ABSTRACT
Adolescents with perinatal HIV (PHIV) may be at higher risk of anxiety and depression than HIV negative young people. We investigated prevalence of anxiety and depression symptoms in 283 PHIV and 96 HIV-affected (HIV-negative) young people in England recruited into the Adolescents and Adults Living with Perinatal HIV (AALPHI) cohort. We used Hospital Anxiety and Depression Scale (HADS) scores and linear regression investigated predictors of higher (worse) scores.115 (41%) and 29 (30%) PHIV and HIV-affected young people were male, median age was 16 [interquartile range 15,18] and 16 [14,18] years and 241 (85%) and 71 (74%) were black African, respectively. There were no differences in anxiety and depression scores between PHIV and HIV-affected participants. Predictors of higher anxiety scores were a higher number of carers in childhood, speaking a language other than English at home, lower self-esteem, ever thinking life was not worth living and lower social functioning. Predictors of higher depression scores were male sex, death of one/both parents, school exclusion, lower self-esteem and lower social functioning. In conclusion, HIV status was not associated with anxiety or depression scores, but findings highlight the need to identify and support young people at higher risk of anxiety and depression.
Introduction
Developmental and etiological models of anxiety suggest exposure to uncontrollable life events in early life may lead individuals to perceive events as out of their control. This can lead to a vulnerability for anxiety and possible subsequent depression (Chorpita & Barlow, Citation1998). Young people with perinatal HIV (PHIV) may be at increased risk of anxiety and depression compared to other adolescents (Gadow et al., Citation2010, Citation2012; Malee et al., Citation2011; Mellins et al., Citation2012; Mellins & Malee, Citation2013) because of a complex mix of psycho-social issues and biomedical factors that are associated with chronic illness. Additionally, there may be a greater number of uncontrollable adverse factors which may affect mental health in this group. Having an understanding of the prevalence and risk factors for anxiety and depression among young people with PHIV, and comparison to HIV-affected young people can help ensure that appropriate support can be provided.
In the UK, 50% of a sample of 3258 adults with HIV had anxiety and depression, compared to around a quarter in a study of 8503 adults from the general population (Miners et al., Citation2014). However studies in children and adolescents with HIV in Europe have been limited by small sample sizes and a lack of general population or HIV-affected comparison groups (Bomba et al., Citation2010; Funck-Brentano et al., Citation2016). Several large sub-Saharan African studies have investigated mental health problems in HIV+ young people (known or assumed to be PHIV) (Dow et al., Citation2016; Kim et al., Citation2015; CitationMutumba et al., Citation2017; Woollett, Cluver, Bandeira, & Brahmbhatt, Citation2017). In a South African multi-clinic study of 343 young people 27% had symptoms of anxiety, depression or post-traumatic syndrome (PTSD) (Woollett et al., Citation2017). In Tanzania 12% of 182 adolescents in a single clinic had depressive symptoms, 10% emotional and behavioural symptoms and 14% PTSD (Dow et al., Citation2016). Similarly in a large multi-clinic study in Malawi including 562 young people 19% had depressive symptomology (Kim et al., Citation2015). The majority of studies with an HIV-affected comparator are from the USA. Perhaps surprisingly, most recent USA based studies found no evidence of greater mental health problems in PHIV compared to HIV-affected (perinatally HIV exposed or HIV affected), young people, but higher prevalence in both PHIV and HIV-affected groups compared to the general population (Gadow et al., Citation2010, Citation2012; Malee et al., Citation2011; Mellins et al., Citation2012). These findings highlight the importance of including appropriate control groups in interpreting study findings (Elkington et al., Citation2011; Vreeman, McCoy, & Lee, Citation2017).
We investigated the prevalence of symptoms of anxiety and depression and explored associations with a wide range of psychosocial factors, in older adolescents with and without PHIV in England. This is the first moderately sized study with a comparator group to investigate this issue in England or Europe.
Methods
The Adolescents and Adults Living with Perinatal HIV (AALPHI) cohort is a prospective study evaluating the impact of HIV and antiretroviral (ART) exposure on young people with PHIV and HIV negative young people affected by HIV. Detailed methods have been reported elsewhere (Judd et al., Citation2016). Participants were enrolled between 2013 and 2015 from HIV clinics and community services in England and underwent a two-hour face-to-face interview, including computer-assisted survey interviewing for sensitive questions, after giving informed consent. Ethical approval was obtained from Leicester Research Ethics Committee. PHIV participants were aged 13–21 years. HIV-affected young people were: aged 13–23 years; HIV negative on a point-of-care test at interview; living in the same household as a PHIV participant in AALPHI, or had a sibling, friend or partner who was a PHIV participant in AALPHI, or had an HIV positive parent; and awareness of HIV in the family (where appropriate). HIV-affected participants born to mothers with HIV may have been exposed to HIV and/or ART in utero but it was not possible to confirm in which participants this was the case. All participants had lived in the UK for ≥6 months and could speak and understand English.
Anxiety and depression scores were measured using the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, Citation1983). Scores range from 0 to 21, with higher scores indicating more severe anxiety or depression. Scores were categorised using standard definitions as normal (<7), mild (8–10), moderate (11–15) or severe (>15) (Zigmond & Snaith, Citation1983). Self-esteem was measured using the Rosenberg self-esteem scale (scores range from 0 to 30: higher scores indicate better self-esteem) (Rosenberg, Citation1965). Normative data sources for HADS and self-esteem are detailed in Supplementary Table 1. A residential deprivation score measured deprivation (Income Deprivation Affecting Children Index (IDACI), ranging from 0 to 1; higher score indicates more severe deprivation) (Department for Communities and Local Government, Citation2011). Social support was measured using the Social Functioning score from the Pediatric Quality of Life Inventory (PedsQL) (Teenage report for 13–18 and Young Adult report for 18–25 years); scores range from 0 to 100 and a higher score indicates better social functioning (Varni, Citation2012).
A cognitive composite of executive functions (neuropsychological scores (NPZ score)) was calculated using manufacturer normative data for six domains (executive function; speed of information processing; attention/working memory, learning and memory and fine motor skills) and the mean across these domains was calculated (NPZ-6) (further details of the individual cognitive test are available in Judd et al., Citation2016).
For the PHIV group only the effect of the following HIV-related health factors on anxiety and depression scores were considered: age diagnosed with HIV, age starting ART and current ART status, current efavirenz (EFV) use (due to potential association with depression), nadir and most recent CD4 cell count, most recent viral load ≤50 copies/mL vs. >50 copies/mL, median cumulative years with viral load <400 copies/mL, HIV disclosure factors (age told HIV status and ever told anyone HIV status) and current feeling about HIV status.
Statistical analysis
Data were analysed using STATA version 13 (Stata Corp, College Station, Texas, USA).
Descriptive statistics (χ2, Mann–Whitney Wilcoxon Test) summarised sociodemographic and HADS data by HIV status.
Linear regression and Wald p-values assessed potential associations between variables and anxiety/ depression scores. Variables which attained p < 0.15 in univariable analyses were considered for inclusion in multivariable analyses using backwards selection. All multivariable models included HIV status as well as a priori factors associated with anxiety and depression scores (sex, age, ethnicity, born abroad). A two-tailed p value of <0.05 was considered statistically significant. Other variables considered in the analysis were selected on the basis of the literature and are listed in .
Table 1. Characteristics of PHIV+ and HIV- participants.
A model for young people with PHIV only additionally considered the effect of HIV-related health factors on anxiety and depression scores ().
Three sensitivity analyses were conducted. Firstly, for young people with PHIV only, we included all variables which were significant in the overall models as well as the HIV-related variables, to check that loss of power from the reduced sample size was not affecting model outcomes. Secondly, due to the potential for mental health variables to be outcomes of anxiety and depression rather than antecedents, sensitivity analyses excluded these variables from the models. Thirdly, we restricted the models to ≥16 years only to investigate any potential effect of using HADS, WAIS-IV and Color Trails 1 and 2 scales for those aged <16 years of age.
Results
A total of 283 PHIV and 96 HIV-affected participants completed HADS. Of the 96 HIV-affected young people, 46 (48%) had a mother with HIV, 38 (40%) were siblings of young people with PHIV in the study, 8 (8%) had PHIV siblings who were not in the study, and 4 (4%) had a close friend who was a young person with PHIV. Sociodemographic characteristics of the two groups were generally similar (). Two-thirds were female, median age overall was 16 years, most were black African and born outside of the UK. For around a quarter (24%) of HIV-affected young people, one or both parents had died, compared to 37% for the PHIV group. Mean scores for self-esteem were similar across both groups, 12% of PHIV and 19% of HIV-affected participants have ever self-harmed, and 39% in both groups reported ever feeling life was not worth living. Similar proportions reported having ever smoked and used alcohol, while the proportion ever using recreational drugs was 15% in PHIV and 29% in HIV-affected participants (p = 0.003).
For the PHIV group, median age at first presentation to care in the UK was 4 years [interquartile range (IQR) 0,8] (). Median nadir CD4 was 226 c/mm3 [128,367] and CD4 at interview 599 c/mm3 [407,782]. Around three-quarters of those on ART (74%) had never had a CDC C event and 87% were on ART at interview. Around three-quarters (74%, 177/238) had a viral load ≤50 c/mL at interview, median age at start of ART was 7 years [3,11] and median cumulative number of years with a suppressed viral load (<400 c/mL) was 6 years [3,9].
Table 2. HIV-related health factors for PHIV+ participants.
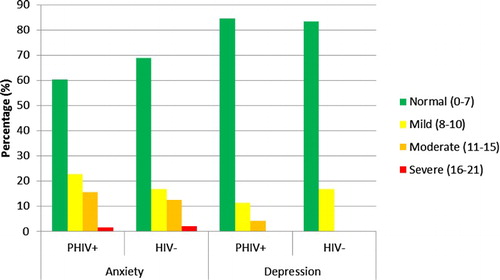
presents anxiety and depression scores by HIV status. Around two-thirds (60% PHIV vs 69% HIV-affected, p = 0.145) scored in the “normal” range for anxiety, and similarly around four-fifths (84% vs 83% respectively, p = 0.795) for depression. Only four PHIV and two HIV-affected participants had a “severe” score for anxiety and none for depression.
Raw and z-score adjusted anxiety and depression mean scores did not differ between PHIV and HIV-affected participants (all p values ≥0.1; ) and were very close to the UK population means. For self-esteem, similarly, there were no differences in raw and z-scores between PHIV and HIV-affected participants (both p values > 0.8), although mean z-scores for both groups were nearly two standard deviations lower than the population means.
Table 3. Raw and adjusted anxiety, depression and self esteem scores, for PHIV+ and HIV- participants.
In a multivariable model for anxiety, there was no evidence for young people with PHIV having greater anxiety scores than HIV-affected young people (multivariable coefficient 0.14, 95%CI −0.03, 0.31; ). Speaking a language other than English at home (0.48, 95%CI 0.01, 0.95), having a higher number of main carers (0.06, 95%CI 0.02,0.10), having ever thought life was not worth living (0.26, 95%CI 0.09,0.43) lower self-esteem scores (−1.27, 95%CI −1.60,−0.95, 001 per 5 unit increase) and lower social functioning scores (−0.22, 95%CI −0.35,−0.08 per 25 unit increase) were associated with an increased number of anxiety scores.
Table 4. Univariable and multivariable predictors of increased anxiety and depression scores.
For depression, there were no differences in scores between PHIV and HIV-affected participants (multivariable coefficient 0.08, 95%CI −0.10, 0.25). Being male (female −0.29, 95%CI −0.45,−0.13), death of one or both parents (0.23, 95%CI 0.07, 0.39), ever being excluded from school (0.27, 95%CI 0.07, 0.47), lower self-esteem scores (−1.52, 95%CI −1.83,−1.20 per 5 unit increase) and lower social functioning scores (−0.14, 95%CI −0.27,−0.01 per 25 unit increase) were associated with a higher number of depression scores.
In a model including young people with PHIV only, factors associated with increased anxiety scores were similar to the overall model, except that speaking a language other than English was no longer significant either univariably or multivariably (). Ever having been excluded from school and social functioning were no longer associated with higher depression scores, whilst feeling less supported in relation to one’s HIV status was associated with higher depression scores (multivariable coefficient −0.04, 95%CI −0.06,−0.01), whilst other coefficients changed minimally.
Table 5. Univariable and multivariable predictors of increased anxiety and depression scores for PHIV+ only.
In the first and third sensitivity analyses, findings were very similar (data not shown). In the second sensitivity analysis, final multivariable model variables were the same except that for anxiety the effect of sex became significant (multivariable coefficient 0.21, 95%CI 0.04, 0.39), whilst for depression, it was no longer significant (−0.01, 95%CI −0.19, 0.17).
Discussion
In our study of 283 PHIV and 96 HIV-affected young people, with median age 16 years, overall anxiety and depression scores were similar between the two groups, both before and after adjustment for other variables. In total 40% of PHIV and 31% of HIV-affected participants scored mild to severe for anxiety and 16% and 17% mild to moderate for depression. These results are similar to other recent studies finding no evidence of a difference in prevalence of mental health problems by HIV status, (Elkington et al., Citation2011; Gadow et al., Citation2012; Mellins et al., Citation2012; Mutumba et al., Citation2016) and suggest that contextual factors rather than HIV itself may have an important role (Mellins & Malee, Citation2013). Another explanation for the lack of difference by HIV status is that anxiety and depression in young people with PHIV may be lessened through regular contact with health services and mental health support (Gadow et al., Citation2012).
Prevalence of mental health problems in young people with PHIV varies across different populations in the literature (Chernoff, Nachman, & Williams, Citation2009; Gadow et al., Citation2012; Malee et al., Citation2011; Mellins et al., Citation2009; Mutumba et al., Citation2016). This may be due to different mental health problems being assessed, with differing definitions, and different healthcare settings and contextual factors. In our study prevalence of mental health problems was similar to normative data, but two large USA cohorts found higher prevalence in young people with PHIV than young people in the general population (Gadow et al., Citation2012; Mutumba et al., Citation2016). Both of these studies used assessment tools which investigated a wider range of psychiatric symptoms over more than one time period, which may contribute to higher prevalence compared to our study. In contrast, a third large cross-sectional study from the USA found higher prevalence of mental health problems in the HIV-affected group compared to PHIV group at assessment (38% vs 25%, p < 0.01), (Malee et al., Citation2011) using behavioural and emotional symptom checklists, rather than psychiatric assessments in the other studies.
Socio-demographic differences between the studies also complicate the picture. In the USA many families studied had a history of psychiatric disorders and substance-abuse, (Elkington et al., Citation2011; Malee et al., Citation2011) whilst in the UK, most young people with PHIV were born in sub-Saharan Africa, have migrated to the UK (Bamford & Lyall, Citation2015) and there is no published evidence of drug misuse in this group. These distinct experiences may impact differently on the risk of anxiety and depression.
Although young people with PHIV in our study appear not to be at increased risk of anxiety or depression symptoms compared to normative data, 40% scored at least mild symptoms of anxiety and similarly, 15% scored at least mild symptoms of depression. While it is reassuring that many young people with PHIV appear to be coping well, mental health problems in young people with PHIV may have an even more profound effect than in other youth due to the wider health implications associated with HIV. Mental health problems in young people with PHIV have been associated with reduced adherence (Mutumba et al., Citation2016; Hudelson & Cluver, Citation2015) and retention in care (Lowenthal et al., Citation2014) and increased sexual risk behaviours, (Kapetanovic et al., Citation2011; Mellins et al., Citation2011), highlighting the need to identify young people at increased risk and providing the right support at the right time. Also of concern, although levels of self-esteem were similar in the PHIV and HIV-affected groups, they were nearly two standard deviations lower than normative data, and self-esteem was associated with both anxiety and depression in multivariable models. Self-esteem may better reflect the long-term effects of cumulative adverse factors to which these young people have been exposed, than anxiety and depression.
A strength of our study was its ability to explore associations between anxiety and depression scores and a wide range of psychosocial factors in addition to HIV status. In our analysis being male, having an increased number of main carers during childhood, speaking a language other than English at home, death of one or both parents, ever having felt that life was not worth living, lower self-esteem, worse social functioning and ever having been excluded from school, were all related to either higher anxiety and/ or depression scores. Some other studies have found higher depression and anxiety in females compared to males, (Breeman, Cotton, Fielding, & Jones, Citation2015; Mellins & Malee, Citation2013; Mellins et al., Citation2012; Mutumba et al., Citation2016; Paus, Keshavan, & Giedd, Citation2008) whilst others have not (Lewis, Abramowitz, Koenig, Chandwani, & Orban, Citation2015; Malee et al., Citation2011). Findings from studies of fostering suggest that multiple placements are associated with later mental health problems, in keeping with a higher number of main carers being associated with increased anxiety in our study (Newton, Litrownik, & Landsverk, Citation2000; Rubin et al., Citation2004). Speaking a language other than English at home may reflect uncertain residency or negative effects of immigration. The number of young people who had experienced a close bereavement was high in this study and may be further complicated in the context of having HIV in the family (Battles & Wiener, Citation2002). The combination of higher anxiety scores and ever feeling life is not worth living is certainly a concern because of the link between unrecognised or untreated mental health problems and co-morbidities and suicide (Malee et al., Citation2011; Thapar, Collishaw, Pine, & Thapar, Citation2012). Studies have found that young people with PHIV are concerned about disclosing their status to their peers which can lead to feelings of isolation, (Battles & Wiener, Citation2002; Mutumba et al., Citation2015) and better social support has been found to improve psychological outcomes. One large study found that young people who were excluded from school had often experienced social disadvantage including bereavements, and felt depressed and lonely following educational exclusion (Berridge, Brodie, Pitts, Porteous, & Tarling, Citation2001).
Our study has a number of limitations. Firstly we only investigated anxiety and depression rather than a wider range of psychiatric symptoms or mental health problems, as we were constrained by interview length, which needed to be acceptable to young people. Our analysis was cross-sectional, and there is a possibility that symptoms of anxiety and depression contributed to other mental health variables (e.g., self-esteem, self-harm), rather than were outcomes, although our sensitivity analysis had similar results. Selection of an appropriate tool to measure mental health was challenging given the time constraints and that most tools are designed either for children or adults. HADS is used widely in the UK across chronic health conditions and has some normative data in young adults. However HADS is not a diagnostic tool as it dichotomises anxiety and depression as two unrelated problems, and so is more an indicator of psychological distress (Cosco, Doyle, Ward, & McGee, Citation2012) which would require confirmatory psychological assessment for a formal diagnosis. Finally age-appropriate normative data were not always available resulting in the downward extrapolation of measures for use with younger ages; however, the AALPHI cohort had its own control group of HIV-affected young people, which formed the primary comparison group.
In conclusion, we found no difference in the prevalence of increased anxiety and depression scores between PHIV and HIV-affected young people, and levels were similar to UK normative data. However, for both PHIV and HIV-affected young people levels of self-esteem were significantly lower than population norms. Key factors found to be associated with a greater anxiety and depression scores included lower self-esteem, lower social functioning, being male and having ever thought life was not worth living. Our findings underscore the need for young people with PHIV to be regularly screened for mental health problems. Where routine screening for anxiety and depression is not possible, these key factors may be useful for clinical staff to help identify a potentially more vulnerable sub-population to monitor and prioritise for assessment.
Supplementary_Table_1_v1.0.doc
Download MS Word (34.5 KB)Acknowledgements
Author contributions: MLP, AA-P, DM, CF, ME, AW, DMG and AJ designed the mental health aspects of the study and conceived this analysis. MLP, KS and KR conducted study interviews. FP conducted the statistical analysis with support from AJ and DF. MLP wrote the first draft of the manuscript, with assistance from AJ. All authors contributed to the interpretation of the data, commented on the draft, and approved the final version.
We thank all the young people, parents and staff from all the clinics and voluntary services in AALPHI.
Project team: S. Brice, A. Judd, M. Le Prevost, A. Mudd, F. Parrott, K. Rowson, K. Sturgeon.
Investigators: M. Conway, K. Doerholt, D. Dunn, C. Foster, D.M. Gibb, A. Judd (PI), S. Kinloch, N. Klein, H. Lyall, D. Melvin, K. Prime, C. Sabin, M. Sharland, C. Thorne, P. Tookey.
MRCC CTU Data Services: C. Diaz Montana, K. Fairbrother, M. Rauchenberger, N. Tappenden, S. Townsend.
Steering Committee chairs: D. Gibb, D. Mercey (2012–2015), C. Foster (2016-).
Patient and public involvement: Children’s HIV Association Youth Committee.
NHS clinics (named alphabetically): LONDON: Chelsea and Westminster NHS Foundation Trust, F. Boag, P. Seery; Great Ormond Street Hospital NHS Foundation Trust, M. Clapson, V. Noveli; Guys and St Thomas’ NHS Foundation Trust, A. Callaghan, E. Menson; Imperial College Healthcare NHS Trust, C. Foster, A. Walley; King’s College Hospital NHS Foundation Trust, E. Cheserem, E. Hamlyn; Mortimer Market Centre, Central and North West London NHS Foundation Trust, R. Gilson, T. Peake; Newham University Hospital, S. Liebeschuetz; North Middlesex University Hospital NHS Trust, J. Daniels; Royal Free London NHS Foundation Trust, T. Fernandez, S. Kinloch de Loes; St George’s University Hospitals NHS Foundation Trust, S. Storey, K. Prime. REST OF ENGLAND: Alder Hey Children’s NHS Foundation Trust, S. Paulus, A. Riordan; Birmingham Heartlands, Heart of England NHS Foundation Trust J. Daglish, C. Robertson; Bristol Royal Infirmary, University Hospitals Bristol NHS Foundation Trust, J. Bernatonlene, L. Hutchinson, University Hospitals Bristol NHS Foundation Trust, M. Gompel, L. Jennings; Leeds Teaching Hospitals NHS Trust, M. Dowie, S. O’Riordan; University Hospitals of Leicester NHS Trust, W. Ausalut, S. Bandi; North Manchester General Hospital, Pennine Acute Hospitals NHS Trust, P. McMaster, C. Murphy; Royal Liverpool and Broadgreen University Hospitals NHS Trust, M. Chaponda, S Paulus. Voluntary services (named alphabetically): Blue Sky Trust, C. Dufton, B. Oliver; Body and Soul, J. Marsh; Faith in People, I. Clowes; Positively UK, M. Kiwanuka; Positive Parenting & Children, B. Chipalo.
Disclosure statement
Marthe Le Prevost, Diane Melvin, Francesca Parrott, Caroline Foster, Deborah Ford, Michael Evangeli, Kate Sturgeon Diana M Gibb and Ali Judd have no potential conflicts of interest. Katie Rowson works part-time for the Childrens HIV Association (CHIVA). Alan Winston has received investigator initiated grants, speaker fees or honoraria from GSK, ViiV, BMS, Merck and Janssen. Alejandro Arenas-Pinto has received research grants from ViiV Healthcare, Janssen Cilag and Pfizer, not related to the submitted work.
Additional information
Funding
References
- Bamford, A., & Lyall, H. (2015). Paediatric HIV grows up: Recent advances in perinatally acquired HIV. Archives of Disease in Childhood, 100(2), 183–188. doi: 10.1136/archdischild-2014-306079
- Battles, H. B., & Wiener, L. S. (2002). From adolescence through young adulthood: Psychosocial adjustment associated with long-term survival of HIV. Journal of Adolescent Health, 30(3), 161–168. http://doi.org/S1054139X0100341X doi: 10.1016/S1054-139X(01)00341-X
- Berridge, D., Brodie, I., Pitts, J., Porteous, D., & Tarling, R. (2001). The independent effects of permanent exclusion from school on the offending careers of young people. RDS Occasional Paper, 71, i–58.
- Bomba, M., Nacinovich, R., Oggiano, S., Cassani, M., Baushi, L., Bertulli, C., … Badolato, R. (2010). Poor health-related quality of life and abnormal psychosocial adjustment in Italian children with perinatal HIV infection receiving highly active antiretroviral treatment. AIDS Care, 22(7), 858–865. doi: 10.1080/09540120903483018
- Breeman, S., Cotton, S., Fielding, S., & Jones, G. T. (2015). Normative data for the Hospital Anxiety and Depression Scale. Quality of Life Research, 24(2), 391–398. doi: 10.1007/s11136-014-0763-z
- Chernoff, M., Nachman, S., & Williams, P. (2009). Mental health treatment patterns in perinatally HIV-infected youth and controls. Pediatrics. Retrieved from http://pediatrics.aappublications.org/content/124/2/627.short
- Chorpita, B. F., & Barlow, D. H. (1998). The development of anxiety: The role of control in the early environment. Psychological Bulletin, 124(1), 3–21. doi: 10.1037/0033-2909.124.1.3
- Cosco, T. D., Doyle, F., Ward, M., & McGee, H. (2012). Latent structure of the Hospital Anxiety and Depression Scale: A 10-year systematic review. Journal of Psychosomatic Research, 72(3), 180–184. doi: 10.1016/j.jpsychores.2011.06.008
- Crawford, J. R., Henry, J. D., Crombie, C., & Taylor, E. P. (2001). Normative data for the HADS from a large non-clinical sample. British Journal of Clinical Psychology, 40, 429–434. doi: 10.1348/014466501163904
- Department for Communities and Local Government. (2011). The English indices of deprivation 2010: The income deprivation affecting children index and the income deprivation affecting older people index. London: Author.
- Dow, D. E., Turner, E. L., Shayo, A. M., Mmbaga, B., Cunningham, C. K., & O’Donnell, K. (2016). Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care, 28(7), 825–833. doi: 10.1080/09540121.2016.1139043
- Elkington, K. S., Robbins, R. N., Bauermeister, J. A., Abrams, E. J., McKay, M., & Mellins, C. A. (2011). Mental health in youth infected with and affected by HIV: The role of caregiver HIV. Journal of Pediatric Psychology, 36(3), 360–373. doi: 10.1093/jpepsy/jsq094
- Funck-Brentano, I., Assoumou, L., Veber, F., Moshous, D., Frange, P., & Blanche, S. (2016). Resilience and life expectations of perinatally HIV-1 infected adolescents in France. The Open AIDS Journal, 10(1), 209–224. doi: 10.2174/1874613601610010209
- Gabhainn, S., & Mullan, E. (2003). Self-esteem norms for Irish young people. Psychological Reports, 92, 829–830. doi: 10.2466/pr0.2003.92.3.829
- Gadow, K. D., Angelidou, K., Chernoff, M., Williams, P. L., Heston, J., Hodge, J., & Nachman, S. (2012). Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. Journal of Developmental & Behavioral Pediatrics, 33(6), 456–468. doi: 10.1097/DBP.0b013e31825b8482
- Gadow, K. D., Chernoff, M., Williams, P. L., Brouwers, P., Morse, E., Heston, J., … Nachman, S. (2010). Co-occuring psychiatric symptoms in children perinatally infected with HIV and peer comparison sample. Journal of Developmental & Behavioral Pediatrics, 31(2), 116–128. doi: 10.1097/DBP.0b013e3181cdaa20
- Hudelson, C., & Cluver, L. (2015). Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: A systematic review. AIDS Care, 27(7), 805–816. doi: 10.1080/09540121.2015.1011073
- Judd, A., Le Prevost, M., Melvin, D., Arenas-Pinto, A., Parrott, F., Winston, A., … Gibb, D. M. (2016). Cognitive function in young persons with and without perinatal HIV in the AALPHI cohort in England: Role of non–HIV-related fact. Clinical Infectious Diseases, 63, 1380–1387. doi: 10.1093/cid/ciw568
- Kapetanovic, S., Wiegand, R. E., Dominguez, K., Blumberg, D., Bohannon, B., Wheeling, J., & Rutstein, R., the LEGACY Consortium. (2011). Associations of medically documented psychiatric diagnoses and risky health behaviors in highly active antiretroviral therapy-experienced perinatally HIV-infected youth. AIDS Patient Care and STDs, 25(8), 493–501. doi: 10.1089/apc.2011.0107
- Kim, M. H., Mazenga, A. C., Yu, X., Devandra, A., Nguyen, C., Ahmed, S., … Sharp, C. (2015). Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry, 15, 264. doi: 10.1186/s12888-015-0649-9
- Lewis, J. V., Abramowitz, S., Koenig, L. J., Chandwani, S., & Orban, L. (2015). Negative life events and depression in adolescents with HIV: A stress and coping analysis. AIDS Care, 27(10), 1265–1274. doi: 10.1080/09540121.2015.1050984
- Lowenthal, E. D., Bakeera-kitaka, S., Marukutira, T., Chapman, J., Goldrath, K., & Ferrand, R. A. (2014). Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: A review of emerging challenges. The Lancet Infectious Diseases, 14(7), 627–639. doi: 10.1016/S1473-3099(13)70363-3
- Malee, K. M., Tassiopoulos, K., Huo, Y., Siberry, G., Williams, P. L., Hazra, R., … Mellins, C. A. (2011). Mental health functioning among children and adolescents with perinatal HIV infection and perinatal HIV exposure. AIDS Care, 23(12), 1533–1544. doi: 10.1080/09540121.2011.575120
- Mellins, C. A., Brackis-Cott, E., Leu, C., Elkington, K. S., Dolezal, C., Wiznia, A., … Abrams, E. J. (2009). Rates and types of psychiatric disorders in perinatally HIV-infected youth and seroconverters. Journal of Child Psychology and Psychiatry, 50(9), 1131–1138. doi: 10.1111/j.1469-7610.2009.02069.x
- Mellins, C. A., Elkington, K. S., Leu, C. S., Santamaria, E. K., Dolezal, C., Wiznia, A., … Abrams, E. J. (2012). Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care, 24(8), 953–962. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=22519762 doi: 10.1080/09540121.2012.668174
- Mellins, C. A., & Malee, K. M. (2013). Understanding the mental health of youth living with perinatal HIV infection: Lessons learned and current challenges. Journal of the International AIDS Society, 16(1), 18593. doi: 10.7448/ias.16.1.18593
- Mellins, C. A., Tassiopoulos, K., Malee, K., Moscicki, A.-B., Patton, D., Smith, R., … Seage, G. R. (2011). Behavioral health risks in perinatally HIV-exposed youth: Co-occurrence of sexual and drug use behavior, mental health problems, and nonadherence to antiretroviral treatment. AIDS Patient Care and STDs, 25(7), 413–422. doi: 10.1089/apc.2011.0025
- Miners, A., Phillips, A., Kreif, N., Rodger, A., Speakman, A., Fisher, M., … Burman, B. (2014). Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: A cross-sectional comparison with the general population. The Lancet HIV, 1(1), e32–e40. doi: 10.1016/S2352-3018(14)70018-9
- Mutumba, M, Bauermeister, JA, Elkington, KS, Bucek, A, Dolezal, C, Leu, CS, & Mellins, CA. (2016). A prospective analysis of changes in mental health symptoms among perinatally HIV-infected and HIV-exposed but uninfected urban youths. The Journal of Adolescent Health?: Official Publication of the Society for Adolescent Medicine, 58(4), 460–466. doi: 10.1016/j.jadohealth.2015.12.014
- Mutumba, M, Bauermeister, JA, Harper, GW, Musiime, V, Lepkowski, J, Resnicow, K, & Snow, RC. (2017). Psychological distress among Ugandan adolescents living with HIV: Examining stressors and the buffering role of general and religious coping strategies. Global public health, 12(12), 1479–1491. doi: 10.1080/17441692.2016.1170871
- Mutumba, M., Bauermeister, J. A., Musiime, V., Byaruhanga, J., Francis, K., Snow, R. C., & Tsai, a. C. (2015). Psychosocial challenges and strategies for coping with HIV among adolescents in Uganda: A qualitative study. AIDS Patient Care and STDs, 29(2), 86–94. doi: 10.1089/apc.2014.0222
- Newton, R. R., Litrownik, A. J., & Landsverk, J. A. (2000). Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse and Neglect, 24(10), 1363–1374. doi: 10.1016/S0145-2134(00)00189-7
- Paus, T., Keshavan, M., & Giedd, J. N. (2008). Why do many psychiatric disorders emerge during adolescence? Nature Reviews Neuroscience, 9(12), 947–957. doi: 10.1038/nrn2513
- Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press.
- Rubin, D. M., Alessandrini, E. A., Feudtner, C., Mandell, D. S., Localio, A. R., Hadley, T., & Objective, A. (2004). Placement stability and mental health costs for children in foster care. Pediatrics, 113(5), 1336–1341. doi: 10.1542/peds.113.5.1336
- Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. doi: 10.1016/S0140-6736(11)60871-4
- Varni, J. W. (2012). Pediatric quality of life inventory TM PedsQL. Lyon: MAPI Research Trust.
- Vreeman, R. C., McCoy, B. M., & Lee, S. (2017). Mental health challenges among adolescents living with HIV. Journal of the International AIDS Society, 20(0), 100–109. doi: 10.7448/IAS.20.4.21497
- Woollett, N., Cluver, L., Bandeira, M., & Brahmbhatt, H. (2017). Identifying risks for mental health problems in HIV positive adolescents accessing HIV treatment in Johannesburg. Journal of Child and Adolescent Mental Health, 29(1), 11–26. doi: 10.2989/17280583.2017.1283320
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6880820 doi: 10.1111/j.1600-0447.1983.tb09716.x