ABSTRACT
HIV serostatus disclosure plays an important role in HIV transmission risk reduction and is positively associated with HIV medication adherence and treatment outcomes. However, to date, no study has quantified the role of disclosure across the HIV treatment cascade, particularly in Sub-Saharan Africa. We used data from a cohort of HIV-infected adults in Northern Tanzania to describe associations between disclosure and engagement and retention in the HIV treatment cascade. Between 2008 and 2009, the Coping with HIV/AIDS in Tanzania (CHAT) study enrolled 260 clients newly diagnosed with HIV and 492 HIV-infected patients in established HIV care in two large HIV care and treatment centers in Northern Tanzania. Participants aged 18 and older completed annual clinical assessments and twice-annual in-person interviews for 3.5 years. Using logistic regression models, we assessed sociodemographic correlates of HIV serostatus disclosure to at least one household member, and associations between this disclosure measure and linkage to care, evaluation for antiretroviral therapy (ART) eligibility, ART coverage, and rates of undetectable HIV RNA levels during the follow-up period. Married individuals and those diagnosed earlier were more likely to have disclosed their HIV infection to at least one household member. During follow-up, HIV serostatus disclosure was associated with higher rates of linkage to care, evaluation for ART eligibility, and ART coverage. No significant association was observed with rates of undetectable viral loads. Marginal effects estimates suggest that a 10 percentage-point lower probability of linkage to care for those who did not disclose their HIV serostatus (86% vs. 96%; p = 0.035) was compounded by an 18 percentage-point lower probability of ever receiving a CD4 count (62% vs. 80%; p = .039), and a 20 percentage-point lower probability of ever receiving ART (55% vs. 75%; p = .029). If causal, these findings suggest an important role for disclosure assistance efforts across the HIV treatment cascade.
*CHAT Research Team: Bernard Agala, Amy Hobbie, Beatrice Lema, Yombya Madukwa, Restituta Mvungi, Wendy Ricky, Donna Safely, Ludovic Samora, and Blandina Zenze.
Introduction
Approximately 71% of persons living with HIV, or 24.7 million, are in Sub-Saharan Africa (SSA) (UNAIDS, Citation2014). Impressively, the number of AIDS-related deaths in SSA fell by 39% between 2005 and 2013 (UNAIDS, Citation2014), with the decrease attributed to increased access to antiretroviral therapy (ART) (UNAIDS, Citation2014). However, recent estimates suggest that only as few as 13% of infected persons initiated and have been retained on ART (Okeke, Ostermann, & Thielman, Citation2014).
The HIV treatment cascade is a framework designed to describe the steps necessary for effective treatment, from being tested for HIV, linked to care, retained in care, prescribed antiretroviral therapy, to attaining virologic suppression (AIDS.gov & U.S. Department of Health & Human Services, Citation2014; De Cock, Citation2014). As treatment options continue to expand in SSA and elsewhere, understanding barriers and facilitators of HIV care and treatment across the treatment cascade is critical in order to maximize the efficacy of HIV care programs.
HIV serostatus disclosure plays an important role in HIV transmission risk reduction and numerous studies have described associations between disclosure and elements of the HIV treatment cascade. Systematic reviews identified fear of disclosure as an important barrier to linkage to care (Govindasamy, Ford, & Kranzer, Citation2012) and highlighted the role of disclosure as an enabling factor in ART initiation, adherence, and retention (Hodgson et al., Citation2014). Several additional studies have described associations between HIV serostatus disclosure and virologic suppression (Labhardt et al., Citation2014; Muller, Bode, Myer, Stahl, & von Steinbuchel, Citation2011; Ramadhani et al., Citation2007; Teshome Yimer & Yalew, Citation2015). However, no study to date has quantified the role of disclosure across the elements of the HIV treatment cascade.
This analysis of HIV-infected Tanzanian adults examines associations of HIV serostatus disclosure to household members with indicators of linkage to care and treatment outcomes across the HIV treatment cascade. Specifically, in a cohort of persons newly diagnosed with HIV we explore the associations between disclosure and linkage to care, obtaining a CD4+ lymphocyte count (used in this context as an indicator of ever being evaluated for ART eligibility), and ART coverage; and in a cohort of patients in established care we explore associations with sustained virologic suppression.
Methods
Study participants
From November 2008 to October 2009, the Coping with HIV/AIDS in Tanzania (CHAT) observational cohort study sequentially enrolled 260 individuals newly diagnosed with HIV at voluntary HIV counseling and testing sites in Moshi, Tanzania, and randomly selected 492 HIV patients in established care at the regional public hospital or the private zonal referral hospital. Eligible participants were ages 18 and above. The goal of the CHAT study was to examine the influence of demographic and psychosocial characteristics on risk behaviors, health services utilization, and health outcomes among HIV-infected persons in Tanzania. The detailed sampling approach and study cohort characteristics have been previously described (Belenky et al., Citation2014; Ostermann et al., Citation2014; Pence et al., Citation2012; Thielman et al., Citation2014).
Data collection
Participants completed in-person interviews every 6 months for 3.5 years. Interviews, conducted in Kiswahili, assessed demographic and health characteristics, HIV treatment history, including linkage to care and ART, and HIV serostatus disclosure. Clinical assessments were conducted annually and included viral load measurements for participants on ART and a review of participants’ CD4+ lymphocyte counts from medical records.
Measures
HIV serostatus disclosure after 3.5 years was assessed using the question “How many of the people living with you in your household know that you are HIV positive?” Owing to variation in household sizes, responses were recoded to a binary variable indicating disclosure to at least one household member. While this indicator captures only a single dimension of disclosure and cannot characterize the complex processes involving the timing, means, intent, or targets of disclosure, it could be uniformly constructed across diverse living arrangements and household sizes, and thus used to analyze systematic variation in outcomes across participants.
Three elements of the HIV treatment cascade characterized newly diagnosed participants’ engagement in HIV care. First, the 3.5-year follow-up assessment included a review of all HIV care and treatment centers (CTCs) participants had ever attended. Linkage to care was defined as any visit to any CTC during the study period. Second, the availability of any CD4+ lymphocyte count was used as an indicator of whether newly diagnosed individuals had ever been evaluated for ART eligibility. Third, self-reports at the 3.5-year follow-up interview were used to describe whether individuals had ever been on ART.
For patients enrolled into the study while in established HIV care and who were on ART at least 6 months prior to baseline, virologic suppression was assessed by a binary variable describing whether patients had a consistently undetectable viral load, defined as all HIV RNA measurements during the study period below the detectable threshold of 150 copies/ml. This variable definition was chosen to account for variable patterns of participant follow-up and re-entry into the study and low rates of virologic failure at individual assessments.
Other characteristics, evaluated at baseline, included age, gender, education, rural vs. urban residence, time since diagnosis, number of lifetime partners, lifetime reports of commercial sex, physical and mental health as measured by the Short-Form 8 health survey (Ware, Kosinski, Dewey, & Gandek, Citation2001) and a composite score summarizing participants’ agreement with 12 stigma questions (Visser, Makin, Vandormael, Sikkema, & Forsyth, Citation2009).
Analysis
Descriptive statistics and multivariate logistic regression analysis were used to describe differences in disclosure rates between newly diagnosed individuals and those in established care, correlates of disclosure through the end of the 3.5-year study period, and associations between disclosure and the elements of the treatment cascade. Student's t-tests and Fisher's exact tests assessed the significance of bivariate associations; multivariate regression models were estimated with robust standard errors.
Ethics statement
Study activities were approved by the Kilimanjaro Christian Medical Center Institutional Review Board (IRB) in Tanzania and the Duke University Health System IRB in the USA. Written informed consent was obtained from all participants.
Results
summarizes participant characteristics at baseline, rates of HIV serostatus disclosure, and correlates of disclosure over time. Of 260 newly diagnosed participants, 175 were observed at the 3.5-year follow-up assessment. Among 492 patients in established care, 435 completed the final assessment.
Table 1. Participant characteristics at enrollment and HIV serostatus disclosure over time.
Newly diagnosed individuals and patients in established care exhibited significant differences in disclosure rates, both at enrollment (p < .001) and after 3.5 years of follow-up (p = .015). Among newly diagnosed individuals, rates of disclosure increased from 45% to 75% during the study period; among patients in established care rates increased from 74% to 84%. There was little systematic variation in disclosure with participant characteristics. Being married, time since diagnosis, and treatment at the regional public hospital (as opposed to the private zonal referral hospital) were associated with an increased likelihood of disclosure.
and show significant associations between disclosure and three of the four elements of the HIV treatment cascade evaluated. In bivariate analyses, rates of linkage to care, evaluation for ART eligibility, and ART coverage were higher among newly diagnosed individuals who reported disclosure to at least one household member. In multivariate analyses, disclosure to at least one household member was associated with higher rates of linkage to care (OR 4.75; 95% CI [1.11–20.26]; p = .035), assessment of ART eligibility (OR 2.60; [1.12–6.04]; p = .039) and ever having been on ART (OR 2.56; [1.13–5.79]; p = .029) during the 3.5-year follow-up period. Disclosure was not significantly associated with maintaining a consistently suppressed viral load among persons in established care and on ART at study enrollment.
Figure 1. HIV serostatus disclosure and engagement in HIV care during a 3.5-year follow-up period. Note: Statistical significance assessed using Fisher's exact test. 1Consistently undetectable viral load, threshold of 150 cells/mm3, in up to 4 assessments at baseline, 12, 24 and 36 months, fewer in the case of loss to follow-up; among participants who were on ART at least 180 days prior to enrollment.
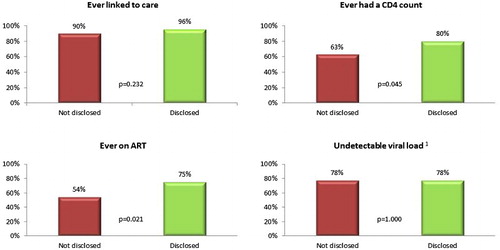
Table 2. HIV serostatus disclosure and retention in the HIV treatment cascade during a 3.5-year follow-up period.
Discussion
In a cohort of Tanzanian adults who were newly diagnosed with HIV infection, serostatus disclosure to at least one household member during a 3.5-year follow-up period was associated with higher rates of linkage to care, evaluation for ART eligibility, and ART treatment. While the causality of the observed associations could not be evaluated, the marginal effects estimates from the estimated models suggest that participants who did not disclose their HIV serostatus had a 10 percentage-point lower probability of linkage to care (86% vs. 96%; p = .035), compounded by an additional 18 percentage-point lower probability of ever receiving a CD4 count (62% vs. 80%; p = .039), and a 20 percentage-point lower probability of ever receiving ART (55% vs. 75%; p = .029) during the 3.5-year follow-up period. The findings are consistent with theoretical models of disclosure (Qiao, Li, & Stanton, Citation2013) and prior evidence on the role of stigma and fears of disclosure in limiting uptake and continuation of HIV treatment (Duff, Kipp, Wild, Rubaale, & Okech-Ojony, Citation2010; Hodgson et al., Citation2014; Medley, Garcia-Moreno, McGill, & Maman, Citation2004; Turan & Nyblade, Citation2013; Wolf et al., Citation2014). In conjunction with other literature on associations between disclosure, ART adherence, and virologic outcomes, and with appropriate caution regarding causal interpretations, these findings support further research on the positive impact that disclosure may have on HIV treatment outcomes.
We acknowledge several limitations. First, causal pathways of the observed associations could not be established. Second, selective loss to follow-up may have biased our estimates. Third, estimates may not be representative of other populations. Finally, by relying on basic dichotomous measures of disclosure and retention in the treatment cascade the study is unable to characterize the complexity underlying the observed relationships. The results thus lack detailed information that may inform disclosure interventions (Dima, Stutterheim, Lyimo, & de Bruin, Citation2014; Kennedy, Fonner, Armstrong, O'Reilly, & Sweat, Citation2015). CHAT was not designed or sufficiently powered to characterize the mechanisms underlying the observed associations.
Conclusion
Disclosure was associated with improved linkage to care, assessment for ART eligibility, and ART initiation, although not long-term viral suppression. If causal, these findings would suggest that efforts to support HIV-infected individuals in disclosure may have the potential to improve outcomes across the HIV treatment cascade.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- AIDS.gov, & U.S. Department of Health & Human Services. (2014). HIV/AIDS care continuum. Retrieved from http://www.aids.gov/federal-resources/policies/care-continuum/
- Belenky, N. M., Cole, S. R., Pence, B. W., Itemba, D., Maro, V., & Whetten, K. (2014). Depressive symptoms, HIV medication adherence, and HIV clinical outcomes in Tanzania: A prospective, observational study. PLoS One, 9(5), e95469. doi:10.1371/journal.pone.0095469
- De Cock, K. M. (2014). Editorial commentary: Plus ca change … Antiretroviral therapy, HIV prevention, and the HIV treatment cascade. Clinical Infectious Diseases, 58(7), 1012–1014. doi:10.1093/cid/ciu026
- Dima, A. L., Stutterheim, S. E., Lyimo, R., & de Bruin, M. (2014). Advancing methodology in the study of HIV status disclosure: The importance of considering disclosure target and intent. Social Science & Medicine, 108, 166–174. doi:10.1016/j.socscimed.2014.02.045
- Duff, P., Kipp, W., Wild, T. C., Rubaale, T., & Okech-Ojony, J. (2010). Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. Journal of the International AIDS Society, 13, 37. doi:10.1186/1758-2652-13-37
- Govindasamy, D., Ford, N., & Kranzer, K. (2012). Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: A systematic review. AIDS, 26(16), 2059–2067. doi: 10.1097/QAD.0b013e3283578b9b
- Hodgson, I., Plummer, M. L., Konopka, S. N., Colvin, C. J., Jonas, E., Albertini, J., … Fogg, K. P. (2014). A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One, 9(11), e111421. doi: 10.1371/journal.pone.0111421
- Kennedy, C. E., Fonner, V. A., Armstrong, K. A., O'Reilly, K. R., & Sweat, M. D. (2015). Increasing HIV serostatus disclosure in low and middle-income countries: a systematic review of intervention evaluations. AIDS, 29( Suppl 1), S7–S23. doi:10.1097/QAD.0000000000000671
- Labhardt, N. D., Bader, J., Ramoeletsi, M., Kamele, M., Lejone, T. I., Cheleboi, M., … Klimkait, T. (2014). Clinical and socio-demographic predictors for virologic failure in rural Southern Africa: Preliminary findings from CART-1. Journal of the International AIDS Society, 17(4 Suppl 3), 19666. doi: 10.7448/IAS.17.4.19666
- Medley, A., Garcia-Moreno, C., McGill, S., & Maman, S. (2004). Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organisation, 82(4), 299–307.
- Muller, A. D., Bode, S., Myer, L., Stahl, J., & von Steinbuchel, N. (2011). Predictors of adherence to antiretroviral treatment and therapeutic success among children in South Africa. AIDS Care, 23(2), 129–138. doi:10.1080/09540121003758523
- Okeke, L., Ostermann, J., & Thielman, N. M. (2014). Enhancing linkage and retention in HIV care: A review of interventions for highly resourced and resource-poor settings. Current HIV/AIDS Reports. doi:10.1007/s11904-014-0233-9
- Ostermann, J., Whetten, K., Reddy, E., Pence, B., Weinhold, A., Itemba, D., … Team, C. R. (2014). Treatment retention and care transitions during and after the scale-up of HIV care and treatment in Northern Tanzania. AIDS Care, 26(11), 1352–1358. doi:10.1080/09540121.2014.882493
- Pence, B. W., Shirey, K., Whetten, K., Agala, B., Itemba, D., Adams, J., … Shao, J. (2012). Prevalence of psychological trauma and association with current health and functioning in a sample of HIV-infected and HIV-uninfected Tanzanian adults. PLoS One, 7(5), e36304. doi:10.1371/journal.pone.0036304
- Qiao, S., Li, X., & Stanton, B. (2013). Theoretical models of parental HIV disclosure: A critical review. AIDS Care, 25(3), 326–336. doi:10.1080/09540121.2012.712658
- Ramadhani, H. O., Thielman, N. M., Landman, K. Z., Ndosi, E. M., Gao, F., Kirchherr, J. L., … Crump, J. A. (2007). Predictors of incomplete adherence, virologic failure, and antiviral drug resistance among HIV-infected adults receiving antiretroviral therapy in Tanzania. Clinical Infectious Diseases, 45(11), 1492–1498. doi:10.1086/522991
- Teshome Yimer, Y., & Yalew, A. W. (2015). Magnitude and predictors of anti-retroviral treatment (ART) failure in private health facilities in Addis Ababa, Ethiopia. PLoS One, 10(5), e0126026. doi:10.1371/journal.pone.0126026
- Thielman, N. M., Ostermann, J., Whetten, K., Whetten, R., Itemba, D., Maro, V., … Team, C. R. (2014). Reduced adherence to antiretroviral therapy among HIV-infected Tanzanians seeking cure from the Loliondo healer. JAIDS Journal of Acquired Immune Deficiency Syndromes, 65(3), e104–e109. doi:10.1097/01.qai.0000437619.23031.83
- Turan, J. M., & Nyblade, L. (2013). HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: A review of the evidence. AIDS and Behavior, 17(7), 2528–2539. doi:10.1007/s10461-013-0446-8
- UNAIDS. (2014). The GAP Report. Geneva, Switzerland.
- Visser, M. J., Makin, J. D., Vandormael, A., Sikkema, K. J., & Forsyth, B. W. (2009). HIV/AIDS stigma in a South African community. AIDS Care, 21(2), 197–206. doi:10.1080/09540120801932157
- Ware, J. E., Kosinski, M., Dewey, J. E., & Gandek, B. (2001). How to score and interpret Single-item health status measures: A manual for users of the SF-8 Health Survey: (with a Supplement on the SF-6 Health Survey): QualityMetric, Incorporated.
- Wolf, H. T., Halpern-Felsher, B. L., Bukusi, E. A., Agot, K. E., Cohen, C. R., & Auerswald, C. L. (2014). It is all about the fear of being discriminated [against] … the person suffering from HIV will not be accepted: A qualitative study exploring the reasons for loss to follow-up among HIV-positive youth in Kisumu, Kenya. BMC Public Health, 14, 1154. doi:10.1186/1471-2458-14-1154
