ABSTRACT
Delayed HIV diagnosis and enrollment in HIV care can lead to negative health outcomes for individuals and pose major barriers to achieving the UNAIDS 90-90-90 treatment targets. Household economic strengthening (HES) initiatives are increasingly used to alleviate the direct and indirect costs of HIV testing and linkage to care for those who are diagnosed. The evidence linking HES with a range of HIV outcomes is growing, and this evidence review aimed to comprehensively synthesize the research linking 15 types of HES interventions with a range of HIV prevention and treatment outcomes. The review was conducted between November 2015 and October 2016 and consisted of an academic database search, citation tracking of relevant articles, examination of secondary references, expert consultation, and a gray literature search. Given the volume of evidence, the results are presented and discussed in three papers. This is the second paper in the series and focuses on the 20 studies on HIV testing, diagnosis, and enrollment in care. The results indicate that financial incentives are consistently and independently linked with higher testing uptake and yield among adults. Limited evidence indicates they may also be beneficial for enrollment in care. Evidence for other HES interventions is too sparse to identify clear trends.
Introduction
Poverty and economic insecurity have been linked to HIV risk behaviors and outcomes at all stages of the HIV care and treatment cascade (Centers for Disease Control and Prevention, Citation2014). In addition to social and psychological factors, economic factors, such as travel costs and lost income or opportunity costs when accessing services, can inhibit both access to HIV testing services (HTS) and care initiation (Govindasamy, Ford, & Kranzer, Citation2012; Musheke et al., Citation2013; Thornton, Citation2008). Present-biased perspective, whereby individuals disproportionately prioritize current or short-term benefits (such as completing routine responsibilities or enjoying free time) over potential future benefits (such as long-term health), can also deter testing and linkage to care (Solomon et al., Citation2014).
In 2014, UNAIDS established ambitious targets to increase the proportion of HIV-positive individuals who are diagnosed, receiving care, and virally suppressed. Since then notable progress has been made, and in 2016 an estimated 70% of people living with HIV (PLHIV) aged 15–49 globally knew their status, though only 53% were accessing treatment (UNAIDS Joint United Nations Programme on HIV/AIDS, Citation2017). Access to testing for at-risk populations, followed by expedient linkage into care for those who are positive, are essential to achieving these targets. Delayed diagnosis and care initiation, in turn, have negative implications for disease progression and onward transmission of the virus.
Household economic strengthening (HES) initiatives are increasingly implemented in coordination with biomedical and behavioral approaches to address the economic drivers of the epidemic. The effects of HES interventions on HIV outcomes are often mediated by structural and context-specific factors, however these interventions have the potential to help overcome barriers related to the direct and indirect costs of testing and linkage to care. In addition, behavioral economics is increasingly being applied to overcome actual costs, present-biased perspective, and even social barriers by using tangible financial rewards to motivate and reinforce specific behaviors, including HIV testing and linkage to care (Bassett, Wilson, Taaffe, & Freedberg, Citation2015; Galárraga, Genberg, Martin, Laws, & Wilson, Citation2013; Pettifor, MacPhail, Nguyen, & Rosenberg, Citation2012; Thornton, Citation2008).
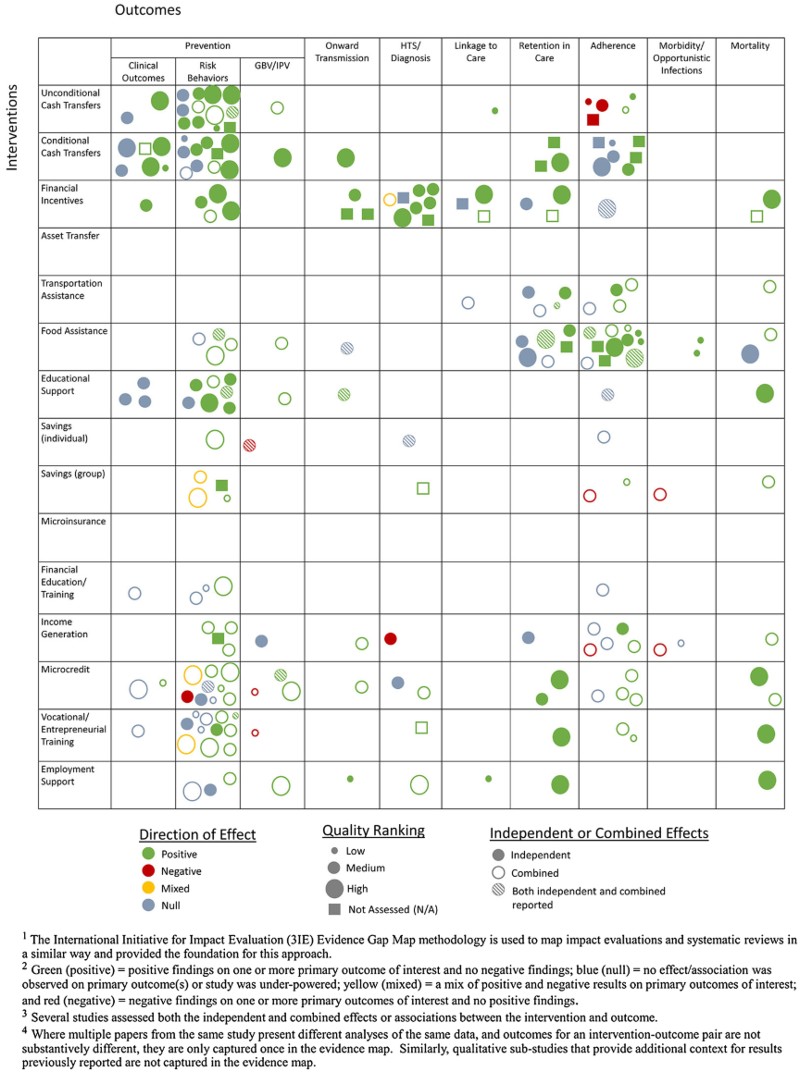
This is the second paper in a three-part series that comprehensively documents the published and gray literature linking a broad set of HES interventions to a range of HIV outcomes. This paper focuses on testing and linkage to care outcomes; the first and third papers in the series (Swann Citation2018a, Citation2018b) cover prevention outcomes and clinical retention and antiretroviral therapy (ART) adherence outcomes, respectively (). Testing and linkage to care (including enrollment in care or ART initiation) are distinct areas of the HIV treatment cascade. In 2015, however, the World Health Organization revised its HIV treatment guidance, recommending that ART be provided to all people who test positive regardless of CD4 count or clinical disease stage (known as the “test and treat” approach), highlighting the important connection between these areas of the cascade. These outcomes are grouped together in this paper based on their proximity within the cascade, but also because of the relative scarcity of evidence on these outcomes.
Table 1. HIV outcomes assessed.
HES interventions can be classified into three categories: provision, protection, and promotion. Provision interventions support basic needs; protection interventions help smooth consumption and protect assets against shocks; and promotion interventions help households to grow their income and assets (Woller, Citation2011). Results are presented by individual HES intervention, and are discussed in the context of these wider categories. Descriptions for each HES intervention are provided in .
Methods
The methodology of this review was described in detail in the first paper in this series, including a description of the search strategy, quality assessment approach and search terms (Swann Citation2018a). Briefly, the review was conducted between November 2015 and October 2016. The initial search was completed using nine academic databases. Four consistent search strings were entered into each database using a list of HES interventions, plus terms associated with different HIV outcomes or population groups. Included evidence had to meet the following criteria: (1) evaluated one or more HES intervention of interest, (2) reported on at least one HIV outcome of interest, (3) available in English, and (4) relevant to low-income contexts or vulnerable populations. There were no geographic exclusion criteria, but studies conducted in high-income countries were only included in the review if the intervention and findings were relevant to low-income or otherwise vulnerable groups. Articles from the initial search were screened for inclusion based on a review of the title and abstract by two reviewers. Relevant records then underwent a full text review by the study author.
Using a citation tracking approach, the reference sections of each of the selected papers were screened for additional pertinent research. In addition, all identified secondary sources were reviewed and all source studies meeting the criteria were included. Recommendations for additional citations were solicited from experts in this field through a half-day consultative meeting. Finally, a gray literature search was conducted. All evidence was assessed for quality using the Department for International Development’s Assessing the Strength of Evidence methodology (DFID, Citation2014).
Using the quality assessment results, each citation was given a rating of high, medium-high, medium or low. This assessment was only applied to written articles as there was insufficient information to complete the assessment for conference abstracts and presentations. For quantitative studies, findings were classified as positive or negative if the results were statistically significant according to a p ≤ 0.05 threshold. Where tests of statistical significance were not conducted/presented, results were classified as null even when directional trends were strong. For qualitative studies, results were classified as positive or negative based on the qualitative data and interpretations presented. Many studies assessed integrated programs, grouping multiple HES, health and/or social services. Whether a study assessed the independent relationship between a specific HES component and the outcome(s) of interest was an important element of analysis.
Results
Results for the full review are reported in the first paper in this series (Swann Citation2018a) including overall study characteristics, PRISMA diagram (see appendix 1) and full evidence map (see appendix 2) (Snilstveit, Vojtkova, Bhavsar, Stevenson, & Gaarder, Citation2016).
Evidence for HTS and linkage to care
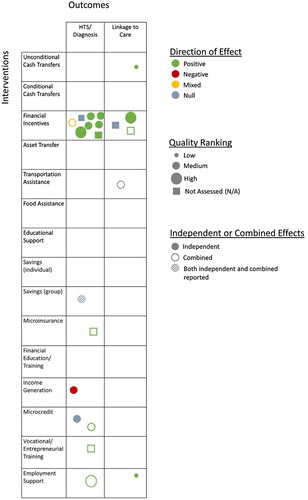
From all search methods, 3,309 unique records were identified and screened; 436 records underwent a full-text review. A total of 108 citations were included in the full evidence review, 20 of which are included in this paper (14 that evaluated HTS and six that assessed linkage to care). HTS outcomes include self-reported and clinical record data on HIV testing uptake, and clinical record data on obtaining HIV test results and testing yield (proportion of all tests that were positive). Linkage to care includes self-reported and clinical record data on uptake of clinical services by PLHIV, enrollment in HIV-related care, and initiation of ART. Evidence for most HES interventions is minimal or lacking for both HTS and linkage to care, highlighting a narrower theoretical link between individual and household economics and these portions of the care and treatment cascade. Forty percent of the studies in this paper rely on self-reported outcomes which can be susceptible to bias; this should be considered when interpreting these findings. The evidence map excerpt for HTS and linkage to care outcomes is provided in .Footnote1
Evidence for both outcomes is presented by HES intervention. Of the 14 HES intervention areas, no evidence was found for six of them (conditional cash transfers, food assistance, asset transfers, financial education and training, education support, and microinsurance) in relation to HTS and linkage to care, therefore they are not discussed below. Where studies included multiple HES interventions, they are discussed in each relevant section. Given the diversity in study characteristics – geography, target group, intervention implementation, study design, sample size, outcome indicators, analysis methods, and overall study contexts – in most cases the studies in this review have only limited comparability. The summaries of literature instead highlight patterns within these characteristics but do not seek to explicitly compare the studies.
Table 2. HES interventions assessed.
Provision interventions
Financial incentives
Eleven studies examined associations between financial incentives and HTS or linkage to care (). The quality of evidence for this intervention is fairly strong, but comparability among studies is limited due to a wide range of incentive amounts (USD 1–125), each of which incentivized unique behaviors in different contexts.
Eight studies evaluated financial incentives and HTS. Seven of these measured the independent association between financial incentives and HTS, providing the most robust evidence for this part of the cascade. In Malawi, incentives were effective at increasing receipt of HIV test results, and the probability of receiving HIV test results increased as incentive values rose (Thornton, Citation2008). In a U.S.-based study, cash incentives were associated with increased testing uptake (Haukoos, Witt, Coil, & Lewis, Citation2005), and in Zimbabwe incentives in the form of grocery items increased couples testing (Sibanda et al., Citation2016). In Pakistan, financial incentives were used to encourage HIV-positive men to bring their wives for HTS and at least 56% of their spouses tested (Khan, Qazi, Nazim, & Khan, Citation2012). Incentives provided to women’s economic empowerment groups in India to identify and accompany pregnant women to clinics were associated with more pregnant women receiving HTS (Madhivanan et al., Citation2013).
Two studies found that financial incentives were associated with improved targeting of HTS, as a greater proportion of incentivized tests resulted in HIV diagnoses compared to traditional HTS outreach (McCoy et al., Citation2013; Nglazi et al., Citation2012). Only one study – of a combined intervention with adolescents in South Africa – found that incentives were not associated with HTS uptake as more youth received HTS at a separate clinic, rather than through the incentive program (Black et al., Citation2014).
In addition, three studies assessed the association between financial incentives and the one-time behavior of linkage to care following an HIV diagnosis. A U.S.-based study found incentives did not significantly increase linkage to care within three months of an HIV diagnosis (El-Sadr, Branson, & Beauchamp, Citation2015). The other studies, conducted in India and Swaziland, found that incentives increased ART initiation and linkage to care, respectively, following a positive HIV test (McNairy et al., Citation2016; Solomon et al., Citation2014).
Table 3. Studies of financial incentives on HTS and linkage to care outcomes.
Unconditional cash transfers
The single study of UCTs for linkage to care found that, for PLHIV, receiving the South Africa Disability Grant was associated with reporting ART initiation (Phaswana-Mafuya, Peltzer, & Petros, Citation2009) (). However, the weak study design and the UCT eligibility requirement of low CD4 counts suggest caution in interpreting this finding. No studies assessed UCTs and HIV testing.
Transportation assistance
Only one study, of a pilot referral intervention in Tanzania, assessed transportation assistance (). It found that the provision of a transportation allowance and community escort was associated with a trend of higher registration at the HIV clinic within six months of diagnosis (Nsigaye et al., Citation2009). No studies assessed transportation assistance and HTS.
Table 4. Studies of other provision interventions on HTS and linkage to care outcomes.
Protection interventions
Savings (individual and group)
Two studies assessed savings and HTS uptake; one focused on individual savings and one on group savings (). The first found that individual savings, either alone or in combination with other HES and sexual health support, did not increase self-reported testing uptake among adolescent girls in Uganda (Austrian & Muthengi, Citation2014). In the other, participants in a multi-component intervention including group savings in Malawi were nearly twice as likely to report having undergone HTS compared to a control group, though the study did not measure the association between HTS uptake and the savings component independently (Galvao, Citation2015; Weinhardt et al., Citation2014). No savings studies assessed an outcome related to linkage to care.
Income generation
Only one qualitative study in Kenya evaluated involvement in an income generating activity (IGA) and HTS (). It found that being a member of a basket weaving cooperative likely created barriers to HTS as members’ higher social status was associated with a perception of greater consequences for HIV disclosure and more concern over HIV-related stigma (Gnauck et al., Citation2013). No studies assessed IGAs and linkage to care.
Table 5. Studies of protection interventions on HTS and linkage to care outcomes.
Promotion interventions
Microcredit
Two studies assessed microcredit interventions and HTS (). A study in South Africa, which provided women with group microcredit, gender and HIV training and community mobilization found that participants were more likely to report accessing HTS than matched controls (Pronyk et al., Citation2008). A study in Haiti found that women involved in microcredit for 12 months or more were no more likely than those participating for less than 12 months to report having ever accessed HTS (Rosenberg, Seavey, Jules, & Kershaw, Citation2011). No studies assessed microcredit interventions and linkage to care.
Vocational and entrepreneurial training
Only one study assessed HTS uptake among participants in an integrated agricultural training, group savings, and HIV and gender education intervention in Malawi, finding that participants in the combined intervention had nearly double the odds of reporting HTS uptake compared to a control group (Galvao, Citation2015; Weinhardt et al., Citation2014) (). No studies assessed vocational or entrepreneurial training and linkage to care.
Employment support
One study assessed HTS uptake among youth in South Africa participating in an HIV, gender, and violence prevention training combined with support to find work or establish a business. It found that, over the course of the intervention, the proportion of male participants reporting HTS increased, but there was no significant increase for females (Jewkes et al., Citation2014). A study conducted in the United States with a diverse population of PLHIV found that use of vocational rehabilitation services, which included vocational counseling and related services to facilitate employment, was associated with higher rates of reported access to medical care (Conyers & Boomer, Citation2014) ().
Table 6. Studies of promotion interventions on HTS and linkage to care outcomes.
Discussion
To achieve the UNAIDS 90-90-90 global targets, traditional approaches must be complemented by innovative strategies to increase routine testing among high-risk groups, and increase linkage to care and treatment initiation. No evidence was found linking CCTs, food assistance, financial education and training, or education support with either testing or enrollment in care. Across the 20 studies on these parts of the cascade, only one intervention (financial incentives) had more than two studies and, with 11 studies, provides the preponderance of evidence in this paper.
Provision interventions demonstrate mostly positive findings for HTS and linkage to care. Financial incentives, in particular, are a pragmatic intervention to motivate uptake of these critical, yet discrete services. This review found evidence that financial incentives – in some cases even very small ones – are consistently and independently linked with higher testing uptake among adults in a range of contexts. Two of three studies also found that financial incentives increased ART initiation or linkage to care. These studies indicate that financial incentives may influence testing and enrollment in care in a number of ways: by directly compensating for the real costs of seeking services such as transportation or lost wages; by helping people overcome present-biased perspective or other psychological barriers to testing and care initiation; or even by providing an economic justification to seek services or start a conversation with partners about testing and care, thereby reducing the associated stigma or social pressures (Sibanda et al., Citation2016; Thornton, Citation2008). The evidence also shows that incentives to promote first-time testing or routine testing among high risk groups could be an important intervention to increase new case finding and testing yield, thereby maximizing HTS funding compared to standard testing approaches. All studies of financial incentives relied on clinical or program records to confirm HTS and care initiation outcomes, which are more reliable and valid than the self-reported outcomes that were used in most of the other studies in this paper. While promising for both outcomes, further research would support a better understanding of the contexts and populations or sub-groups for which incentives are most effective, and inform incentive levels that are both efficacious and cost effective.
There is surprisingly limited evidence for transportation assistance related to these outcomes. Only one study assessed transport support and found that incentives were associated with a strong positive trend (an increase from 18 percent to 64 percent) in clinical registration following an HIV diagnosis, but the study did not report whether the increase was statistically significant. While mobile- and self-testing have reduced the transport barrier for HTS where they are available, transport vouchers could also be a promising intervention to increase HTS and linkage to care after diagnosis. However, they may not have the same ability to overcome psychological or social barriers as broader financial incentives. No studies evaluated HES support and self-testing, though this could be an area for future exploration as self-testing becomes more available and the economic and psychosocial barriers to self-testing are better understood.
Evidence is sparse related to protection and promotion interventions, likely because direct, provision-based HES interventions are most intuitive for achieving one-time or infrequent outcomes like HTS and linkage to care, while protection and promotion support may be overly complex for these objectives. Looking at the three studies of protection interventions together, there are no emergent trends. The evidence for promotion interventions (n = 5) is similarly diverse though all but one reported positive results, with no negative findings. The three combined interventions – all of which had explicit HIV prevention and gender components – had positive findings in relation to HTS, possibly indicating that promotion-focused interventions could augment traditional HIV prevention efforts to encourage testing. Group-based interventions such as savings, IGAs, or microcredit could influence both testing and linkage to care by helping to pay for associated costs and/or providing social support, but are only practical if other economic, social or health outcomes are also desired (as was the case in the studies in this review). In some contexts it may be appropriate to integrate or promote routine testing within these HES interventions, utilizing group cohesion to encourage uptake.
While financial incentives were largely assessed independently, 25 percent of the studies in this paper (or 44 percent of the non-financial incentives studies) assessed integrated interventions, without isolating the direct association of any one intervention component on the outcomes. This limits our understanding of the contribution, if any, of each intervention component to the outcomes of interest. No study in this review assessed both HTS and linkage to care outcomes. With the advent of the universal test and treat approach, linkage to care following diagnosis is an area of renewed emphasis for epidemic control, yet early research on the approach shows that treatment initiation is the weakest of 90-90-90 targets (Plazy et al., Citation2016). Given that treatment initiation following diagnosis is a common attrition point within the HIV treatment cascade, this could be an area for future research on promising HES approaches such as cash and non-cash incentives.
The study limitations are discussed in greater detail in the first paper in this series (Swann Citation2018a). They include the introduction of reviewer bias in the inclusion of a quality assessment, which was mitigated through the creation of a structured codebook and using two reviewers. Categorization of studies into each intervention and outcome was done through a thorough assessment of the study details; when methodological details were limited categorization was based careful review of available information. Linkage to care was particularly varied in terms of outcome measures though we opted for inclusiveness, given the intention of this study. Given the variation in study characteristics, there may be additional trends which were not identified from the analytical framework used.
Conclusions
This evidence base points to the effectiveness of financial incentives for increasing HTS uptake and yield. Incentives also show some promise for increasing linkage to care and ART initiation. Evidence for other HES interventions is too sparse to identify any trends, though this limited evidence is expected based on the theories of change linking individual and household economics with HTS and care initiation. Given the discrete nature of these behaviors, it is logical that the most studied – and found to be mostly effective – HES approaches are similarly targeted and discrete, rather than more traditional, longer-term economic strengthening. The types of economic interventions most frequently used to support this portion of the HIV cascade actually do not focus on strengthening household economics, and instead work by using tangible incentives to shift the psychology of individuals in a way that encourages testing and enrollment in care.
Acknowledgments
We would like to acknowledge the excellent work of Cheryl Tam, formerly of FHI 360, in screening and assessing the quality of articles included in this review. We are grateful to several FHI 360 colleagues, including Whitney Moret for her contributions to this manuscript, Allison Burns and Tamara Fasnacht for their support in the literature search, and Jenae Tharaldson for her assistance preparing the manuscript. Finally, we would like to thank the researchers, donors and practitioners who participated in the half-day consultative meeting held on 13 July 2016 for their thoughtful input and expertise on this topic.
Disclosure statement
The author has no conflicts of interest to declare.
ORCID
Mandy Swann http://orcid.org/0000-0003-0348-8024
Additional information
Funding
Notes
1 Green (positive) = positive findings on one or more primary outcome of interest and no negative findings; blue (null) = no effect/association was observed on primary outcome(s) or study was under-powered; yellow (mixed) = a mix of positive and negative results on primary outcomes of interest; and red (negative) = negative findings on one or more primary outcomes of interest and no positive findings.
References
- Adato, M., & Bassett, L. (2012). Social protection and cash transfers to strengthen families affected by HIV and AIDS. In M. Adato, & L. Bassett (Eds.), Social protection and cash transfers to strengthen families affected by HIV and AIDS (pp. 1–3). Washington: International Food Policy Research Institute.
- Anema, A., Vogenthaler, N., Frongillo, E. A., Kadiyala, S., & Weiser, S. D. (2009). Food insecurity and HIV/AIDS: Current knowledge, gaps, and research priorities. Current HIV/AIDS Reports, 6(4), 224–231. doi: 10.1007/s11904-009-0030-z
- Austrian, K., & Muthengi, E. (2014). Can economic assets increase girls’ risk of sexual harassment? Evaluation results from a social, health and economic asset-building intervention for vulnerable adolescent girls in Uganda. Children and Youth Services Review, 47, 168–175. doi: 10.1016/j.childyouth.2014.08.012
- Bassett, I. V., Wilson, D., Taaffe, J., & Freedberg, K. A. (2015). Financial incentives to improve progression through the HIV treatment cascade. Current Opinion in HIV and AIDS, 10(6), 451–463. doi: 10.1097/coh.0000000000000196
- Black, S., Wallace, M., Middelkoop, K., Robbertze, D., Bennie, T., Wood, R., & Bekker, L.-G. (2014). Improving HIV testing amongst adolescents through an integrated Youth Centre rewards program: Insights from South Africa. Children and Youth Services Review, 45, 98–105. doi: 10.1016/j.childyouth.2014.03.025
- Centers for Disease Control and Prevention. (2014). Understanding the HIV care continuum.
- Cluver, L. D., Operario, D., Lane, T., & Kganakga, M. (2011). “I can’t go to school and leave her in so much pain”: Educational shortfalls among adolescent “young carers” in the South African AIDS epidemic. Journal of Adolescent Research, 27(5), 581–605. doi: 10.1177/0743558411417868
- Conyers, L., & Boomer, K. B. (2014). Examining the role of vocational rehabilitation on access to care and public health outcomes for people living with HIV/AIDS. Disability and Rehabilitation, 36(14), 1203–1210. doi: 10.3109/09638288.2013.837968
- Deb, A., & Kubzansky, M. (2012). Bridging the gap: The business case for financial capability. New York: Monitor Group and Citi Foundation.
- DFID. (2014). Assessing the strength of evidence. London: DFID.
- El-Sadr, W., Branson, B., & Beauchamp, G. (2015). Effect of financial incentives on linkage to care and viral suppression: HPTN 065. Seattle: CROI.
- Galárraga, O., Genberg, B. L., Martin, R. A., Laws, M. B., & Wilson, I. B. (2013). Conditional economic incentives to improve HIV treatment adherence: Literature review and theoretical considerations. AIDS and Behavior, 17(7), 2283–2292. doi: 10.1007/s10461-013-0415-2
- Galvao, L. W. (2015). Outcomes of a large-scale multilevel economic and food security structural intervention on HIV vulnerability in rural Malawi: The SAGE4health study. Paper presented at the 2015 APHA annual meeting & expo, Chicago, IL.
- Gnauck, K., Ruiz, J., Kellett, N., Sussman, A., Sullivan, M. A., Montoya, M., … Mwanthi, M. A. (2013). Economic empowerment and AIDS-related stigma in rural Kenya: A double-edged sword? Culture Health & Sexuality, 15(7), 851–865. doi: 10.1080/13691058.2013.789127
- Govindasamy, D., Ford, N., & Kranzer, K. (2012). Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: A systematic review. AIDS, 26(16), 2059–2067. doi: 10.1097/QAD.0b013e3283578b9b
- Guo, Y., Li, X., & Sherr, L. (2012). The impact of HIV/AIDS on children’s educational outcome: A critical review of global literature. AIDS Care, 24(8), 993–1012. doi: 10.1080/09540121.2012.668170
- Haukoos, J. S., Witt, M. D., Coil, C. J., & Lewis, R. J. (2005). The effect of financial incentives on adherence with outpatient human immunodeficiency virus testing referrals from the emergency department. Academic Emergency Medicine, 12(7), 617–621. doi: 10.1197/j.aem.2005.02.016
- Heise, L., Lutz, B., Ranganathan, M., & Watts, C. (2013). Cash transfers for HIV prevention: Considering their potential. Journal of the International AIDS Society, 16, 18615. doi: 10.7448/ias.16.1.18615
- Jewkes, R., Gibbs, A., Jama-Shai, N., Willan, S., Misselhorn, A., Mushinga, M., … Skiweyiya, Y. (2014). Stepping stones and creating futures intervention: Shortened interrupted time series evaluation of a behavioural and structural health promotion and violence prevention intervention for young people in informal settlements in Durban, South Africa. BMC Public Health, 14, 1571. doi: 10.1186/1471-2458-14-1325
- Khan, A., Qazi, R., Nazim, N., & Khan, A. (2012). Response to conditional cash transfers: Prevention of HIV infection in wives in Pakistan. Journal of the International AIDS Society, 15, 150.
- Lankowski, A. J., Siedner, M. J., Bangsberg, D. R., & Tsai, A. C. (2014). Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: A systematic review. AIDS and Behavior, 18(7), 1199–1223. doi: 10.1007/s10461-014-0729-8
- Madhivanan, P., NiranjanKumar, B., Shaheen, R., Jaykrishna, P., Ravi, K., Gowda, S., … Krupp, K. (2013). Increasing antenatal care and HIV testing among rural pregnant women with conditional cash transfers to self-help groups: An evaluation study in rural Mysore, India. Journal of Sexually Transmitted Diseases, 2013, 1–6. doi: 10.1155/2013/971458
- McCoy, S. I., Shiu, K., Martz, T. E., Smith, C. D., Mattox, L., Gluth, D. R., … Padian, N. S. (2013). Improving the efficiency of HIV testing with peer recruitment, financial incentives, and the involvement of persons living with HIV infection. JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(2), e56–e63. doi: 10.1097/QAI.0b013e31828a7629
- McNairy, M., Lamb, M., Gachuhi, A., Nuwagaba-Biribonwoha, H., Burke, S., Mazibuko, S., … Link4Health Study Group. (2016). LINK4HEALTH: a cluster-randomized controlled trial evaluating the effectiveness of a combination strategy for linkage to and retention in HIV care in Swaziland. Journal of the International AIDS Society, 19(Suppl 15), 66.
- Musheke, M., Ntalasha, H., Gari, S., McKenzie, O., Bond, V., Martin-Hilber, A., & Merten, S. (2013). A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Public Health, 13(1), 442. doi: 10.1186/1471-2458-13-220
- Nglazi, M. D., van Schaik, N., Kranzer, K., Lawn, S. D., Wood, R., & Bekker, L. G. (2012). An incentivized HIV counseling and testing program targeting hard-to-reach unemployed men in Cape Town, South Africa. JAIDS Journal of Acquired Immune Deficiency Syndromes, 59(3), E28–E34. doi: 10.1097/QAI.0b013e31824445f0
- Nsigaye, R., Wringe, A., Roura, M., Kalluvya, S., Urassa, M., Busza, J., & Zaba, B. (2009). From HIV diagnosis to treatment: Evaluation of a referral system to promote and monitor access to antiretroviral therapy in rural Tanzania. Journal of the International AIDS Society, 12, 31. doi: 10.1186/1758-2652-12-31
- Pettifor, A., MacPhail, C., Nguyen, N., & Rosenberg, M. (2012). Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS and Behavior, 16(7), 1729–1738. doi: 10.1007/s10461-012-0240-z
- Phaswana-Mafuya, N., Peltzer, K., & Petros, G. (2009). Disability grant for people living with HIV/AIDS in the Eastern Cape of South Africa. Social Work in Health Care, 48(5), 533–550. doi: 10.1080/00981380802595156
- Plazy, M., Farouki, K. E., Iwuji, C., Okesola, N., Orne-Gliemann, J., Larmarange, J., … Dray-Spira, R. (2016). Access to HIV care in the context of universal test and treat: Challenges within the ANRS 12249 TasP cluster-randomized trial in rural South Africa. Journal of the International AIDS Society, 19(1), 20913. doi: 10.7448/ias.19.1.20913
- Pronyk, P. M., Kim, J. C., Abramsky, T., Phetla, G., Hargreaves, J. R., Morison, L. A., … Porter, J. D. H. (2008). A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS, 22(13), 1659–1665 doi: 10.1097/QAD.0b013e328307a040
- Rosenberg, M. S., Seavey, B. K., Jules, R., & Kershaw, T. S. (2011). The role of a microfinance program on HIV risk behavior among Haitian women. AIDS and Behavior, 15(5), 911–918. doi: 10.1007/s10461-010-9860-3
- Rutherford, S. (2000). The poor and their money. New Delhi: Oxford University Press.
- Sibanda, E., Tumushime, M., Mufuka, J., Gudukeya, S., Mavedzenge, S. N., Bautista-Arredondo, S., … Cowan, F. (2016). Results of a cluster-randomized trial of non-financial incentives to increase uptake of couples counselling and testing among clients attending PSI mobile HIV services in rural Zimbabwe. Journal of the International AIDS Society, 19(Supplement 5), 62.
- Snilstveit, B., Vojtkova, M., Bhavsar, A., Stevenson, J., & Gaarder, M. (2016). Evidence & gap maps: A tool for promoting evidence informed policy and strategic research agendas. Journal of Clinical Epidemiology, 79, 120–129. doi: 10.1016/j.jclinepi.2016.05.015
- Solomon, S. S., Srikrishnan, A. K., Vasudevan, C. K., Anand, S., Kumar, M. S., Balakrishnan, P., … Lucas, G. M. (2014). Voucher incentives improve linkage to and retention in care among HIV-infected drug users in Chennai, India. Clinical Infectious Diseases, 59(4), 589–595. doi: 10.1093/cid/ciu324
- Swann, M. (2018a). Economic strengthening for HIV prevention and risk reduction: A review of the evidence. AIDS Care. doi: 10.1080/09540121.2018.1479029
- Swann, M. (2018b). Economic strengthening for retention in HIV care and adherence to antiretroviral therapy: A review of the evidence. AIDS Care. doi: 10.1080/09540121.2018.1479030
- Thornton, R. L. (2008). The demand for, and impact of, learning HIV status. American Economic Review, 98(5), 1829–1863. doi:10.1257/aer.98.5.1829.
- UNAIDS Joint United Nations Programme on HIV/AIDS. (2017). Ending AIDS: Progress towards the 90–90–90 targets global AIDS update. Geneva: UNAIDS.
- Weinhardt, L. S., Galvao, L. W., Mwenyekonde, T., Grande, K. M., Stevens, P., Yan, A. F., … Watkins, S. C. (2014). Methods and protocol of a mixed method quasi-experiment to evaluate the effects of a structural economic and food security intervention on HIV vulnerability in rural Malawi: The SAGE4health study. SpringerPlus, 3, 296. doi: 10.1186/2193-1801-3-296
- Woller, G. (2011). Livelihood and food security conceptual framework. Washington, DC: FHI 360, LIFT.
Appendices
Appendix 1. PRISMA diagram on selection of studies for full review
Appendix 2. HES and HIV outcomes evidence map for full review