for the persistence of endemic eye diseases in the north of the country, and the resultant high local burden of blindness. Historical neglect, under British-colonial government, was such that, by the 1950s, perhaps three percent of the North’s total population was clinically blind, with rates as high as twenty percent in some villages (Waddy, Citation1956). As with many of the other diseases endemic in this peripheral part of the country, throughout much of the twentieth century, blindness went ‘unnoticed, or if noticed, disregarded’ (Patterson, Citation1978, p. 109–110).
The gravity of biomedicine’s historic and epistemic centre, and the normativity which it continues to define, are materially present in Andrea’s fieldnotes. The eye chart most commonly used at UDS, the ‘Tumbling E’ or, as it was described originally, the ‘Illiterate E’ eye chart represents a relatively recent development in the testing of visual acuity. Developed in the late 1970s, this chart was initially used in order to compare the visal acuity of indigenous Australians in comparison to that of Europeans settled in Australia (Taylor, Citation1981). In this respect, the Tumbling E was developed in order to judge a racialised population against a European construction of normality, and in pursuit of their continued racialisation. On another level, and as the anthropologist Jack Goody once explained with reference to the North of Ghana, technologies which privilege literacy – written legal contracts in Goody’s example – ‘place the unschooled at a very definite disadvantage and turn them from non-literates into illiterates’ (Goody, Citation1980, p. 146). While the Tumbling E charts are clearly a useful tool, their material presence in Tamale also serves to highlight Ghana’s peripheral position in biomedical frameworks and traditional centres of knowledge production. Perhaps because of this, part of what students learn in the clinical setting is to disregard the chart and the methods which they had been taught in the classroom. In practice, as in the fieldnotes above, nurses and doctors use their hands and pen torches in a more improvised fashion, with the Tumbling E just one part of this material assemblage. Here, clinicians teach a form of assessment which begins with the whole patient, not just with the eye, and also not from the assumption that everyone should be able see the chart or read the letters on it.
Siting medical education away from the models and simulated material found in the classroom, the eye clinic offers an alternative way of learning about patients, one which better reflects local epidemiologies. These practices reach towards what Canguilhem had called for in the mid-twentieth century – recognising ‘the categories of health and disease only on the level of experience … and not on the level of science. Science explains experience but it does not for all that annul it’ (Canguilhem, Citation2007, p. 198). Due to the limitations inherent in educational technologies inherited from elsewhere, the privileging of experience over received understandings of medicine is simply more necessary at UDS than in the European schools.Footnote4
The quiet history of epistemic localisation in the north of Ghana compliments the renewed interest in the geopolitics of knowledge. Emphasising the influence of European epistemologies in the endurance of colonial power structures, decolonial theorists have called for ‘epistemic disobedience’ as a means to disrupt the authority of European intellectual tradition in non-European universities (Mignolo, Citation2009; Nyamnjoh, Citation2019). This also requires some reflection on the materials through which knowledge is reproduced. Educational technologies privilege knowledge over experience, they are predicated on historically- and spatially-contingent epistemologies and, while co-existing practices of improvisation and performance can subvert these tools, their relative immutability encourages some degree of epistemic obedience (Nott, Citationforthcoming). As agential actors in the reproduction of biomedicine, the material origins of educational technologies bear express relevance to the globalisation of biomedicine, the construction of a universalist medical imaginary, and the attendant peripheralisation of any localised forms of medical knowledge. Disruption of the material assemblages which sustain these traditions has not really been considered as part of any such action, nor has what these ideas mean for epistemologies of medicine (Harding, Citation2016). UDS’ necessary reliance on clinical settings for the localisation of medical learning forms part of the long and largely unsung history of African innovation in biomedicine (e.g. Tilley, Citation2011; Mavhunga, Citation2018). Confronted with technologies that reproduce alien constructions of the normal and pathological, siting education away from the classroom allows for more reflexive, localised spectra of what is to be expected in the patient population.
Conclusion
In 2019, London’s Moorfields Eye Hospital and University College London received ethical approval to link data from its collection of more than 15,000 eye scans with patient information drawn from elsewhere in the UK’s National Health Service. The researchers hope that machine learning and artificial intelligence will soon allow eye scans to be used as an advanced predictor of a wide range of pathologies – from Alzheimer’s to heart disease (The Economist, Citation2019). With ever-increasing surety and at ever-more granular scales, such technologies are contributing to a ‘total pathology’ (Engelmann, Citation2020) and, in doing so, are shifting the boundaries of the normal and the pathological. However, the construction of normality and pathology in biomedicine has long been central to its critique. As Canguilhem (Citation2008) argued from the 1940s, absolute insight into disease is predicated on absolute understandings of what the normal body is like. That the normal contributes to the normative, or what is healthy is conflated with what is morally right, was fundamental to Michel Foucault’s later philosophy of medicine. Normality was then cast as an important tool in the development of biopower and biopolitics from the late nineteenth century onwards (Foucault, Citation1979, Citation2004). As STS research continues to emphasise, the discipliniary potential of normativity endures in contemporary technologies, reproducing the assumptions, and sometimes also the prejudices, of the society from which they derive (e.g. Benjamin, Citation2019). In order to illustrate this, the social study of science in the present must pay greater attention to the historied materialities which shape contemporary medical practice.
The material conditions of medical education are under-researchered actors in this respect, and in the reproduction of the normal and pathological body. As such, this article has asked how variations in the material culture of medical education in three different medical schools has contributed to variations in the construction of what is normal and what is not. We consider these educational technologies as often being ‘immutable mobiles,’ movable technologies which encourage the reproduction of practices across time and space (Latour, Citation1990, p. 7). As material evangalists for specific and innately historical ideas within medicine, differences in the constellations of teaching tools results in a different material episteme of biomedicine in each school. As our historical implosion of ethnographic vignettes has shown, past practices and old epistemologies endure within these variable constellations of technology. Bounded to the time–space of their construction by the immutability of their design, how these schools approach the slippery concepts of pathology and normality continues to be influenced by the agential histories which materialise in the technologies used for teaching. Yet, as we see in educational practices in Ghana, there are also signs of alternative ways of knowing with these objects, ways of blurring boundaries, and of dispersing standards through experimentation, innovation, and resistance to the epistemic traditions bound up in these technologies.
At Semmelweis, the oldest university in our research, a thorough introduction to anatomy, taught in conjunction with extensive cadaveric dissection, has been the basis of instruction since the late-nineteenth century. Here, the continued primacy of dissection and the study of post-vital tissue reproduces the nineteenth-century conflation of the normal and the archetypical. Developed in the 1970s as a provincial university and, in part, as a reaction to the dominant, didactic tradition apparent at Semmelweis and in the Netherlands’ older medical schools, Maastricht’s focused on clinical problem solving rather than on abstracted anatomy. Learning from a PBL curriculum and in a purpose-built ‘skills laboratory,’ normality and abnormality are purposefully blurred through the pronounced use of patient simulations, including the students’ own bodies. This approach offers students greater insight into a spectrum of normality, as well as its social construction, but is ultimately still bounded by the technologies which illustrate and define any such spectrum. In other words, our analysis shows that although students in the Maastricht Skillslab are introduced to a spectrum of bodily manifestation, it is a spectrum which is still historically and spatially contingent.
Our third site, the University for Development Studies, opened in the 1990s in order to train medical practitioners in the historically marginal north of Ghana. Another adherent of PBL, and with close ties to the medical school in Maastricht, UDS has also invested in a Skillslab and, along with it, a considerable number of imported models, mannequins and diagnostic tools. However, these technologies are often rooted in a relatively alien construction of what is normal and what is not. Because of this, introducing students to the elusive concepts of normality and pathology requires a more reflexive use of educational technologies, and a more conditional approach to the imported standards which they tend to reproduce. At UDS, an early, experiential introduction to the practicalities of community medicine is, then, an entirely necessary response to the material limitations of the educational tools found in the classroom.
In this respect, the material practice of medical education at UDS also offers some redress to longstanding biases at the heart of biomedicine. Largely out of necessity, medical school practice in the north of Ghana resists the representations and often alien standards typically found in teaching materials imported from Europe or North America. By teaching around and beyond these materials, Ghanaian eductors also challenge their ontological assuredness and intellectual bases.
STS scholarship has recently mobilised Canguilhem’s work on normality in order to consider the diagnostic value of technologies which allow for uncertainty (Engelmann, Citation2019). Uncertainty provides a degree of reflexivity, privileging action based on lived experience of events, rather than deference to knowledge of pre-existing norms and standards (Jerak-Zuiderent, Citation2012). At UDS, the uncertain value of educational tools which are drawn from the European history of biomedicine – and which are somewhat limited as a result – also offers some resistance to the Euro-centric orientation of biomedical epistemology. This is a tradition which has long employed racialised, gendered, ableist and heteronormative standards as part of a biopolitical construction of the normal and pathological (e.g. Davis, Citation1995; Warner, Citation1999; Carter, Citation2007). In African contexts, as in other previously colonised spaces, these ideas have also been employed as a means of subjugation, and continue to cast African experience as tangential to the development of medical science (e.g. Comaroff, Citation1993; Mkhwanazi, Citation2016). However, UDS’s privileging of experience over inherited epistemology provides something of a break from the ‘cognitive empires’ of Euro-American epistemology (Santos, Citation2018), as well as from the historical and material determinants of normality and pathology as understood in its traditional, metropolitan centres. The same epistemic disobedience which has been forwarded as a means to sever intellectual dependence on European tradition in postcolonial contexts might also offer a liberatory challenge to the historical and material determinants of normative othering in European contexts too.
Acknowledgements
This article has been drawn from a larger collaborative project, ‘Making Clinical Sense: A Comparative Study of How Doctors Learn in Digital Times’ (www.makingclinicalsense.com). Our colleagues on this project have contributed significantly to the ideas developed in this article and offered sage advice on earlier drafts. We would particularly like to thank Andrea and Rachel for their generosity in sharing their own fieldnotes and photographs with us. Their own work from their medical school ethnographies is forthcoming. A version of this paper was shared with the Maastricht University Science, Technology and Society Studies research group during our annual Summer Harvest, and we are grateful for the comments we received, especially those from Denise Petzold. The paper was also presented online at the Society for the Social Studies of Science meeting in 2020, thanks to the organisers and attendees for the discussion which emerged. Mieneke te Hennepe generously toured us around the storerooms of the Rijksmuseum Boerhaave. Finally, we are ever grateful to our friends in the medical faculties at the University for Development Studies, Maastricht University, and Semmelweis University. It is their generosity and openness which has made this research possible.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
John Nott
John Nott is a historian of health and medicine, and currently a Research Fellow in Science, Technology and Innovation Studies at the University of Edinburgh.
Anna Harris
Anna Harris is an Associate Professor of the Social Studies of Medicine at Maastricht University. Working at the intersections of STS and anthropology, her ethnographic research largely concerns the material, sensory and bodily nature of medical practices.
Notes
1 The fundus is the concave interior surface of the eye, opposite the lens which includes the retina, optic disc, macula and fovea.
2 These assumptions have been challenged by recent ethnographies which highlight the enduring personhood of the cadaver. This should, however, be understood as a historical shift and cannot be taken to undermine the affective weight of dissection (Hallam, Citation2017; Olejaz, Citation2017).
3 Canguilhem is quoting French surgeon René Leriche here. Normal physiology is constructed by a constellation of epistemic tools and reinforced by an even broader constellation of everyday technologies. The world is sized and scaled according to the assumption that the majority of people have 20/20 vision. It is only those whose eyes cannot be corrected to this standard that exist beyond the pale of normality. It is beyond this, that the disabled body begins to be constructed.
4 This has grown into a central feature of UDS’ pedagogic practice. Early on in their programme, UDS embeds students in the diverse range of environments found across the North of Ghana. This has been seen to contribute to the university’s successful retention of gradute doctors in these spaces (Amalba et al., Citation2016).
References
- Adjaye-Gbewonyo, K. and Vaughan, M. (2019) Reframing NCDs? An analysis of current debates, Global Health Action, 12(1), pp. 1–10.
- Amalba, A., van Mook, W. N. K. A., Mogre, V. and Scherpbier, A. J. J. A. (2016) The effect of community based education and service (COBES) on medical graduates’ choice of specialty and willingness to work in rural communities in Ghana, BMC Medical Education, 16(1), pp. 1–7.
- Audiovisuele Dienst Rijksuniversiteit Limburg. (1975) Slechte en Goede Interviews (Maastricht: ADRL).
- Audiovisuele Dienst Rijksuniversiteit Limburg. (1980) Dokter, ik heb zo’n pijn in m’n been (Maastricht: ADRL).
- Atkinson, P. and Pugsley, L. (2005) Making sense of ethnography and medical education, Medical Education, 39(2), pp. 228–234.
- Barad, K. (2007) Meeting the Universe Halfway: Quantum Physics and the Entanglement of Matter and Meaning (Durham, NC: Duke University Press).
- Barany, M. J. and MacKenzie, D. (2014) Chalk: materials and concepts in mathematics research, in: C Coopmans (Eds) Representation in Scientific Practice Revisited, pp. 107–120 (Cambridge, MA: MIT Press).
- Becker, H., Geer, B., Hughes, E. and Strauss, A. (1961) Boys in White: Student Culture in Medical School (Chicago: The University of Chicago Press).
- Bening, R. B. (2005) University for Development Studies in the History of Higher Education in Ghana (Accra: Centre for Savana Art and Civilisation).
- Benjamin, R. (2019) Race After Technology: Abolitionist Tools for the New Jim Code (Cambridge: Polity).
- Bowker, G. C. and Star, S. L. (2000) Sorting Things Out: Classification and its Consequences (Cambridge, MA: MIT Press).
- Burri, R. V. and Dumit, J. (2008) Social studies of scientific imaging and visualization, in: E. J. Hackett (Eds) The Handbook of Science and Technology Studies, pp. 297–317 (Cambridge, MA: MIT Press).
- Canguilhem, G. (2007) The Normal and the Pathological (New York: Zone Books).
- Canguilhem, G. (2008) Knowledge of Life (New York: Fordham University Press).
- Carter, J. (2007) The Heart of Whiteness: Normal Sexuality and Race in America, 1880– 1940 (Durham, NC: Duke University Press).
- Cassell, J. (1991) Expected Miracles: Surgeons at Work (Philadelphia: Temple University Press).
- Cassell, J. (1998) The Woman in the Surgeon’s Body (Boston: Harvard University Press).
- Collin et Cie. (1925) Catalogue D’instruments de Chirurgi (Paris: Collin et Cie).
- Colenbrander, A. (2008) The historical evolution of visual acuity measurement, Visual Impairment Research, 10(2–3), pp. 57–66.
- Comaroff, J. (1993) The diseased heart of Africa: medicine, colonialism and the black body, in: S. Lindenbaum, and M. M Lock (Eds) Knowledge, Power, and Practice: The Anthropology of Medicine and Everyday Life, pp. 305–329 (Berkeley: University of California Press).
- Cryle, P. and Stephens, E. (2017) Normality: A Critical Genealogy (Chicago: University of Chicago Press).
- Daston, L. and Galison, P. (2010) Objectivity (New York: Zone Books).
- Davis, L. (1995) Enforcing Normalcy: Disability, Deafness and the Body (London: Verso).
- de Laet, M. and Mol, A. (2000). ‘The Zimbabwe Bush Pump: Mechanics of a Fluid Technology’, Social Studies of Science, 30(2), pp. 225–63.
- Dumit, J. (2014) Writing the implosion: teaching the world one thing at a time, Cultural Anthropology, 29(2), pp. 344–362.
- Elliot, D. B., Yang, K. C. H. and Whitaker, D. (1995) Visual acuity changes throughout adulthood in normal, healthy eyes: seeing beyond 6/6, Optometry and Vision Science, 72(3), pp. 186–191.
- Engelmann, L. (2019) Picturing the unusual: uncertainty in the historiography of medical photography, Social History of Medicine, 34(2), pp. 375–398.
- Engelmann, L. (2020) Into the deep – AI and total pathology, Science as Culture, 29(4), pp. 625–629.
- Fenwick, T. (2014). ‘Sociomateriality in Medical Practice and Learning: Attuning to What Matters’, Medical Education, 48(1), pp. 44–52.
- Foucault, M. (1979) The History of Sexuality. Vol. 1: The Will to Knowledge (London: Penguin).
- Foucault, M. (2003) The Birth of the Clinic: An Archaeology of Medical Perception (London: Routledge).
- Foucault, M. (2004) Society Must be Defended: Lectures at the Collège de France, 1975-76 (London: Penguin).
- Fox, R. (1989) The Sociology of Medicine: A Participant Observer’s View (Englewood Cliffs: Prentice Hall).
- Germano, W. (2017) Eye Chart (New York: Bloomsbury Academic).
- Good, B. J. (1994) Medicine, Rationality and Experience: An Anthropological Perspective (Cambridge: Cambridge University Press).
- Good, B. and DelVecchio Good, M.-J. (1993) “Learning medicine”: the constructing of medical knowledge at Harvard medical school, in: S. Lindenbaum, and M. Lock (Eds) Knowledge, Power, and Practice: The Anthropology of Medicine and Everyday Life, pp. 81–107 (Berkeley: University of California Press).
- Goody, J. (1980) Rice-burning and the green revolution in northern Ghana, The Journal of Development Studies, 16(2), pp. 136–155.
- Hacking, I. (1990) The Taming of Chance (Cambridge: Cambridge University Press).
- Hallam, E. (2017) Relational anatomy: dissecting and memorialising the dead in medical education, Medicine Anthropology Theory, 4(4), pp. 99.
- Haraway, D. (1991) A cyborg manifesto: science, technology, and socialist-feminism in the late twentieth century, in: D. Haraway (Ed) Simians, Cyborgs and Women: The Reinvention of Nature, pp. 149–181 (New York: Routledge).
- Haraway, D. (1997) Modest_Witness@Second_Millennium.FemaleMan©Meets_OncoMouseTM: Feminism and Technoscience (New York: Routledge).
- Harding, S. (2016) Latin American decolonial social studies of scientific knowledge: alliances and tensions, Science, Technology, & Human Values, 41(6), pp. 1063–1087.
- Hargittai, I. and Hargittai, M. (2015) Budapest Scientific: A Guidebook (Oxford: Oxford University Press).
- Hartridge, G. (1907) The Ophthalmoscope: A Manual for Students (London: J. & A. Churchill).
- Hirschauer, S. (1991) The manufacture of bodies in surgery, Social Studies of Science, 21(2), pp. 279–319.
- Holmes, S., Jenks, A. and Stonington, S. (2011) Clinical subjectivation: anthropologies of contemporary biomedical training, Culture, Medicine, and Psychiatry, 35(2), pp. 105–112.
- Jerak-Zuiderent, S. (2012) Certain uncertainties: modes of patient safety in healthcare, Social Studies of Science, 42(5), pp. 732–752.
- Johnson, E. (2005) The ghost of anatomies past: simulating the one-sex body in modern medical training, Feminist Theory, 6(2), pp. 141–159.
- Johnson, E. (2008) Simulating medical patients and practices: bodies and the construction of valid medical simulators, Body & Society, 14(3), pp. 105–128.
- Klijn, A. (2016) The Maastricht Experiment: On the Challenges Faced by a Young University, 1976–2016 (Nijmegen: Vantilt).
- Kumoji, R. and Nott, J. (2022) The pathology museum and Korle Bu, in: J. Nott, and A. Harris (Eds) Making Sense of Medicine: Material Culture and the Reproduction of Medical Knowledge, pp. 281–294 (Bristol: Intellect).
- Latour, B. (1990) Drawing things together, in: M. Lynch, and S Woolgar (Eds) Representation in Scientific Practice, pp. 19–68 (Cambridge, MA: MIT Press).
- Latour, B. (2000) On the partial existence of existing and nonexisting objects, in: L Daston (Eds) Biographies of Scientific Objects, pp. 247–269 (Chicago: University of Chicago Press).
- Lock, M. M. and Nguyen, V.-K. (2010) An Anthropology of Biomedicine (Oxford: Wiley-Blackwell).
- Mavhunga, C. C. (2018) The Mobile Workshop: The Tsetse Fly and African Knowledge Production (Cambridge, MA: MIT Press).
- Mignolo, W. D. (2009) Epistemic disobedience, independent thought and decolonial freedom, Theory, Culture & Society, 26(7–8), pp. 159–181.
- Mkhwanazi, N. (2016) Medical anthropology in Africa: The trouble with a single story, Medical Anthropology, 35(2), pp. 193–202.
- Mol, A. (2002) The Body Multiple: Ontology in Medical Practice (Durham, N.C.: Duke University Press).
- Nott, J. (forthcoming) Material history, historied materials, and the question of epistemic freedom in Ghana’s medical schools.
- Nott, J. and Harris, A. (2020) Sticky models: history as friction in obstetric education, Medicine Anthropology Theory, 7(1), pp. 44–65.
- Nott, J. and Harris, A. (Eds.) (2022) Making Sense of Medicine: Material Culture and the Reproduction of Medical Knowledge (Bristol: Intellect).
- Nyamnjoh, F. B. (2019) Decolonizing the university in Africa, in: Nic Cheeseman (Eds) Oxford Research Encyclopedia of Politics, pp. 1–36 (Oxford: Oxford University Press).
- Olejaz, M. (2017) When the dead teach: exploring the postvital life of cadavers in danish dissection labs, Medicine Anthropology Theory, 4(4), pp. 125.
- Patterson, K. D. (1978) River blindness in northern Ghana, in: K. D. Patterson, and G. W. Hartwig (Eds) Disease in African History: An Introductory Survey and Case Studies, pp. 88–117 (Durham, NC: Duke University Press).
- Pope, C. (2005) Conducting ethnography in medical settings, Medical Education, 39, pp. 1180–1187.
- Prentice, R. (2013) Bodies in Formation: An Ethnography of Anatomy and Surgery Education (Durham, NC: Duke University Press).
- Rice, T. (2008) “Beautiful murmurs”: stethoscopic listening and acoustic objectification, The Senses and Society, 3(3), pp. 293–306.
- Rice, T. (2013) Hearing and the Hospital: Sound, Listening, Knowledge and Experience (Canon Pyon: Sean Kingston Publishing).
- Rosenberg, C. E. (1989) Disease in history: frames and framers, The Milbank Quarterly, 67, pp. 1–15.
- Santos, B. (2018) The End of the Cognitive Empire: The Coming of Age of Epistemologies of the South (Durham, NC: Duke University Press).
- Schuetze, C. F. (2013) Medical Students Head to Eastern Europe, The New York Times, 11 August. Available at: https://www.nytimes.com/2013/08/12/world/europe/medical-students-head-to-eastern-Europe.html (accessed 29 May 2020).
- Servant, V. F. C. (2016) Revolutions and re-iterations: an intellectual history of problem-based learning, PhD, Erasmus Universiteit.
- Taylor, H. R. (1981) Racial variations in vision, American Journal of Epidemiology, 113(1), pp. 62–80.
- Taylor, J. S. (2014) The demise of the bumbler and the crock: from experience to accountability in medical education and ethnography, American Anthropologist, 116(3), pp. 523–534.
- The Economist. (2019) A system based on AI will scan the retina for signs of Alzheimer’s, 18 December. https://www.economist.com/science-and-technology/2019/12/18/a-system-based-on-ai-will-scan-the-retina-for-signs-of-alzheimers.
- Tilley, H. (2011) Africa as a Living Laboratory: Empire, Development, and the Problem of Scientific Knowledge, 1870–1950 (Chicago: University of Chicago Press).
- Underman, K. (2020) Feeling Medicine: How the Pelvic Exam Shapes Medical Training (New York: New York University Press).
- Wachelder, J. C. M. (1992) Universiteit tussen vorming en opleiding: de modernisering van de Nederlandse universiteiten in de negentiende eeuw (Hilversum: Uitgeverij Verloren).
- Waddy, B. B. (1956) Organization and work of the Gold Coast Medical Field Units, Transactions of The Royal Society of Tropical Medicine and Hygiene, 50(4), pp. 313–343.
- Warner, M. (1999) The Trouble with Normal: Sex, Politics and the Ethics of Queer Life (Cambridge, MA: Harvard University Press).
- Wood, C. A. (1891) Lessons in the Diagnosis and Treatment of Eye Diseases (Detroit, MI: G.S. Davis).