ABSTRACT
We assessed attitudes to disclosure to new sexual partners and association with sexual behaviours among HIV-diagnosed gay, bisexual, and other men who have sex with men (GBMSM) in the UK Antiretrovirals, Sexual Transmission Risk and Attitudes (ASTRA) study in 2011-12. Among 1373 GBMSM diagnosed with HIV for ≥3 months and reporting sex in the past three months (84% on antiretroviral therapy (ART), 75% viral load (VL) ≤50c/mL), 56.3% reported higher sexual disclosure (“agree” or “tend to agree” with “I’d expect to tell a new partner I’m HIV-positive before we have sex”). GBMSM on ART with self-reported undetectable VL had lower disclosure than those on ART without self-reported undetectable VL and those not on ART. Higher sexual disclosure was associated with higher prevalence of CLS in the past three months; this was due to its association with CLS with other HIV-positive partners. Higher sexual disclosure was more common among GBMSM who had CLS with other HIV-positive partners only (72.1%) compared to those who had higher-risk CLS with HIV-serodifferent partners (55.6%), other CLS with HIV-serodifferent partners (45.9%), or condom-protected sex only (47.6%). Findings suggest mutual HIV-disclosure and HIV-serosorting were occurring in this population. Knowledge of VL status may have impacted on disclosure to sexual partners.
Background
Disclosure of HIV status to sexual partners has been considered an integral part of HIV prevention; it is theorised that disclosure is associated with increased condom use or adoption of seroadaptive practices, hence reducing HIV transmission risk (Marks & Crepaz, Citation2001; O’Connell, Reed, & Serovich, Citation2015; Serovich, Reed, O’Connell, & Laschober, Citation2018). However, it remains unclear whether increases in the prevalence of disclosure to sexual partners overall have any effect on reducing the prevalence of condomless sex (CLS) (Conserve, Groves, & Maman, Citation2015; Hirsch Allen et al., Citation2014; Przybyla et al., Citation2014; Wilson et al., Citation2016).
Since the introduction of widespread antiretroviral therapy (ART), evidence on the association between non-disclosure and condom use among HIV-diagnosed MSM has been mixed; certain studies found that non-disclosure was associated with higher prevalence of condomless sex or condomless sex with HIV-serodifferent partners (CLS-D) (Cook, Valera, & Wilson, Citation2015; Hirsch Allen et al., Citation2014; Klitzman et al., Citation2007; Morin et al., Citation2005; Parsons et al., Citation2005; Simon Rosser et al., Citation2008; Wilson et al., Citation2016), others found no evidence of an association (Kalichman, DiMarco, Austin, Luke, & DiFonzo, Citation2003; Marks & Crepaz, Citation2001; Poppen, Reisen, Zea, Bianchi, & Echeverry, Citation2005; Przybyla et al., Citation2014; Simoni & Pantalone, Citation2004; van Kesteren, Hospers, van Empelen, van Breukelen, & Kok, Citation2007), while some reported that non-disclosure was linked to condom-protected sex (Abler et al., Citation2015; Klitzman et al., Citation2007; Serovich et al., Citation2018; Simon Rosser et al., Citation2008). Studies that examined levels of disclosure to sexual partners showed that those who disclose to some partners tend to report higher levels of condomless sex compared to those who disclose to none or most/all partners (Abler et al., Citation2015; Brown, Serovich, Kimberly, & Umasabor-Bubu, Citation2015; Durham et al., Citation2013; Parsons et al., Citation2005; Simon Rosser et al., Citation2008). Only two studies from the UK (2008–09) (Elford, Ibrahim, Bukutu, & Anderson, Citation2008; Fox et al., Citation2009) showed prevalence estimates of disclosure to sexual partners, but none examined associations between disclosure and condomless sex.
Following the publication of conclusive evidence on the absence of risk of HIV transmission through condomless anal sex when the HIV-positive partner is on virally suppressive ART, (Rodger et al., Citation2016, Citation2019) the role of disclosure in reducing HIV transmission may be questioned. HIV-status disclosure to a sex partner is now not the most relevant factor in the decision to have condomless or condom-protected sex. In the current era of the “Undetectable = Untransmittable” (U = U) message (The Lancet HIV, Citation2017), communication about antiretroviral treatment/viral load status for an HIV-positive partner and about use of pre-exposure prophylaxis (PrEP) for an HIV-negative partner may be the most relevant factors.
The current study was carried out among HIV-diagnosed GBMSM attending for care in the UK in 2011–12. This may be regarded as the start of the “Treatment as Prevention” (TasP) era, a period of considerable changes in understanding of the impact of undetectable viral load on HIV transmission (Baggaley, White, & Boily, Citation2010; Cohen et al., Citation2011; Rodger et al., Citation2016). There is scarce information since this period on HIV-serostatus disclosure to new sexual partners among GBMSM in the UK, and whether this may be influenced by knowledge of personal viral load status. Our study aims to describe attitudes to disclosure to new sexual partners among sexually active HIV-diagnosed GBMSM in the early TasP era, to examine associations of self-reported viral load status and other factors with disclosure, and to assess associations of disclosure with sexual behaviours, including condomless sex. In the context of the rapidly changing climate of HIV prevention, these results will establish a baseline against which future studies of HIV-serostatus disclosure can be compared.
Methods
ASTRA study
The Antiretrovirals, Sexual Transmission Risk, and Attitudes (ASTRA) study recruited 3258 HIV-diagnosed men and women attending eight hospital HIV outpatient clinics in the UK during 2011–2012 (64% response rate) (Speakman et al., Citation2013). Participants completed a confidential, self-administered questionnaire that sought information on socio-demographic, HIV-related, health and lifestyle factors; sexual behaviours and attitudes. Consent to participate included permission to collect latest HIV plasma viral load from clinic records (latest value available to the participant).
The study was approved by the North West London REC 2 research ethics committee (10/H0720/70).
Attitudes to sexual disclosure
Participants stated their level of agreement to the statement “I‘d expect to tell a new partner that I’m HIV-positive before we have sex” on a 5-level Likert scale (strongly agree, tend to agree, undecided/no opinion/not relevant to me, tend to disagree, and strongly disagree). A dichotomous “sexual disclosure” variable was created, combining “strongly” and “tend to agree” into one category indicating higher sexual disclosure, and “undecided”, “tend to disagree” and “strongly disagree” into another indicating lower sexual disclosure. This measure is based on participants’ stated attitudes to disclosure to new partners rather than directly measuring previous disclosure behaviour, which was not available.
Sexual behaviours
The questionnaire enquired about the following sexual behaviours in the previous three months (Daskalopoulou, Rodger, et al., Citation2017; Lampe et al., Citation2016): any anal or vaginal sex, any condomless sex (CLS), any CLS with HIV-serodifferent partners (CLS-D; CLS with a partner who did not have HIV or whose HIV-status the participant did not know), and any CLS with HIV-seroconcordant partners (CLS-C; CLS with a partner the participant knew also had HIV). Each participant who reported any anal or vaginal sex in the past three months was classified into one of four mutually exclusive categories of sexual behaviour in the past three months: (1.) Higher HIV risk CLS-D: CLS-D and either: not on ART (self-reported) at questionnaire completion or had latest clinic-recorded viral load > 50c/mL; (2.) Other CLS-D (but not higher HIV risk CLS-D); (3.) CLS-C only (no CLS-D partners); (4.) Condom-protected sex only. Self-reported STI diagnosis, group sex (with >1 other person on the same occasion) and use of the internet to find sex in the past three months were also assessed. Participants reported the total number of new sexual partners in the past year and whether they had ever received a diagnosis of hepatitis C.
This analysis includes ASTRA GBMSM diagnosed with HIV for at least three months on the date of questionnaire completion and reporting any anal or vaginal sex in the past three months. The first criterion was used to exclude sexual behaviour occurring prior to diagnosis of HIV, as most sexual behaviour questions had a three-month recall. The second criterion was used to confine the sample under study to those who were sexually active at the time of the questionnaire, and therefore for whom the questions on sexual disclosure were relevant.
Other questionnaire factors
Participants were asked if they had disclosed their HIV serostatus to anyone in their social circle (family, friends, a stable partner, work colleagues) (Daskalopoulou, Lampe, et al., Citation2017). Self-reported personal ART/viral load status was categorised as: not on ART; on ART with self-reported undetectable viral load (≤50c/mL); on ART without self-reported undetectable viral load (including viral load > 50c/mL, does not know viral load, and missing responses) (Lampe et al., Citation2016). Definitions of other sociodemographic, health and lifestyle factors considered are given in .
Table 1. Associations of socio-demographic, mental health, lifestyle, and HIV-related factors with higher sexual disclosure to new sexual partners (N = 1373 GBMSM diagnosed with HIV for ≥3 months and reported sex in the past three months).
Statistical analysis
The prevalence (95%CI) of sexual disclosure categories was assessed among GBMSM who had been diagnosed with HIV for at least 3 months and who were sexually active in the past three months. Associations were examined of various factors with higher sexual disclosure (versus lower sexual disclosure) using modified Poisson regression models with cluster-robust error variances, producing unadjusted and adjusted prevalence ratios (Zou, Citation2004). In the adjusted analyses, for each variable, a separate model was run that included core factors: age (<30, 30–39, 40–49, ≥50 years), ethnicity (white, black, all other), time since HIV diagnosis (3 months-2 years, 2–5, 5–10, 10–15, >15 years), ART status (on or off ART), and stable partner status (HIV-positive, HIV-serodifferent, no stable partner). For the variables related to ART and viral load there was no additional adjustment for ART status.
Associations were then examined of higher sexual disclosure with sexual behaviours (any condomless sex, group sex, use of the internet to find sex, sexually transmitted infections in the past three months; ≥10 new sexual partners in the past year and ever being diagnosed with hepatitis C.) For each sexual behaviour, separate modified Poisson regression models were run with adjustment for the core factors.
Multinomial logistic regression (MNL) was used to examine associations of higher sexual disclosure with different types of condomless sex according to the four-category variable of sexual behaviour. MSM who had higher HIV risk CLS-D (group 1), those who had other CLS-D (group 2), and those who had CLS-C only (group 3) were compared to those who had condom-protected sex only (group 4, reference category). Multivariable MNL included adjustment for all core factors excluding ART status; results are given as adjusted odds ratios with 95% CIs.
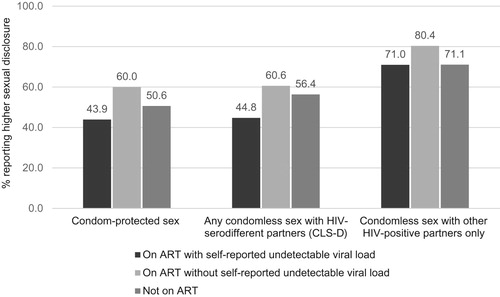
The percentage reporting of higher disclosure was then examined according to both self-reported ART/viral load status and the four-category variable of sexual behaviour.
Sensitivity analyses
In the first sensitivity analysis, sexual disclosure was reclassified into a categorical variable, according to levels of agreement to the statement “I would expect to tell a new partner that I’m HIV-positive before we have sex”: (i.) Higher sexual disclosure (strongly or tend to agree), (ii.) Undecided (undecided/no opinion/not relevant to me), and (iii) Lower sexual disclosure (strongly or tend to disagree). This categorisation aimed to disentangle any difference in the prevalence of sexual behaviours between categories (ii) and (iii), which were grouped in main analyses. Associations were then examined of the three categories of sexual disclosure and sexual behaviours, using modified Poisson regression adjusted for core factors. In the second sensitivity analysis, we restricted the sample to MSM who reported at least one new partner in the past 12 months and examined associations of higher sexual disclosure with sexual behaviours (Web appendix).
Results
ASTRA recruited 2248 HIV-diagnosed GBMSM. This analysis excludes GBMSM who were diagnosed with HIV for fewer than three months (n = 59), who did not report any anal or vaginal sex in the previous three months (n = 797), and who did not complete the sexual disclosure question (n = 19). Among the remaining 1373 MSM, 95.5% identified as gay, 87.7% were of white ethnicity, 84.1% were on ART, and 75.1% had viral load ≤ 50c/mL overall. Distribution of sexual disclosure attitudes (level of agreement to the statement “I’d expect to tell a new partner that I’m HIV-positive before we have sex”) was; 34.3% (95%CI 31.8–36%, n = 471) strongly agree, 22.0% (19.9–24.3%, n = 302) tend to agree, 14.1% (12.4–16.1%, n = 194) undecided, 19.0% (17.0–21.2%, n = 261) tend to disagree, and 10.6% (9.0–12.3%, n = 145) strongly disagree. Combining the first two categories (strongly/tend to agree), higher sexual disclosure was recorded in 56.3% (95%CI 53.7–58.9%, n = 773). Among GBMSM with higher sexual disclosure, 97.5% (n = 751) had disclosed their HIV serostatus to someone in their social circle (family, friends, a stable partner, work colleagues) and 2.5% (19) had not. The corresponding proportions among MSM with lower sexual disclosure were 94.0% (563) and 6.0% (36) respectively.
Associations of various factors with higher sexual disclosure were examined among the 1373 GBMSM who reported anal or vaginal sex in the past three months and had available disclosure information. () In unadjusted analysis, higher sexual disclosure was more prevalent among GBMSM who: were UK-born, had lower educational attainment, had greater financial hardship, had disclosed to at least one other person in their social circle, had an HIV-positive stable partner (versus HIV-serodifferent stable partner or no stable partner), and had clinic-recorded detectable viral load (). In addition, the prevalence of sexual disclosure varied according to self-reported ART/viral load status, being lowest among GBMSM on ART with self-reported undetectable viral load (53.4%), higher in GBMSM not on ART (59.9%) and highest among GBMSM on ART without self-reported undetectable viral load (66.9%). Age, time with diagnosed HIV, religion, employment status, social support, symptoms of depression and anxiety, alcohol consumption, and overall ART status (classified as on or off ART) were not associated with sexual disclosure. There was some evidence that disclosure varied according to ethnicity (being lower among men of Black ethnicity). After adjustment of each factor for core variables (age, ethnicity, time since diagnosis, stable partner status and ART status if relevant) the factors that were associated with higher sexual disclosure in unadjusted analysis remained associated (p < 0.05), with minor or no attenuation of estimates, except for ethnicity. In the adjusted analysis, compared to GBMSM on ART with self-reported undetectable viral load, the prevalence of sexual disclosure was 1.23 times higher among GBMSM on ART without self- reported undetectable viral load and 1.12 times higher among those not on ART (p = 0.004).
The prevalence of higher sexual disclosure (versus lower sexual disclosure) was examined according to sexual behaviours in the past three months (or in the past year). Compared to GBMSM with lower sexual disclosure, those with higher sexual disclosure had higher prevalence of: any condomless sex in the past three months (66.1% vs 52.2% for those with higher vs lower disclosure), and of lifetime hepatitis C diagnosis (21.9% vs. 10.2%), but lower prevalence of all other sexual behaviours (including group sex: 27.7% vs 35.9% and having ≥10 new sex partners in past 12 months: 10.6% vs 15.0%). After adjustment for core factors (), any condomless sex and lifetime hepatitis C remained more prevalent among those with higher sexual disclosure, while group sex in the past three months and ≥10 new sexual partners in the past year remained more prevalent among those with lower sexual disclosure (p < 0.05 for all). Higher sexual disclosure was not significantly associated with other STI diagnosis in the past three months.
Table 2. Adjusted associations of higher sexual disclosure with sexual behaviours (N = 1373 GBMSM diagnosed with HIV for ≥3 months who reported sex in the past three months).
The prevalence of higher sexual disclosure according to the four mutually exclusive categories of sexual behaviour in the past three months was: 55.6% in the higher HIV risk CLS-D group, 45.9% in the other CLS-D group, 72.1% in the CLS-C only group, and 47.6% among GBMSM in the condom-protected sex group. () Therefore, levels of sexual disclosure were higher for the men having condomless sex with HIV-positive partners only, compared to the other three groups (higher HIV risk CLS-D, other CLS-D, or condom-protected sex). After adjustment for core factors, this pattern remained: MSM with higher sexual disclosure were significantly more likely to have CLS with other HIV-positive partners only, relative to MSM who had condom-protected sex, (p < 0.001, ) but there was no significant difference in disclosure for men reporting CLS with HIV-serodifferent partners relative to condom-protected sex. This implies that disclosure of HIV-serostatus was highest with other HIV-positive partners.
Table 3. Associations of higher sexual disclosure with types of condomless sex (CLS) in past three months, relative to condom-protected sex (N = 1373 GBMSM diagnosed with HIV for ≥3 months and reporting sex in the past three months).
We examined the prevalence of higher sexual disclosure according to self-reported viral load on ART and by mutually exclusive sexual behaviour categories. () Among MSM who had either condom-protected sex or any condomless sex with HIV-serodifferent partners (including higher HIV risk CLS-D or other CLS-D), higher sexual disclosure tended to be more prevalent among MSM on ART without self-reported undetectable viral load and those not on ART, while disclosure was lower for MSM on ART with self-reported undetectable viral load (). However, among those reporting CLS with other HIV-positive partners only, disclosure was common throughout and varied less with self-reported ART/viral load status. This may indicate that the association of undetectable self-reported viral load with lower sexual disclosure was more apparent for those having condomless sex with HIV-serodifferent partners or condom-protected sex, and not for those having condomless sex with HIV-positive partners only (for whom viral load level is not relevant to disclosure).
Figure 1. Percentage reporting higher sexual disclosure by self-reported ART/viral load status and sexual behaviour group (N = 1373 GBMSM diagnosed with HIV for ≥3 months and reporting sex in the past three months).
Note: ART; Antiretroviral therapy; Any condomless sex with HIV-serodifferent partners includes higher HIV-risk CLS-D and other CLS-D
In sensitivity analyses, the pattern and magnitude of associations were similar to those in main analyses (Web appendix, Figures A and B).
Discussion
In this large multicentre study of HIV-diagnosed GBMSM attending for care in the UK, 56% of GBMSM who were sexually active in the past three months reported being likely to tell a new sexual partner that they were HIV-positive. Lower socio-economic status, UK place of birth, higher level of social disclosure, and having an HIV-positive stable partner were associated with higher levels of sexual disclosure. Disclosure was less prevalent among GBMSM with self-reported undetectable viral load on ART, compared to those without self-reported undetectable viral load on ART and those not on ART. Levels of sexual disclosure differed across sexual behaviour categories, with reported disclosure being higher among men having condomless sex with other HIV-positive partners only (CLS-C), compared to those having higher HIV risk CLS with HIV-serodifferent partners (CLS-D), other CLS-D, and condom-protected sex.
The prevalence of disclosure to sexual partners is extensively studied in the USA, but less so in the UK. A systematic review of HIV disclosure in 12 US studies (1997–2008) found the prevalence of non-disclosure to sexual partners among GBMSM to range from 20% to 46%, and to casual sex partners from 58% to 62% (Obermeyer, Baijal, & Pegurri, Citation2011). In the last decade, US studies have continued to report a wide range of estimates of non-disclosure among HIV-diagnosed GBMSM attending for HIV care. “Non-disclosure to any sexual partner” was as low as 9.2% in a telephone survey of 704 GBMSM (Durham et al., Citation2013). In a baseline assessment of an randomised controlled trial evaluating efficacy of a safer sex intervention, 31% of 138 GBMSM who reported having sex in the past six months “disclosed to less than 100% of all sex partners” (Przybyla et al., Citation2012) Among 991 young GBMSM ( < 25 years) attending for HIV care, 53.1% “did not disclose to a current sex/romantic partner who was not a boyfriend” (Cook et al., Citation2015) Among 250 MSM enrolled in a disclosure intervention, 28% of sexual encounters involved the participant “not disclosing at or before the specific sexual encounter” (Serovich et al., Citation2018). Evidence from the UK remains limited, with a cross-sectional questionnaire study of HIV-outpatients in Dublin’s largest HIV clinic (2012) reporting that 34% of 97 GBMSM “never disclosed to any of their casual partners in the last 6 months” (Murphy, Hevey, O’Dea, Ní Rathaille, & Mulcahy, Citation2015). In our study, 44% of GBMSM were classified as having lower sexual disclosure, a proxy for non-disclosure to new sex partners. Hence, comparison of non-disclosure prevalence estimates across studies is not straightforward due to varying definitions of non-disclosure behaviour and attitudes, and differences in types of partners studied, as well as differences in population demographics.
Poorer socioeconomic circumstances emerged as independent correlates of higher sexual disclosure in our study. GBMSM with lower educational attainment and higher financial instability were more likely to report sexual disclosure. However, there was no association with employment. This is in contrast to results from two earlier US studies of HIV-diagnosed outpatient GBMSM, in which no association was observed between education, income, and disclosure to casual sex partners in the previous three months (Parsons et al., Citation2005; Simon Rosser et al., Citation2008). In ASTRA, levels of sexual disclosure were highest among GBMSM with an HIV-positive stable partner, and lower among those with an HIV-negative or HIV-unknown serostatus stable partner or no stable partner. This association remained strong after adjustment for socio-demographic and HIV-related factors. HIV-positive GBMSM with HIV-positive stable partners may have had a positive experience of mutual disclosure, and therefore consider a higher likelihood of disclosure to a new sexual partner. Additionally, some HIV-positive GBMSM may be specifically seeking HIV-positive partners (sero-sorting), necessitating mutual disclosure. It was not possible to examine attitudes towards non-disclosure to new sex partners according to new partners’ HIV-serostatus. However, our findings are in line with those from a 2012 US survey of 138 HIV-diagnosed GBMSM outpatients who reported any sex in the past six months,(Przybyla et al., Citation2012) in which disclosure was highest to other HIV-positive partners, lower towards HIV-negative partners, and lowest towards HIV-unknown status casual partners.
Evidence on the association of disclosure to casual sex partners and condomless sex remains mixed. Four diverse US studies did not find significant differences in prevalence of condomless sex with HIV-serodifferent partners among those who did and did not disclose to casual sex partners (Poppen et al., Citation2005; Przybyla et al., Citation2014; Tieu et al., Citation2011; Wilson et al., Citation2016). In two other US studies, however, disclosure to casual partners was independently associated with lower odds of having condomless sex with HIV-serodifferent partners, after adjustment for socio-demographic and lifestyle factors (Morin et al., Citation2005; Simon Rosser et al., Citation2008). In our study, GBMSM with higher sexual disclosure were significantly more likely to have any condomless sex overall; however, this was driven by the fact that they were more likely to have condomless sex with other HIV-positive partners only. This may suggest that HIV transmission risk reduction is taking place, in the form of mutual disclosure between HIV-positive partners and HIV-serosorting. In addition, levels of disclosure were similar among men who had condomless sex with HIV-serodifferent partners (higher HIV risk or other CLS-D) and those who had condom-protected sex.
Our study showed higher prevalence of reported disclosure to new sex partners among men without self-reported undetectable viral load on antiretroviral therapy (ART), and among those not on ART, and lower disclosure among men with self-reported undetectable viral load on ART. The association was not attenuated by adjustment for socio-demographic and HIV-related factors. To date, few other observational studies have reported on this association, with mixed findings (Klitzman et al., Citation2007; O’Connell et al., Citation2015; Simon Rosser et al., Citation2008). Our findings may suggest that HIV-diagnosed GBMSM with perceived undetectable viral load on ART were less likely to disclose their HIV-serostatus due to knowledge of lack of HIV infectiousness. In addition, among men having condomless sex with other HIV-positive partners only, prevalence of disclosure was high regardless of self-reported ART/viral load category. In this context, if the partner’s HIV-positive status is known, HIV transmission and ART/viral load status are irrelevant. These findings provide some suggestion that early knowledge of the protective effect of undetectable viral load in the TasP era (2011/2012) may have influenced sexual attitudes and behaviours among some HIV-diagnosed GBMSM in the UK.
Our study is not without limitations. Disclosure to new sexual partners was not explicitly ascertained; agreement to the statement “I’d expect to tell a new partner that I’m HIV-positive before we have sex” was considered a proxy measure of higher disclosure instead. The direction of associations between various factors, sexual behaviours, and disclosure could not be ascertained in our cross-sectional study. Prevalence of disclosure may also be influenced by non-response and social desirability bias; if disclosure was less prevalent among those who refused study participation or those concerned about privacy and confidentiality, then our study would overestimate disclosure. While epidemiological studies such as ASTRA provide insight into patterns of non-disclosure among a clinic-based population, they are not able to capture the complex circumstances, motivations, and challenges that surround HIV-serostatus disclosure to new sexual partners. Importantly, ASTRA was completed during the early TasP era, so our data may not represent current levels of disclosure and sexual behaviour among HIV-diagnosed GBMSM in the UK. However, results are relevant in establishing a baseline against which future studies of HIV disclosure in the UK can be compared.
Conclusions
In the current era of “U = U” and PrEP, the role of HIV-serostatus disclosure to sex partners is changing. In addition to condom use and CLS between HIV-positive partners, options for avoiding or reducing HIV transmission risk include CLS between HIV-serodifferent partners when the HIV-positive partner has an undetectable viral load, and use of PreP for the HIV-negative partner. The role of disclosure of HIV serostatus in each of these contexts may differ. In this study of HIV-positive GBMSM, there was evidence that self-reported undetectable viral load was associated with lower sexual disclosure; it will be relevant for future studies to continue to assess the impact of self-reported viral load on sexual behaviour and attitudes, as ART use expands, and messages about HIV-prevention options continue to be disseminated.
Supplemental Material
Download MS Word (106.5 KB)Acknowledgements
All ASTRA study participants, ASTRA clinic teams: Royal Free Hospital: Alison Rodger; Margaret Johnson; Jeff McDonnell; Adebiyi Aderonke, Mortimer Market Centre: Richard Gilson; Simon Edwards; Lewis Haddow; Simon Gilson; Christina Broussard; Robert Pralat; Sonali Wayal, Brighton and Sussex University Hospital: Martin Fisher; Nicky Perry; Alex Pollard; Serge Fedele; Louise Kerr; Lisa Heald; Wendy Hadley; Kerry Hobbs; Julia Williams; Elaney Youssef; Celia Richardson; Sean Groth, North Manchester General Hospital: Ed Wilkins; Yvonne Clowes; Jennifer Cullie; Cynthia Murphy; Christina Martin; Valerie George; Andrew Thompson, Homerton University Hospital: Jane Anderson; Sifiso Mguni; Damilola Awosika; Rosalind Scourse East Sussex Sexual Health Clinic: Kazeem Aderogba; Caron Osborne; Sue Cross; Jacqueline Whinney; Martin Jones, Newham University Hospital: Rebecca O’Connell; Cheryl Tawana, Whipps Cross University Hospital: Monica Lascar; Zandile Maseko; Gemma Townsend; Vera Theodore; Jas Sagoo. ASTRA core team: Fiona Lampe; Alison Rodger; Andrew Speakman; Andrew Phillips. ASTRA data management: Andrew Speakman; Marina Daskalopoulou; Fiona Lampe. ASTRA advisory group: Lorraine Sherr; Simon Collins; Jonathan Elford; Alec Miners; Anne Johnson; Graham Hart; Anna-Maria Geretti; Bill Burman. CAPRA grant Advisory Board: Nick Partridge; Kay Orton; Anthony Nardone; Ann Sullivan. The ASTRA Study Group acknowledges the support of the NIHR, through the Comprehensive Clinical Research Network. FCL, ANP, AJR, AS, EW, LS, WJB conceived and designed the study. AS, AJR, EW, JM collected the data, MD drafted the manuscript and conducted all analyses. All authors contributed to data interpretation, writing, revision, and approval of the final manuscript. The views expressed in this manuscript are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Abler, L., Sikkema, K. J., Watt, M. H., Hansen, N. B., Wilson, P. A., & Kochman, A. (2015). Depression and HIV serostatus disclosure to sexual partners among newly HIV-diagnosed men who have sex with men. AIDS Patient Care and STDs, 29(10), 550–558. doi: 10.1089/apc.2015.0122
- Baggaley, R. F., White, R. G., & Boily, M.-C. (2010). HIV transmission risk through anal intercourse: Systematic review, meta-analysis and implications for HIV prevention. International Journal of Epidemiology, 39(4), 1048–1063. doi: 10.1093/ije/dyq057
- Brown, M. J., Serovich, J. M., Kimberly, J. A., & Umasabor-Bubu, O. (2015). Disclosure and self-efficacy among HIV-positive men who have sex with men: A comparison between older and younger adults. AIDS Patient Care and STDs, 29(11), 625–633. doi: 10.1089/apc.2015.0133
- Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., … Fleming, T. R. (2011). Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine, 365(6), 493–505. doi: 10.1056/NEJMoa1105243
- Conserve, D. F., Groves, A. K., & Maman, S. (2015). Effectiveness of interventions promoting HIV serostatus disclosure to sexual partners: A systematic review. AIDS and Behavior, 19(10), 1763–1772. doi: 10.1007/s10461-015-1006-1
- Cook, S. H., Valera, P., & Wilson, P. A. (2015). HIV status disclosure, depressive symptoms, and sexual risk behavior among HIV-positive young men who have sex with men. Journal of Behavioral Medicine, 38(3), 507–517. doi: 10.1007/s10865-015-9624-7
- Daskalopoulou, M., Lampe, F. C., Sherr, L., Phillips, A. N., Johnson, M. A., Gilson, R., … Rodger, A. J. (2017). Non-disclosure of HIV status and associations with psychological factors, ART non-adherence, and viral load non-suppression among people living with HIV in the UK. AIDS and Behavior, 21(1), 184–195. doi: 10.1007/s10461-016-1541-4
- Daskalopoulou, M., Rodger, A. J., Phillips, A., Sherr, L., Elford, J., McDonnell, J., … Lampe, F. C. (2017). Condomless sex in HIV-diagnosed men who have sex with men in the UK: Prevalence, correlates, and implications for HIV transmission. Sexually Transmitted Infections, 93(8), 590–598. https://doi.org/sextrans-2016-053029 doi: 10.1136/sextrans-2016-053029
- Durham, M. D., Buchacz, K., Richardson, J., Yang, D., Wood, K., Yangco, B., … HOPS Investigators. (2013). Sexual risk behavior and viremia among men who have sex with men in the HIV outpatient study, United States, 2007–2010. JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(3), 372–378. doi: 10.1097/QAI.0b013e31828c20d8
- Elford, J., Ibrahim, F., Bukutu, C., & Anderson, J. (2008). Disclosure of HIV status. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47(4), 514–521. doi: 10.1097/QAI.0b013e318162aff5
- Fox, J., White, P. J., Macdonald, N., Weber, J., McClure, M., Fidler, S., & Ward, H. (2009). Reductions in HIV transmission risk behaviour following diagnosis of primary HIV infection: A cohort of high-risk men who have sex with men. HIV Medicine, 10(7), 432–438. doi: 10.1111/j.1468-1293.2009.00708.x
- Hirsch Allen, A. J., Forrest, J. I., Kanters, S., O’Brien, N., Salters, K. A., McCandless, L., … Hogg, R. S. (2014). Factors associated with disclosure of HIV status among a cohort of individuals on antiretroviral therapy in British Columbia, Canada. AIDS and Behavior, 18(6), 1014–1026. doi: 10.1007/s10461-013-0623-9
- Kalichman, S. C., DiMarco, M., Austin, J., Luke, W., & DiFonzo, K. (2003). Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine, 26(4), 315–332. doi: 10.1023/A:1024252926930
- Klitzman, R., Exner, T., Correale, J., Kirshenbaum, S. B., Remien, R., Ehrhardt, A. A., … Charlebois, E. (2007). It’s not just what you say: Relationships of HIV dislosure and risk reduction among MSM in the post-HAART era. AIDS Care, 19(6), 749–756. doi: 10.1080/09540120600983971
- Lampe, F., Daskalopoulou, M., Phillips, A., Speakman, A., Johnson, M., Gilson, R., … Rodger, A. (2016). Sexual behaviour among people with HIV according to self-reported antiretroviral treatment and viral load status. Aids (london, England), 30(11), 1745–1759. doi: 10.1097/QAD.0000000000001104
- The Lancet HIV. (2017). U=U taking off in 2017. The Lancet HIV, 4(11), e475. doi: 10.1016/S2352-3018(17)30183-2
- Marks, G., & Crepaz, N. (2001). HIV-positive men’s sexual practices in the context of self-disclosure of HIV status. Journal of Acquired Immune Deficiency Syndromes, 27(1), 79–85. doi: 10.1097/00042560-200105010-00013
- Morin, S. F., Steward, W. T., Charlebois, E. D., Remien, R. H., Pinkerton, S. D., Johnson, M. O., … Chesney, M. A. (2005). Predicting HIV transmission risk among HIV-infected men who have sex with men. JAIDS Journal of Acquired Immune Deficiency Syndromes, 40(2), 226–235. doi: 10.1097/01.qai.0000166375.16222.eb
- Murphy, P. J., Hevey, D., O’Dea, S., Ní Rathaille, N., & Mulcahy, F. (2015). Optimism, community attachment and serostatus disclosure among HIV-positive men who have sex with men. AIDS Care, 27(4), 431–435. doi: 10.1080/09540121.2014.987105
- Obermeyer, C. M., Baijal, P., & Pegurri, E. (2011). Facilitating HIV disclosure across diverse settings: A review. American Journal of Public Health, 101(6), 1011–1023. doi: 10.2105/AJPH.2010.300102
- O’Connell, A. A., Reed, S. J., & Serovich, J. A. (2015). The efficacy of serostatus disclosure for HIV transmission risk reduction. AIDS and Behavior, 19(2), 283–290. doi: 10.1007/s10461-014-0848-2
- Parsons, J. T., Schrimshaw, E. W., Bimbi, D. S., Wolitski, R. J., Gómez, C. A., & Halkitis, P. N. (2005). Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. Aids (London, England), 19(Suppl 1), S87–S97. doi: 10.1097/01.aids.0000167355.87041.63
- Poppen, P. J., Reisen, C. A., Zea, M. C., Bianchi, F. T., & Echeverry, J. J. (2005). Serostatus disclosure, seroconcordance, partner relationship, and unprotected anal intercourse among HIV-positive Latino men who have sex with men. AIDS Education and Prevention, 17(3), 227–237. doi: 10.1521/aeap.17.4.227.66530
- Przybyla, S., Golin, C., Widman, L., Grodensky, C., Earp, J. A., & Suchindran, C. (2014). Examining the role of serostatus disclosure on unprotected sex among people living with HIV. AIDS Patient Care and STDs, 28(12), 677–684. doi: 10.1089/apc.2014.0203
- Przybyla, S., Golin, C. E., Widman, L., Grodensky, C. A., Earp, J. A., & Suchindran, C. (2012). Serostatus disclosure to sexual partners among people living with HIV: Examining the roles of partner characteristics and stigma. AIDS Care, 25(5), 566–572. doi: 10.1080/09540121.2012.722601
- Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., van Lunzen, J., … Lundgren, J. (2016). Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA, 316(2), 171. doi: 10.1001/jama.2016.5148
- Rodger, A. J., Cambiano, V., Phillips, A. N., Bruun, T., Raben, D., Lundgren, J., … Janeiro, N. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428–2438. doi: 10.1016/S0140-6736(19)30418-0
- Serovich, J. M., Reed, S. J., O’Connell, A. A., & Laschober, T. C. (2018). Relationship between serostatus disclosure and categories of HIV transmission risk in men who have sex with men living with HIV. International Journal of STD & AIDS, 29, 744–750. doi: 10.1177/0956462417752267
- Simoni, J. M., & Pantalone, D. W. (2004). Secrets and safety in the age of AIDS: Does HIV disclosure lead to safer sex? Topics in HIV Medicine : A Publication of the International AIDS Society, USA, 12(4), 109–118.
- Simon Rosser, B. R., Horvath, K. J., Hatfield, L. A., Peterson, J. L., Jacoby, S., Stately, A., & the Positive Connections Team. (2008). Predictors of HIV disclosure to secondary partners and sexual risk behavior among a high-risk sample of HIV-positive MSM: Results from six epicenters in the US. AIDS Care, 20(8), 925–930. doi: 10.1080/09540120701767265
- Speakman, A., Rodger, A., Phillips, A. N., Gilson, R., Johnson, M., Fisher, M., … Lampe, F. C. (2013). The “antiretrovirals, sexual transmission risk and attitudes” (ASTRA) study. design, methods and participant characteristics. PloS One, 8(10), e77230. doi:10.1371/journal.pone.0077230
- Tieu, H.-V., Xu, G., Bonner, S., Spikes, P., Egan, J. E., Goodman, K., … Koblin, B. A. (2011). Sexual partner characteristics, serodiscordant/serostatus unknown unprotected anal intercourse and disclosure among human immunodeficiency virus-infected and uninfected black men who have sex with men in New York city. Sexually Transmitted Diseases, 38(6), 1. doi: 10.1097/OLQ.0b013e318203e2d7
- van Kesteren, N. M. C., Hospers, H. J., van Empelen, P., van Breukelen, G., & Kok, G. (2007). Sexual decision-making in HIV-positive men who have sex with men: How moral concerns and sexual motives guide intended condom use with steady and casual sex partners. Archives of Sexual Behavior, 36(3), 437–449. doi: 10.1007/s10508-006-9125-4
- Wilson, P. A., Kahana, S. Y., Fernandez, M. I., Harper, G. W., Mayer, K., Wilson, C. M., & Hightow-Weidman, L. B. (2016). Sexual risk behavior among virologically detectable human immunodeficiency virus-infected young men who have sex with men. JAMA Pediatrics, 170(2), 125–131. doi: 10.1001/jamapediatrics.2015.3333
- Zou, G. (2004). A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. doi: 10.1093/aje/kwh090
