Abstract
Objectives
The objective is to assess the perception of gynecologists regarding patients’ adherence to vulvovaginal atrophy (VVA) treatments, to evaluate the gynecologists’ opinions on what their patients think about treatment adherence, and to compare the gynecologists’ opinions with the patients’ own perceptions within the CRETA study.
Methods
Spanish gynecologists who participated in the CRETA study were asked to fill out an online 41-item questionnaire to evaluate their views on VVA management.
Results
From 29 centers across Spain, 44 gynecologists completed the survey. Their mean age was 47.2 years old, two-thirds of them were women, and the average professional experience was over 20 years. According to the gynecologists, the therapy most frequently used by VVA-diagnosed women was vaginal moisturizers (45.5%), followed by local estrogen therapy (36.4%) and ospemifene (18.2%). Nevertheless, ospemifene was viewed as the therapeutic option with the most efficacy, easiest route of administration, shorter time to symptom improvement, lower percentage of dropouts, and higher treatment adherence.
Conclusions
Spanish gynecologists are in general agreement with their patients regarding VVA treatment preferences and the main issues for adherence and effectiveness. However, there is an opportunity for doctor–patient communication improvement. Among the three therapeutic options evaluated, ospemifene is regarded as offering some competitive advantages.
Introduction
Vulvovaginal atrophy (VVA), considered as part of the genitourinary syndrome of menopause (GSM), is a chronic and progressive condition associated with aging and hypoestrogenism [Citation1–5]. According to epidemiological studies, VVA prevalence is high [Citation6]. Reported data range from 63 to 80% in Western countries amongst postmenopausal women who visited a gynecologist [Citation3,Citation7–9]. REVIVE [Citation10] and EVES [Citation11] surveys concluded that VVA affects approximately 50% of all postmenopausal women in Europe. VVA develops gradually over the years and does not resolve spontaneously, which negatively affects women’s sex life, emotional health, and quality of life (QoL) [Citation3,Citation6,Citation9,Citation11–14]. Therefore, it is important to treat this condition properly and timely [Citation6].
Until recently, available therapeutic options included over-the-counter moisturizers and lubricants, vaginal estrogens (local estrogen therapy, LET), and systemic estrogens. However, some patients reject hormones because of the possible perceived risk of cancer and consider local therapies uncomfortable, difficult to apply, and messy. Consequently, VVA treatments have high discontinuation and dissatisfaction rates [Citation8,Citation10,Citation15–17]. One option to improve traditional VVA therapies is ospemifene, a systemic third-generation selective estrogen receptor modulator, with oral administration, intended for the treatment of moderate to severe VVA symptoms [Citation11,Citation15,Citation18,Citation19]. The drug has proven to be safe and effective in improving symptoms [Citation11,Citation15,Citation18–20], increasing treatment satisfaction and adherence [Citation3,Citation15,Citation21], improving self-reported women’s QoL [Citation22], and even decreasing all-cause healthcare costs [Citation16].
Despite the high impact of VVA on women’s lives, its high prevalence, and the safe and effective therapeutic options available, this condition remains underdiagnosed and undertreated [Citation3,Citation10,Citation23,Citation24]. This disparity is thought to be primarily a consequence of women’s unwillingness to report symptoms to their gynecologists [Citation3,Citation10,Citation13,Citation17]. This embarrassment, discouragement, and unwillingness to report are strongly linked to communication constraints between patients and physicians [Citation13]. Lack of awareness of gynecologists may also contribute to the poor diagnosis and undertreatment of VVA [Citation8,Citation17]. In fact, awareness and knowledge of this condition do not seem to have improved over the years among physicians [Citation3].
To optimize postmenopausal women’s healthcare, it would be of great importance to know gynecologists’ perception of VVA and to check if it matches that of postmenopausal women. In this sense, the CRETA study has already reported the VVA patients’ perception of the condition and their satisfaction and adherence with current therapeutic options [Citation21]. This manuscript assesses the perception of gynecologists regarding patients’ treatment effectiveness and adherence, evaluates gynecologists’ insights on what their patients think about treatment adherence and effectiveness, and compares them with patients’ own perceptions.
Methods
Study design
The CRETA was a descriptive, observational, cross-sectional, and multicenter study conducted in 29 private and public hospitals and medical centers across Spain from June 2020 to September 2021 (NCT04607707) [Citation21]. The primary objective of the study was to measure and evaluate treatment satisfaction among women with VVA. Moreover, CRETA also aimed to analyze other outcomes, such as treatment adherence, self-reported experience of postmenopausal women treated for VVA symptoms, and women’s QoL, as well as gynecologists’ opinions on patients’ perception of adherence, and comparison between the points of view of both agents. This paper focuses on the latter.
Ethical approval for this study was given at all the involved centers by the Ethics Committee for Research with medicinal products from the León and Bierzo Health Areas. The study complied with the Declaration of Helsinki for Human Research and guaranteed patients’ data confidentiality. Details regarding patients with VVA and the development of the study have already been described [Citation21].
Study procedures, questionnaire administration, and data analysis
Women participating in the CRETA study completed a 48-item questionnaire about sociodemographic data, the relationship between women and their gynecologists, perceptions about the VVA condition, women’s satisfaction, medication adherence [Citation21], and the Cervantes QoL scale [Citation22]. Gynecologists involved in the CRETA study were asked to complete an anonymous online questionnaire regarding their professional experience treating VVA, treatment prescribed to their patients, preferences, perceived adherence, and efficacy of each treatment option, as well as their perception of what their patients thought about the condition and the therapies. The questionnaire had 41 items that assessed all these aspects of VVA and its management. It was structured in two major sections: (1) gynecologists’ demographic data and gynecologists’ opinions as healthcare professionals; (2) gynecologists’ opinions on VVA patients’ perception regarding the condition and the therapeutic options.
The study aimed to collect data from 900 women at 60 different centers. The sample size was set to achieve an accuracy of 3%, estimated with a 95% asymptotic two-tailed confidence interval, assuming a recruitment rate of 50%. However, the final number of participating centers was smaller than initially projected, mainly because the recruiting process was interrupted due to the increased demand for care caused by the COVID-19 pandemic. The analysis of the results from the gynecologist’s questionnaire was based on a descriptive statistics report. All analyses were carried out based on the overall sample of participating gynecologists and VVA treatment type. Data are expressed as mean ± standard deviation (SD).
Results
Demographic features and clinical experience of gynecologists
From the 29 centers and hospitals participating in the CRETA study, the survey was specifically designed for and completed by 44 gynecologists. Most of them (n = 34) also recruited patients (ranging from 4 to 75 patients per practitioner) who completed the patients’ survey reported in our previous manuscript [Citation21].
The gynecologists’ mean age was 47.2 years, the majority females (75%), with over 20 years of professional experience (average of 20.8 years). The average number of patients with VVA seen per year was 65.5, and most gynecologists performed one or two follow-ups per year for each of these patients. More than half of these women (59.3%) were diagnosed with moderate to severe VVA. More precise values of these demographic and clinical data are compiled in .
Table 1. Demographic features of the gynecologists and data regarding patient management.
Gynecologists’ own perception and opinion on what patients think about VVA and treatment adherence
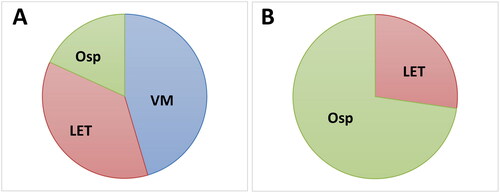
According to the professional experience of the gynecologists, the therapeutic options most frequently used by women diagnosed with moderate to severe VVA were vaginal moisturizers (45.5% of patients), followed by LET (36.4%) and, lastly, ospemifene (18.2%). Results are graphically depicted in .
Figure 1. Gynecologist perception regarding: (A) percentage of most frequently used therapeutic options for the treatment of VVA amongst their patients diagnosed with VVA; and (B) treatment efficacy in reversing VVA histological changes. LET, local estrogen therapy; osp, ospemifene; VM, vaginal moisturizers.
Regarding the gynecologists’ opinion of the patients’ knowledge about VVA, most gynecologists (72.7%) considered that their patients had a low level of knowledge about VVA as a treatable condition, while only 4.5% of gynecologists considered that patients had a high level of knowledge. Regarding treatment choices according to the patient’s level of knowledge, 54.5% of gynecologists reported that patients with a higher level of knowledge used LET, 27.3% used moisturizers, and 18.2% used ospemifene. Treatment rejection by patients from the gynecologists’ insight was greater for LET (72.7% of gynecologists), whose main concern was safety, followed by ospemifene (54.5%), whose main concern was also safety and, lastly, vaginal moisturizers (47.7%), whose main reason for treatment rejection was messiness.
Regarding treatment adherence, 90.9% of practitioners considered that patients under 60 years of age showed greater adherence to treatment, and 84.1% of gynecologists thought that oral treatment for other pathologies might improve treatment adherence to oral therapy for VVA. Most gynecologists (86.4%) agreed that the administration route that could improve treatment adherence was oral intake, while the most effective posology would be daily or weekly dosing (45.5% of the agreement for both). As for the proportion of missed treatments, gynecologists reported that the treatment with the highest average percentage of missed intakes/application was vaginal moisturizers (58.0%), followed by LET (50.9%) and, lastly, ospemifene (23.4%).
In relation to treatment effectiveness and improvement of the condition’s features, 72.7% of gynecologists considered ospemifene as the most effective treatment for reversing the histological changes induced by VVA despite being the least frequently used (), while only 27.3% chose LET as the most effective therapy (). Likewise, according to gynecologists’ experience, the therapy that provided a faster improvement of symptoms was ospemifene, followed by LET and, lastly, moisturizers. The treatments that generated more side effects as perceived by gynecologists, in order of preference and higher percentage, were ospemifene, followed by LET and vaginal moisturizers. Numerical values are detailed in .
Table 2. Gynecologists’ opinion about VVA patients’ perception regarding the efficacy and safety of the different therapeutic options. Data are expressed as percentage of practitioners who selected each option (n = 44).
Regarding treatment duration, most gynecologists (90.9%) prescribed a treatment period greater than 6 months to their patients with VVA for all the therapeutic options analyzed. Nevertheless, they reported that there was a percentage of patients (around 30%) in all treatment options that never started the therapy despite the physician’s prescription. Likewise, they stated that a percentage of women discontinued treatment before finishing the prescription period, which was lower for ospemifene-treated patients. Physicians reported that 29.5% of patients who abandoned a prescribed treatment later requested another one. As second-line therapy, gynecologists’ preferences were as follows: ospemifene (56.8%), LET (29.5%), and moisturizers (13.6%). Gynecologists thought the main reasons for treatment dropout were the price of ospemifene, concern about cancer risk for LET, and time to improve moisturizers. Physicians perceived that the treatment with the longest adherence time was ospemifene (8.4 months), and the treatment with the longest time to symptom improvement was vaginal moisturizers (2.8 months). Data are detailed in .
Table 3. Gynecologists’ perception about the treatment duration and adherence of the different therapeutic options.
According to gynecologists’ perceptions of patients’ views, the main positive aspects of the treatment with ospemifene highlighted by the patients were ease of administration route (59.1% of practitioners) and improvement in sex life (11.4%). Likewise, the main positive features of LET were the degree of improvement (43.2%) and improvement in sex life (18.2%). Finally, the positive aspects highlighted for vaginal moisturizers were being a non-hormonal method without concerns regarding the risk of cancer (56.8%) and being affordable (18.2%).
Discussion
The results of the survey reported in this paper showed that Spanish gynecologists are in general agreement with their patients regarding the main issues of VVA treatment preferences, efficacy, and adherence. As described in other studies [Citation8,Citation10,Citation15–17,Citation25,Citation26], gynecologists participating in the survey were generally aware of the prevalence of VVA, as well as the general low adherence, low level of satisfaction, and high discontinuation rate showed by women diagnosed with this condition. On the other hand, gynecologists in our study (72%) considered that women had a low level of knowledge about VVA as a treatable condition, which has also been reported in other studies in our country [Citation27]. This is in line with the results reported in other studies that pointed out the need to initiate educational programs with menopausal women so that they can better understand and manage the symptoms associated with VVA [Citation28]. Despite gynecologists’ perception, almost 85% of patients participating in the CRETA study reported that they were already aware of the concept of VVA [Citation21]. We need to bear in mind that women included in the CRETA study were already in treatment for VVA symptoms, and more than half had medium-high educational levels [Citation22]. Moreover, as a direct result of the inclusion criteria used in the CRETA study, most patients (around 60%) presented moderate to severe VVA symptoms. All these factors could have made these women more knowledgeable and more prone to discuss and use VVA treatments than the general Spanish population of menopausal women. Therefore, the different perceptions about knowledge of the condition reported by gynecologists and patients in the CRETA study show that there is an opportunity for improvement in the communication between gynecologists and their patients. Practitioners should address issues regarding VVA symptoms as women are more likely to obtain their information from them than from other reliable sources [Citation29]. Education is important so that women can understand the genitourinary changes that occur associated with menopause and get counseling about how to manage them [Citation24]. Along this line, some initiatives have been carried out to improve the patient–doctor relationship in menopausal women [Citation23].
Regarding positive attributes associated with VVA treatments, results from the CRETA study showed that ospemifene had an overall better score compared to LET and vaginal moisturizers concerning route of administration, easiness to use, positive impact on sex life, lack of interference on women’s lives, and shorter time to symptom improvement, as perceived by patients [Citation21]. Although the perception is more positive for ospemifene, vaginal moisturizers and LET are prescribed more often. The reason for this discrepancy is that ospemifene is a relatively recent therapeutic option for patients with VVA and was initially considered as a second option for women who would not accept LET [Citation15,Citation18,Citation20]. Nevertheless, clinical data, including the CRETA study [Citation21,Citation22], have shown that ospemifene is a suitable therapeutic option for long-term VVA treatment in a wide range of patients.
In our study, most gynecologists agreed that oral intake can greatly improve treatment adherence and, therefore, achieve better management of the condition. This preference for oral intake has been reported in other studies [Citation17,Citation21]. Moreover, according to patients’ self-reported perception, ospemifene improves QoL to a greater extent than vaginal moisturizers or LET [Citation22]. This is also in agreement with gynecologists’ perceptions, who reported ease of administration and improvement in sex life as the two main positive aspects regarding ospemifene treatment. All aspects related to sex life seem to have a profound impact on women’s QoL, and most of them believe that an active sex life is important [Citation22,Citation29]. Accordingly, most patients in the CRETA study were sexually active, and the ospemifene cohort gave more importance to their sex life [Citation22]. It is well known that VVA has a significant negative impact on menopausal women’s sex life [Citation6,Citation17], but this is an aspect often underestimated by gynecologists [Citation30]. In fact, a lack of communication has been reported between women suffering from GSM and their gynecologists [Citation27]. Therefore, the positive effects of ospemifene on patients’ sex lives could be one of the main underlying reasons for the more positive perception toward this drug (faster symptom improvement and higher efficacy) reported by patients [Citation21,Citation22] and gynecologists alike. In fact, the prevalence of patients with a sexual problem has been reported to increase four times when they were asked about sexuality during gynecologist visits [Citation31]. Therefore, asking postmenopausal women about sexuality is a valuable tool that might help to achieve better management of VVA symptoms and their impact on the patient’s life.
A direct relationship has been suggested between medical treatment satisfaction and patient compliance [Citation32]. Consequently, it is not highly surprising that treatments acting directly on vaginal physiology (such as LET and ospemifene), rather than acting only upon symptoms (like vaginal moisturizers), showed higher patient satisfaction and treatment adherence. In the CRETA study, the reported patients’ satisfaction was significantly higher and treatment discontinuation was significantly lower in the ospemifene group compared to LET or vaginal moisturizer cohorts [Citation21]. In general, the perception of gynecologists in our study seems to agree with the patient’s perspective. Ospemifene has proven to have an efficacy profile comparable to or even better than local vaginal estrogens, which are considered the standard of care for physiological relief of VVA [Citation24,Citation33,Citation34]. This, added to the preferred route of administration and the possibility of daily dosing, as the scheme preferred by patients [Citation21], gives ospemifene a competitive advantage over other therapeutic options for the treatment of VVA.
Among the disadvantages perceived, surveyed patients using ospemifene were mostly worried about the medication’s price and safety profile [Citation21]. This agrees with the gynecologists’ perception since they also noted a greater rejection of LET and ospemifene based on safety concerns. According to gynecologists in the DIADEM study, the main reason for ospemifene treatment interruption was also price, followed by the fear of negative effects despite its safety profile [Citation25]. We can argue that patients first reject hormonal treatment, probably due to the perceived risk of cancer, and then, they also reject systemic treatments, perhaps as a general concern about unspecific drug side effects. Strikingly, gynecologists also shared the perception of ospemifene being the therapeutic option with the most possible side effects. The safety concern is excessive despite published results showing ospemifene to be safe after several years of follow-up and real-life studies [Citation15,Citation16,Citation18,Citation20,Citation25,Citation34,Citation35]. The fear of negative effects reported by 65.9% of gynecologists in our study, as well as their patients [Citation21], suggest that the profile of the risks and benefits of ospemifene has not been adequately explained to physicians and, thereby, to patients. A similar conclusion was reported in the DIADEM study [Citation25]. Therefore, gynecologists’ awareness of VVA treatments and their pitfalls is another aspect that would greatly benefit from improvement.
Ours is one of the few studies that has assessed gynecologists’ perceptions and opinions regarding the VVA condition. Despite its valuable results, our study suffers from the limitations inherent to surveys, including a self-reporting bias and the selection of a relatively small number of practitioners. Therefore, studies with larger samples are needed to support our results. Moreover, we should bear in mind a possible selection bias: gynecologists who participated in the CRETA study could be the most sensitized and have greater knowledge and experience on VVA diagnosis and its management. Although gynecologists deal with VVA in their daily practice, a significant difference has been reported between those working in the public sector and those focused on private practice [Citation26]. This difference was not considered in our study. Future studies should address whether demographic features (e.g. age, location, experience, etc.) influence gynecologists’ perceptions.
Conclusions
In general, the gynecologists participating in our study are aware of the burden of VVA symptoms upon the growing population of postmenopausal women. Gynecologists seem to generally agree with their patients regarding treatment preferences and the main issues for adherence deficiencies, although there is an opportunity for communication and VVA management improvement. Better physician awareness, better patient education, and improvement in patient–gynecologist communication are essential to improve treatment adherence and to achieve better treatment outcomes. According to gynecologists’ perceptions, ospemifene can help to reduce the burden of VVA symptoms, emerging as an optimal therapeutic approach regarding effectiveness and safety, and could help to maximize patient adherence.
Financial support
The study received financial support from Shionogi S.L.U.
Reprint requests
Reprints will not be available.
Acknowledgments
The authors thank Kalispera medical writing S. L. and J. L. Ramírez for supporting medical writing.
Disclosure statement/financial Disclosure statement
Shionogi S.L.U. sponsored the study and provided support for the medical writing assistance by Kalispera medical writing S.L. RS-B has received consulting fees and speaker´s honoraria from Shionogi and research funding from Astellas, Exeltis, Isdin, Mitra, CumLaude. SP has received consulting fees and speaker’s honoraria from Shionogi and Bayer HC, Exeltis, Gedeon Richter, NovoNordisk, Procare H, Serelys, Lacer, Sandoz, Pfizer, and Theramex. MJC has received consulting fees and speaker´s honoraria from Shionogi. AJGC and JJQM are currently working at Shionogi S.L.U. For the remaining authors, none were declared.
References
- Portman DJ, Gass ML, Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the international society for the study of women’s sexual health and the North American menopause society. Menopause 2014;21:1–6. doi: 10.1097/GME.0000000000000329.
- Lev-Sagie A. Vulvar and vaginal atrophy: physiology, clinical presentation, and treatment considerations. Clin Obstet Gynecol 2015;58:476–491. doi: 10.1097/GRF.0000000000000126.
- Kingsberg SA, Krychman M, Graham S, et al. The women’s EMPOWER survey: identifying women’s perceptions on vulvar and vaginal atrophy and its treatment. J Sex Med 2017;14:413–424. doi: 10.1016/j.jsxm.2017.01.010.
- Mac Bride MB, Rhodes DJ, Shuster LT. Vulvovaginal atrophy. Mayo Clin Proc 2010;85:87–94. doi: 10.4065/mcp.2009.0413.
- Cagnacci A, Carbone MM, Palma F, AGATA study. Prevalence and association between objective signs and subjective symptoms of vaginal atrophy: the AGATA study. Menopause 2016;23:1139–1145. doi: 10.1097/GME.0000000000000675.
- Palacios S, Cancelo MJ, Castelo Branco C, et al. Vulvar and vaginal atrophy as viewed by the spanish REVIVE participants: symptoms, management and treatment perceptions. Climacteric 2017;20:55–61. doi: 10.1080/13697137.2016.1262840.
- Faubion SS, Kingsberg SA, Clark AL, et al. The 2020 genitourinary syndrome of menopause position statement of the North American menopause society. Menopause 2020;27:976–992.
- Palma F, Volpe A, Villa P, et al. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: the AGATA study. Maturitas 2016;83:40–44. doi: 10.1016/j.maturitas.2015.09.001.
- Santoro N, Komi J. Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med 2009;6:2133–2142. doi: 10.1111/j.1743-6109.2009.01335.x.
- Panay N, Palacios S, Bruyniks N, et al. Symptom severity and quality of life in the management of vulvovaginal atrophy in postmenopausal women. Maturitas 2019;124:55–61. doi: 10.1016/j.maturitas.2019.03.013.
- Palacios S, Nappi RE, Bruyniks N, et al. The European vulvovaginal epidemiological survey (EVES): prevalence, symptoms and impact of vulvovaginal atrophy of menopause. Climacteric 2018;21:286–291. doi: 10.1080/13697137.2018.1446930.
- DiBonaventura M, Luo X, Moffatt M, et al. The association between vulvovaginal atrophy symptoms and quality of life among postmenopausal women in the United States and Western Europe. J Womens Health (Larchmt) 2015;24:713–722. doi: 10.1089/jwh.2014.5177.
- Nappi RE, Palacios S, Bruyniks N, et al. The burden of vulvovaginal atrophy on women’s daily living: implications on quality of life from a face-to-face real-life survey. Menopause 2019;26:485–491. doi: 10.1097/GME.0000000000001260.
- Moral E, Delgado JL, Carmona F, et al. Genitourinary syndrome of menopause. Prevalence and quality of life in spanish postmenopausal women. The GENISSE study. Climacteric 2018;21:167–173. doi: 10.1080/13697137.2017.1421921.
- Cagnacci A, Xholli A, Venier M. Ospemifene in the management of vulvar and vaginal atrophy: focus on the assessment of patient acceptability and ease of use. Patient Prefer Adherence 2020;14:55–62. doi: 10.2147/PPA.S203614.
- Faught BM, Soulban G, Yeaw J, et al. Ospemifene versus local estrogen: adherence and costs in postmenopausal dyspareunia. J Comp Eff Res 2019;8:1111–1123. doi: 10.2217/cer-2019-0091.
- Nappi RE, Palacios S, Panay N, et al. Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE survey. Climacteric 2016;19:188–197. doi: 10.3109/13697137.2015.1107039.
- Archer DF, Goldstein SR, Simon JA, et al. Efficacy and safety of ospemifene in postmenopausal women with moderate-to-severe vaginal dryness: a phase 3, randomized, double-blind, placebo-controlled, multicenter trial. Menopause 2019;26:611–621. doi: 10.1097/GME.0000000000001292.
- Palacios S, Panay N, Sánchez-Borrego R, et al. Earlier treatment of vulvovaginal atrophy in post-menopausal women may improve treatment outcomes. J Gynecol Women’s Health 2019;16:555928.
- Simon JA, Altomare C, Cort S, et al. Overall safety of ospemifene in postmenopausal women from placebo-controlled phase 2 and 3 trials. J Womens Health (Larchmt) 2018;27:14–23. doi: 10.1089/jwh.2017.6385.
- Sánchez Borrego R, de Diego Pérez de Zabala MV, Alfageme Gullón MJ, et al. Satisfaction and medication adherence in women with vulvovaginal atrophy: the CRETA study. Climateric 2023;26:437–444.
- Palacios S, Sánchez Borrego R, Suárez Álvarez B, et al. Impact of vulvovaginal atrophy therapies on postmenopausal women’s quality of life. Maturitas 2023;172:46–51. doi: 10.1016/j.maturitas.2023.03.007.
- Ashkenazy R, Peterson ME. PAUSE: a patient-centric tool to support patient-provider engagement on menopause. Clin Med Insights Womens Health 2018;11:1179562X18757467. doi: 10.1177/1179562X18757467.
- Faubion SS, Sood R, Kapoor E. Genitourinary syndrome of menopause: management strategies for the clinician. Mayo Clin Proc 2017;92:1842–1849. doi: 10.1016/j.mayocp.2017.08.019.
- Alvisi S, Baldassarre M, Gava G, et al. Knowledge of genito-urinary syndrome of menopause among Italian gynecologists: the DIADEM survey. Maturitas 2021;143:89–95. doi: 10.1016/j.maturitas.2020.09.011.
- González Rodríguez SP, Cornellana Puigarnau MJ, Cancelo Hidalgo MJ. Perception and attitudes of Spanish gynecologists against the genitourinary syndrome during the menopause. VUVAGINE Study. Prog Obstet Ginecol 2016;59:134–140.
- Baquedano Mainar L, Sánchez Méndez S, Dieste Pérez P, et al. Women’s knowledge about the genitourinary syndrome of menopause: adherence to its treatments in the COVID-19 era in a sample of them: COMEM-GSM study. BMC Womens Health 2021;21:398.
- Krychman M, Graham S, Bernick B, et al. The women’s EMPOWER survey: women’s knowledge and awareness of treatment options for vulvar and vaginal atrophy remains inadequate. J Sex Med 2017;14:425–433. doi: 10.1016/j.jsxm.2017.01.011.
- Cumming GP, Herald J, Moncur R, et al. Women’s attitudes to hormone replacement therapy, alternative therapy and sexual health: a web-based survey. Menopause Int 2007;13:79–83. doi: 10.1258/175404507780796424.
- Cancelo Hidalgo MJ, Palacios S, del Pino P. Differences in perception of genitourinary syndrome of menopause by gynecologists and postmenopausal women in Spain. Prog Obstet Ginecol 2019;62:436–442.
- Cuerva MJ, Gonzalez D, Canals M, et al. The sexual health approach in postmenopause: the five-minutes study. Maturitas 2018;108:31–36. doi: 10.1016/j.maturitas.2017.11.009.
- Volpicelli Leonard K, Robertson C, Bhowmick A, et al. Perceived treatment satisfaction and effectiveness facilitators among patients with chronic health conditions: a self-reported survey. Interact J Med Res 2020;9:e13029. doi: 10.2196/13029.
- Bruyniks N, Biglia N, Palacios S, et al. Systematic indirect comparison of ospemifene versus local estrogens for vulvar and vaginal atrophy. Climacteric 2017;20:195–204. doi: 10.1080/13697137.2017.1284780.
- Reid RL, Black D, Derzko C, et al. Ospemifene: a novel oral therapy for vulvovaginal atrophy of menopause. J Obstet Gynaecol Can 2020;42:301–303. doi: 10.1016/j.jogc.2019.10.039.
- Goldstein SW, Winter AG, Goldstein I. Improvements to the vulva, vestibule, urethral meatus, and vagina in women treated with ospemifene for moderate to severe dyspareunia: a prospective vulvoscopic pilot study. Sex Med 2018;6:154–161. doi: 10.1016/j.esxm.2018.03.002.
