ABSTRACT
Orphans and separated children (OSC) are a vulnerable population whose numbers are increasing, particularly in sub-Saharan Africa and Asia. Over 153 million children worldwide have lost one or both parents, including 17 million orphaned by AIDS, and millions more have been separated from their parents. As younger orphans enter adolescence, their sexual health and HIV-related risk behaviors become key considerations for their overall health. Importantly, their high prevalence of exposure to potentially traumatic events (PTEs) may put OSC at additional risk for adverse sexual health outcomes. The Positive Outcomes for Orphans study followed OSC randomly sampled from institution-based care and from family-based care, as well as a convenience sample of non-OSC, at six sites in five low-and middle-income countries. This analysis focused on the 90-month follow-up, during which adolescents 16 and older were assessed for sexual health, including age at sexual debut, past-year sex, past-year condom use, and perceptions of condom use. We specifically examined the relationship between PTEs and sexual health outcomes. Of the 1258 OSC and 138 non-OSC assessed, 11% reported ever having sex. Approximately 6% of participants reported recent sex and 5% reported having recent unprotected sex. However, 70% of those who had recent sex reported that they did not use a condom every time, and perceptions of condom use tended to be unfavorable for protection against sexual risk behavior. Nearly all (90%) of participants reported experiencing at least one lifetime PTE. For those who experienced “any” PTE, we found increased prevalence of recent sex (PR = 1.39 [0.47, 4.07]) and of recent unprotected sex (PR = 3.47 [0.60, 19.91]). This study highlights the need for caregivers, program managers, and policymakers to promote condom use for sexually active OSC and identify interventions for trauma support services. Orphans living in family-based care may also be particularly vulnerable to early sexual debut and unprotected sexual activity.
Introduction
Orphans and separated children (OSC) are a vulnerable population whose numbers are increasing, particularly in sub-Saharan Africa and Asia (UNICEF, Citation2012). Over 153 million children worldwide have lost one or both parents, including 17 million orphaned by AIDS, and millions more have been separated from their parents due to abandonment, war, or other such circumstances. Providing supportive services for this large number of orphans through childhood and adolescence has become a major challenge for individual governments and international donors (UNICEF, Citation2009).
As younger orphans enter adolescence, their sexual health and HIV-related risk behaviors become key health considerations. Earlier sexual debut has been associated with forced sex, older partners, lower educational attainment, multiple lifetime partners, and reduced probability of condom use at most recent sexual encounter, all of which increase risk of acquiring HIV or other sexually transmitted diseases (Hallett et al., Citation2007; Lugoe, Klepp, & Skutle, Citation1996; Pettifor, O'Brien, Macphail, Miller, & Rees, Citation2009; Pettifor, van der Straten, Dunbar, Shiboski, & Padian, Citation2004). Some research has shown earlier sexual debut among maternal and double orphans, but has been limited to single-country studies (Birdthistle et al., Citation2008; McGrath, Nyirenda, Hosegood, & Newell, Citation2009; Mkandawire, Tenkorang, & Luginaah, Citation2013; Thurman, Brown, Richter, Maharaj, & Magnani, Citation2006). Palermo et al. found an association between orphanhood and earlier sexual debut using the Demographic and Health Surveys (DHS), but data were limited to females 17–19 (Palermo & Peterman, Citation2009).
OSC may be at particular risk for poor sexual health due not only to loss of their parents but also to increased exposure to other potentially traumatic experiences (PTEs) (Whetten, Ostermann, Whetten, O'Donnell, & Thielman, Citation2011). PTEs such as exposure to violence and sexual abuse have been associated with sexual health risk among adolescents in other populations (Cedar Project et al., Citation2008; Wilson, Woods, Emerson, & Donenberg, Citation2012). Further, trauma has been associated with outcomes such as depression and anxiety, as well as with poor coping and reduced social functioning, all of which have been shown to predict risk behaviors, including sexual risk behaviors, in adolescents (Okello, Nakimuli-Mpungu, Musisi, Broekaert, & Derluyn, Citation2013; Talbot et al., Citation2013). Given the high prevalence of trauma in general and abuse in particular in the OSC population (Gray et al, Citation2015a; Whetten et al., Citation2011), sexual debut and perceptions of safer sex behaviors among OSC may be affected by those earlier traumas.
The unique experience of OSC, coupled with their increased vulnerability to adverse health outcomes including HIV infection, necessitates a better understanding of their sexual health behaviors. Associations between PTEs and sexual health are of particular interest given that PTEs are highly prevalent in OSC in low- and middle-income countries (LMIC), PTEs have been linked to sexual health in other adolescent populations, and adolescent OSC in LMIC are disproportionately exposed to HIV. The Positive Outcomes for Orphans (POFO) study longitudinally followed OSC randomly sampled from both institution-based care and family-based care for 90 months. Here, we examine multiple aspects of sexual health behavior at 90-month follow-up among older adolescents and young adults, with emphasis on exploring the association of lifetime trauma history with current sexual practices. The results will inform interventions around sexual health as well as policies aimed at caring for the increasing OSC population.
Methods
Recruitment
The POFO study is a longitudinal study conducted at six sites in five LMIC: Battambang District, Cambodia; Addis Ababa, Ethiopia; Hyderabad, India; Nagaland, India; Bungoma District, Kenya; and Kilimanjaro Region, Tanzania. These six sites were selected to reflect geographic, political, religious, and cultural diversity of places OSC live.
OSC are children who have had one or both parents die (orphaned) or who have been separated from one or both parents due to abandonment, war, or other such circumstances, with no expectation of reunification with the parent(s). At baseline, OSC between ages 6–12 were enrolled from two groups: those living in institution-based care and those living in family-based care. At each study site, 250 OSC were randomly sampled from a comprehensive list of institutions, defined as structures housing children from at least two different families and at least five total children. An additional 250 family-dwelling OSC were randomly sampled from families in 50 geographic clusters defined at each site. Community lists or house-to-house census enabled identification of households for random selection. Finally, a convenience sample of 50 non-OSC was enrolled from the same geographic areas as the family-based OSC, providing a non-orphan qualitative comparison group from the same region. Additional sampling details are defined elsewhere (Whetten et al., Citation2009, Citation2011).
Baseline data collection occurred between May 2006 and February 2008, depending on site. Surveys were administered verbally in the child's native language by gender-specific interviewers who underwent substantial training and observation before being certified to conduct interviews. The current analysis focuses on participants at the 90-month follow-up, when measures of sexual health were added for participants who were ≥16 years old.
Measures
Sexual health
Participants who were at least 16 years of age were asked if they had ever had a sexual partner (yes or no), and were then asked the age at which they first had vaginal or anal sex. Interviewers specified that the sex could have been either consensual or forced. Due to cultural differences surrounding the assessment of age, in some cases children who were 15 were considered “older” and responded to questions targeting older children; in those instances, their information was retained in the analysis. This phenomenon occurred at all sites.
Participants who reported ever having sex were also asked if they had vaginal or anal sex in the past year (recent sex) and if so, if they had used a condom “never”, “some of the time”, “most of the time”, or “every time”. We collapsed those responses into a dichotomous variable that identified whether the participant had any unprotected sex in the past year (0 = used a condom every time, 1 = used a condom never, some, or most of the time). We did this for several reasons: (1) the overall outcome prevalence for unprotected sex was low and further splitting the data would produce imprecise estimates, (2) prior precedent for dichotomization (Pence et al., Citation2010, Citation2012), and importantly, (3) substantive interest in describing behavior that puts adolescents at risk of HIV. Any unprotected sex elevates risk, particularly in areas with relatively high HIV prevalence. For both the recent sex and unprotected sex variables, participants who had already indicated they had never had sex were coded as 0.
Additionally, participants were asked if they had ever heard of condoms and about their perceptions of peer norms surrounding condom use. Peer norms were assessed with a series of seven questions such as “People I know talk about condoms with a partner”; answers were recorded on a 4-point Likert scale from 0 = “strongly disagree” to 3 = “strongly agree”. The scale constructed from these seven items had high internal consistency (Cronbach's alpha 0.91), and an exploratory factor analysis showed strong support for a single factor. Participants with missing data on up to two questions were assigned a score reflecting the mean of the answered items, as recommended to produce the most valid estimates possible (Siddiqui, Citation2015).
Potentially traumatic experiences
We assessed PTEs with the Life Events Checklist (LEC), which includes a 17-item list of “things I have seen and heard”. The LEC has been used cross-culturally and validated in multiple populations (Elhai, Gray, Kashdan, & Franklin, Citation2005; Gray, Litz, Hsu, & Lombardo, Citation2004). Participants indicated whether they had experienced each event never, once, or more than once. They further indicated whether the event occurred in the past year, prior to the past year, or both. Because we were interested in lifetime trauma, we considered the event to be endorsed if it occurred one or more times, at any point in the past year or prior to the past year.
For consistency across POFO studies (Gray et al., Citation2015a, Citation2015b; Whetten et al., Citation2011), and in keeping with similar work (Mugavero et al., Citation2006), we collapsed the 17 PTEs into six mutually exclusive categories: (i)disasters or accidents, (ii) war, riots, or killings, (iii) physical or sexual abuse, (iv) witnessing violence in the care setting, (v) witnessing family death, and (vi) being forced to the care setting. Endorsement of any item in a category was coded as endorsement of the category. Because parental death or separation was the defining characteristic for the OSC population, it was not considered a PTE, unless the participant was present at the death and watched the death happen, in which case an item in the category “witnessing family death” was included. We additionally defined “any” trauma as endorsement of any of the six trauma categories. We also calculated a continuous trauma score (“total trauma”) ranging from 0 to 17 representing a sum of traumas experienced by the child.
Covariates
We included several covariates in our analyses: gender (male as referent), study site (Kenya as the referent because it had the greatest number having initiated sex), orphan type (institution-dwelling OSC (referent), family-dwelling OSC, non-OSC), OSC status (both parents alive (referent), one parent deceased, both parents deceased), age in years (continuous), grade-for-age (continuous), and ever alcohol use (binary). Updates to OSC status before 90-month follow-up were incorporated into adjusted analyses.
Grade-for-age reflected the departure from expected educational achievement given the participant's age. On-target was given a value of 0; below-target was assigned a negative value reflecting the number of years behind; and above-target was assigned a positive value reflecting the number of years ahead. The highest expected attainment in this population is 12 years. Assuming schooling began at age 5, maximum attainment was expected at age 17; therefore, “on-target” was 12 years for anyone ≥17.
Alcohol use was specified as drinking “more than a few sips” and excluded drinking for religious purposes. Most respondents were non-drinkers, so we dichotomized alcohol use into a binary variable (0 = never, 1 = ever).
Analyses
To estimate the prevalence of sexual debut by age, we used Kaplan–Meier survival methods. Figures are presented as failure (1 – survival) curves to reflect the proportion who had initiated sex by each age. Participants contributed person-time at risk until the age at which they first had sex. Those who reported never having engaged in sexual intercourse contributed person-time at risk until their current age in years, at which point they were censored. We present sexual initiation by age curves for the whole population as well as stratified by gender, study site, and orphan type (institution-dwelling OSC, family-dwelling OSC, and non-OSC). We additionally examined trauma experienced by age 12 as a predictor of age of sexual debut after age 13. To ensure temporality between exposure and outcome, we excluded OSC who initiated sex before age 13. We present sexual initiation by age curves stratified by any trauma (any vs. none) and by abuse (any vs. none) by age 12.
We estimated the prevalence (or mean) of each of the four sexual health outcomes (any recent sex, any unprotected recent sex, ever heard of condoms, and condom norms) for each level of each of the key study characteristics (site, gender, OSC type, OSC status, alcohol use, and age) to explore variation in outcomes among key characteristics. For binary outcomes, we used log-binomial regression to estimate prevalences and 95% confidence intervals (CIs); for the continuous outcome, we used linear regression to estimate means and 95% CIs. We then estimated the association between each of the trauma categories and each sexual health outcome, controlling for the above-described covariates.
All models were weighted to account for the complex survey design, including stratification by site and clustering by sampling unit (institution or geographic cluster of families), as detailed elsewhere (Whetten et al., Citation2009). Sampling weights for institution-based OSC were calculated as the inverse of the product of the probabilities of selection at the institution and child levels; the enumerated lists of institutions and children in each study region enabled calculation of those probabilities. Because the overall population sizes for family-based OSC and non-OSC were unknown, such probabilities could not be calculated; each subject was therefore assigned a weight of 1, as in prior analyses (Whetten et al., Citation2009, Citation2014).
The Duke University Institutional Review Board (IRB) as well as local IRBs at each site approved this study. Primary caretakers or institutional administrators provided consent at baseline and when survey changes were made; all subjects provided assent until they could provide consent at 18. Site-specific protocols were developed for handling reports or observations of abuse or other adverse events.
Analyses were conducted in Stata 13 (StataCorp, Citation2013).
Results
At 90-month follow-up, 1258 OSC and 138 non-OSC were assessed (). Participant ages ranged from 15–20 years, (mean 17.1; standard deviation 1.2). Among OSC, 44% were institution-dwelling and 56% were family-dwelling. The gender distribution was similar across the three types of children (56% male institution-dwelling OSC, 54% male family-dwelling OSC and 46% male non-OSC). Double orphans were more likely to be in institution-based care (40%) than family-based care (18%). By 90-month follow-up, most participants had attained at least eight years of education.
Table 1. Characteristics of older adolescents in the POFO study population at 90-month follow-up.
Most participants (89%) reported they had never had vaginal or anal sex (). By age 15, less than 10% of the overall sample had initiated sexual activity (). The cumulative proportion of sexual initiation by age 20 was approximately 25%. Stratified Kaplan–Meier estimates showed slightly earlier sexual debut among males, with the gap narrowing as age approached 20. Kenyan and Tanzanian participants showed earlier sexual debut compared to the other four sites. Family-dwelling OSC reported earlier sexual debut than either institution-dwelling OSC or non-OSC, a gap that persisted at age 20. We observed no differences in age of sexual debut associated with any trauma or with abuse by age 12.
Figure 1. (a–f) Age at first intercourse among adolescents >=16 years old, overall (a) and stratified by gender (b), site (c) and setting (d), any trauma before age 12, (e) and any abuse before age 12 (f).
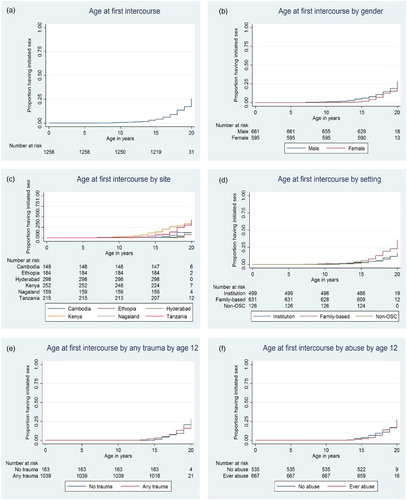
Table 2. Distribution of sexual health outcomes and potentially trauma exposure experience variables.
Approximately 6% of participants reported recent (past-year) sex. While only 4% of the total sample reported having unprotected sex, 70% of those who had recent sex reported they did not use a condom every time. Mean agreement with statements about condom use norms were neutral, closer to disagreement on the 0–3 scale, indicating that participants were less likely to perceive their peers as using or talking about condoms with their partners.
Nearly all (90%) of participants reported experiencing at least one lifetime PTE; the most common was witnessing family death.
Prevalence and mean estimates indicate variation in sexual health across many subgroups (). Kenya and Tanzania had the highest prevalence of recent sex, recent unprotected sex, and condom awareness. However, other sites had more favorable condom use perceptions, with the exception of Ethiopia. Females generally had slightly less favorable outcomes than males. Family-based OSC had much higher prevalence of recent sex and recent unprotected sex compared to institution-based OSC, but had more favorable condom use perceptions. Older age and any alcohol use both had higher prevalence of recent sex and unprotected sex; both also had more favorable condom use perceptions.
Table 3. Prevalence of sexual health outcomes by key characteristics.
Multivariable associations showed increased prevalence of recent sex for those who experienced “any” PTE (PR = 1.39 [0.47, 4.07]) (). Most individual trauma categories were also associated with increased prevalence of recent sex. Estimates of unprotected sex in the past year followed a similar pattern; the magnitude of association with “any” PTE was high (PR = 3.47 [0.60, 19.91]). The imprecision reflected in the CI is due to the high trauma prevalence: only 1 subject who reported having unprotected sex was unexposed to “any” trauma.
Table 4. Multivariable associations between trauma types and sexual health outcomes.
Exposure to “any” PTE, nearly all categories of PTEs, and increasing “total trauma” were associated with having heard of condoms. Increased favorability in perceptions of condom use norms was associated with “any” PTE and all categories of PTEs, though only family violence was statistically significant.
Discussion
We found that less than 10% of OSC and non-OSC reported ever having sex by age 15. While overall prevalence of recent (past-year) sex was fairly low (6%), the prevalence of unprotected sex among those who had recent sex was high (70%). Exposure to trauma, particularly war, riots and killings and “any trauma” was associated with recent sex and recent unprotected sex. All trauma exposures were slightly positively associated with perceptions of condom use. However, overall perceptions of safer sex norms were generally unfavorable.
These findings suggest the need to improve awareness of and comfort with sexual health among adolescents in LMIC, where HIV prevalence is high. For context, estimated adult (ages 15–49) HIV prevalence in 2014 was: Cambodia (0.6%), Ethiopia (1.2%), India (0.3%), Kenya (5.3%), and Tanzania (5.3%) (World Bank, Citation2012; UNAIDS, Citation2012). Though most report not having sex and most report having heard of condoms, the vast majority of sexually active adolescents are not always using condoms.
Furthermore, OSC are in need of protective and support services regarding PTEs. Abuse is of particular concern for sexual risk behavior that can increase the probability of acquiring HIV, and recent findings indicate boys are as vulnerable as girls to physical and sexual abuse (Gray et al., Citation2015b), suggesting programs for boys are as greatly needed as those for girls. Surprisingly, neither any trauma by age 12 nor abuse by age 12 predicted age of sexual debut, possibly due to generally low prevalence of sexual activity. However, our findings do suggest increased prevalence of unprotected sex associated with any trauma and with physical or sexual abuse. In general, PTEs are strongly associated with depression, anxiety, poor coping, and reduced social functioning in children and adolescents; these outcomes in turn increase risk of maladaptive behaviors including sexual risk-taking (Okello et al., Citation2013; Pynoos, Steinberg, & Piacentini, Citation1999; Talbot et al., Citation2013). Promising intervention studies have suggested that evidence-based, locally feasible support such as trauma-focused cognitive behavioral therapy may reduce negative symptomatology from PTEs in LMIC (Murray et al., Citation2014; O'Donnell et al., Citation2014).
A noteworthy finding is that OSC in institution-based care were less likely to report having recent sex or recent unprotected sex than non-OSC or OSC in family-based care. Family-dwelling OSC also reported earlier sexual debut. In general, the growing OSC population is resulting in additional economic constraints and increasing caregiver burden felt by families in LMIC (Heymann, Earle, Rajaraman, Miller, & Bogen, Citation2007; Kidman & Thurman, Citation2014; Miller, Gruskin, Subramanian, Rajaraman, & Heymann, Citation2006). Studies have reported that economically constrained or inadequate orphan care in resource-poor areas can contribute to child- or sibling-headed households, increased child labor, reduced school attendance, and reduced educational attainment, all of which are associated with increased sexual health risk (Birdthistle et al., Citation2009; Case, Paxson, & Abledinger Citation2004; Cluver, Orkin, Boyes, Gardner, & Meinck, Citation2011; Dalen, Nakitende, & Musisi, Citation2009; Daniel & Mathias, Citation2012).
Our study has several strengths. The sample was statistically drawn to be representative of both institution-dwelling and family-dwelling OSC at six sites in five LMIC; an additional convenience sample of non-OSC was identified as a qualitative comparison group. Furthermore, the POFO study has high overall retention: 82% at 36-month follow-up and 69% at 90-month follow-up. We attribute this to dedicated study staff and the rapport interviewers built with study participants. Although the current analysis draws primarily on the 90-month follow-up interview due to the recent introduction of sexual health questions, the longitudinal nature of the study has created long-standing rapport between participants and interviewers, allowing sensitive questions such as those used here to be asked. Importantly, we documented rates of sexual debut across multiple geographically and politically diverse LMIC, across male and female genders, and across multiple ages of adolescence.
This study has several limitations. First, the cross-sectional nature of the current analysis prevents complete temporal assessment. Because trauma exposures are lifetime measures and sexual risk was assessed within the past-year, it is reasonable to assume that most trauma experiences occurred before the sexual risk behaviors, though reverse causality cannot be ruled out. Second, we used self-reported traumatic events and sexual health behaviors. However, a prior study in this population showed that caregiver reports under-reported traumatic experiences (Rajan et al., Citation2014). The sensitive nature of sexual behavior questions can result in reporting more socially desirable answers. Substantial efforts were made to enhance the validity of self-reported data, including matching participants with an interviewer of the same gender, pairing participants with the same interviewer over time, and reminding participants at key points that their responses were confidential. Many respondents did not answer the safer sex peer norms questions. We investigated possible selection bias; responses were non-differential by gender, age, or OSC type, but were differential by site. Nagaland had a very low response percentage (4%); sensitivity analyses excluding Nagaland negligibly changed estimates and conclusions remained the same. The topic may be particularly sensitive there, warranting consideration when formulating educational programs. Finally, measuring PTEs can be difficult, particularly across cultural settings. The LEC was selected for its ability to predict anxiety and depression and its wide use across different cultural settings (Elhai et al., Citation2005).
Healthy sexual behaviors are critically important for adolescents in all settings, but OSC in areas with high prevalence of HIV/AIDS are particularly vulnerable to adverse consequences of risky sexual behavior. This study highlights the need for caregivers, program managers, and policymakers to normalize condom use and identify interventions for trauma support services. Orphans living in family-based care may be particularly vulnerable to early sexual debut and unprotected sexual activity.
Acknowledgements
We acknowledge the following individuals for their essential contributions in study implementation and data collection: Chris Bernard Agala, BA, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States of America; Misganaw Eticha Dubie, MA, Stand for Vulnerable Organization, Addis Ababa, Ethiopia; Dafrosa Itemba, MSc, Tanzania Women Research Foundation, Moshi, Tanzania; Mao Lang and Vanroth Vann, MBA, Homeland (Meatho Phum Ko'mah), Battambang, Cambodia; Dean Lewis, Venkata Gopala Krishna Kaza, MA, and Ira Madan, MA, Sahara Centre for Residential Care & Rehabilitation, Delhi, India; and Augustine Wasonga, MA, MBA, Ace Africa, Bungoma, Kenya.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Birdthistle, I., Floyd, S., Nyagadza, A., Mudziwapasi, N., Gregson, S., & Glynn, J. R. (2009). Is education the link between orphanhood and HIV/HSV-2 risk among female adolescents in urban Zimbabwe? Social Science & Medicine, 68(10), 1810–1818. doi: 10.1016/j.socscimed.2009.02.035
- Birdthistle, I. J., Floyd, S., Machingura, A., Mudziwapasi, N., Gregson, S., & Glynn, J. R. (2008). From affected to infected? Orphanhood and HIV risk among female adolescents in urban Zimbabwe. AIDS, 22(6), 759–766. doi: 10.1097/QAD.0b013e3282f4cac700002030-200803300-00011
- Case, A., Paxson, C., & Ableidinger, J. (2004). Orphans in Africa: Parental death, poverty, and school enrollment. Demography, 41(3), 483–508. doi: 10.1353/dem.2004.0019
- Cedar Project, P., Pearce, M. E., Christian, W. M., Patterson, K., Norris, K., Moniruzzaman, A., … Spittal, P. M. (2008). The Cedar Project: Historical trauma, sexual abuse and HIV risk among young Aboriginal people who use injection and non-injection drugs in two Canadian cities. Social Science Medicine, 66(11), 2185–2194. doi: 10.1016/j.socscimed.2008.03.034S0277-9536(08)00178-0[pii]
- Cluver, L., Orkin, M., Boyes, M., Gardner, F., & Meinck, F. (2011). Transactional sex amongst AIDS-orphaned and AIDS-affected adolescents predicted by abuse and extreme poverty. JAIDS Journal of Acquired Immune Deficiency Syndromes, 58(3), 336–343. doi: 10.1097/QAI.0b013e31822f0d82
- Dalen, N., Nakitende, A. J., & Musisi, S. (2009). “They don't care what happens to us.” The situation of double orphans heading households in Rakai District, Uganda. BMC Public Health, 9, 321. doi: 10.1186/1471-2458-9-321
- Daniel, M., & Mathias, A. (2012). Challenges and coping strategies of orphaned children in Tanzania who are not adequately cared for by adults. African Journal of AIDS Research, 11(3), 191–201. doi: 10.2989/16085906.2012.734978
- Elhai, J. D., Gray, M. J., Kashdan, T. B., & Franklin, C. L. (2005). Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects? A survey of traumatic stress professionals. Journal of Traumatic Stress, 18(5), 541–545. doi: 10.1002/jts.20062
- Gray, C. L., Pence, B. W., Ostermann, J., Whetten, R. A., O'Donnell, K., Thielman, N., & Whetten, K. (2015a). Prevalence and incidence of traumatic experiences among orphans in institutional and family-based care settings in five LMIC: A longitudinal study. Global Health: Science and Practice, 3(3), 395–404. Published online 2015 Aug 25. doi: 10.9745/GHSP-D-15-00093
- Gray, C. L., Pence, B. W., Ostermann, J., Whetten, R. A., O'Donnell, K., Thielman, N., & Whetten, K. (2015b). Gender (in)differences in prevalence and incidence of traumatic experiences among orphaned and separated children living in five low and middle income countries. Global Mental Health, 1–11. doi: 10.1017/gmh.2015.1
- Gray, M. J., Litz, B. T., Hsu, J. L., & Lombardo, T. W. (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. doi: 11/4/330[pii]10.1177/1073191104269954
- Hallett, T. B., Lewis, J. J., Lopman, B. A., Nyamukapa, C. A., Mushati, P., Wambe, M., … Gregson, S. (2007). Age at first sex and HIV infection in rural Zimbabwe. Studies in Family Planning, 38(1), 1–10. doi: 10.1111/j.1728-4465.2007.00111.x
- Heymann, J., Earle, A., Rajaraman, D., Miller, C., & Bogen, K. (2007). Extended family caring for children orphaned by AIDS: Balancing essential work and caregiving in a high HIV prevalence nations. AIDS Care, 19(3), 337–345. doi: 10.1080/09540120600763225
- Kidman, R., & Thurman, T. R. (2014). Caregiver burden among adults caring for orphaned children in rural South Africa. Vulnerable Children and Youth Studies, 9(3), 234–246. doi: 10.1080/17450128.2013.871379
- Lugoe, W. L., Klepp, K. I., & Skutle, A. (1996). Sexual debut and predictors of condom use among secondary school students in Arusha, Tanzania. AIDS Care, 8(4), 443–452. doi: 10.1080/09540129650125632C44WK8B82T8ERYHT[pii]
- McGrath, N., Nyirenda, M., Hosegood, V., & Newell, M. L. (2009). Age at first sex in rural South Africa. Sexually Transmitted Infections, 85(Suppl 1), i49–i55. doi: 10.1136/sti.2008.03332485/Suppl_1/i49[pii]
- Miller, C. M., Gruskin, S., Subramanian, S. V., Rajaraman, D., & Heymann, S. J. (2006). Orphan care in Botswana's working households: Growing responsibilities in the absence of adequate support. American Journal of Public Health, 96(8), 1429–1435. doi: 10.2105/AJPH.2005.072280
- Mkandawire, P., Tenkorang, E., & Luginaah, I. N. (2013). Orphan status and time to first sex among adolescents in northern Malawi. AIDS and Behavior, 17(3), 939–950. doi: 10.1007/s10461-011-0120-y
- Mugavero, M., Ostermann, J., Whetten, K., Leserman, J., Swartz, M., Stangl, D., & Thielman, N. (2006). Barriers to antiretroviral adherence: The importance of depression, abuse, and other traumatic events. AIDS Patient Care and STDs, 20(6), 418–428. doi: 10.1089/apc.2006.20.418
- Murray, L. K., Skavenski, S., Michalopoulos, L. M., Bolton, P. A., Bass, J. K., Familiar, I., … Cohen, J. (2014). Counselor and client perspectives of Trauma-focused Cognitive Behavioral Therapy for children in Zambia: A qualitative study. Journal of Clinical Child and Adolescent Psychology, 43(6), 902–914. doi: 10.1080/15374416.2013.859079
- O'Donnell, K., Dorsey, S., Gong, W., Ostermann, J., Whetten, R., Cohen, J. A., … Whetten, K. (2014). Treating maladaptive grief and posttraumatic stress symptoms in orphaned children in Tanzania: Group-based trauma-focused cognitive-behavioral therapy. Journal of Traumatic Stress, 27(6), 664–671. doi: 10.1002/jts.21970
- Okello, J., Nakimuli-Mpungu, E., Musisi, S., Broekaert, E., & Derluyn, I. (2013). War-related trauma exposure and multiple risk behaviors among school-going adolescents in Northern Uganda: The mediating role of depression symptoms. Journal of Affective Disorders, 151(2), 715–721. doi: 10.1016/j.jad.2013.07.030
- Palermo, T., & Peterman, A. (2009). Are female orphans at risk for early marriage, early sexual debut, and teen pregnancy? Evidence from sub-Saharan Africa. Studies in Family Planning, 40(2), 101–112. doi: 10.1111/j.1728-4465.2009.00193.x
- Pence, B. W., Raper, J. L., Reif, S., Thielman, N. M., Leserman, J., & Mugavero, M. J. (2010). Incident stressful & traumatic life events and HIV sexual transmission risk behaviors in a longitudinal, multi-site cohort study. Psychosomatic Medicine, 72(7), 720–726. PMCID: PMC3691861 doi: 10.1097/PSY.0b013e3181e9eef3
- Pence, B. W., Shirey, K., Whetten, K., Agala, B., Itemba, D., Adams, J., … Shao, J. (2012). Prevalence of psychological trauma and association with current health and functioning in a sample of HIV-infected and HIV-uninfected Tanzanian Adults. PLoS One, 7(5), e36304. PMCID: PMC335144 [pii] doi: 10.1371/journal.pone.0036304
- Pettifor, A., O'Brien, K., Macphail, C., Miller, W. C., & Rees, H. (2009). Early coital debut and associated HIV risk factors among young women and men in South Africa. International Perspectives on Sexual and Reproductive Health, 35(2), 82–90. doi: 10.1363/ifpp.35.082.093508209
- Pettifor, A. E., van der Straten, A., Dunbar, M. S., Shiboski, S. C., & Padian, N. S. (2004). Early age of first sex: A risk factor for HIV infection among women in Zimbabwe. AIDS, 18(10), 1435–1442. doi: 00002030-200407020-00010[pii]
- Pynoos, R. S., Steinberg, A. M., & Piacentini, J. C. (1999). A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological Psychiatry, 46(11), 1542–1554. doi: 10.1016/S0006-3223(99)00262-0
- Rajan, D. G., Shirey, K., Ostermann, J., Whetten, R., O'Donnell, K., & Whetten, K. (2014). Child and caregiver concordance of potentially traumatic events experienced by orphaned and abandoned children. Vulnerable Children and Youth Studies, 9(3), 220–233. doi: 10.1080/17450128.2013.855346
- Siddiqui, O. I. (2015). Methods for computing missing item response in psychometric scale construction. American Journal of Biostatistics, 5(1), 1–6. doi:10.3844/amjbsp.2015.1.6.
- StataCorp. (2013). Stata statistical software: Release13. College Station, TX: StataCorp LP.
- Talbot, A., Uwihoreye, C., Kamen, C., Grant, P., McGlynn, L., Mugabe, I., … Zolopa, A. (2013). Treating psychological trauma among Rwandan orphans is associated with a reduction in HIV risk-taking behaviors: A pilot study. AIDS Education and Prevention, 25(6), 468–479. doi: 10.1521/aeap.2013.25.6.468
- Thurman, T. R., Brown, L., Richter, L., Maharaj, P., & Magnani, R. (2006). Sexual risk behavior among South African adolescents: Is orphan status a factor? AIDS and Behavior, 10(6), 627–635. doi: 10.1007/s10461-006-9104-8
- UNAIDS, Government of India. (2012). Technical report, India. HIV estimates 2012. Retrieved Feburary 12, 2015, from http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/data-and-analysis/tools/spectrum/India2012report.pdf
- UNICEF. (2009). Promoting quality education for orphans and vulnerable children. 2009. Retrieved April 15, 2015, http://www.unicef.org/spanish/education/files/Promoting_Quality_Education_for_Orphans_and_Vulnerable_Children_Programmes_from_Eastern_and_Southern_Africa.pdf
- UNICEF. (2012). State of the World's Children 2012: Children in the urban world. New York. Retrieved April 25, 2014, from, http://www.unicef.org/sowc2012/pdfs/SOWC202012-Main20Report_EN_13Mar2012.pdf.
- Whetten, K., Ostermann, J., Pence, B. W., Whetten, R. A., Messer, L. C., Ariely, S., … Positive Outcomes for Orphans Research, T. (2014). Three-year change in the wellbeing of orphaned and separated children in institutional and family-based care settings in five low- and middle-income countries. PLoS One, 9(8), e104872. doi: 10.1371/journal.pone.0104872
- Whetten, K., Ostermann, J., Whetten, R. A., Pence, B. W., O'Donnell, K., Messer, L. C., & Thielman, N. M. (2009). A comparison of the wellbeing of orphans and abandoned children ages 6–12 in institutional and community-based care settings in 5 less wealthy nations. PLoS One, 4(12), e8169. doi: 10.1371/journal.pone.0008169
- Whetten, K., Ostermann, J., Whetten, R., O'Donnell, K., & Thielman, N. (2011). More than the loss of a parent: Potentially traumatic events among orphaned and abandoned children. Journal of Traumatic Stress, 24(2), 174–182. doi: 10.1002/jts.20625
- Wilson, H. W., Woods, B. A., Emerson, E., & Donenberg, G. R. (2012). Patterns of violence exposure and sexual risk in low-income, Urban African American girls. Psychology of Violence, 2(2), 194–207. doi: 10.1037/a0027265
- World Bank. (2012). Prevalence of HIV (% of population ages 15–49). Retrieved February 12, 2015, from http://data.worldbank.org/indicator/SH.DYN.AIDS.ZS
