ABSTRACT
Despite a growing population of youth living with HIV, few interventions have been developed to address their unique mental health needs and to promote resilience. Based on our prior needs assessment, a mental health intervention, Sauti ya Vijana ( The Voice of Youth), was developed to address identified mental health needs and promote resilience. The intervention emphasized resilience strategies for identifying and coping with stressful events, supporting strong familial and social relationships, and planning for a safe and healthy living environment through stigma reduction, planning for disclosure, and instilling hope for the future. Ten group sessions (two of which were joint youth/caregiver sessions) and two individual sessions were developed around these three resilience domains. Youth living with HIV (average age 17.4 years), who were receiving antiretroviral therapy and attending HIV adolescent clinic in Tanzania were randomized to intervention or treatment as usual. Trained group leaders led the intervention sessions. Near perfect program fidelity by the group leaders and unanimous acceptance of the intervention by the youth was documented. SYV successfully promoted youth resilience as measured by youth-reported utilization of new coping skills, improved peer and caregiver relationships, reduced stigma, and improved confidence to live positively according to their personal values.
Introduction
Adolescence is a complex developmental stage that is further complicated by living with HIV. It is a time when the peer group and ‘fitting in’ become top priorities, and isolation due to HIV-related stigma can be devastating. Concerns of accidental disclosure of the youth’s HIV status followed by rejection by friends, may lead to poor antiretroviral therapy (ART) adherence. Romantic relationships may also pose a unique challenge for youth as they negotiate fear of disclosure, condom use, higher risk sex, and potential transmission of HIV to others (Mhalu, Leyna, & Mmbaga, Citation2013; Ramaiya et al., Citation2016; Toska, Cluver, Hodes, & Kidia, Citation2015).
Mental health difficulties may further complicate life among youth living with HIV (YLWH). Symptoms of depression, trauma, and/or other emotional difficulties were present in approximately 32% of 280 YLWH interviewed across two clinic sites in Moshi, Tanzania (D. Dow, Shayo et al., July Citation2016; D. E. Dow, Turner et al., Citation2016). This prevalence of mental health difficulties was similar to other reports from Kenya (Kamau, Kuria, Mathai, Atwoli, & Kangethe, Citation2012), Zambia (Menon, Glazebrook, Campain, & Ngoma, Citation2007), Uganda (Musisi & Kinyanda, Citation2009), and Botswana (Lowenthal et al., Citation2012). In a study from Rwanda, the odds of having mental health symptoms were higher among children and youth living with or affected by HIV compared to HIV-unaffected peers (Betancourt et al., Citation2014).
Despite these challenges, youth can survive and even thrive while living with HIV. Resilience, the capacity to overcome adversity with positive outcomes, is a function of several important factors, including the ability to identify and cope with stressful events, to maintain strong familial and social relationships, and to cultivate a safe and healthy living environment (Bhana et al., Citation2016). A study evaluating predictors of mental health resilience among HIV-orphans found that physical health; food security; better caregiving; peer relationship quality; and lower exposure to community violence, bullying or stigma were associated with better and sustained mental health resilience (Collishaw, Gardner, Lawrence Aber, & Cluver, Citation2016). The literature on resilience in YLWH is limited, but what exists emphasizes the importance of learning how to identify and harness resilience factors and to test interventions for YLWH (Betancourt, Meyers-Ohki, Charrow, & Hansen, Citation2013).
Key resilience factors helped inform the design of this mental health intervention that was tailored to YLWH in Moshi, Tanzania. The primary objective of the overall study was to examine the feasibility and acceptability of the group delivered mental health intervention. The aim of the present analysis was to describe the impact the intervention had on youth resilience.
Methods
The study was an individually randomized group treatment feasibility study comparing a mental health intervention called Sauti ya Vijana (SYV; The Voice of Youth) to treatment as usual (TAU) (NCT02888288). TAU consisted of routine care with clinic counselors or social workers. There were no clinical psychologists or psychiatrists available for referral in this region. YLWH who were 12–24 years of age, attending adolescent HIV clinic at either Kilimanjaro Christian Medical Centre or Mawenzi Regional Referral Hospital, and receiving ART, and who knew their HIV status were eligible to participate. Recruitment into the study took place during these adolescent HIV clinics. For the purpose of this analysis, we reported on participants randomized to the intervention arm; youth randomized to TAU did not participate in any study group activities.
Sauti ya Vijana (SYV)
This mental health intervention was developed to address the primary mental health needs and worries expressed by youth during formative research by our team using a mixed-methods design (D. E. Dow, Turner et al., Citation2016; Gichane et al., Citation2017; Ramaiya et al., Citation2016). The session-by-session protocol, outlined in , was informed by existing evidence-based treatment models selected to improve treatment adherence, reduce mental health symptoms, and increase youth resilience. SYV consisted of 10 group sessions and two individual sessions. Group sessions were delivered in the native language, Kiswahili, and each lasted approximately 90 minutes.
The first four group sessions encouraged youth to identify their worries about living with HIV and to utilize relaxation methods such as deep breathing and mindfulness activities to cope with distress. Youth learned to use the cognitive triangle (Cognitive Behavioral Therapy, CBT) to identify and change negative thoughts, feelings, and behaviors, to understand and cope with HIV-related stress (Cohen, Mannarino, & Deblinger, Citation2017).
Emphasis on nurturing strong familial and social relationships was targeted for group sessions five through seven with a joint youth/caregiver meeting designed to prepare caregivers to listen and support their youth in trauma narratives. Trauma narratives involved youth telling about when they first learned they have HIV. The approach to the trauma narrative was adapted from CBT practice and from the adaptation for bereaved orphaned children in Moshi, Tanzania (Deblinger, Pollio, & Dorsey, Citation2016; O’Donnell et al., Citation2014). The approach to the narrative using a timeline – “What happened before”, the event: “How I learned about having HIV/AIDS”, “What happened after”, and “How I am now” – was adapted from Interpersonal Psychotherapy (IPT) (Markowitz, Svartberg, & Swartz, Citation1998; Weissman, Markowitz, & Klerman, Citation2007). Youth then identified their social support system using concentric circles of support, another activity adapted from IPT, to consider who in their lives provide the most intimate, close, and extended support.
Group sessions eight through ten incorporated prior session teachings to cultivate a safe and healthy living environment through choices influenced by stigma, education about HIV, disclosure, and values. The underlying assumptions and practice of motivational interviewing (Miller, Citation2000; Miller & Rollnick, Citation2002, Citation2013) were used throughout the SYV intervention, but particularly in these final group meetings during which the youth worked to identify their values, how their values match their behavior, and how those values might inform their future goals.
Group leaders
SYV was led by group leaders between the ages of 24 to 30 years of age. The six group leaders (three male and three female) were chosen based on mixed experiences. Half of the group leaders had a lived experience (HIV-infected and graduated from the adolescent HIV clinic); others had prior experience in delivering a mental health intervention for children (O’Donnell et al., Citation2014). Education levels ranged from secondary school to higher education including a diploma in social work. All group leaders were fluent in Kiswahili and proficient in English. They underwent an extensive two-week, in-country SYV training by the lead U. S. based clinical psychologist and principal investigator using an explicit script for each group meeting. Group leaders continued to practice each weekly session under supervision one day prior to the Saturday group session. Group leaders were sex-concordant with participants in their group. Two group leaders led the intervention and one group leader kept detailed session notes for each youth and ensured protocol delivery using the session-specific fidelity checklist. Session notes and fidelity checklists were reviewed during supervision meetings after completion of each weekly session.
Participants
Participants were individually randomized in three waves and grouped by sex and clinic site. Group size ranged from 8 to 11 participants. If siblings were enrolled, the first sibling was randomized and the second sibling was assigned to the same treatment arm to minimize contamination. When agreed to by the youth participants, their identified caregivers, who were already aware of the youth’s HIV status, were invited to participate in two joint youth/caregiver sessions and a home visit. The inclusion of caregivers in the protocol was designed to engage caregiver participation to strengthen familial relationships and help caregivers support their youth, but was not required for youth enrollment. Session content was delivered in same-sex groups, but male and female groups joined together for the final fun game and refreshments at the end of each session. All youth and caregivers who participated in SYV signed confidentiality agreements to reduce worry about potential gossip from group participation. Participants received mobile telephone call reminders the day before each session; transportation was reimbursed, and a small snack was provided. The intervention sessions built on prior learning and skills, so participants who missed more than two sessions were not able to continue in their assigned wave, but they were offered a future opportunity to participate in the intervention.
Plan of analysis
Baseline characteristics of youth from their pre-intervention questionnaire and chart review were summarised with simple statistics using Stata 15 software (StataCorp, College Station, Texas). The pre-intervention questionnaire included demographic, socioeconomic, mental health, risk-taking behavior, and HIV-related information. Participants were directly asked if they knew how they acquired HIV in the questionnaire. If they were unsure, criteria used to define perinatal HIV transmission included age at HIV diagnosis or age at ART initiation being less than 10 years as determined from retrospective chart review or youth report that their mother died of HIV in the questionnaire. If these criteria were met, youth were designated as perinatal transmission; otherwise, transmission status was categorized as uncertain.
Feasibility and acceptability of the intervention were assessed through quantitative and qualitative methods. SYV group leaders documented attendance, punctuality, and fidelity to the intervention using detailed fidelity checklists. Fidelity checklists included a list of all the important teaching components in each session and were tracked by one of the trained SYV group leaders. If the topic was covered during the session, the group leader would check the box as well as track the amount of time required to complete each teaching objective. SYV group leaders also documented activity discussions during the sessions (example in ) and qualitative narratives from youth based on the weekly group sessions, individual session notes, and final exit interviews (examples in quotes throughout results). These findings were translated to English by SYV group leaders and extracted to examine whether YLWH found the intervention acceptable. Study results are presented based on resilience themes that emerged throughout the intervention content development and delivery ().
Table 1. Protocol components of Sauti ya Vijana (SYV).
Ethics
Participants 18 years or older provided written informed consent in the local language of Kiswahili. For participants under 18 years, a parent or guardian provided permission along with youth assent. Participants who turned 18 years during the study were re-consented. The Duke University Medical Center Institutional Review Board, the KCMC Research Ethics Committee, and the Tanzanian National Institute Medical Review approved the study protocol.
Results
A total of 58 youth received the SYV intervention. The average age was 17.4 years; 15 (25.9%) were double orphans (both parents deceased), and 13 (22.4%) identified a grandparent as the primary caregiver (). The majority, 50 (86.2%), were perinatally HIV-infected. Approximately one-quarter reported having ever had sexual intercourse of whom 38.5% had disclosed their status to their partner.
Table 2. Description of the participants.
Feasibility
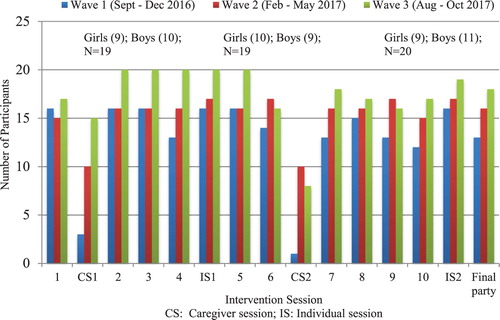
Feasibility was demonstrated with good attendance and fidelity to the intervention. Youth attendance to all sessions in wave 1 was 77%, 85% in wave 2, and 92% in wave 3. Caregiver attendance was 13% in wave 1; 63% in wave 2; 69% in wave 3 (). In total, four (7%) youth randomized to intervention never attended a group session; another three (5%) missed more than 2 sessions and were not able to continue in their current wave. Fidelity to the SYV protocol was documented at nearly 100%.
Acceptability
Identifying and coping with stressful events
Youth were very interested to learn more about mental health and resilience through the weekly group sessions. Common stressful events and ways of coping identified by youth are listed in . The stress and worries described by youth were similar across each wave in both female and male groups. Groups discussed common coping strategies that could be helpful or unhelpful, and new ways of coping were introduced. New coping strategies included deep breathing, relaxation techniques, and mindfulness activities, use of the cognitive triangle, and mind distraction/concentration games such as counting backwards.
Table 3. Youth Identified Common Stressors and Worries and Ways of Coping
They really enjoyed this [deep breathing] because they said they could feel the relaxation in their bodies after doing it. (Male group leader)
The triangle helped a lot. Sometimes she was thinking, maybe she should not take medicine, but when she thought about the triangle it made her change her mind … it helped her to take medicine. (16 year old female, reported by female group leader)
He likes the triangle because he never knew the connection between thoughts, feelings, and behavior and that he can change it. (22 year old male, reported by male group leader)
Two male youth in Wave 1 came to group sessions inebriated by alcohol. After individual discussions and counseling by the group leaders, the boys slowly changed their behavior to become very engaged in the group sessions. One of the boys mentioned that sometimes he began drinking alcohol by 7 am because it helped reduce his worries. In an individual session, he told the group leader that he used the cognitive triangle, but some of his worries or bad thoughts were very difficult, and the triangle did not always work. With time, additional education from the sessions, and support from the group, by session seven neither youth arrived to group sessions under the influence of alcohol or drugs. After completing SYV , one of the boys went on to become a peer youth leader, teaching an HIV education curriculum as a role model in the adolescent clinic.
Promoting strong familial and social relationships
Strengthening familial and social relationships was a key component of SYV. As noted in the youth list of worries, they experienced stress around the fear of disclosure to others and stress remembering events surrounding their own HIV disclosure. To help youth deal with the trauma related to learning about their own HIV status, they were asked to share individually with a group leader their memories about when they learned they have HIV. Then, if willing, they shared a part of their story with their group, and finally, with their caregiver. The purpose was for youth to practice talking about this traumatic experience, to normalize the experience with support from their peers, and for their caregiver to listen and hear the story from the youth’s perspective. All youth were willing to share their story individually with the group leader and just over half (55%) shared a part of their memories with the group. In total, only 40% of caregivers attended session six, but those that did found the youth narrative helpful in understanding the youth’s experience.
“It was her first time to share her memory. She said she felt peace after sharing and also she said that she has reduced her worries after sharing because she said she is letting go of bad things and she stays and keep good things.” (16 year old female, reported by female group leader)
“He really enjoys the sessions and it helps his life since he started. He wants to sit down with his family to discuss his HIV status and how it affects his life and how he can improve his life.” (22 year old male, reported by male group leader)
“He chose to share the story. He mentions that through sharing the part of the story, it helped him to reduce the stress. He said that through talking about the difficult memory, it helped him to have more confidence. He will teach his friends about how to talk about their memories because he has seen the positive helpful changes in himself that can result.” (18 year old male, reported by male group leader)
During the trauma narratives, many youth had asked their caregiver why they had to take medication and were not told the truth. Many figured out their HIV diagnosis on their own. Youth described relief at the opportunity to engage in these difficult conversations with their caregivers and, when possible, to cultivate a closer and more supportive relationship. Caregivers who attended the joint sessions also commented that they were seeing positive changes in their youth by way of ART adherence, attitude, confidence, and reduced worries and anxiety.
Now she is very close to her mother and every Saturday session her mom asks what she learned, and she asks if there is another caregiver session. (16 year old female, reported by female group leader)
Sometimes he can find his uncle has thoughts about him. He used to teach his uncle relaxation techniques, which he has been taught from SYV Project. It helps in improving the relationship between them. Other times he tells his uncle not to think much about him, because now he values the medicines since they will help him to live without any problem and to reach his goals. (17 year old male, reported by male group leader)
He felt a lot better after sharing with his sister and that he had been feeling like he wanted to share for a long time. He said that now he will be planning to share with his stepmother. (21 year old male, reported by male group leader)
The peer support fostered during the intervention was also an important resilience component. Participants in each group attended the same HIV clinic, but became much closer in the small group sessions.
He found youth like him who are facing the same problem [HIV] and he took the problem as part of his life and sees himself the same as others. This problem doesn’t bother him anymore. (23 year old male, reported by male group leader)
She is happy and has peace. She is not sad anymore because she used to stay lonely and was not happy, but through interacting with her fellow participants it makes her feel okay. (16 year old female, reported by female group leader)
Safe and healthy living environment
Though many youth participating in the study lived in poverty, the intervention sought to enhance a safe and healthy living environment through improving disclosure skills, identifying and realizing one’s own life values, and reducing stigma. The treatment protocol dichotomized stigma into internal stigma and external stigma (Gray, Citation2002). Many youths were unaware of their own self-stigmatizing beliefs. Using the cognitive triangle, youth learned to change the self-stigmatizing thoughts, leading to a change in their feelings and behaviors. Many youth felt the stigma session and use of the cognitive triangle around stigma was one of the most powerful sessions.
“She realized that there is no need to stigmatize yourself. The triangle has changed her.” She said, “You may see they stigmatize you, but sometimes you have to give yourself hope. Everyone should fight with her or his situation.” (16 year old female, reported by female group leader)
He increased more in confidence about his condition and the sessions helped him to decrease negative thoughts. His previous stress related to HIV has gone away. (21 year old male, reported by male group leader)
Youth shared stories about stigma at home. Some youth felt isolated in the family; several youth reported having to use their own plate, cup, and utensils. Others reported experiencing stigma at school, both from the teachers and the students. SYV used education about HIV transmission to help them build confidence to educate their community as to why people should not be afraid of someone living with HIV.
“She wants to give stigma education about how you can [and cannot] get HIV, because through the session she learned different things and reduced trauma, and now she has peace and is feeling good. She thanked us for teaching because she lost hope, but now she discovered she is not alone.” (14 year old female, reported by female group leader)
Disclosure in the context of enhancing a safe and healthy living environment was another favorite topic. Youth discussed reasons they might choose to disclose their HIV status, such as at home to family members to gain adherence support, or to sexual partners to help protect them from HIV transmission. They also described fear and reluctance about disclosure, due to the fear of isolation, gossip, and abandonment by lovers, family, and friends. Youth engaged in role-playing using five steps of disclosure and became more comfortable with the idea; however, no youth reported actually disclosing their HIV status to a new person during the intervention.
Using principles of motivational interviewing (Miller, Citation2000; Miller & Rollnick, Citation2002), youth were encouraged to identify their personal values. Many named health, education, and honesty as priority values; they also noted the difficulties in living according to those values in the context of living with HIV. They were able to imagine themselves after six months and how their behavior might be more compatible with these values. During final exit interviews, youth unanimously said they would recommend the SYV intervention to other YLWH.
Adaptations were made to the intervention based on youth and caregiver feedback and group leader observations. Punctuality was a challenge. A reward system was started to encourage punctual arrivals to group sessions. Youth who arrived on time received a sticker and the three youth with the most stickers were given a small prize (such as socks, soap, and sugar). Caregiver attendance was also a challenge with only 13% attendance across caregiver sessions in the first wave. Home visits were instituted prior to the intervention in subsequent waves, which improved caregiver attendance to over 60%. Finally, group leaders described secondary trauma after listening to many difficult and challenging life stories of youth. All group leaders received training about handling their own feelings and setting boundaries between youth and group leaders.
Discussion
Results from the study indicated that the SYV mental health intervention led by group leaders was highly feasible and acceptable and increased resilience among Tanzanian youth. Few interventions have been published that address mental health and resilience factors among HIV-infected youth in Africa. A U. S. based program, CHAMPS+, has been adapted to the South African context (Bhana et al., Citation2014; Mellins et al., Citation2014) and more recently to Thailand (Pardo et al., Citation2017); however, this intervention targets younger children (10–14 years old) in a family-centered approach. An unpublished six-session program from Rwanda, Kigali Imbereheza Project (KIP), sought to address mental health and ART adherence of youth living with HIV led by indigenous youth leaders (Donenberg et al., Citation2017). In Zimbabwe, cognitive behavioral therapy using lay health care workers showed success, though focused on adults (Chibanda et al., Citation2016).
SYV incorporated joint caregiver sessions to underscore the importance of promoting strong family relationships in youth resilience (Gichane et al., Citation2017). Three dedicated sessions (initial individual session, and group sessions five and six) focused on youth narratives, an approach that was used with prior success among orphaned children suffering from grief (O’Donnell et al., Citation2014). Use of the narrative was a highly unique aspect of the intervention; it helped to reduce trauma, normalize experiences among peers, and promote communication between caregivers and youth. As has been reported in prior research (Ramos et al., Citation2018), the majority of youth in this study had learned their HIV status on their own. Although all caregivers who listened to the youth’s narratives were already aware of the youth’s HIV status, few had ever heard the story from the youth’s perspective.
The narratives also prepared youth for disclosure to others. Of those youth who reported sexual activity, just over a third (38.5%) had disclosed their HIV status to their sexual partner. The majority of youth found these sessions very helpful, though not all youth were ready to share their very personal story with others. It was always the decision of the youth whether or not to share their memories of learning about their HIV status.
Limitations of the study included lack of professionally trained local clinical psychologists or psychiatrists to assist with referrals and intervention delivery. Despite this limitation, the group leaders did an outstanding job addressing mental health needs to improve resilience among youth. There exists the possibility of desirability bias given that the fidelity checklists and session notes were documented by the group leaders who had a vested interest in the success of the project. Feedback from clinical providers and caregivers outside the context of this project suggest that dramatic improvement was noted in medication adherence, confidence, and desire of youth in SYV to teach their peers what they learned during the intervention. Finally, considering the social protection aspects of resilience found in the Child-sensitive HIV-inclusive Social Protection Conceptual Framework (Toska et al., Citation2016), SYV focused on the care and capabilities inputs to address mental health, stigma, life skills, and strengthening the social support network. This project was not able to address structural components such as poverty that, no doubt, influence protective factors and resilience. Youth with food insecurity, lack of school tuition, and unemployment were referred to the hospital-based social worker to assist participants within the local standard of care.
Future steps
Based on youth discussions during SYV, future interventions for this population should also include content regarding gender-based violence and sexual reproductive health. As is promoted by the UNAIDS three lens approach (UNAIDS, Citation2018), the success of SYV was largely due to engaging youth and group leaders before and during the intervention content design. Early engagement of local governments and policymakers will also be necessary to ensure implementation when SYV is found to be efficacious as well as feasible and acceptable.
SYV is among the first mental health interventions published for youth living with HIV in Africa. The intervention was highly acceptable, feasible, and shows great promise in promoting resilience in this vulnerable and neglected population.
Acknowledgements
We would like to thank the six incredible group leaders involved in the project (Suzan Kitomari, Stanny Komu, Nickson Kwayu, Happyness Ngowi, Leonia Rugalabamu, Melkizedick Urio) whose content delivery and empathy were key to the success of the project. We thank the clinical staff and social workers at Kilimanjaro Christian Medical Centre and Mawenzi Regional Referral Hospital Care and Treatment Center for their help in recruitment and referrals. Finally, we are so grateful to the youth participants and their caregivers for their trusting participation in the project and making this work very meaningful for all involved.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Betancourt, S., Kanyanganzi, F., Fawzi, M. C., Sezibera, V., Cyamatare, F., … Kayiteshonga, Y. (2014). HIV and child mental health: A case-control study in Rwanda. Pediatrics, 134(2), e464–e472. doi: 10.1542/peds.2013-2734
- Betancourt, T. S., Meyers-Ohki, S. E., Charrow, A., & Hansen, N. (2013). Annual research review: Mental health and resilience in HIV/AIDS-affected children – a review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 54(4), 423–444. doi: 10.1111/j.1469-7610.2012.02613.x
- Bhana, A., Mellins, C. A., Petersen, I., Alicea, S., Myeza, N., Holst, H., … McKay, M. (2014). The VUKA family program: Piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care, 26(1), 1–11. doi: 10.1080/09540121.2013.806770
- Bhana, A., Mellins, C. A., Small, L., Nestadt, D. F., Leu, C. S., Petersen, I., … McKay, M. (2016). Resilience in perinatal HIV+ adolescents in South Africa. AIDS Care, 28(Suppl. 2), 49–59. doi: 10.1080/09540121.2016.1176676
- Chibanda, D., Weiss, H. A., Verhey, R., Simms, V., Munjoma, R., Rusakaniko, S., … Araya, R. (2016). Effect of a primary care-based psychological intervention on symptoms of common mental disorders in Zimbabwe: A randomized clinical trial. JAMA, 316(24), 2618–2626. doi: 10.1001/jama.2016.19102
- Cohen, J., Mannarino, A., & Deblinger, E. (2017). Treating trauma and traumatic grief in children and adolescents. New York: The Guilford Press.
- Collishaw, S., Gardner, F., Lawrence Aber, J., & Cluver, L. (2016). Predictors of mental health resilience in children who have been parentally bereaved by AIDS in urban South Africa. Journal of Abnormal Child Psychology, 44(4), 719–730. doi: 10.1007/s10802-015-0068-x
- Deblinger, E., Pollio, E., & Dorsey, S. (2016). Applying trauma-focused cognitive-behavioral therapy in group format. Child Maltreatment, 21(1), 59–73. doi: 10.1177/1077559515620668
- Donenberg, G., Cohen, M., Ingabire, C., Fabri, M., Kendall, A., & Remera, E. (2017). Changes in ART adherence among Rwandan youth following a trauma-informed cognitive behavioral intervention. 9th IAS conference on HIV science (IAS 2017), Paris, France.
- Dow, D., Shayo, A., Turner, E., Mmbaga, B., Cunningham, C., & O’Donnell, K. (2016, July). Mental health and associated virologic outcomes among HIV-infected adolescents in Tanzania. Poster TUPEB123. Paper presented at the international AIDS conference, Durban, South Africa.
- Dow, D. E., Turner, E. L., Shayo, A. M., Mmbaga, B., Cunningham, C. K., & O’Donnell, K. (2016). Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care, 28(7), 825–833. doi: 10.1080/09540121.2016.1139043
- Gichane, M. W., Sullivan, K. A., Shayo, A. M., Mmbaga, B. T., O, K., Cunningham, D., … E, D. (2017). Caregiver role in HIV medication adherence among HIV-infected orphans in Tanzania. AIDS Care, 1–5. doi: 10.1080/09540121.2017.1391986
- Gray, A. J. (2002). Stigma in psychiatry. Journal of the Royal Society of Medicine, 95(2), 72–76. doi: 10.1177/014107680209500205
- Kamau, J. W., Kuria, W., Mathai, M., Atwoli, L., & Kangethe, R. (2012). Psychiatric morbidity among HIV-infected children and adolescents in a resource-poor Kenyan urban community. AIDS Care, 24(7), 836–842. doi: 10.1080/09540121.2011.644234
- Lowenthal, E., Lawler, K., Harari, N., Moamogwe, L., Masunge, J., Masedi, M., … Gross, R. (2012). Rapid psychosocial function screening test identified treatment failure in HIV+ African youth. AIDS Care, 24(6), 722–727. doi: 10.1080/09540121.2011.644233
- Markowitz, J. C., Svartberg, M., & Swartz, H. A. (1998). Is IPT time-limited psychodynamic psychotherapy? The Journal of Psychotherapy Practice and Research, 7(3), 185–195.
- Mellins, C. A., Nestadt, D., Bhana, A., Petersen, I., Abrams, E. J., Alicea, S., … McKay, M. (2014). Adapting evidence-based interventions to meet the needs of adolescents growing up with HIV in South Africa: The VUKA case example. Global Social Welfare, 1(3), 97–110. doi: 10.1007/s40609-014-0023-8
- Menon, A., Glazebrook, C., Campain, N., & Ngoma, M. (2007). Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: Implications for peer-support programs. Journal of Acquired Immune Deficiency Syndromes, 46(3), 349–354. doi: 10.1097/QAI.0b013e3181565df0
- Mhalu, A., Leyna, G. H., & Mmbaga, E. J. (2013). Risky behaviours among young people living with HIV attending care and treatment clinics in Dar Es Salaam, Tanzania: Implications for prevention with a positive approach. Journal of The international Aids Society, 16, 17342. doi: 10.7448/IAS.16.1.17342
- Miller, W. R. (2000). Motivational enhancement therapy: Description of counseling approach. In J. J. Boren, L. S. Onken, & K. M. Carroll (Eds.), Approaches to drug abuse counseling (pp. 89–93). Bethesda, MD: National Institute on Drug Abuse.
- Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change. New York: Guilford Press.
- Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). New York, NY: Guilford Press.
- Musisi, S., & Kinyanda, E. (2009). Emotional and behavioural disorders in HIV seropositive adolescents in urban Uganda. East African Medical Journal, 86(1), 16–24. doi: 10.4314/eamj.v86i1.46923
- O’Donnell, K., Dorsey, S., Gong, W., Ostermann, J., Whetten, R., Cohen, J. A., … Whetten, K. (2014). Treating maladaptive grief and posttraumatic stress symptoms in orphaned children in Tanzania: Group-based trauma-focused cognitive-behavioral therapy. Journal of Traumatic Stress, 27(6), 664–671. doi: 10.1002/jts.21970
- Pardo, G., Saisaengjan, C., Gopalan, P., Ananworanich, J., Lakhonpon, S., Nestadt, D. F., … McKay, M. M. (2017). Cultural adaptation of an evidence-informed psychosocial intervention to address the needs of PHIV+ youth in Thailand. Global Social Welfare, 4(4), 209–218. doi: 10.1007/s40609-017-0100-x
- Ramaiya, M. K., Sullivan, K. A., Donnell, K. O., Cunningham, C. K., Shayo, A. M., Mmbaga, B. T., & Dow, D. E. (2016). A qualitative exploration of the mental health and psychosocial contexts of HIV-positive adolescents in Tanzania. PLoS One, 11(11), e0165936. doi: 10.1371/journal.pone.0165936
- Ramos, J. V., Mmbaga, B. T., Turner, E. L., Rugalabamu, L. L., Luhanga, S., Cunningham, C. K., & Dow, D. E. (2018). Modality of primary HIV disclosure and association with mental health, stigma, and antiretroviral therapy adherence in Tanzanian youth living with HIV. AIDS Patient Care and STDs, 32(1), 31–37. doi: 10.1089/apc.2017.0196
- Toska, E., Cluver, L. D., Hodes, R., & Kidia, K. K. (2015). Sex and secrecy: How HIV-status disclosure affects safe sex among HIV-positive adolescents. AIDS Care, 27(Suppl. 1), 47–58. doi: 10.1080/09540121.2015.1071775
- Toska, E., Gittings, L., Hodes, R., Cluver, L. D., Govender, K., Chademana, K. E., & Gutierrez, V. E. (2016). Resourcing resilience: Social protection for HIV prevention amongst children and adolescents in eastern and Southern Africa. African Journal of Aids Research, 15(2), 123–140. doi: 10.2989/16085906.2016.1194299
- UNAIDS. (2018). Youth and HIV. Accessed on August 17, 2018. Accessed at http://www.unaids.org/en/resources/documents/2018/youth-and-hiv
- Weissman, M., Markowitz, J., & Klerman, G. (2007). Clinician’s quick guide to interpersonal psychotherapy. New York: Oxford University Press.