Abstract
Fertility awareness-based (FAB) methods represent a term that includes all family planning methods that are based on the identification of the fertile window. They are based on the woman’s observation of physiological signs of the fertile and infertile phases of the menstrual cycle. The first approach consists basically in symptothermal methods accompanied by cervical mucus measurements and clinical menstrual cycling data recording. The second most often used methods are the urinary measurement of E3G and luteinizing hormone (LH) with a personalized computer system. Hence these systems lack the efficacy of the continuous circadian and circamensual measurement of the core body temperature. Only this approach enables the accurate detection of the ovulation during the fertile window. A new medical device called OvulaRing has been developed to fill this gap. In the present study, the system and its first clinical results are presented. OvulaRing is a medical device used just like a tampon. The device is a vaginal ring of evatane that contains an integrated biosensor. This sensor measures continuously every 5 min the core body temperature throughout the entire cycle. This device allows a circadian and circamensual intravaginal exact measurement. With this system, 288 measurements are created per day. The system can detect retrospectively and predict prospectively the fertile window of the users. One hundred and fifty eight women aged between 18 and 45 years used this medical device in an open non-randomized clinical study for 15 months. A total of 470 cycles could be recorded and were able for analysis. By the same time in a subgroup of patients, hormonal assessments of LH, follicle-stimulating hormone, estradiol and progesterone as well as vaginal ultrasound were performed in parallel between the 9th and the 36th day of the cycle. The validation error due to software errors was 0.89% for the retrospective analysis; that means that the accuracy for the detection of the ovulation was 99.11%. Accuracy of 88.8% for a window of 3 days before ovulation, the day of ovulation and the 3 days after ovulation was achieved for the prospective analysis. In the subgroup of woman with recorded pregnancies, it could be shown that after 3.79 months of use (median) pregnancies were observed. In 67.72% in up to 3 months, in 16.36% between 3 and 6 months of use, in 7.27% between 7 and 9 months, in 5.45% between 10 and 12 months and in 1.82% between 13 and 15 months of use of the system. With this new web-based system, a precise determination of the fertile window even in women with ultralong cycles (>35 days) could be detected independently of their personal live circumstances. Exact determination of the fertile window is herewith possible so that OvulaRing represents an evolution in the FAB method for the cycle diagnosis of women with regular, irregular or anovulatory menstrual cycles.
Chinese abstract
基于自我生育意识的方法(FAB)是一个包含所有计划生育方法的术语。它们的基础是女性对月经周期中易受孕和不易受孕阶段的生理迹象的观察和确定。第一种方法主要是包括监测宫颈粘液变化和月经周期中临床数据记录。第二种最常用的方法是用个人计算机系统对尿液中的E3G和黄体生成素(LH)进行测量。因此, 这些方法都缺乏对体核体温的连续昼夜节律和周期性测量的功效。只有这种方式能够在生育窗口期间精确监测排卵。为了填补这个空白, 我们开发了一种名为OvulaRing的新型医疗设备。在本研究中, 该系统及其临床研究结果首次呈现。OvulaRing是一种像卫生棉条一样使用的医疗设备。该装置是含有一个集成生物传感器的阴道乙烯环。该传感器通过整个循环连续测量体核体温, 间隔时间为5分钟, 每天进行288次测量。可以进行昼夜生物节律和月经周期性的阴道内精确测量。该系统可以回顾性地监测以及预测用户的易受孕窗口。在一个开放性的非随机临床试验研究中, 158名18-45岁的妇女使用这种医疗器械共15个月。共记录470个月经周期并进行分析。与此同时, 在同一个亚组的患者中, 在月经周期的第9天和第36天之间同时检测LH, 促卵泡激素, 雌二醇和孕酮以及阴道超声。回顾性研究的系统偏差导致的错误为0.89%, 这意味着排卵监测的准确性是99.11%。排卵前3天窗口期的确定准确率为88.8%, 排卵日和排卵后3天窗口期通过前瞻性分析得到。在记录到怀孕的女性亚组中, 使用该系统至妊娠时间的中位数为3.79个月。其中, 使用达3个月者, 其妊娠率为67.72%, 使用3-6个月者妊娠率为16.36%, 7-9个月者妊娠率为7.27%, 10-12个月者妊娠率5.45%, 13-15个月的妊娠率为1.82%。有了这个新的基于网络的系统, 甚至在超长月经周期(> 35天)的女性中, 无需注意个人的生活环境, 也可以精确确定易受孕窗口。因此, 在具有规律或不规律甚至无排卵的月经周期的女性中, OvulaRing作为FAB方法的进化, 用于精确确定易受孕生育窗口是可行的。
Introduction
Fertility awareness-based (FAB) methods is a term that includes all family planning methods that are based on the identification of the fertile time. They are based on the woman’s observation of physiological signs of the fertile and infertile phases of the menstrual cycle. This knowledge can be used to plan or avoid pregnancy. FAB methods depend on two key variables: first, the accurate identification of the fertile days of a woman’s menstrual cycle (the fertile time) and second, the modification of sexual behavior either to plan a pregnancy or to use this knowledge to avoid pregnancy. When couples use FAB methods of family planning to avoid pregnancy, they practice different sexual behavior during the fertile time. When FAB methods involve sexual abstinence during the fertile time, this method is called natural family planning (NFP). When FAB methods involve occasionally using a barrier method during the fertile time, the method is called FAB method with barriers. It must also be recognized that although many couples state they are practicing a FAB method, sometimes they do not adhere to the guidelines and unprotected intercourse or other kinds of genital contact occur during the fertile time. Since the first descriptions of FAB by Pryll [Citation1], the efficacy of FAB methods to avoid pregnancy has been critically reviewed by several authors [Citation2–9]. Several issues have been identified when attempting to compare the different FAB methods.
The first is that most FAB methods have evolved concurrently over the last 40 years in different countries; each has been led by pioneers who have developed guidelines for their respective groups. This has resulted in many cases in a lack of evidence-based guidelines being developed and subsequently modified to conform to best scientific evidence.
The second issue is that efficacy rates may vary because they are derived from studies done with volunteers and researchers from different cultural backgrounds where motivation to avoid pregnancy and rigor of research methods may vary [Citation10–12]. To be able to make an informed choice when selecting a family planning method, couples need to know the efficacy of a method when used consistently and imperfectly. Trussell and Grummer-Strawn [Citation13,Citation14] are critical about how efficacy has been calculated in previous studies. They argue that previously published rates of method and user failure for all contraceptive methods suffer from methodological errors and are biased downwards. Trussell and Grummer-Strawn [Citation13,Citation14] recommend a new model of calculating perfect and imperfect use pregnancy rates which up to now has rarely been applied. This is likely to be due to the fact that this approach requires documentation of all sexual behavior during each cycle. Frank Herrmann et al. [Citation15] described a cohort of couples who used a method that consisted of recording the cervical secretion pattern, changes of basal body temperature and the application of a calculation rule. It is called the symptothermal method (STM) of NFP. The beginning and the end of the fertile time are identified by two parameters in order to have double-check system.
The following two guidelines are given to each couple to identify the first fertile day–both guidelines are applied and the first fertile day is the earliest day identified:
Change of cervical secretion: first appearance of cervical secretion.
Calculation guideline: the first fertile day is the sixth day of the cycle (In NFP methodology, this is called the ‘5 days rule’ which states that the first 5 days of the cycle are infertile days.) or after a woman has completed 12 cycles of use this guideline is replaced by a calculation that takes the earliest temperature rise in the last 12 cycles and subtracts 7 days to identify the first fertile day (In NFP methodology, this is called the ‘minus eight rule’: earliest temperature rise in the last 12 cycles minus 8 days to identify the last infertile day.)
But independent of these existing methods, it is known that during the average woman’s menstrual cycle, there are 6 days when intercourse can result in pregnancy; this ‘fertile window’ comprises the 5 days before ovulation and the day of ovulation itself [Citation16–18]. Just as the day of ovulation varies from cycle to cycle so does the timing of the six fertile days. Reliable methods to predict ovulation are lacking, therefore predicting the fertile window is also unreliable. Clinical guidelines suggest the cycle days during which the fertile window is most likely to occur, but these guidelines are outdated. Wilcox et al. [Citation19] provided in a cohort of more than 200 women new estimates based on a prospective study. In only ∼30% of women is the fertile window entirely within the days of the menstrual cycle identified by clinical guidelines—that is, between Days 10 and 17. Most women reach their fertile window earlier and others much later. Women should be advised that the timing of their fertile window can be highly unpredictable, even if their cycles are usually regular.
Another approach for determining the exact window of fertility is the hormonal one. Researchers have used a variety of approaches in an attempt to measure hormone levels in a meaningful way given the inherent variability of these markers. Nevertheless, many studies rely on a single serum sample drawn on an arbitrary day of each woman’s menstrual cycle, which seems inadequate, even with adjustment for cycle day or for cycle phase status (determined by the sample’s progesterone level) [Citation20–22]. Other studies have attempted to time specimen collection to key hormonal events based on self-reported cycle length or cycle day or the assumption that the luteal phase is 14 days [Citation23–25], but these methods assume that women can reliably report their cycle length or that the timing of hormonal fluctuations is the same across women, both of which are unlikely to be true [Citation26–30]. The ‘gold standard’ is daily collection of first-morning urine specimens, which ensures that critical hormone windows are captured if compliance is adequate, but the protocol is burdensome, which affects recruitment and compliance. Ideally, it would be possible to characterize hormone levels across the menstrual cycle by collecting fewer, well-timed measurements, but it is unclear what algorithm should be applied to prospectively assess when the samples should be collected. So, luteinizing hormone (LH) measuring systems have been developed to close this gap [Citation31]. But these participants that were provided with home fertility monitors that measured urinary estrone-3-glucuronide and LH had monitor recording data that showed a surge during 76% of the first cycles and 78% of the second cycles [Citation31].
Therefore, new and more accurate systems have to be developed. In this article, we present a new concept for improving the accuracy in the detection of the fertile window of women.
A medical device called OvulaRing has been developed and first clinical data have been obtained that demonstrate the evolution in this segment of fertility monitoring.
Material and methods
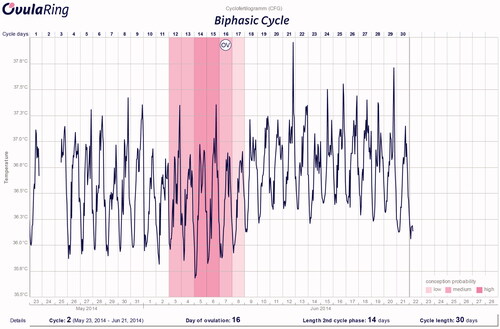
OvulaRing is a medical device used just like a tampon. The device is a vaginal ring of evatane that contains an integrated biosensor. This sensor measures continuously every 5 min the core body temperature throughout the entire cycle. This device allows a circadian and circamensual intravaginal exact measurement. With this system, 288 measurements are created per day. With a reading device and a mobile software, the data are transferred to a central database and evaluated. With the use of mathematical algorithmic, these data are evaluated and a prediction model is assessed. The system is able to predict retrospectively and prospectively the fertile window of the users. Three recorded cycles from which two have to be ovulatory are needed to obtain the accurate data of this new technology in the prospective data evaluation.
One hundred and fifty eight women aged between 18 and 45 years used this medical device in an open non-randomized clinical study for 15 months. The body mass index (BMI) of these women ranged between 18.2 and 36.9 with a median of 22.2. A total of 470 cycles could be recorded and were able for analysis. By the same time in a subgroup of patients hormonal assessments of LH, follicle-stimulating hormone, estradiol and progesterone were performed in parallel between the 9th and the 36th day of the cycle using commercially available ELISA assays.
All the data were expressed in form of a cyclofertilogram (CFG). This is the graphical representation of the obtained circadian and circamensual data or the continuous 5-min measurement.
A subgroup of women was specifically evaluated in regard to the rate of intended pregnancies with the use of this tracking system. Sixty-two women were retrospectively randomized for the analyses. Of these women, data were obtained from 55 and the time use of the system till achieving a pregnancy was evaluated.
The present clinical trials were approved by the ethical committees of the University of Dresden, Germany (EK270072013) and the University of Leipzig, Germany (EK-MPK-MO-1/12–1).
Results
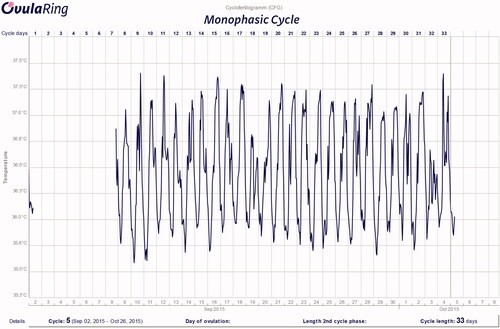
From the recorded 470 cycles, 83.4% were biphasic cycles. The shortest biphasic cycle had a length of 20 days and the longest of 58 days ( depicts a CFG of an ultralong ovulatory biphasic cycle). Of the cycles, 8.8% showed are reduced corpus luteum phase (<12 days) and 16.6% of the cycles were monophasic or even anovulatory (). The shortest monophasic cycle had a length of 20 days and the longest of 77 days. Of the anovulatory cycles, 10.1% had a length of >50 days.
Figure 1. CFG of a patient with a PCOS. Ovulation occured at Day 47. This CFG shows a pregnancy as the core body temperature remains high.
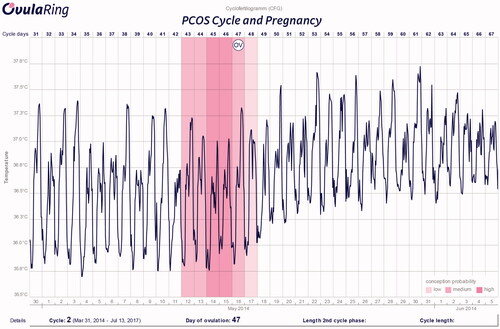
It could be shown that 69.5% of the women had an ovulation after the 15th day (54.9%) of the menstrual cycle or before the 13th day (14.6%). In 17.3% of the cycles, ovulation was detected at Day 20 or later of the menstrual cycle
In fifteen percent of the women with cycles ≥35 days, a PCOS syndrome was diagnosed with ovulations even after the 36th day of the cycle. Of these women, 4.5% showed ovulations after Day 26 of the cycle.
The median body core temperature was in all monophasic cycles 36.6 °C and 36.7 °C in the biphasic cycles.
The interindividual changes of ovulation showed a median average of 3 days.
Using this fertility awareness system, the validation error for the retrospective analysis was 3.69%; that means that the accuracy of the detection of the ovulation was 96.31%. Only 0.89% of the validation errors were due to software errors and the remaining 2.8% were due to compliance errors of the users. Excluding users errors the exact determination of ovulation was 99.11%.
In regard to the efficacy to predict the window of opportunity after three measured ovulatory cycles this was the following: accuracy of 88.8% for a window of 3 days before ovulation, the day of ovulation and the 3 days after ovulation.
In the subgroup of woman with recorded pregnancies, it could be shown that after 3.79 months of use (median) pregnancies were observed. In 67.72% in up to 3 months, in 16.36% between 3 and 6 months of use, in 7.27% between 7 and 9 months, in 5.45% between 10 and 12 months and in 1.82% between 13 and 15 months of use of the system ( depicts a CFG with ovulation).
Discussion
In one of the first reviews ever published to specify the fertile window by Pryll (1916) [Citation1], a high amount of pregnancies occurred during the Days 6–11 of the menstrual cycles that were recorded. Even if his analyses were not intended to define a fertile window, it shows retrospectively the high variation in the accuracy of this item especially taking into consideration that he described the follicular ovulation days of Schröder (Days 14, 15 and 16) and the follicular ovulation day after Fränkel (Day 20). These data suggest that the follicular phase of those recorded women must have been shorter than expected [Citation1]. Many effects have been taken since then to define with more accuracy the fertile window of the menstrual cycle.
Modern methods available on the market are based on symptotermal systems using the clinical data of menstruation, the single-morning wake-up measuring of the body temperature and the observation of the consistency of the cervical mucus [Citation15] or on the determination of hormones in the urine of women. Here, the combination of LH and E3G and also the clinical data of menstruation are used to define the window of fertility [Citation32]. But as shown by Direito et al. [Citation32], the interindividual variability of ovulation detected by ultrasound and LH surge ranged from −6 to +5 days demonstrating that also these measuring systems are not able to define precisely the individual characteristics of the female cycles.
The development of a device that measures constantly every 5 min the body core temperature represents therefore an evolution in the accuracy of the determination of the cycle characteristics and the window of fertility. As a continuous circadian and circamensual measurement is performed, a fast and exact awareness of temperature can be achieved. The fact that the rise in the body core temperature occurs not during the supposed time of the morning wake up but in the early night time, so that the accuracy of the main parameter in symptotermal systems is enhanced.
As the rise of the temperature occurs not only after the surge of progesterone [Citation33] and the lowest core temperature is associated with the peak of E3G [Citation32] and as E3G, LH surge and progesterone are not always associated with an exact prediction of the ovulation day [Citation32], the fertile window detection remains complicated.
We could show with our new development that, using a consumer-friendly system that doesn’t require urinary sample collection and allows a free daily behavior of the users and is applicable for women with continuous changing working and sleeping times, a precise ovulation day determination of 96.5% in retrospective cycles and in 88.5% in prospective cycles with a window of 7 days could be described.
This will help women in their realization of conception as they will improve their own knowledge of the fertile window.
Disclosure statement
Prof. Dr. P.-A. is Medical Director of Exeltis West Europe & Germany.
References
- Pryll W. Kohabitationstermin und Kindsgeschlecht. Muenchner Medizinische Wochenschrift 1916;45:1579–82.
- Frank-Herrmann P, Freundl G, Baur S, et al. Effectiveness and acceptability of the symptothermal method of natural family planning in Germany. Am J Obstet Gynecol 1991;165:2052–4.
- De Leizaola-Cordonnier A. Natural family planning effectiveness in Belgium. Adv Contracept 1995;11:165–72.
- Barbato M, Bertolotti G. Natural Methods for fertility control: a prospective study. Int J Fertil Suppl 1988;33:48–51.
- Hilgers TW, Stanford JB. Creighton Model NaProEducation Technology for avoiding pregnancy. Use effectiveness. J Reprod Med 1998;43:495–502.
- Howard MP, Stanford JB. Pregnancy probabilities during use of the Creighton model fertility care system. Arch Fam Med 1999;8:391–402.
- Kambic RT, Girotto S, Bressan F. The effectiveness of natural family planning methods for birth spacing: a comprehensive review. In: Girotto S, Bressan F, eds. Human fertility regulation: demographic and statistical aspects. Verona: Edizioni Libreria Cortina; 1999:63–90.
- Tietze C, Lewit S. Statistical evaluation of contraceptive methods. Clin Obstet Gynecol 1974;17:121–38.
- Grimes DA, Gallo MF, Grigorieva V, Nanda K, Schulz KF. Fertility awareness-based methods for contraception. Cochrane Database Syst Rev 2004;18:CD004860.
- World Health Organization. A prospective multicentre trial of the ovulation method of natural family planning. I. The teaching phase. Fertil Steril 1981;36:152–8.
- Xu JX, Yan JH, Fan DZ, Zhang DW. Billings natural family planning in Shanghai, China. Adv Contracept 1994;10:195–204.
- Indian Council of Medical Research Task Force on Natural Family Planning. Field trial of billings ovulation method of natural family planning. Contraception 1996;53:69–74.
- Trussell J, Grummer-Strawn L. Contraceptive failure of the ovulation method of periodic abstinence. Fam Plann Perspect 1990;22:65–75.
- Trussell J, Grummer-Strawn L. Further analysis of contraceptive failure of the ovulation method. Am J Obstet Gynecol 1991;165:2054–60.
- Frank-Herrmann P, Heil J, Gnoth C, et al. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple’s sexual behaviour during the fertile time: a prospective longitudinal study. Hum Reprod 2007;22:1310–19.
- Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation: effects on the probability of conception, survival of the pregnancy and sex of the baby. N Engl J Med 1995;333:517–21.
- Wilcox AJ, Weinberg CR, Baird DD. Post-ovulatory ageing of the human oocyte and embryo failure. Hum Reprod 1998;13:394–7.
- Dunson DB, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod 1999;14:1835–9.
- Wilcox AJ, Dunson D, Baird DD. The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. BMJ 2000;18:1259–62.
- Rosenberg CR, Pasternack BS, Shore RE, et al. Premenopausal estradiol levels and the risk of breast cancer: a new method of controlling for day of the menstrual cycle. Am J Epidemiol 1994;140:518–25.
- Yu H, Shu XO, Shi R, et al. Plasma sex steroid hormones and breast cancer risk in Chinese women. Int J Cancer 2003;105:92–7.
- Potischman N, Hoover RN, Brinton LA, et al. Case-control study of endogenous steroid hormones and endometrial cancer. J Natl Cancer Inst 1996;88:1127–35.
- Ahmad N, Pollard TM, Unwin N. The optimal timing of blood collection during the menstrual cycle for the assessment of endogenous sex hormones: can interindividual differences in levels over the whole cycle be assessed on a single day? Cancer Epidemiol Biomarkers Prev 2002;11:147–51.
- Tworoger SS, Sluss P, Hankinson SE. Association between plasma prolactin concentrations and risk of breast cancer among predominately premenopausal women. Cancer Res 2006;66:2476–82.
- Sarwar R, Niclos BB, Rutherford OM. Changes in muscle strength, relaxation rate and fatiguability during the human menstrual cycle. J Physiol 1996;493:267–72.
- Harlow SD, Ephross SA. Epidemiology of menstruation and its relevance to women’s health. Epidemiol Rev 1995;17:265–86.
- Fehring RJ, Schneider M, Raviele K. Variability in the phases of the menstrual cycle. J Obstet Gynecol Neonatal Nurs 2006;35:376–84.
- Small CM, Manatunga AK, Marcus M. Validity of self-reported menstrual cycle length. Ann Epidemiol 2007;17:163–70.
- Windham GC, Elkin E, Fenster L, et al. Ovarian hormones in premenopausal women: variation by demographic, reproductive and menstrual cycle characteristics. Epidemiology 2002;13:675–84.
- Jukic AM, Weinberg CR, Wilcox AJ, et al. Accuracy of reporting of menstrual cycle length. Am J Epidemiol 2008;167:25–33.
- Howards PP, Schisterman EF, Wactawski-Wende J, et al. Timing clinic visits to phases of the menstrual cycle by using a fertility monitor: the BioCycle study. Am J Epidemiol 2009;169:105–12.
- Direito A, Bailly S, Mariani A, Ecochard R. Relationships between the luteinizing hormone surge and other characteristics of the menstrual cycle in normally ovulating women. Fertl Steril 2013;99:279–85.
- Coyne MD, Kesick CM, Doherty TJ, et al. Circadian rhytm changes in core temperature over menstrual cycle: methods for noninvasive monitoring. Am J Physiol Regul Integr Comp Physiol 2000;279:316–20.