ABSTRACT
Female sex workers (FSWs) are at increased risk of HIV and face significant barriers to clinic-based HIV testing, including provider stigma and privacy constraints. HIV self-testing (HIVST) has been proven to significantly increase HIV testing among FSWs. Less is known, however, about how FSWs make meaning of oral-fluid HIV self-tests, and the unintended ways they use and understand this novel technology. From October 2016 to March 2017, we conducted 61 in-depth interviews with FSWs (n = 31) in Kampala, Uganda. Eligible participants were: female, ≥18 years, exchanged sex for money or goods, and had not recently tested for HIV. We used inductive coding to identify emerging themes and re-arranged these into an adapted framework. Unintended desirable ways FSWs described self-testing included as a means to test others, to bolster their reputation as a health-conscious sex worker, and to avoid bearing witness to suffering at health facilities. Unintended undesirable meanings ascribed to self-testing included misunderstandings about how HIV is transmitted (via saliva versus blood) and whether self-tests also test for other infections. HIVST can increase FSWs’ knowledge of their own HIV status and that of their sexual partners, but messaging and intervention design must address misunderstandings and misuses of self-testing.
Trial registration: ClinicalTrials.gov identifier: NCT02846402.
Introduction
HIV testing is essential for both treatment and prevention of HIV infection. In sub-Saharan Africa, which accounted for 64% of all HIV infections in 2018 (UNAIDS, Citation2019), HIV testing is primarily conducted at healthcare facilities. However, numerous barriers to facility-based HIV testing exist, including long travel and wait times, and lack of privacy (Chanda, Perez-Brumer, et al., Citation2017; Musheke et al., Citation2013). HIV self-testing (HIVST) entails a person collecting their oral-fluid and interpreting their own test results; this approach allows for testing at a time and place of an individual’s choosing (WHO, Citation2020). HIVST has been proven to overcome barriers to facility-based testing and increase recent and frequent testing among diverse populations in different settings (Hatzold et al., Citation2019; Johnson et al., Citation2017). Numerous sub-Saharan African countries have recently expanded their HIV testing guidelines to include HIVST and are working to scale HIVST services nationally (HIVST.org, Citation2019; WHO, Citation2019).
HIVST has the potential to particularly benefit key populations that are at increased risk of HIV infection and have additional barriers to accessing traditional health services, including female sex workers (FSWs) (Baral et al., Citation2012; Chanda, Perez-Brumer, et al., Citation2017; Shannon et al., Citation2015). Previous studies have shown peer-delivered HIVST increases recent and repeat testing among FSWs in high HIV prevalence settings (Chanda, Ortblad, et al., Citation2017; Figueroa et al., Citation2015; Ortblad et al., Citation2017). However, other studies suggest that FSWs might have difficulties interpreting HIV self-test results and there remains uncertainty around unintended ways FSWs may use HIV self-tests (Ortblad, Kibuuka Musoke, et al., Citation2018; Ortblad, Musoke, et al., Citation2018).
In this study we use qualitative data to explore how FSWs in Kampala, Uganda use and make meaning of HIV self-tests and with what consequences, stratified by desirability (from a public health perspective) and intention (from an interventionist perspective). We conducted this research in Kampala, the capital city of Uganda, because there are ∼13,000 FSWs living there and one in three of these FSWs is estimated to be living with HIV (CDC, Citation2013). In this setting, FSWs are prioritized by the Ministry of Health in Uganda for the delivery of targeted HIV prevention and treatment interventions, but there are no HIV testing requirements for FSWs in this setting (Uganda Ministry of Health, Citation2020). Systematically capturing factors that lead to unintended outcomes of health interventions can help researchers and policy makers better plan for the future by recognizing potential intervention pitfalls and understanding an intervention's holistic value.
Methods
Study design
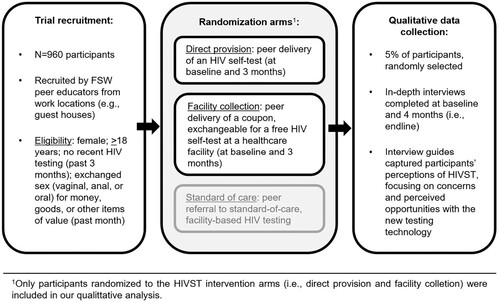
This qualitative study was part of a larger randomized trial (N = 960) designed to test the effect of two different peer-based HIVST delivery models on HIV testing outcomes (ClinicalTrials.gov: NCT02846402) (Ortblad et al., Citation2017). The trial design, recruitment process, and inclusion criteria are specified in . All peer educators were trained on how to counsel participants on HIV/STI prevention and facilitate linkage to free, facility-based treatment and prevention services. At enrollment, all participants were counseled on HIV testing and received a toll-free hotline number, which they were encouraged to call for referral to standard, facility-based HIV testing and treatment, or for guidance on HIVST (intervention arms only). The HIV self-tests delivered were the OraQuick Rapid HIV-1/2 Antibody Test (OraSure Technologies, Bethlehem, PA), which came with a pictorial and written step-by-step instruction guide (available in Luganda and English) on self-test use, results interpretation, and linkage to follow-up care.
The Institutional Review Board at the Harvard T. H. Chan School of Public Health (IRB16-0885) and Mildmay Uganda Research Ethics Committee (REF 0105 ± 2016) approved this study. All participants completed informed consent.
Data collection and analysis
We interviewed participants (in intervention arms only) at two time points to capture their perceptions of HIVST before and after having the opportunity to self-test. We reached saturation of themes before interviewing our target 5% of trial participants, but continued to collect data in the event that new themes arose. Qualitative interview guides were developed by the research team and refined after pilot testing. Coordination and invitation to interview was done in partnership with FSWs peer educators via phone or contact address. All interviews were conducted by a qualitative researcher (in Luganda or English) in a private setting of the participant’s choice, and were audiotaped, transcribed, and translated verbatim into English for analysis. Participants were compensated 16,500 Uganda Shillings (∼$5 USD) for their time and transportation costs.
We analyzed 61 transcripts from 31 participants: 31 baseline and 30 follow-up transcripts (4 months following enrollment). We used inductive coding on 16 information-rich transcripts to develop a list of hierarchical codes that were applied to all transcripts using Atlas.ti. After recognizing that participants were using the self-tests in unintended ways, coded text was re-arranged into a framework on unintended intervention outcomes adapted from work by Turcotte-Tremblay et al. (Citation2017). We evaluated unintended uses, meanings, and consequences of HIVST among participants, which we organized into desirable and undesirable categories. We defined “uses” as how and with whom participants describe using or intending to use the self-test. We defined “meaning” as participants’ attitudes, understandings and self-perceptions after having used the self-test. And we defined “consequences” as participants’ actions post HIVST.
Results
At enrollment, the median age of participants was 30 years and a majority of participants had completed primary or secondary education (81%, n = 25), . At four months, all participants (100%, n = 30) reported testing for HIV since the start of the trial and all but one reported using an HIV self-test (97%, n = 29) (Ortblad et al., Citation2017). Of the 30 participants who completed in-depth interviews at 4 months, 4 (13%) self-reported testing HIV positive.
Table 1. Participant characteristics at enrollment, n = 31.
In this section, unintended factors are classified according to whether they were desirable or undesirable (from the perspective of public health practitioners), and arranged along a uses, meaning, consequences axis (see ). While our results emphasize unintended consequences, we also briefly summarize intended consequences.
Table 2. Unintended uses, meanings and consequences of HIVST among FSW in Uganda.
Unintended uses of HIVST
Desirable
Participants talked extensively about their intention to test long-term clients and partners. Participants described happiness at the thought of administering HIVST on long-term clients “because of love … because I love him,” (age 35, baseline) and because testing had long been a source of tension with clients who say they intend to test but ultimately do not. With clients who are not routine or long-term, participants described that they most likely would not agree to test, but that the interaction with the client could be used as a proxy to gauge his status because “if testing scares a client off, you just know that there is something they are hiding,” (age 29, 4 months).
Along with testing or planning to test clients, participants described plans to test their children – however, no participant described actually undertaking this action.
Undesirable
As anticipated by program planners, some participants described using the self-tests incorrectly and misinterpreting self-test results. Moreover, two participants described coercive testing (e.g., wanting to test a fellow FSW who claimed to be negative). As a means to gauge whether the test really worked, one participant (age 29, 4 months) described her plan to conduct “my own little experiment” by underhandedly testing a friend who is known to be living with HIV. “I'll just tell her to, ‘rub this on your gums’ and then I'll know … if the tests are real.” This is undesirable because if an individual is adhering to an HIV treatment regimen, they may be virally suppressed and thus test negative despite living with HIV.
Unintended meanings of HIVST
Desirable
While it was expected that participants would favor HIVST over facility-based testing due to increased privacy, the intensity with which many participants described the “misery” and “awful” nature of HIV testing within health facilities was not expected. Participants described feeling physically sick as they watched others walk out of a testing room “with tears that you cannot hide” (age 24, baseline), weeping with grief or shouting “I am dead, mum, I am dead” (age 22, 4 months). One participant said “your heart shakes” (age 36, 4 months) and several participants said they say sorry to those who receive a positive HIV test result, which is obvious because the woman is grief stricken and has spent a longer time with the heath provider or is carrying “a bag full of medications” (age 28, baseline). Several participants said that while walking through corridors or sitting in a queue that they feel they are being constantly watched and judged by others awaiting their appointments.
In instances of a positive self-test result, participants described feeling better prepared for a facility-based confirmatory test because they knew what result to expect, which meant they could better maintain their composure and minimize unintentional disclosure.
One participant described how she was excited to begin testing her clients, which would allow her reputation as “the healthy sex worker” to spread, and this would make her more profitable:
I feel like if you ask them to test first, they will know you are serious about your health and that will attract more clients for you. They will tell their friends about the sex worker who is health conscious so they will also come and pay for healthy sex. (age 29, 4 months)
Undesirable
Participants described misunderstanding the self-test's results and accuracy window. At least one participant thought her negative test result implied that she had no HIV and no other sexually transmitted diseases. Another participant said that she could use the test in lieu of “running around and looking for PEP [post-exposure prophylaxis]” (age 29, 4 months) when a condom bursts or if a client commits rape, while another participant said that, “ … I can go and get the kit and test myself early, so I know where I stand” (age 37, 4 months).
Unprompted, participants also talked at length about how HIVST led to feelings of incredulity (about the results) and sparked questions about the nature of HIV transmission:
Because we have grown up being told that there is no HIV in saliva and that is why many people kiss the infected and get away with it. Now out of the blue, you guys come and say that HIV can be detected from the gums?! Trust me you are going to have a lot of trouble explaining yourselves to the masses until they understand you. (age 40, 4 months)
One participant reported that a group of participants all agreed to go for follow-up testing regardless of their self-test results “just to have proof” because they were incredulous about the self-test's accuracy given its reliance on saliva. Several participants seemed skeptical that “such a small bottle” used at home can give true HIV results.
Finally, two participants described wariness of the motives behind those introducing HIV self-tests in Uganda and wanted to know what foreign governments had to gain from this intervention, or whether the intervention team was part of “the illuminati” (a conspiracy group).
Unintended consequences of HIVST
Desirable
Among those with a reported HIV-negative status, the theme of “being more cautious and careful” (age 37, 4 months) by, for example, rethinking “live sex” (condomless sex), avoiding the urge to “get drunk and lose control” (age 35, 4 months) with clients, and reducing the current number of sexual partners emerged. A more cautious lifestyle was described as something that “made sense” because counseling, testing and learning one's status had reminded participants to “love life” and that “earnings may reduce, but what is more important is to stay healthy” age 32 (4 months). As one participant said, “Before I tested for HIV, I would struggle with the decision to say no especially when the money is good, but now I don’t anymore. It is either on or we don’t go at all” (age 37, 4 months). A similar, consistent theme did not emerge among those who disclosed a positive test result. Some participants who tested HIV positive described needing to protect their clients from infection, while others did not.
Another unexpected outcome of HIVST involved participants describing how knowing one's HIV-negative status compelled care seeking for other ailments, as it is common for them to avoid healthcare facilities for “aches and pains” or “strange bleeding” because they feared HIV testing.
Undesirable
Some participants described how they intend to use HIV self-tests to test clients and determine whether they would agree to condomless sex and thus earn more money per sexual transaction. The data did not suggest a pattern in terms of condomless sex, which was described by nearly all participants as something done to varying degrees depending on the status of the participant, the extent to which she needed to earn money that night, and her relationship to the client (i.e., length of the relationship and beliefs about the client’s HIV status).
As anticipated, participants said that a positive self-test result could spark thoughts of suicide, compel rash decisions, or cause participants to “forget everything for a moment, like the brain freezes and you can't even think of calling that referral number (for follow-up advice)” (age 30, baseline). Furthermore, some participants described how self-tests could lead to intimate partner violence, particularly if an FSW tests positive while her partner tests negative.
Intended: uses, meanings, and consequences
Participants emphasized that self-tests allowed individuals to control the testing experience as far as timing and place, which enabled privacy and mitigated unintentional disclosure. Participants also described how HIVST could allow those who test positive to grieve, which is not feasible in clinic-based settings.
Participants described HIVST as less burdensome and invasive, easily transportable and quick compared to clinic-based testing. Taking a self-test also bolstered a sense of control because respondents had accomplished something perceived as difficult and frightening (taking the test) and had come to terms with their HIV status. Participants also spoke at length about the happiness of avoiding facility-based providers who, when administering HIV tests, were often described in a negative light.
Discussion
This study found that FSWs engaged with HIV self-tests in both desirable and undesirable, unintended and intended ways. Unintended desirable findings included FSWs intending to use HIVST to test others, viewing HIVST as a means to avoid bearing witness to suffering at health facilities, and using HIVST to bolster their reputation as health-conscious sex workers. Unintended undesirable findings included some FSWs who described intending to test others (without understanding how viral suppression works), misunderstanding how to interpret self-test results, and expressing incredulity about the motives for those distributing HIVST. As intended by program planners, FSWs felt a sense of control from testing at a time and place of their choosing.
These findings can help inform the delivery of HIVST to FSWs and other high-risk groups in sub-Saharan African settings where HIVST is currently being scaled. Specifically, these findings can inform the development of new delivery models or other interventions that could supplement HIVST delivery to maximize health benefits. For example, many FSWs expressed an interest in using HIV self-tests to test others, including clients, long-term sexual partners, or children. Qualitative research in Uganda and Kenya suggests that secondary distribution – wherein an individual is given several self-tests that can be distributed in their social network – is possible, but that it can also spark conflict and thus requires pre-empting tense situations and mitigating violence (Maman et al., Citation2017; Matovu et al., Citation2017, Citation2018). Thus, new models for secondary HIV self-test delivery via FSWs should be explored to determine if secondary distribution is safe, and if it increases recent HIV testing and linkage to healthcare services among those receiving the self-tests.
Our findings are largely consistent with HIVST research in Uganda. Quantitative research with the same cohort of FSWs found that learning one's HIV status led to decreases in the severity of depressive symptoms (Ortblad et al., Citation2020) and knowledge of an HIV-negative status led to increases in condom use (Ortblad et al., Citation2019), both factors that may be at least partially explained by the qualitative data showing that HIVST sparked feelings of self-worth, and a desire to live healthy, full lives (Wachinger et al., Citation2020). A qualitative study among FSWs in Rakai, Uganda, which pre-empted the distribution of HIVST kits, found that FSWs perceived HIVST as advantageous because it bolsters privacy and convenience, but problematic because it circumvents formal counseling, which is echoed in our data stemming from actual experience (Burke et al., Citation2017).
Several findings highlight opportunities to reinforce or redirect course in terms of messaging around HIVST. For example, many FSWs were concerned that HIVST might lead to false perceptions about HIV transmission (i.e., via oral-fluid instead of via blood) and many FSWs had false perceptions about how soon HIVST could detect HIV following infection (i.e., immediately after a risky sexual encounter). To validate the new HIV testing technology, many FSWs were also interested in testing individuals they knew were living with HIV, which is problematic because individuals on HIV treatment can be virally suppressed and test negative (Cohen et al., Citation2016). These findings emphasize the importance of pairing HIV self-test delivery with some form of a counseling intervention to avoid the spread of misinformation. More research should be conducted to determine the appropriate level and form of counseling to deliver with HIVST.
This study must be viewed in light of limitations. First, women were only given two HIV self-tests (one at a time) with specific instructions to only test themselves. This may limit their likelihood to disclose alternative intentions or behaviors. Additionally, at the time these interviews were conducted, HIVST was only available for study purposes in Uganda, which may have affected responses, particularly incredulity about the validity of self-test results. Finally, FSWs in urban Kampala have access to free and FSW-focused health services, which might not reflect FSWs in other settings.
Overall, HIVST has the potential to improve the lives of FSWs. If not delivered with care, however, HIVST might result in unintended false perceptions of HIV transmission or individuals’ HIV status, thus interventions should be carefully developed to supplement HIVST delivery with adequate information to maximize the benefits of this new technology.
Acknowledgements
This study was funded by the International Initiative for Impact Evaluation (3ie). SM was supported by The Olympia-Morata-Program of Heidelberg University. KFO was supported by the National Institute for Mental Health (R01-MH113572 and K99-MH121166). CEO was supported in part by the National Institute on Drug Abuse (T32-DA013911) and the National Institute of Allergy and Mental Health (R25-MH083620). TB was funded by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professorship endowed by the German Federal Ministry of Education and Research. He was also supported by the Wellcome Trust, the European Commission, and the National Institute of Child Health and Human Development (R01-HD084233), the National Institute of Allergy and Infectious Disease (R01-AI124389 and R01-AI112339) and the Fogarty International Center (D43-TW009775). AMTT received a fellowship from the Canadian Institutes of Health Research (CIHR). Oral HIV self-tests were obtained from OraSure Technologies at cost.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Baral, S., Beyrer, C., Muessig, K., Poteat, T., Wirtz, A. L., Decker, M. R., Sherman, S. G., & Kerrigan, D. (2012). Burden of HIV among female sex workers in low-income and middle-income countries: A systematic review and meta-analysis. The Lancet Infectious Diseases, 12(7), 538–549. https://doi.org/10.1016/S1473-3099(12)70066-X
- Burke, V. M., Nakyanjo, N., Ddaaki, W., Payne, C., Hutchinson, N., Wawer, M. J., Nalugoda, F., & Kennedy, C. E. (2017). HIV self-testing values and preferences among sex workers, fishermen, and mainland community members in Rakai, Uganda: A qualitative study. PLOS One, 12(8), e0183280. https://doi.org/10.1371/journal.pone.0183280
- CDC. (2013). Crane survey: select results from recent surveys, Kampala 2012/3. Retrieved March 28, 2017, from http://documentslide.com/documents/crane-survey-select-results-from-recent-surveys-kampala-20123-men-who-have.html
- Chanda, M., Ortblad, K., Mwale, M., Chongo, S., Kanchele, C., Kamungoma, N., Fullem, A., Dunn, C., Barresi, L., Harling, G., Barnighausen, T., & Oldenburg, C. (2017). HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial. PLOS Medicine, 14(11), e1002442. https://doi.org/10.1371/journal.pmed.1002442
- Chanda, M., Perez-Brumer, A., Ortblad, K., Mwale, M., Chongo, S., Kamungoma, N., Kanchele, C., Barresi, L., Barnighausen, T., & Oldenburg, C. (2017). Barriers and facilitators to HIV testing among Zambia female sex workers in three transit hubs. AIDS Patient Care and STDs, 31(7), 290–296. https://doi.org/10.1089/apc.2017.0016
- Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., Hakim, J. G., Kumwenda, J., Grinsztejn, B., Pilotto, J. H. S., Godbole, S. V., Chariyalertsak, S., Santos, B. R., Mayer, K. H., Hoffman, I. F., Eshleman, S. H., Piwowar-Manning, E., Cottle, L., Zhang, X. C., … Fleming, T. R. (2016). Antiretroviral therapy for the prevention of HIV-1 transmission. New England Journal of Medicine, 375(9), 830–839. https://doi.org/10.1056/NEJMoa1600693
- Figueroa, C., Johnson, C., Verster, A., & Baggaley, R. (2015). Attitudes and acceptability on HIV self-testing among key populations: A literature review. AIDS and Behavior, 1–17. https://doi.org/10.1007/s10461-015-1097-8
- Hatzold, K., Gudukeya, S., Mutseta, M. N., Chilongosi, R., Nalubamba, M., Nkhoma, C., Munkombwe, H., Munjoma, M., Mkandawire, P., Mabhunu, V., Smith, G., Madidi, N., Ahmed, H., Kambeu, T., Stankard, P., Johnson, C. C., & Corbett, E. L. (2019). HIV self-testing: Breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. Journal of the International AIDS Society, 22(Suppl. 1), e25244. https://doi.org/10.1002/jia2.25244
- HIVST.org. (2019). Policy & regulations for HIVST. Retrieved September 8, 2020 from http://www.hivst.org/policy/
- Johnson, C. C., Kennedy, C., Fonner, V., Siegfried, N., Figueroa, C., Dalal, S., Sands, A., & Baggaley, R. (2017). Examining the effects of HIV self-testing compared to standard HIV testing services: A systematic review and meta-analysis. Journal of the International AIDS Society, 20, 1. https://doi.org/10.7448/ias.20.1.21594
- Maman, S., Murray, K. R., Mavedzenge, S. N., Oluoch, L., Sijenje, F., Agot, K., & Thirumurthy, H. (2017). A qualitative study of secondary distribution of HIV self-test kits by female sex workers in Kenya. PLoS One, 12(3), e0174629. https://doi.org/10.1371/journal.pone.0174629
- Matovu, J. K., Buregyeya, E., Arinaitwe, J., & Wanyenze, R. K. (2017). “ … if you bring the kit home, you [can] get time and test together with your partner”: Pregnant women and male partners’ perceptions regarding female partner-delivered HIV self-testing in Uganda – A qualitative study. International Journal of STD & AIDS, 28(13), 1341–1347. https://doi.org/10.1177/0956462417705800
- Matovu, J. K., Kisa, R., Buregyeya, E., Chemusto, H., Mugerwa, S., Musoke, W., Vrana, C. J., Malek, A. M., Korte, J. E., & Wanyenze, R. K. (2018). “If I had not taken it [HIVST kit] home, my husband would not have come to the facility to test for HIV”: HIV self-testing perceptions, delivery strategies, and post-test experiences among pregnant women and their male partners in Central Uganda. Global Health Action, 11(1), 1503784. https://doi.org/10.1080/16549716.2018.1503784
- Musheke, M., Ntalasha, H., Gari, S., Mckenzie, O., Bond, V., Martin-Hilber, A., & Merten, S. (2013). A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health, 13, 220. https://doi.org/10.1186/1471-2458-13-220
- Ortblad, K. F., Kibuuka Musoke, D., Ngabirano, T., Nakidende, A., Magoola, J., Kayiira, P., Taasi, G., Barresi, L., Haberer, J. E., McConnell, M., Oldenburg, C., & Barnighausen, T. (2017). Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial. PLoS Medicine, 14(11), e1002458. https://doi.org/10.1371/journal.pmed.1002458
- Ortblad, K. F., Kibuuka Musoke, D., Ngabirano, T., Nakitende, A., Taasi, G., Barresi, L. G., Bärnighausen, T., & Oldenburg, C. E. (2018). HIV self-test performance among female sex workers in Kampala, Uganda: A cross-sectional study. BMJ Open, 8(11), e022652. https://doi.org/10.1136/bmjopen-2018-022652
- Ortblad, K. F., Musoke, D. K., Chanda, M. M., Ngabirano, T., Velloza, J., Haberer, J. E., McConnell, M., Oldenburg, C. E., & Bärnighausen, T. (2020). Knowledge of HIV status is associated with a decrease in the severity of depressive symptoms among female sex workers in Uganda and Zambia. Journal of Acquired Immune Deficiency Syndromes (1999), 83(1), 37–46. https://doi.org/10.1097/QAI.0000000000002224
- Ortblad, K. F., Musoke, D. K., Ngabirano, T., Nakitende, A., Haberer, J. E., McConnell, M., Salomon, J. A., Bärnighausen, T., & Oldenburg, C. E. (2018). Female sex workers often incorrectly interpret HIV self-test results in Uganda. Journal of Acquired Immune Deficiency Syndromes, 79(1), e42–e45. https://doi.org/10.1097/QAI.0000000000001765
- Ortblad, K. F., Musoke, D. K., Ngabirano, T., Salomon, J. A., Haberer, J. E., McConnell, M., Oldenburg, C. E., & Bärnighausen, T. (2019). Is knowledge of HIV status associated with sexual behaviours? A fixed effects analysis of a female sex worker cohort in urban Uganda. Journal of the International AIDS Society, 22(7), e25336. https://doi.org/10.1002/jia2.25336
- Shannon, K., Strathdee, S. A., Goldenberg, S. M., Duff, P., Mwangi, P., Rusakova, M., Reza-Paul, S., Lau, J., Deering, K., Pickles, M. R., & Boily, M.-C. (2015). Global epidemiology of HIV among female sex workers: Influence of structural determinants. Lancet, 385(9962), 55–71. https://doi.org/10.1016/S0140-6736(14)60931-4
- Turcotte-Tremblay, A.-M., Gali-Gali, I. A., De Allegri, M., & Ridde, V. (2017). The unintended consequences of community verifications for performance-based financing in Burkina Faso. Social Science & Medicine (1982), 191, 226–236. https://doi.org/10.1016/j.socscimed.2017.09.007
- Uganda Ministry of Health. (2020). MARPI – Most at risk populations initiatives. Retrieved September 7, 2020, from http://www.marpi.org
- UNAIDS. (2019). UNAIDS data 2019. https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf
- Wachinger, J., Ortblad, K., Musoke, D. K., Nakitende, A., Oldenburg, C., Bärnighausen, T., & McMahon, S. A. (2020). But I gathered my courage: Participation in an HIV self-testing trial as a pathway to empowerment among Ugandan sex workers. 38th annual conference of the German Society of Tropical Paediatrics and International Child Health.
- WHO. (2019). Consolidated guidelines on HIV testing services for a changing epidemic. file:///C:/Users/katort/Downloads/WHO-CDS-HIV-19.31-eng.pdf.
- WHO. (2020). HIV self-testing. Retrieved September 9, 2020, from http://www.who.int/hiv/topics/self-testing/en/