Introduction
Polycystic ovary syndrome (PCOS) is a very common clinical condition often recurring in endocrinology. Women with PCOS may require advice for many reasons: hyperandrogenism-related symptoms (acne, hirsutism), chronic anovulation and infertility, menstrual disorders, oncologic prevention in case of endometrial hyperplasia, and clinical management of the main metabolic disorders related to obesity and insulin resistance (IR), very often present in these patients.
IR is a special state in which a specific quantity of insulin evokes an abnormal biological response. The processes linked to this condition may concern anomalies involving the secretion of pancreatic cells (abnormal insulin or incomplete conversion of proinsulin to insulin), high blood concentration of hormones counterregulatory to insulin, anti-insulin antibodies or antibodies anti-insulin receptor, and also target organs disorders (because of a reduced quantity of insulin receptors or post-receptor defects). Insulin binds a tyrosine-kinase receptor and activates two possible intracellular pathways: the first one is regulated by the activation of IP3-kinase (inositol 1,4,5-tryphosphate), associated to an enhanced peripheral glucose linking and NO production in endothelium. The second pathway has anabolic function and is linked to the activation of mitogen-activated protein kinase (MAPK), enabling the proliferation of smooth muscle, monocyte migration, and plasminogen activator inhibitor 1 activation (PAI-1).
Methodologically, the assessment of IR may be performed with the euglycemical hyperinsulinemic clamp (based on the infusion of a specific amount of insulin as to stabilize its blood concentration to a constant level of 100 U/mL for 120 min). The evaluation of the amount of glucose necessary to maintain normal glycemia helps to understand the exogenous insulin capacity in letting glucose into tissues. This relatively complex test is the standard method to assess the tissue sensitivity to exogenous insulin.
In clinical practice, the quantitative analysis of IR is easily understandable by the homeostatic model assessment index (HOMA), with reference to two formulas (IR):
HOMA-IR: Fasting glycemia x fasting insulin/22.5 (to apply when glucose is in molar units, mmol/L)
HOMA-IR: Fasting glycemia x fasting insulin/405 (to apply when glucose in mass units, mg/dL)
Normal values are between 0.23 and 2.5. Weblink: http://www.societaitalianadiendocrinologia.it/html/cnt/Strumenti_di_Calcolo,asp.
Women with PCOS have a mean reduction in peripheral sensitivity to insulin assessed about 27%, independently of body mass index [Citation1]. In addition, meta-analysis data show a link of increase of the body mass to a further reduction of about 8% in insulin sensitivity [Citation1].
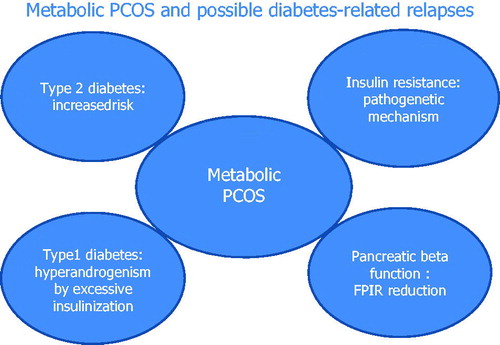
The risk of developing Diabetes Mellitus type-2 (DM2) for women with obesity and PCOS at the same time appear to be as significant and such risk justifies putting PCOS into the clinical conditions which require screening for DM2 (): http://www.standarditaliani.it/.
Table 1. Risk categories deserving screening for potential development of DM2.
A prospective study published on Diabetes in 2012 analyzed 255 women suffering from PCOS for about 10 years (mean follow-up: 17 years). Age-standardized DM2 prevalence resulted 39.3% at the end of the follow-up, significantly higher than the prevalence found in the same-age female population [Citation2].
Regarding diabetes, interest in PCOS is not only limited to DM2. It seems appropriate to mention that girls who have type-1 DM can also have hyperandrogenism (peculiar trait of PCOS) caused by an excessive administration of exogenous insulin, resulting in a hyperstimulation of theca cells in ovary, which produce sexual hormones [Citation3].
Below are physiopathological features involving women having PCOS, with specific focus on diabetological issues.
Traditional physiopathological characteristics
Visceral obesity (abdominal circumference >80 cm in women) engenders an increase of non-esterified fatty acids (NEFAs) in bloodstream. NEFAs are a primary energetic source for skeletal muscles (which consumes 70% of glucose during the post-absorption phase). The preferential employment of NEFAs and peripheral glucose causes a hyperglycemia tendency, which is counteracted by a fast pancreatic response (phase of hyperinsulinism). As a consequence, a chronic condition of normoglicemic hyperinsulinism and excess of insulin occur. The latter causes generalized vasoconstriction, increased sodium reuptake, and lipidic anabolism.
Traditional physiopathological characteristics (with low consideration in clinical practice)
Also, insulin is important in the hepatic district, stimulating glycogenesis, inhibiting glycogenolysis, gluconeogenesis and ketogenesis. When glycogen reaches its saturation point (5–6%), fatty acids synthesis increases, leading the fatty acids to move to adipose tissue. In clinical practice, obese women with PCOS may develop a chronic inflammatory hepatic condition, also known as non-alcoholic steatohepatitis (NASH), which may vary from 30 to 86% in many case studies. NASH reaches 100% occurrence in those case studies which use both ultrasound screening and laboratory exams as well [Citation4]. The only presence of adipose liver, associated to enlarged waist measurement, identifies these women as phenotypically thin but metabolically fat, even in absence of increased BMI (). Consequently, NASH in PCOS-suffering women is an important marker of further IR.
Table 2. Main differential factors between metabolic obesity and phenotypical obesity. Weblink: http://link.springer.com/article/10.1007/BF03345285
Unconventional physiopathological characteristics
Hyperinsulinism is characteristically associated to reduce sexual hormone binding protein (SHBG) production in liver, as a consequence of the inhibitory action of insulin. In women with PCOS, reduced SHBG blood concentrations are linked to a further reduction of about 10% in insulin sensitivity. This can be added up to the adverse action caused by the increase of body mass index, as previously stated [Citation1]. Several researches have proved a negative correlation between SHBG levels and insulin sensitivity [Citation5]. In addition, most prospective studies support the role of reduced SHBG levels as a possible predictive factor of DM2 development [Citation6]. How SHBG reduction may influence insulin sensitivity is still unknown. It is possible to assume that IR is a consequence of abnormal sexual hormones transport and thus, this causes a reduced glucose uptake in muscular tissue [Citation6].
Secretory-cell activity in suffering-PCOS women
There is an ever increasing number of studies focused on the progressive loss of the secretory-cell activity in women suffering from PCOS. After the administration of endovenous glucose load, insulin is released in a biphasic way. The first acute response is called first phase insulin response (FPIR) and begins within 1 min after the administration of glucose, reaches its peak in 3–5 min and lasts about 10 min. In vivo, this phase is independent from pre-stimulus glycemia. Technically, FPIR is correspondent to the sum of all blood insulin levels up to 10 min. The loss of FPIR is an early marker of defective insulin secretion, which is seen in prediabetic people (both type 1 and type 2 diabetes). Changes in insulin secretion occurring after endovenous glucose load tend to happen earlier than the changes seen after oral glucose load. Disposition index values (an indicator expressing the ratio between the increase of insulin secretion of beta cells and peripheral insulin sensitivity) prove that suffering-PCOS women, especially when obese, show a significantly decreased FPIR compared to obese non-PCOS women [Citation7]. Recent experimental surveys demonstrated an inverse relation between the progressive FPIR loss and the activation of Nuclear Factor-KB-mediated pre-oxidation (NF-Kappa light chain enhancer of B cells) [Citation8]. In clinical practice, the quantitative assessment of beta cells pancreatic secretion can be evaluated by HOMA-B% index, that is the HOMA index expressing the pancreatic beta cells activity. Roughly, the value of 100 shows that 100% of beta cells works, whereas a value of 0 shows no function in pancreatic beta cells.
When glycemia is in mmol/L it is possible to apply this formula: HOMA-B% = (20 × fasting insulin blood level)/(fasting glycemia −3.5). Instead, when glycemia is in mg/dL it is possible to apply this formula: HOMA-B% = (360 × fasting insulin blood level)/(fasting glycemia −63).
Brown adipose tissue and PCOS
Besides visceral and subcutaneous adipose tissue, another type is the brown adipose tissue (BAT), which is traceable in paravertebral (cervical vertebrae) supraclavicular, interscapular and perirenal depots. Its most important task is to produce heat in low temperatures, a process called cold-induced thermogenesis. Mitochondria in BAT cells contain the protein Uncoupling Protein 1 (UCP1), which is able to ‘undo’ the oxidative phosphorylation (aerobic energetic process involved in cell respiration) and ‘switching’ lipids from ATP production (chemical energy) to heat production (thermic energy). In addition to low temperatures, BAT is activated by excessive food intake. Theoretically, this whole process, based on the transformation of excess food intake into heat loss, should guarantee the body weight homeostasis, independently of the excessive intake.In over nourished rats an increment in thermogenesis has been documented, preventing the develop of obesity. Postprandial thermogenesis increases by 0.5–1 degree thanks to this BAT-mediated process, keeping the energy balance stable despite the caloric surplus. Many improvements such as increased body temperature, increased oxygen use and diminished insulin counter regulation have been proved after transplants of BAT in PCOS-suffering experimental models [Citation9].
Genetic features of insulin resistance in PCOS-suffering women
Several genetic alterations may modify insulin activity and beta cells secretory capacity in women with PCOS [Citation10]. summarizes the main genes involved in the different modulation of the metabolic asset in this category. Leptin-mediated signal and PPAR-gamma receptor function may be altered too (leptin is a hormone produced by the adipose tissue. inhibits the adipose tissue growth by lessening the appetite and lipogenesis and increasing the energy use and lipolysis. PPAR-gamma is a regulator of fatty acid deposits and glucose metabolism).
Table 3. Main genes involved in determining dysmetabolic PCOS.
Conclusion
Sedentary lifestyle and over nutrition may be accelerating causes for metabolic PCOS. Nevertheless, this may be subject to genetic mechanisms and hormonal features not often considered in clinical practice. The main task of endocrinologists, considering the multidisciplinary approach in this syndrome (metabolic, reproductive, esthetic disorders, and potential oncologic risks), is to evaluate each patient, according to their phenotype as early as possible, in order to guide them to a change in lifestyle, proper pharmacologic treatment and eventually to prevent the ever increasing lifetime cardiovascular risks bound to occur in these women ().
Rosita A. Condorelli, Aldo E. Calogero, Maurizio Di Mauro and Sandro La Vignera Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy [email protected]
Disclosure statement
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Cassar S, Misso ML, Hopkins WG, et al. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic-hyperinsulinaemic clamp studies. Hum Reprod 2016;31:2619–31.
- Gambineri A, Patton L, Altieri P, et al. Polycystic ovary syndrome is a risk factor for type 2 diabetes: results from a long-term prospective study. Diabetes 2012;61:2369–74.
- Escobar-Morreale HF, Roldàn-Martìn MB. Type 1 diabetes and polycystic ovary syndrome: systematic review and meta-analysis. Diabetes Care 2016;39:639–48.
- Vassilatou E. Nonalcoholic fatty liver disease and polycystic ovary syndrome. World J Gastroenterol 2014;20:8351–63.
- Wallace IR, McKinley MC, Bell PM, Hunter SJ. Sex Hormone binding globulin and insulin resistance. Clin Endocrinol (Oxf) 2013;78:321–9.
- Le TN, Nestler JE, Strauss JF III, Wickam EP III. Sex hormone-binding globulin and type 2 diabetes mellitus. Trends Endocrinol Metab 2012;23:32–40.
- Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev 1997;18:774–800.
- Malin S, Kirwan JP, Sia CL, Gonzàles F. Pancreatic β-cell dysfunction in polycystic ovary syndrome: role of hyperglycemia-induced nuclear factor-κB activation and systemic inflammation. Am J Physiol Endocrinol Metab 2015;308:E770–7.
- Yuan X, Hu T, Zhao H, et al. Brown adipose tissue transplantation ameliorates polycystic ovary syndrome. Proc Natl Acad Sci USA 2016;113:2708–13.
- Calogero AE, Calabrò V, Catanuso M, et al. Understanding polycystic ovarian syndrome pathogenesis: an updated of its genetic aspects. Endocrinol Invest 2011;34:630–44.