?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
To evaluate whether Zi Gui Nv Zhen capsules (ZGNZC) can increase the fertility rate of Chinese women with infertility due to thin endometrium.
Methods
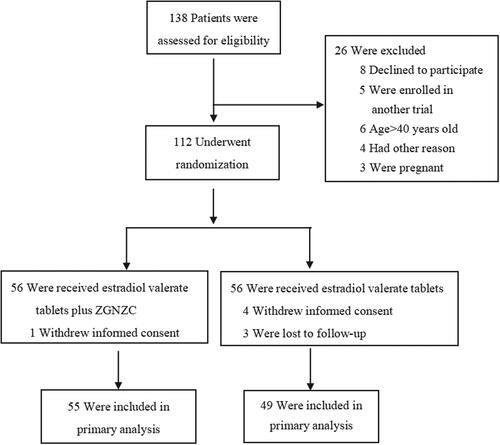
Prospective, randomized, open-labeled 3-monthly study; 104 patients (aged 20–40 years) receiving either ZGNZC (experimental group, n = 55) or not (control group, n = 49). Main outcomes: thickness/type of the endometrium during ovulation and pregnancy rate. Between-group analysis (A) compares the experimental vs. control group, and within-group analysis (B) compares data at baseline and after study in the experimental group.
Results
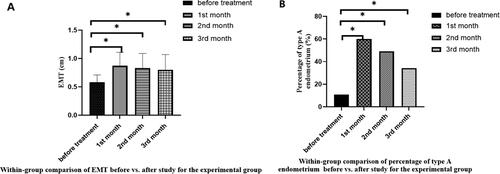
(A) Between-group-analysis: Patients with ZGNZC had a higher endometrium thickness (0.8 ± 0.27 vs. 0.68 ± 0.10; p < .05) and higher type A endometrium rates (34.2% vs. 13.2%; p < .05) than the control group. Pregnancy rates were higher in the experimental than in the control group (43.6% vs. 22.4%; p < .05). (B) Within-group-analysis: ZGNZC increased endometrium thickness (0.58 ± 0.13 vs. 0.87 ± 0.24 vs. 0.83 ± 0.26 vs. 0.80 ± 0.27), and type A endometrium rates (10.9% vs. 60.0% vs. 49.0% vs. 34.2%) (all p < .05). Univariate analysis of pregnancy with other study parameters showed positive and significant correlations between pregnancy and administration of ZGNZC (p < .05). All hepato-renal biomarkers remained within the norm. There were no adverse events.
Conclusions
In infertile women with thin endometrium who wish to conceive, two months’ application of ZGNZC can improve endometrial properties and proliferation, which is necessary for a healthy pregnancy, and increase the clinical pregnancy rate in our prospective randomized observational study.
Introduction
Female fertility is closely related to female health and the reproduction of offspring. For women, the uterus is a unique organ for the gestation of the fetus. When diseases appear in the uterus, it will inevitably affect the female’s reproductive ability. The thin endometrium is considered to be a critical factor in embryo implantation failure [Citation1].
Infertile women with thin endometrium are given high-dose estrogen supplementation to promote endometrial proliferation, and researchers have given sildenafil, low-dose aspirin, and other drugs [Citation2–6]. Still, it is difficult to improve the endometrium microenvironment. There are still controversies about using the drugs mentioned above in clinical practice. However, Chinese women often fear the hormone therapy (HT), and it cannot be used for patients with certain hormone-dependent tumors [Citation7]. Traditional Chinese Medicine (TCM) has thousands of years of history in treating infertility. The concept of ‘differentiation and treatment’ of TCM enables the implementation of thin endometrium treatment and has no disadvantages such as those caused by hormone therapy [Citation8].
ZGNZC was created by Ms. Minru Liu, the first female Master of TCM. It has been used successfully to treat menopausal symptoms in China and some Western countries. Professor Ruan Xiangyan, Department of Gynecological Endocrinology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, and her team found in the preliminary study that ZGNZC combined with a physiological dose of estrogen therapy can effectively increase endometrial thickness. Our study would further confirm the efficacy and safety of ZGNZC for fertility in infertile women with thin endometrium, and investigate whether ZGNZC can represent an alternative in infertile women with thin endometrium based on endometrial changes. It should be observed if this concept could increase the clinical pregnancy rate compared to a control. In addition, within-group analysis would also compare data from each cycle to the baseline in the experimental group to explore the time and duration of drug onset of ZGNZC.
Materials and methods
Sample and settings
This study was a prospective, randomized open-labeled study in which patients attending the Department of Gynecological Endocrinology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University between September 2018 and August 2020 was recruited. One hundred twelve women aged 20–40 years with infertility due to thin endometrium were identified as eligible participants. They were randomly assigned in a 1:1 ratio using Stratified Blocked Randomization to receive either ZGNZC or not. One woman withdrew her informed consent in the experimental group and 4 in the control group, and three were lost to follow-up in the control group. Finally, 104 women were distributed into the experimental group (n = 55) and control group (n = 49) ().
Thin endometrium was diagnosed based on the following indicators: Between days 14 and 16 of the menstrual cycle, when the LH peak day or the dominant follicles reached ≥18 mm in diameter, endometrial thickness was measured <8 mm. And patients whose endometrial thickness had not improved significantly after using high-dose estradiol valerate (4 mg/d or above), the endometrial thickness <8 mm on the ovulation day of 2 consecutive menstrual cycles [Citation9]. Inclusion criteria were women between 20 and 40 years old who plan to have a pregnancy; meet the diagnostic criteria of thin endometrium; meet the diagnostic criteria for infertility; the semen examination excluded the male factor. Exclusion criteria were pregnancy and other treatment concepts for infertile women with thin endometria, such as sildenafil and pentoxifylline, renal, and/or hepatic disease. Overt endocrine disease, severe allergic constitution, previous or current malignant diseases, and alcohol abuse; abnormal anatomical structure of reproductive organs, cervical insufficiency, severe cervical laceration, blocked fallopian tube, and endometrial tuberculosis; received sex hormone therapy currently or within four weeks before enrollment (6 months for long-acting preparations); using traditional Chinese medicine and/or other drugs for endometrial thinning therapy at present or within four weeks before enrollment; previous or present history of arterial thromboembolism (e.g. angina, myocardial infarction) and/or venous thromboembolism (e.g. deep vein thrombosis and pulmonary embolism); one of the spouses has chromosomal abnormalities.
Endocrine hormones and the thickness/type of endometrium were assessed at baseline and after three months as main endpoints. In addition, safety parameters of renal and hepatic function and lipids were tested. The primary outcomes were the parameters for the thickness/type of endometrium and the pregnancy rate evaluation. The study of patient was terminated immediately if pregnancy occurred.
The experimental group was treated with both Chinese and Western medicine, while the control group was treated with Western medicine alone. All group participants were treated with estradiol valerate tablets at 2 mg/once daily for two months. The experimental group was given both estradiol valerate tablets and ZGNZC simultaneously. They were given ZGNZC on the first day of the cycle, and were stopped when the pregnancy test result was positive. ZGNZC was available as 0.35 g/capsule and was taken as 1.05 g/three times a day, i.e. nine capsules daily. In the third month, all the participants stopped taking the medication, but the study continued.
Zi Gui Nv Zhen capsules (ZGNZC)
ZGNZC was developed by Han Sheng Tang Herbal Technologies Co., Ltd (Hong Kong, China). Each capsule is made from the following Chinese herbs: Fructus ligustri lucidi (2000 mg), Cordyceps (3 mg), Radix rehmanniae preparata (500 mg), Radix panacis quinquefolii (3 mg), Radix angelicae sinensis (300 mg), Radix astragali (300 mg), and Fructus corni (300 mg), etc.
Ethics approval
All patients gave their informed consent. The ethics committee of Beijing Obstetrics and Gynecology Hospital, Capital Medical University, reviewed and approved the study protocol (Protocol number 2018-KY-042-03; Registration number ChiCTR1800020269).
Laboratory evaluation
Blood samples were collected via venipuncture after overnight fasting for at least 8 h on days 2–4 of the menstrual cycle. The serum was separated by centrifugation and stored at −20 °C. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), progesterone (P), thyroid-stimulating hormone (TSH), and cortisol (COR) were measured by Immulite 2000 (Diagnostic Products Corp, Los Angeles, USA). Alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN) were measured by Synchron LX-20 (Beckman Coulter Corp, USA).
Ultrasound measurement
The same doctor assessed the endometrium thickness (EMT) and the endometrium type. EMT and the endometrium type were started to perform by transvaginal ultrasonography from the 8th to 10th days of the cycle, and were assessed every 2–3 days until after ovulation. EMT was measured at the thickest part in the plane of central longitudinal axis of uterus. The distance from the hyperechogenic interface between the endometrium and the myometrium to the opposite interface including the midline echo, which represented twice of the endometrial thickness, was measured. When the LH peak day or the dominant follicles reached ≥ 18 mm in diameter, the EMT measurements were repeated at least 3 times, and the mean value was recorded for analysis [Citation10]. Endometrium type A showed a triple-line type characterized by a hypoechoic endometrium with well-defined hyperechoic outer walls and a central echogenic line. Type B showed isoechoic endometrium with poorly defined outer walls and central echogenic line. Type C showed homogeneous hyperechoic endometrium [Citation11].
Sample size calculation and statistical analysis
We used the following formula for calculating the minimal sample size for this type of study:
Previous research estimated that the clinical pregnancy rate of infertile women with thin endometrium after estrogen treatment was about 10%, and the clinical pregnancy rate of ZGNZC was about 35%. The statistical significance level was set at 5% (α = .05) using a one-sided test and 80% power (1−β), Q1=Q2=0.5, π1=35%, π2=10%, πc=Q1π1+Q2π2=0.5*0.35 + 0.5*0.1 = 0.225, δ = π1-π2=25%. We calculated that the minimum sample size should be n = 70.
We used SPSS software 16.0 (SPSS Inc., Chicago, IL). The normality of distribution was assessed with the Kolmogorov-Smirnov test. The quantitative variables which were normally distributed were presented as mean ± standard deviation (SD), and values not normally distributed were presented as the median and interquartile range (IQR). Age, FSH, E2, P, COR, TSH, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and body mass index (BMI) were presented with median and IQR. The t-test and Mann-Whitney U test were used to compare median values. χ2 tests were used to compare the frequency. A p-value < .05 was considered to be statistically significant.
Results
Clinical characteristics of the study population
There were no significant differences between all baseline characteristics like age, BMI, years of infertility, and intrauterine operation. There were also no statistically significant differences regarding the biochemical safety parameters COR, TSH, AST, ALT, and BUN ().
Table 1. Basic characteristics of the two groups.
Between-group comparison (experimental vs. control group) at baseline and the end of the study
There were no statistically significant differences between E2, P, and ultrasound measurements of endometrium like EMT and percentage of type A endometrium at baseline. Participants treated with ZGNZC had a significantly (p < .05) greater endometrium thickness during ovulation, a higher percentage of type A endometrium, and a pregnancy rate higher than the control ().
Table 2. Between-group comparison of the experimental vs. control group.
Within-group comparison (baseline vs. end of study) for the experimental group
After treatment with ZGNZC, the participants had a significantly greater endometrium thickness (0.58 ± 0.13 vs. 0.87 ± 0.24 vs. 0.83 ± 0.26 vs. 0.80 ± 0.27) (all p < .05) (), and a higher percentage of type A endometrium (10.9% vs. 60.0% vs. 49.0% vs. 34.2%) (all p < .05) () in each cycle than before treatment.
Pregnancy rate
At the end of the first month, there were eight pregnancies in the experimental group and four in the control group. After the second month, there were nine additional pregnancies in the experimental group and seven in the control group. At the end of the third month, seven more participants were pregnant in the experimental group, while no patient was pregnant in the control group. Thus, the experimental group’s cumulative pregnancy rate was 43.6% (24/55, including three miscarriages), and the pregnancy rate of the control group was 22.4% (11/49, including one miscarriage) (miscarriages 5–6 weeks after pregnancy). The pregnancy rate of the experimental group was significantly (p < .05) higher than that of the control group (). All of the pregnant women had natural pregnancies.
Univariate analysis of pregnancy
In a univariate analysis of pregnant women, we found that age, BMI, P, EMT, and whether endometrium was endometrial type A were no statistically significant differences between pregnant and non-pregnant groups. At the same time, the number of pregnant participants treated with ZGNZC was significantly (p = .022) higher than the control group ().
Table 3. Univariate analysis of pregnancy-related factors.
Safety parameters and tolerability
There were no statistically significant differences for AST, ALT, and BUN (). There were no side effects for the liver and kidneys, and also no other adverse events were found associated with using ZGNZC. The participants rated the tolerability as good.
Discussion
As the main results of our study, we found that ZGNZC significantly increased the thickness of the endometrium, the percentage of type A endometrium, and the pregnancy rate. Furthermore, we found that the endometrial thickness and the percentage of type A endometrium in the first month were the highest. As the study progressed, the differences decreased slightly. In the third month of the study, the participants discontinued ZGNZC. However, the thickness/type of the endometrium was still higher than before the study, indicating that the drug had a fast onset of action and a long-lasting effect. Additionally, the percentage of type A endometrium was higher, thereby improving endometrial type, both preconditions for a successful clinical pregnancy.
From our study, a univariate analysis of the age, height, weight, BMI, AMH level, P, EMT, and endometrial type A status and whether to receive ZGNZC treatment by pregnant participants, found that the participants treated with ZGNZC had a significant difference between pregnant and non-pregnant. We can also suggest that ZGNZC can help to improve the clinical pregnancy rate.
Endometrial factors are the key factors affecting the success of embryo implantation [Citation1]. Insufficient endometrial receptivity causes approximately two-thirds of implantation failures [Citation12]. EMT is a marker of endometrial receptivity and a prognostic factor [Citation13]. If EMT is less than 6 mm, from the point of view of infertility, almost no pregnancy occurs [Citation14,Citation15]. A Meta-analysis of 22 studies showed that thin endometrium increases the incidence of adverse outcomes in patients with in vitro fertilization-embryo transfer (IVF-ET) [Citation16].
The theory of TCM believes that the ‘kidney governs reproduction’, ‘kidney is the innate foundation’, and ‘menstrual water flows out of the kidneys’, emphasizing the relationship between menstruation, reproduction, and the kidney (in the wording of TCM). Ms. Minru Liu pointed out that infertility in women with thin endometrium is due to insufficient kidney Yin and inability to adapt to the evolution of the menstrual cycle, resulting in decreased menstrual flow and ovulation disorders. As a special form of TCM, ZGNZC was to invigorate the kidney Yin (nourish blood), lay the material foundation, promote the growth of the endometrium, the synchronous development of the endometrium, improve the receptivity of the endometrium, regulate and promote the maturity of the follicle.
ZGNZC contains 100% pure, natural herbal ingredients. There are (1) estrogen-like and androgen-like substances in Fructus ligustri lucidi, which increased estradiol levels and the number of follicles in rabbits [Citation17–19]. (2) Ginsenoside exerts its estrogenic activity by binding to the estrogen receptor (ER) [Citation20,Citation21]. (3) Fructus corni regulates immunological protection [Citation22–26]. In animal experiments, ZGNZC increased the expression of ER, thereby improving endometrial receptivity [Citation27,Citation28].
ZGNZC has several strengths: ZGNZC is a capsule that is convenient to take. Using ZGNZC avoids typical side effects of HRT, such as the risk of endometrial cancer, cardiovascular risks, and abnormal uterine bleeding [Citation29,Citation30].
The study’s strength is that infertile women with thin endometrium are usually treated with high-dose hormones such as estrogen. However, Chinese women often worry about the hormone therapy, and there are important warnings for risk patients and contraindications for using the hormone. Different forms of TCM have already been suggested for fertility preservation. However, until now, Zi Gui Nv Zhen capsules have not been investigated for this indication.
The weakness of this trial was that no animal model was established, so the mechanism and target of action of ZGNZC in promoting endometrial growth and improving endometrial receptivity could not be explained from the protein level or mRNA level. There was no placebo control due to the limited clinical conditions, so some statistical results lack robust and objective evidence support.
Conclusion
In Chinese women with infertility due to thin endometrium, ZGNZC, a herbal product of TCM, increased the clinical pregnancy rate. The tolerability was good and all liver and kidney function safety parameters remained within the norm. Thus, ZGNZC is mainly used for fertility preservation in patients with infertility due to thin endometrium, mainly because it can also be used if HRT is contraindicated. The overall results of this study using ZGNZC are very promising for continuing this research to obtain robust results regarding the increase in the pregnancy rate.
Acknowledgment
The authors especially thank Prof. Xingming Li of Capital Medical University (Beijing, China) for his assistance in the data’s statistical analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author (RXY), upon reasonable request.
Additional information
Funding
References
- Nagori CB, Panchal SY, Patel H. Endometyial regeneration using autologous adult stem cells followed by conception by in vitro fertili zation in a patient of severe Asherman s syndrome[J]. J Hum Reprod Sci. 2011;4(1):1–6. doi: 10.4103/0974-1208.82360.
- Mahajan N, Sharma S. The endometrium in assisted reproductive technology: how thin is thin? [J]. J Hum Reprod Sci. 2016;9(1):3–8. doi: 10.4103/0974-1208.178632.
- Ranisavljevic N, Raad J, Anahory T, et al. Embryo transfer strategy and therapeutic options in infertile patients with thin endometrium: a systematic review[J]. J Assist Reprod Genet. 2019;36(11):2217–2231. doi: 10.1007/s10815-019-01576-w.
- Vartanyan E, Tsaturova K, Devyatova E. Thin endometrium problem in IVF programs[J]. Gynecol Endocrinol. 2020;36(sup1):24–27. doi: 10.1080/09513590.2020.1816724.
- Li X, Luan T, Zhao C, et al. Effect of sildenafil citrate on treatment of infertility in women with a thin endometrium: a systematic review and meta-analysis[J]. J Int Med Res. 2020;48(11):300060520969584. doi: 10.1177/0300060520969584.
- Wang TF, Kang XM, Zhao AM, et al. Low-dose aspirin improves endometrial receptivity in the midluteal phase in unexplained recurrent pregnancy loss[J]. Int J Gynaecol Obstet. 2020;150(1):77–82. doi: 10.1002/ijgo.13160.
- Sullivan SD, Sarrel PM, Nelson LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause[J]. Fertil Steril. 2016;106(7):1588–1599. doi: 10.1016/j.fertnstert.2016.09.046.
- Zhang X, Li Y, Pan X, et al. Meta-analysis of randomized controlled trials of traditional chinese medicine in the treatment of decline in ovarian reserve[J]. Tianjin Journal of Traditional Chinese Medicine. 2018;35(11):839–845.
- Yuan X, Saravelos SH, Wang Q, et al. Endometrial thickness as a predictor of pregnancy outcomes in 10787 fresh IVF-ICSI cycles[J]. Reprod Biomed Online. 2016;33(2):197–205. doi: 10.1016/j.rbmo.2016.05.002.
- Nakamura Y, Ono M, Yoshida Y, et al. Effects of clomiphene citrate on the endometrial thickness and echogenic pattern of the endometrium[J]. Fertil Steril. 1997;67(2):256–260. doi: 10.1016/S0015-0282(97)81907-3.
- Chen SL, Wu FR, Luo C, et al. Combined analysis of endometrial thickness and pattern in predicting outcome of in vitro fertilization and embryo transfer: a retrospective cohort study[J]. Reprod Biol Endocrinol. 2010;8:30. doi: 10.1186/1477-7827-8-30.
- Ledee-Bataille N, Lapree-Delage G, Taupin JL, et al. Concentration of leukaemia inhibitory factor (LIF) in uterine flushing fluid is highly predictive of embryo implantation[J]. Hum Reprod. 2002;17(1):213–218. doi: 10.1093/humrep/17.1.213.
- Kane M, Morgan P, Coonan C. Peptide growth factors and preimplantation development[J]. Hum Reprod Update. 1997;3(2):137–157. doi: 10.1093/humupd/3.2.137.
- Schild RL, Knobloch C, Dorn C, et al. Endometrial receptivity in an in vitro fertilization program as assessed by spiral artery blood flow, endometrial thickness, endometrial volume, and uterine artery blood flow[J]. Fertil Steril. 2001;75(2):361–366. doi: 10.1016/s0015-0282(00)01695-2.
- Yaman C, Ebner T, Jesacher K, et al. Sonographic measurement of endometrium thickness as apredictive value for pregnancy through IVF[J]. UltraschallMed. 2002;23:2562–2569.
- Kasius A, Smit JG, Torrance HL, et al. Endometrial thickness and pregnancy rates after IVF: a systematic review[J]. Hum Reprod Update. 2014;20(4):530–541. doi: 10.1093/humupd/dmu011.
- Zhang HA. Clinical study on bushen huoxue culuan recipe in treating infertility patients suffering from diminished ovarian reserve[D] Thesis of Master of Medicine. China Academy of Chinese Medical Sciences, 2018.
- Yin X-D, Xue X-O, Wang J-S, et al. Effect of Bushen Huoxue recipe on women with thin endometrial ovulation disorder and a rat model of thin endometrium resulted from kidney deficiency-related blood stasis[J]. Gynecol Endocrinol. 2021;37(5):e1781079–437. doi: 10.1080/09513590.2020.1781079.
- Huang W, Yang Y. Pharmacological and clinical research progress of fructus ligustri lucidi and its active components[J]. Modern J Integr Tradition Chin Western Med. 2003;12(7):772–774.
- Moore RK, Otsuka F, Shimasaki S. Molecular basis of bone morphogenetic protein-15 signaling in granulosa cells[J]. J Biol Chem. 2003;278(1):304–310. doi: 10.1074/jbc.M207362200.
- Ma B, Qin X, et a1. The research progress of American Gineseng clinical pharmacology (2004–2010)[J]. J Jiangxi Univer TCM. 2001;23(5):88–92.
- Huang C, Song K, Ma W, et al. Immunomodulatory mechanism of Bushen Huoxue recipe alleviates cyclophosphamide-induced diminished ovarian reserve in mouse model[J]. J Ethnopharmacol. 2017;208:44–56. doi: 10.1016/j.jep.2017.06.022.
- Li L. The related research of the diminished ovarian reserve intervened by jiajian yijing decoction[D] Thesis of Master of Medicine. Guangzhou University of Chinese Medicine, 2015.
- Ayesha JV, Goswami D. Premature ovarian failure: an association with autoimmune diseases[J]. J Clin Diagn Res. 2016;10(10):C10–C12.
- Fan Y, Chang Y, Wei L, et al. Apoptosis of mural granulosa cells is increased in women with diminished ovarian reserve[J]. J Assist Reprod Genet. 2019;36(6):1225–1235. doi: 10.1007/s10815-019-01446-5.
- Hunzicker-Dunn ME, Lopez-Biladeau B, Law NC, et al. PKA and GAB2 play Central roles in the FSH signaling pathway to PI3K and AKT in ovarian granulosa cells[J]. Proc Natl Acad Sci U S A. 2012;109(44):E2979–E2988.
- Jiang X. Experimental study on the effect of kidney-tonifying compound on the bone of ovariectomized female rats[D] Thesis of Doctoral of Medicine. Chendu University of Chinese Medicine, 2004.
- Zhang RT, Wu HN, Yu GH, et al. Effective components and signaling pathways of epimedium brevicornumbased on network pharmacology[J]. Zhongguo Zhong Yao Za Zhi. 2018;43(23):4709–4717. doi: 10.19540/j.cnki.cjcmm.20180905.001.
- Satirapod C, Wingprawat S, Jultanmas R, et al. Effect of estradiol valerate on endometrium thickness during clomiphene citrate-stimulated ovulation[J]. J Obstet Gynaecol Res. 2014;40(1):96–101. doi: 10.1111/jog.12130.
- Baber RJ, Panay N, Fenton A, IMS Writing Group. 2016 IMS recommendations on women’s midlife health and menopause hormone therapy[J]. Climacteric. 2016;19(2):109–150. doi: 10.3109/13697137.2015.1129166.