Abstract
The aim of this study is to evaluate the outcomes of single embryo transfer in patients with good ovarian reserve in the IVF program using time-lapse microscopy. This is a retrospective cohort study in a private IVF center in Russia. Comparison was done between 90 IVF cycles using time-lapse (study group) and 113 IVF cycles using standard culture (control group). Within each group, subgroups were selected with selective transfer of one embryo for 5 days (5SET) and elective transfer of one embryo for 5 days (5eSET). The primary outcome of the study was pregnancy rate. Secondary outcomes were miscarriage rates, live birth. Pregnancy rate did not significantly differ between the groups – 64.2% in the study group and control group. In the study group, the delivery rate was 54% in the subgroup 5eSET and 51.1% in the subgroup 5SET (p = .940). In the control group, the type of the embryo transfer significantly influenced on the delivery rate: in the 5eSET subgroup the birth rate was 54.4%, and in the 5SET subgroup it was 34.3% (p = .055; by Fisher's exact method p = .052). There were no adverse effects of the intervention. Selection of a single blastocyst based on information derived from time-lapse monitoring can help embryo selection for transfer.
Introduction
Since the onset of IVF, the morphological assessment of human embryos has been the main method used by embryologists to assess the development and selection of embryos for transfer. Historically, a daily assessment of the development of embryos at specific points in time has been used to solve this problem. But removal of the embryo from the incubator for evaluation can provide information only about the ‘momentary’ state of the embryo from the entire highly dynamic period of preimplantation development.
Despite the success of modern ART, about 70–80% of the initiated cycles do not lead to pregnancy, which is mainly due to implantation problems. Classical morphological assessment of developing embryos in vitro is not enough. Through the use of time lapse microscopy (TLM) it is possible to increase the pregnancy rate [Citation1].
The use of continuous embryo monitoring through TLM is a modern method for selecting an embryo for transfer. With the introduction of microscopy with a time interval, we have entered a new era of embryology, thanks to which we can evaluate the morphology of embryos as a continuum, with image fixation every few minutes [Citation2].
The combining selection based on morphological factors with metabolic, protein, and genetic markers in culture media may increase pregnancy and live birth rates and become the standard of selecting embryos with the highest implantation potential [Citation3].
Currently, conflicting data have been obtained on the results of using TLM. The retrospective study indicated that embryo culture in the EmbryoScope incubator may improve live birth rates, and that conventional culture methods may negatively impact embryo growth and implantation potential [Citation4].
Several randomized controlled trials are under way to evaluate the benefits of using TLM. Current retrospective and prospective studies underline the utility of this technology in a clinical setting with promising results [Citation5–8].
Thanks to the creation of algorithms based on neural networks, embryos can be ranked 5–6 days of development depending on their implantation perspective, which will establish a direct correlation with the frequency of procreation [Citation9]. This will significantly reduce the time before pregnancy and childbirth, and also allow avoiding unnecessary embryo transfer procedures, which is accompanied by a waste of economic, time and psychological resources.
Objective: To evaluate the outcome of single embryo transfer in patients with good ovarian reserve in the IVF program using time-lapse microscopy.
Materials and methods
The study included 208 women with infertility, with a good ovarian reserve (getting ≥8 oocytes for retrieval) which transferred one embryo on the fifth day of culture in the IVF program during 2013–2015. The study group consisted of 95 patients with single embryo transfer in the IVF program using time-lapse microscopy system. The control group consisted of 113 patients with a single embryo transfer in the IVF program using traditional culture and selection of an embryo for transfer.
The embryological stage of the IVF program was carried out in a study group using a video system for the development of the embryos Primovision (Vitrolife, Gothenburg, Sweden). The transfer of the embryos was carried out on the basis of their compliance with key morphodynamic parameters and reference values of the system. The evaluation system developed by Gardner in 1999 was used in the control group to assess the quality of embryos.
In the both groups, cultivation was carried out using a universal medium continuous single culture (Irvine Scientific, Santa Ana, CA).
Results
The pregnancy rate, birthrate, and pregnancy loss were evaluated in the comparison groups. Within each group, two subgroups were selected: with one selective 5 days embryo transfer (subgroup 5SET) and elective transfer of one embryo for 5 days (subgroup 5eSET).
The groups did not statistically differ due to the causes of infertility, the infertility duration and the ordinal number of this IVF program.
The average women age in the study group and in the control group was 31.40 ± 0.38 and 30.65 ± 0.37 years, respectively (p>.05). The average number of oocytes retrieval in the study group and in the control group was 11.87 ± 0.32 and 12.49 ± 0.40, respectively (p>.05). The average number of zygotes also did not differ between the study and control groups (8.62 ± 0.33 and 8.66 ± 0.34, respectively (p>.05)). As the main outcome of embryo transfer in the IVF program is the live birth, we have analyzed all the outcomes of embryo transfer in the IVF program – absence of pregnancy, loss of pregnancy at the different times and delivery.
As shown from , the clinical pregnancy rate in the IVF program did not differ between the two groups and was 64.2% in the study group and 60.2% in the control group (p = .65). There were no cases of multiple pregnancies in both groups.
Table 1. Embryo transfer outcomes in the patients of the study group and the control group.
Among all embryo transfer outcomes, the proportion of the births was 52.6% in the study group and 42.5% in the control group (p>.05). The term delivery rate was 51.6% in the study group and 41.6% in the control group (p>.05). In one case in the each group, the delivery ended prematurely (1.1% in the study group and 0.9% in the control group). The rate of all cases of the early pregnancy loss (biochemical pregnancies and losses up to 12 weeks of gestation) in the study group was 11.6%, in the control group 17.7%, although the difference was no significant.
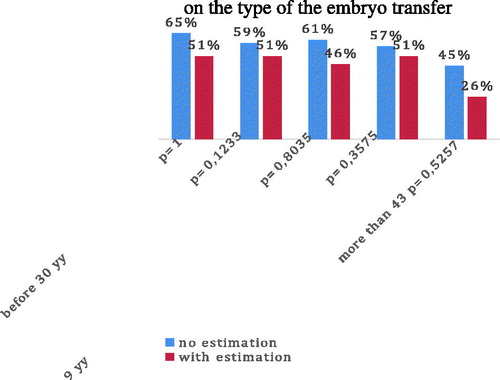
According to the literature, an elective embryo transfer increases the likelihood of the favorable transfer outcomes [Citation10], a comparative analysis was conducted of the pregnancy rate and the delivery rate depending on the type of the transfer ().
Table 2. Pregnancy rate depending on the type of embryo transfer.
In the study group, the clinical pregnancy rate was 68% with elective embryo transfer (5eSET subgroup) and 60% with non-elective transfer (5SET subgroup) (p = .550), in the control group 71.7% and 52.2%, respectively (p = .059; by Fisher's exact method p = .050).
Thus, in the study group, the clinical pregnancy rate was high regardless of the variant of embryo transfer, while in the control group there was a clear advantage in the elective transfer of the embryos.
As shown from , in the study group, the delivery rate was 54% in the subgroup 5eSET and 51.1% in the subgroup 5SET (p = .94). In the control group, the type of the embryo transfer significantly influenced on the delivery rate: in the 5eSET subgroup, the birth rate was 54.4%, and in the 5SET subgroup, it was 34.3% (p = .055; by Fisher's exact method p = .052).
Table 3. Delivery rate depending on the type of embryo transfer.
Thus, among women using time-lapse microscopy, regardless of the type of embryo transfer, the delivery rate was high (54.0% and 51.1%) and not differ ().
Discussion and conclusions
Current publications contain conflicting data on the effect of TLM on the outcomes of the IVF program.
We obtained high clinical pregnancy rate in the both groups of our study (64.2% study group and 60.2% control group), which may indicate the absence of a negative impact on the embryos culture using the continuous monitoring system. The use of time-lapse microscopy showed an advantage in the reducing the early pregnancies loss rate, although the difference was no significant.
In our study, the use of TLM gave a higher clinical pregnancy rate, and delivery rate in the non-elective transfer subgroup. The absence of the statistical significance connected with the lack of the power of the criterion due to the small sample size. However, the difference in the delivery rate is 20% (95% CI: 1.5–37%) with OR = 2.28 (95% CI: 1.06–4.91), depending on the type embryo transfer, undoubtedly deserves attention and clinical judgment.
The technology of using TL microscopy minimizes the contact of the embryo with the external environment, which may be one of the factors leading to the formation of embryos with a higher implantation potential.
Continuous monitoring of embryos with time-lapse provides more information on embryo kinetics and morphology compared to standard daily evaluation.
There is no doubt that in the future the complex systems (morphology, dynamics, and metabolomics) will be created for noninvasive assessment of the embryo quality, which will automate the process of selecting one embryo for transfer. This will reduce the likelihood of human and environmental factors and, as a result, to increase the birthrate on embryo transfer.
The use of time-lapse microscopy can reduce the negative impact of environmental factors, increasing the quality of embryos on transfer. As a result, differences in the incidence of pregnancy and delivery in the subgroups of elective and selective embryo transfer were not reliably detected.
Early pregnancy loss in the groups was not statistically different. Thus, further accumulation of factual material is necessary for analyzing such indicators as the cumulative pregnancy rate in ART cycles using a video surveillance system, as well as monitoring the remote consequences of using this technology.
Disclosure statement
None of the authors report any conflict of interest with this research.
References
- Meseguer М, Rubio I, Cruz M, et al. Embryo incubation and selection in a time-lapse monitoring system improves pregnancy outcome compared with a standard incubator: a retrospective cohort study. Fertil Steril. 2012;98:1481–1489.e10.
- Meseguer M. Time-lapse: the remaining questions to be answered. Fertil Steril. 2016;105:295–296.
- Wang SX. The past, present, and future of embryo selection in in vitro fertilization: frontiers in reproduction conference. Yale J Biol Med. 2011;84:487–490.
- McEvoy K, Brison D, Roberts SA. One year retrospective analysis comparing live birth outcomes from embryos grown and transferred from an undisturbed time-lapse culture system with a conventional culture system. Presented at: 32nd Annual Meeting of the European Society of Human Reproduction and Embryology; 2016 Jul 3–6; Helsinki, Finland.
- Adamson GD, Abusief ME, Palao L, et al. Improved implantation rates of day 3 embryo transfers with the use of an automated time-lapse-enabled test to aid in embryo selection. Fertil Steril. 2016;105:369–375.
- Diamond MP, Suraj V, Behnke EJ, et al. Using the Eeva Test™ adjunctively to traditional day 3 morphology is informative for consistent embryo assessment within a panel of embryologists with diverse experience. J Assist Reprod Genet. 2015;32:61–68.
- Rubio I, Galán A, Larreategui Z, et al. Clinical validation of embryo culture and selection by morphokinetic analysis: a randomized, controlled trial of the EmbryoScope. Fertil Steril. 2014;102:1287–1294.
- Yang Z, Zhang J, Salem SA, et al. Selection of competent blastocysts for transfer by combining time-lapse monitoring and array CGH testing for patients undergoing preimplantation genetic screening: a prospective study with sibling oocytes. BMC Med Genomics. 2014;7:38.
- Fishel S, Campbell A, Montgomery S, et al. Time-lapse imaging algorithms rank human preimplantation embryos according to the probability of live birth. Reprod Biomed Online. 2018;37:304–313.
- Lee AM, Connell John MT, Csokmay JM, et al. Elective single embryo transfer – the power of one. Contracept Reprod Med. 2016;1:11.