Abstract
Steroid cell tumors not otherwise specified are rare sex cord-stromal tumors of the ovary that may produce various steroids and are associated with hirsutism and virilization. We report a rare case of ovarian steroid cell tumor with subsequent spontaneous pregnancy after tumor removal. A 31-year-old woman presented with secondary amenorrhea, hirsutism, and inability to conceive. Clinical and diagnostic evaluations revealed a left adnexal mass and elevated serum total testosterone and 17α-hydroxyprogesterone levels. She underwent a left salpingo-oophorectomy, and histopathological examination confirmed the diagnosis of a steroid cell tumor not otherwise specified. Her serum total testosterone and 17α-hydroxyprogesterone normalized one month after surgery. Her menses resumed spontaneously one month after the operation. She spontaneously conceived 12 months after the surgery. The patient had an uncomplicated pregnancy and delivered a healthy male infant. In addition, we reviewed the literature on steroid cell tumors not otherwise specified with subsequent spontaneous pregnancies after surgery and data regarding pregnancy outcomes.
Introduction
Steroid cell tumors of the ovary are classified as sex cord stromal tumors and have been categorized into three subtypes: stromal luteoma, Leydig cell tumors, and not otherwise specified (NOS). Steroid cell tumor NOS is the most common subtype and usually develops in reproductive-aged women, with an average age of 43 years. The major presenting symptoms of steroid cell tumor NOS are hirsutism and virilization caused by high levels of sex hormones. Surgical management is an appropriate treatment for ovarian steroid cell tumors [Citation1]. There has been limited data on ovarian steroid cell tumor NOS regarding fertility outcomes after surgery. To the best of our knowledge, only two cases of spontaneously conceived pregnancies with good outcomes have been reported [Citation2,Citation3].
This report describes a case of steroid cell tumor NOS in a reproductive-aged woman with elevated total serum testosterone and 17α-hydroxyprogesterone (17-OHP). After the surgical removal of the ovarian tumor, the patient conceived and delivered a healthy baby without complications. This study was approved by the Institutional Review Board of the Faculty of Medicine at the Prince of Songkla University (approval number: REC. 65-363-12-1). Patient approval for publication was obtained.
Case report
A 31-year-old woman was referred to the reproductive endocrinology clinic because of secondary amenorrhea for two years and a one-year history of hirsutism. She had normal childhood development and a normal sexual life for 10 years, without other medical problems. She had menarche at age 16, and regular menses lasting 3–4 days had occurred every 30 days since then. She had oligomenorrhea four years prior to the development of amenorrhea. She reported that excess hair had started at age 30, with progressive aggravation for several months, requiring weekly chin and daily upper lip shaving. She also reported hair loss for four months. She had never had a pregnancy. She denied taking any medication. She had two older sisters, and none had the same symptoms as the patient. The patient’s family history was negative for any type of cancer or infertility.
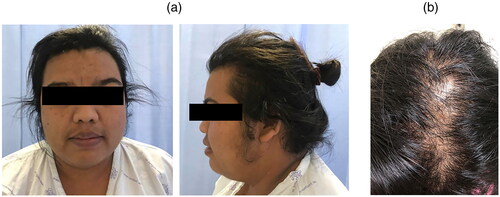
Physical examination revealed an obese female with a body mass index of 35.6 kg/m2 and normal blood pressure (BP 128/66 mmHg). Significant findings included temporal and parietal hair recession and male-pattern baldness (). Excessive coarse hair was present on her upper lip, chin, upper and lower abdomen and back, and inner thigh, giving a score of 16 according to the modified Ferriman–Gallwey scoring system. She also had acanthosis nigricans in the posterior neck and armpit. Acne, deepening voice, and other clinical features of Cushing’s syndrome were absent. Abdominal examination revealed no palpable mass. Genital examination revealed female external genitalia with a clitoris sized 1.0 cm in diameter and 1.2 cm in length.
Figure 1. Findings of virilization. (a) Hirsutism of face. (b) Male-pattern baldness (with permission from the patient).
Laboratory testing demonstrated a significant elevation in serum total testosterone (20.7 ng/mL) and 17α-hydroxyprogesterone (17-OHP) (10.9 ng/mL). Early morning cortisol, estradiol, follicle-stimulating hormone, luteinizing hormone, thyroid-stimulating hormone, and prolactin levels were within normal limits (). Pelvic ultrasound showed a left ovarian hyperechoic mass measuring 5 × 5 cm. Computed tomography (CT) of the whole abdomen revealed the absence of an adrenal mass and the left ovary was 7.8 × 5.2 × 4.8 cm with a contained 5.8 × 4.7 × 4.5-cm well-defined enhancing fatty mass without calcification, no lymph node enlargement, and no intraabdominal ascites ().
Figure 2. (a) Ultrasonographic appearance of left ovarian hyperechoic mass sized 5 × 5 cm. (b) Computed tomography of abdomen shows an enhancing lesion (7.8 × 5.2 × 4.8 cm) with contained 5.8 × 4.7 × 4.5-cm well-defined enhancing fatty mass without calcification likely arising from the left ovary (arrow).
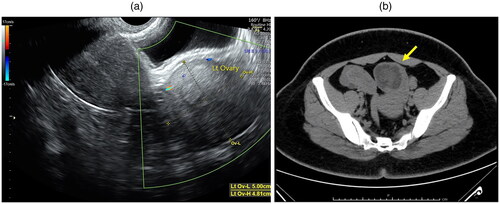
Table 1. Body weight and laboratory results before and after surgery.
Exploratory laparotomy was performed instead of a laparoscopic approach because malignancy could not be excluded. Intraoperatively, an enlarged left ovary measuring 6 × 6 cm was observed, and the right ovary had a polycystic ovary-like appearance. Exploration of the liver, spleen, and omentum was normal. No ascites or lymph node enlargement were observed. The left salpingo-oophorectomy was performed.
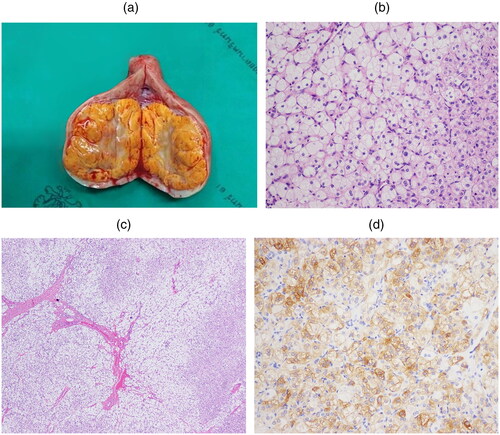
Pathological examination of the surgical specimen revealed a well-circumscribed left ovarian mass measuring 6 × 6 × 6 cm. The cut section of the specimen exhibited a lobulated and yellowish color (). Histological findings revealed large polygonal tumor cells with abundant granular eosinophilic cytoplasm, round nucleoli, and a prominent central nucleolus (). Tumor cells were arranged in a diffuse pattern separated by fibrous septa, without nuclear atypia or mitotic figures, and no Reinke crystals were identified (). The cells were negative for mucin, periodic acid-Schiff, and periodic acid-Schiff diastase. Immunohistochemistry findings showed that the cells were positive for inhibin () but negative for AE1/AE3 and cluster of differentiation 68. These findings are consistent with those of steroid cell tumors.
Figure 3. (a) Cross-sectional appearance of the left ovary. The ovarian tumor cut surfaces are well-circumscribed, yellowish color, and lobulated. (b) Tumor cells have round to polygonal shape with eosinophilic to clear cytoplasm and oval nucleus. (c) Tumor cells arrange in cord and sheet (*) with fibrovascular tissue (arrow). (d) Tumor cells show positive for alpha-inhibin immunostaining.
Her hormonal testing 4 weeks after surgery showed total testosterone and 17-OHP were reduced to 0.48 ng/mL and 1.54 ng/mL, respectively (). Her regular menstruation resumed one month after the surgery. Her hirsutism and alopecia also improved, and she lost approximately 18 kg of weight within 5 months after surgery. She spontaneously conceived 12 months after the surgery. She had an uncomplicated pregnancy and delivered a healthy male infant weighing 3,495 g at 38 weeks of gestation.
Discussion
Androgen-producing tumors are a rare cause of hyperandrogenism in women, accounting for approximately 0.2% [Citation4], and should be considered when serum total testosterone levels are above 150 ng/dL [Citation5,Citation6]. The major presenting symptoms of androgen-producing tumors are rapid-onset and progressive severe hyperandrogenisms, such as clitoromegaly, male-pattern hair loss, and voice deepening. In this patient, the presence of clitoromegaly, progressive hyperandrogenism, and significantly high serum total testosterone levels led us to consider the possibility of an androgen-producing tumor. Transvaginal ultrasound and CT were performed and revealed an enlarged left ovarian tumor without an adrenal mass. An androgen-secreting ovarian tumor was diagnosed and treated with salpingo-oophorectomy.
The patient was diagnosed with a steroid cell tumor NOS of the ovary. These tumors can occur between the ages of 3 and 93 years, with an average age of 43 years. Most tumors are unilateral, with only 6% of patients being found to be bilateral. Three-fourths of steroid cell tumor NOS can secrete a variety of hormones, including testosterone, estradiol, cortisol, and infrequently prorenin [Citation1]. Most of these tumors secrete testosterone, which causes hirsutism or virilization accounting for 56–77% of cases [Citation1,Citation7]. Approximately 6–23% secrete estrogen, which is associated with abnormal uterine bleeding or postmenopausal bleeding [Citation1,Citation7]. In addition, endometrial adenocarcinoma has been reported in women with ovarian tumors [Citation8], and 6–10% of cases are associated with Cushing’s syndrome [Citation9,Citation10]. Rarely, hypertension and hypokalemia can also be unique presentations in cases of elevated serum prorenin levels from ovarian steroid cell tumors [Citation11].
Surgery is an appropriate treatment for ovarian steroid cell tumors. The operative procedure should be individualized based on age, surgical stage, tumor histopathology, and the desire for fertility. In young patients who wish to preserve fertility, unilateral salpingo-oophorectomy is the preferred choice of treatment for stage IA tumors similar to other rare types of ovarian cancer such as ovarian germ cell tumors [Citation12]. However, older females who do not wish to conceive should undergo total abdominal hysterectomy with bilateral salpingo-oophorectomy and complete surgical staging. Adjuvant chemotherapy should be considered if the histological examination of the tumor is malignant. However, data on adjuvant therapy for advanced diseases are limited. In the present case, considering that the patient was young with a benign clinical course and wished to preserve fertility, a unilateral salpingo-oophorectomy was performed.
Most of these tumors have benign behavior; however, malignant behavior occurs in 25–43% of patients [Citation1,Citation7]. The most important consideration is whether the tumor has malignant potential. Hayes and Scully reported that the most accurate predictor of malignancy in these tumors is ≥2 mitotic figures per 10 high-power fields. Other features including grade 2–3 nuclear atypia, necrosis, hemorrhage, and a diameter of ≥7 cm were also found to be associated with malignancy [Citation1]. In the present case, the gross and histological findings were consistent with the characteristics of the ovarian steroid cell tumor NOS and did not exhibit any of these malignant features.
In patients with androgen-producing tumors, an incorrect diagnosis of polycystic ovarian syndrome (PCOS) or late-onset congenital adrenal hyperplasia (CAH) that leads to medical therapy would be detrimental to the patients because some androgen-producing tumors could be malignant and delayed surgical excision of tumors can lead to irreversible virilization.
Differentiating androgen-producing tumors from CAH can be challenging. Wong et al. [Citation13] recently reviewed 21 cases of steroid cell tumor NOS with pretreatment 17-OHP results and found a prevalence of elevated 17-OHP levels of 81%. Thus, elevated 17-OHP is commonly observed in steroid cell tumor NOS, which is consistent with our patient. Among the 17 cases with elevated 17-OHP levels, five were initially diagnosed with non-classic CAH, resulting in delayed diagnosis of steroid cell tumors because of the ambiguity of diagnostic testing. For instance, a significant increase in 17-OHP after adrenocorticotropic hormone (ACTH) stimulation is typical for congenital adrenal hyperplasia, whereas the ACTH stimulation test in most patients diagnosed with steroid cell tumors resulted in no response or insignificant changes. Surprisingly, 20% of these patients demonstrated positive 17-OHP responses to ACTH stimulation owing to the presence of ACTH receptors on these tumors. Therefore, 17-OHP responsiveness to ACTH stimulation in steroid cell tumors may lead to an incorrect diagnosis of CAH. In the present case, the ACTH stimulation test was not performed, and the patient proceeded directly to surgical treatment.
Unilateral salpingo-oophorectomy was performed and the patient was followed by measuring 17-OHP levels postoperatively. The possibility of co-existing CAH should be considered if virilization persists or serum total testosterone and 17-OHP levels do not decrease after surgical resection. In the present case, the 17-OHP level significantly declined to normal 4 weeks after the operation.
Androgen levels typically normalize after tumor removal. In the present case, testosterone levels decreased from 20.7 ng/mL to 4.8 ng/mL within 4 weeks after surgical treatment. She resumed regular menstruation. She spontaneously conceived 12 months after the surgery and had an uncomplicated pregnancy. There is little data regarding the fertility of steroid cell tumor NOS following surgical treatment.
We reviewed the literature on the fertility of patients with steroid cell tumors. A PubMed search in English using ‘steroid cell tumor’ or ‘lipid cell tumor’ and ‘pregnancy’ was performed. Only two case reports of steroid cell ovarian tumor NOS in patients who conceived were identified. Both patients had an uncomplicated pregnancy and delivered a term singleton after surgery [Citation11,Citation13] ().
Table 2. A summary of steroid cell tumors, not otherwise specified with spontaneous pregnancy reported after surgery.
In conclusion, ovarian steroid cell tumors NOS are rare. Most of these tumors are benign, unilateral, and usually present with virilizing symptoms. The present case is unique because the patient with infertility and virilizing symptoms spontaneously conceived after surgical removal of the tumor. Moreover, elevated 17-OHP levels are commonly seen in steroid cell tumor NOS. Thus, androgen-producing ovarian tumors with elevated 17-OHP levels can proceed directly to surgical treatment and carefully follow the 17-OHP levels. Incorrectly diagnosed late-onset CAH is detrimental because of the malignant potential of the tumors and delayed surgical excision can lead to irreversible virilization.
Acknowledgments
The authors would like to thank the participant in this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Hayes MC, Scully RE. Ovarian steroid cell tumors (not otherwise specified). A clinicopathological analysis of 63 cases. Am J Surg Pathol. 1987;11(11):1–5.
- Sielert L, Liu C, Nagarathinam R, et al. Androgen-producing steroid cell ovarian tumor in a young woman and subsequent spontaneous pregnancy. J Assist Reprod Genet. 2013;30(9):1157–1160.
- Uyanıkoglu H, Ozer G, Kahraman S. A spontaneous pregnancy and live birth in a woman with primary infertility following the excision of an ovarian adrenal rest tumor: a rare case. Clin Exp Reprod Med. 2020;47(4):319–322.
- Kaltsas GA, Isidori AM, Kola BP, et al. The value of the low-dose dexamethasone suppression test in the differential diagnosis of hyperandrogenism in women. J Clin Endocrinol Metab. 2003;88(6):2634–2643.
- Waggoner W, Boots LR, Azziz R. Total testosterone and DHEAS levels as predictors of androgen-secreting neoplasms: a populational study. Gynecol Endocrinol. 1999;13(6):394–400.
- Friedman CI, Schmidt GE, Kim MH, et al. Serum testosterone concentrations in the evaluation of androgen-producing tumors. Am J Obstet Gynecol. 1985;153(1):44–49.
- Taylor HB, Norris HJ. Lipid cell tumors of the ovary. Cancer. 1967;20(11):1953–1962.
- Luk WT, Lee N, Chang TC, et al. Lipid cell tumor of the ovary associated with endometrial adenocarcinoma–a case report. Changgeng Yi Xue Za Zhi. 1989;12(4):244–248.
- Elhadd TA, Connolly V, Cruickshank D, et al. An ovarian lipid cell tumour causing virilization and cushing’s syndrome. Clin Endocrinol. 1996;44(6):723–725.
- Donovan JT, Otis CN, Powell JL, et al. Cushing’s syndrome secondary to malignant lipoid cell tumor of the ovary. Gynecol Oncol. 1993;50(2):249–253.
- Anderson PW, d‘Ablaing G, 3rd, Penny R, et al. Secretion of prorenin by a virilizing ovarian tumor. Gynecol Oncol. 1992;45(1):58–61.
- Di Tucci C, Casorelli A, Morrocchi E, et al. Fertility management for malignant ovarian germ cell tumors patients. Crit Rev Oncol Hematol. 2017;120:34–42.
- Wong FCK, Chan AZ, Wong WS, et al. Hyperandrogenism, elevated 17-hydroxyprogesterone and its urinary metabolites in a young woman with ovarian steroid cell tumor, not otherwise specified: case report and review of the literature. Case Rep Endocrinol. 2019;2019:9237459.
