ABSTRACT
Pre-Exposure Prophylaxis (PrEP) is a potential game-changer for HIV. We used PrEP introduction for Young Women Who Sell Sex (YWSS) in a rural South Africa district to understand community norms and PrEP coverage in YWSS. Between 2017 and 2018, we measured awareness and uptake of PrEP in a representative cohort of 2184 Adolescent Girls and Young Women (AGYW) aged 13–22. We conducted group discussions with young people and community members (19); key informant interviews (9), in-depth interviews with 15–24 year-olds (58) and providers (33). Interviews were analysed using thematic analysis. PrEP awareness increased from 2% to 9%. Among 965 AGYW sexually-active by 2018, 13.4% (95%CI: 11.4%–15.7%) reported transactional sex and 10.6% (95%CI: 8.85–12.7%) sex for money. Of the 194 YWSS, 21 were aware of PrEP, but none had used it. Youth were enthusiastic about PrEP as tool for HIV prevention; whilst older community members were cautious about a technology they had limited experience with but could benefit select groups. Teachers and healthcare providers were concerned that PrEP would lower personal responsibility for sexual health. In conclusion, the narrow and limited introduction of PrEP to YWSS reduced the accessibility and reach. Introducing PrEP as part of sexual healthcare may improve demand and access for YWSS.
Introduction
The HIV epidemic in South Africa (SA) remains an intractable problem (Chimbindi et al., Citation2018; HSRC, Citation2017; UNAIDS, Citation2018). This is, despite efficacious, efficient and safe biomedical tools, including daily oral tenofovir/emtricitabine for Pre-Exposure Prophylaxis (PrEP), use of which can reduce HIV-acquisition risk by >90% (McCormack et al., Citation2016); and antiretroviral therapy (ART), which reduces mortality and eliminates onward HIV transmission to sexual partners (Cohen et al., Citation2012; Rodger et al., Citation2016).
WHO recommended including tenofovir-based PrEP as part of combination prevention for individuals at substantial risk of HIV, e.g., female-sex workers (FSW) and vulnerable populations such as adolescent girls and young women (AGYW), particularly young women who sell sex (YWSS) (Dunkle et al., Citation2004; Stoebenau et al., Citation2016; Wamoyi et al., Citation2016; World Health Organization, Citation2015). The South African National Department of Health subsequently rolled-out oral PrEP to select FSW sites in 2016 and for HIV prevention in AGYW in 2017 (South Africa National Department of Health, Citation2017). However, the potential for biomedical HIV prevention, such as PrEP, to have a substantial impact on the epidemic depends on uptake and adherence by those at substantial risk of HIV acquisition and transmission (Hargreaves et al., Citation2016; Marrazzo et al., Citation2015; Yun et al., Citation2018). This has remained a challenge, especially amongst AGYW, with belief in effectiveness of PrEP, social cohesion, support for use from partner, friends and family as facilitators to uptake and adherence (Amico et al., Citation2017; Marrazzo et al., Citation2015; Van Damme et al., Citation2012).
The current strategy in many southern African settings is to introduce PrEP as an intervention that targets the most vulnerable and powerless populations, e.g., self-identifying FSWs (operationally defined as women who sell sex) often young women who sell sex (YWSS), who lack social support and face stigma from communities and healthcare systems models (South Africa National Department of Health, Citation2017). We have limited evidence of how targeted roll-out of newer biomedical interventions will be received and experienced by wider communities, and specifically how this impacts on the population-wide HIV prevention cascade (Cowan et al., Citation2016; Hargreaves et al., Citation2016; Krakower & Mayer, Citation2016).
We use the opportunity of a PrEP introduction for YWSS (aged 15–24) by the Determined Resilient Empowered AIDS-free Mentored and Safe (DREAMS) partnership (“UNAIDS: DREAMS initiative for adolescent girls and young women in South Africa,”, Citation2015) as part of combination prevention in a rural KwaZulu-Natal setting with high HIV incidence (Vandormael et al., Citation2019) and no prior PrEP availability, to explore the impact on community norms and PrEP coverage in YWSS (Birdthistle et al., Citation2018). We use a mixed methods approach based on a theoretical framework of access (McIntyre et al., Citation2009) to describe PrEP access, awareness and uptake for AGYW, and community norms around PrEP.
Methods
Study site
The Africa Health Research Institute (AHRI) is located in Hlabisa sub-district in uMkhanyakude district, northern KwaZulu-Natal, in an area selected for DREAMS implementation (“UNAIDS: DREAMS initiative for adolescent girls and young women in South Africa,”, Citation2015). The study area is a health and demographic surveillance system site (Herbst et al., Citation2015), predominantly rural, with high levels of unemployment and an HIV incidence rate of >5% per annum among AGYW (Chimbindi et al., Citation2018). There were few targeted HIV prevention interventions for adolescents and youth in this area prior to DREAMS, and no sex-worker programmes until 2016.
Population, data collection and measures
We used data from the mixed-method process evaluation for the implementation of DREAMS in this area (Birdthistle et al., Citation2018). The evaluation collected qualitative data from a range of stakeholders (service users, service providers and community members) during participatory community-mapping and quantitative data from a population-representative cohort of AGYW in 2017 and 2018.
The quantitative aspect of the evaluation consisted of a random sample of 2184 AGYW aged 13–22 years, stratified by age and residential location, to measure the level of access to PrEP, PrEP awareness and uptake at population level in those who are eligible and followed them up in 2018 (Birdthistle et al., Citation2018). We assessed PrEP awareness based on a question asking if the respondent had ever heard of PrEP and uptake based on two questions asking if they have ever been offered or were currently taking PrEP. Transactional sex and sex-work were evaluated using three validated questions:
Transactional sex: In the past 12 months, have you ever had sex with anyone because you needed (or your partner provided) a material item that was important to you, such as clothing, telephone, money for rent, transportation in their car?;
Clients for transactional sex: In the past 12 months how many different people have you become sexually involved with because they provided you or you expected that they would provide you with money?;
Sex-work: Some people have sex with other people for a living; would you consider yourself to be such a person? (Wamoyi et al., Citation2019)
Data were collected electronically using RedCap software (University, Citation2006) and self-completed by the participant on a tablet computer to improve privacy.
The qualitative aspect of the evaluation included several components, this is described in more detail in our work (Zuma et al., Citation2019). First, a participatory community-mapping of four purposively sampled communities (one semi-urban, two rural and one deep-rural) to recruit key informants for interview. These informants included DREAMS implementing partners (n = 33), community-based group discussions (n = 17) and natural group discussions (n = 2). Second, the evaluation also captured structured observation data to understand the context and processes through which PrEP was delivered in uMkhanyakude (n = 2). Third, we conducted in-depth interviews with 10–35 year-olds (n = 58) and stakeholder interviews with local and district municipality, government departments including health and social development (n = 9). All interviews and group discussions were conducted in the local language isiZulu by a team of native Zulu-speakers, five females and four males, who have worked and resided in the study area for at least five years. All interviews were audio-recorded, transcribed verbatim, translated into English. Data were managed using Nvivo version 11 (QSR International Pty Ltd, Citation2018).
Analysis
We use the HIV prevention cascade framework (Hargreaves et al., Citation2016) to monitor PrEP roll-out and broader impact, informed by the “framework of access” developed by McIntyre et al. (McIntyre et al., Citation2009) to guide our analysis and evaluate general healthcare access. We describe population-level awareness and uptake of PrEP among two populations: AGYW and YWSS (AGYW reporting transactional and sex for money). The framework of access provides a lens to understand what the drivers of uptake are and the extent they affect uptake. We define access to PrEP healthcare as follows: availability in terms of awareness or knowledge of PrEP and the way in which it was delivered; acceptability in terms of perceived benefit of PrEP, community attitudes around PrEP and support for optimal use of PrEP and last affordability in terms of costs, including indirect costs of accessing PrEP (Cowan et al., Citation2016; Hargreaves et al., Citation2016; McIntyre et al., Citation2009).
We thematically coded the qualitative data on the community, young people and stakeholders perceptions of PrEP to identify the underlying drivers of uptake and awareness of PrEP, demand for and access to PrEP and the associated challenges (availability); community attitudes and perceived benefits or harms of PrEP, and optimal use of PrEP in terms of who should be prioritised and likely to benefit most from PrEP (acceptability); and last affordability in terms of costs, including indirect costs of accessing PrEP and perceived “costs” to the health system.
Quantitative data were analysed using STATA version 15 (StataCorp, Citation2017) to present the PrEP cascade, i.e., reach, awareness and uptake of PrEP by the target group (YWSS). We described characteristics of AGYW at baseline in 2017 using proportions and 95% confidence intervals (CI), and used chi-square test to test for differences between proportions. By triangulating insights from in-depth community participatory data with quantitative measures of awareness and uptake in those eligible for PrEP, we incorporate insights into the social-structural factors that affected awareness and uptake of PrEP at community-level.
Results
We first describe the population from which these findings are derived both the quantitative and the qualitative interviews, then the roll-out and implementation of PrEP for YWSS in this rural community. We then present the quantitative findings on the uptake of PrEP at a population-level for YWSS and lastly emerging themes on availability, acceptability and affordability of PrEP from our qualitative data.
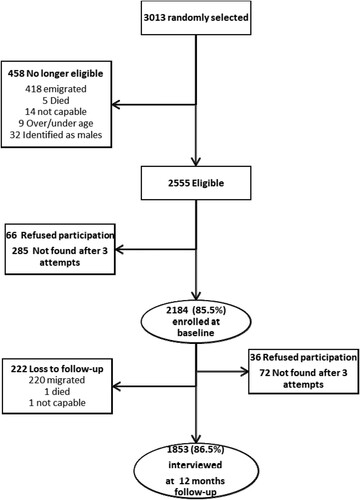
The flow chart below () shows participation in the AGYW cohort at baseline and after 12 months (2017–2018).
Figure 1. Flow chart showing baseline and follow-up in the two survey years 2017–2018 for cohort of AGYW.
A total of about 100 interviews with implementing partners, young people (35 women aged (10–24) and 23 men aged (12–35) and most were in school), and key stakeholders were conducted as well as 19 group discussions including two natural group discussions (total n = 112 participants) were conducted with the community, in 2017.
Implementation of PrEP for young female-sex workers in a rural community
1. Introduction of PrEP
PrEP was introduced in July 2016 to uMkhanyakude district as an intervention targeting YWSS through the DREAMS partnership and by an organisation, experienced in delivering sex-work interventions but new to this rural setting. The implementer conducted a situational analysis of the area to identify “hot-spots” and started enrolling clients for PrEP in August 2016 from these sites; actual PrEP roll-out began in November 2016. For the DREAMS programme, the implementer’s target was to reach approximately 100 HIV uninfected YWSS aged 18–24 years in the two year period that DREAMS was rolled-out.
Challenges of delivering PrEP
Initially, community gatekeepers and owners of bars/taverns, did not want to be associated with the sex-worker programme. Another obstacle was the very tight target age and gender eligibility criteria set by funders (YWSS aged 18–24). FSWs who were underage, or over 24 (the majority), were often eligible for PrEP based on the PrEP screening tool but did not meet the funders’ age criteria. Implementers struggled to recruit eligible YWSS as they did not self-identify as sex-workers, were highly mobile, constantly changing their identity i.e names and contact details and did not see HIV treatment and prevention as a priority.
Facilitators of delivering PrEP
The use of peer workers (former and current sex-workers) for recruitment and follow-up helped start-up and continuity of the programme in the study area because “they understand the language spoken by sex-workers, another sex-worker knows how they greet each other” (Professional nurse) and they could identify with the sex-workers. Mobile services were available and reached the sex-workers where they were and offered them education and services without a long wait time at clinics. One of the HIV counsellors highlighted that this resulted in an increase in treatment of sexually transmitted infections (STI) and suppressed HIV viral loads.
2. Uptake of PrEP at a population level for young women who exchange sex for money and transactional sex
shows the characteristics of the AGYW at baseline. The majority of the AGYW were from the rural (64.1%) areas, most still currently in school (75.3%) and about a fifth (18.5%) having migrated before. AGYW who were not followed-up (n = 331) were older, not in school and had history of migration compared with those who were followed-up. Among the 2184 AGYW in the nested cohort, HIV testing in the last 12 months increased from 45.0% (95%CI:42.9%–47.1%) in 2017 to 53.5% (95%CI:51.3%–55.8%) in 2018 (p < 0.001), while condom use at last sex among the 965 sexually active AGYW did not (53.7%; 95%CI:50.3%–54.0% in 2017 vs. 55.1%; 95%CI:51.6%–58.6% in 2018, p = 0.559).
Table 1. Characteristics of AGYW at baseline in 2017 (N = 2184) and 12-months follow-up (N = 1853).
PrEP awareness increased from 2.0% (95%CI:1.5%–2.7%) in 2017 to 9.0% (95%CI: 7.3%–9.8%) in 2018 in all AGYW, a substantively small but statistically significant increase (p < 0.001). About one in five of sexually active AGYW self-identified themselves as YWSS; 13.4% (95%CI:11.4%–15.7%) reported transactional sex and 10.6% (95%CI:8.8%–12.7%) sex for money.
From 194 YWSS who were PrEP-eligible, n = 166, 85.6% (95%CI:79.8%–89.9%) knew their HIV status and of these, n = 113, 68.1% (95%CI:60.5%–74.8%) were HIV negative. Only n = 12, 10.6% (95%CI:6.08%–17.9%) were aware of PrEP, but none had used PrEP ().
Figure 2. PrEP utilisation cascade among eligible AGYW involved in transactional sex/sex work in 2017–2018 (n = 194).
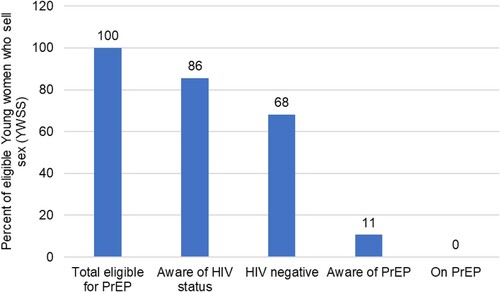
shows the HIV prevention cascade for PrEP-eligible AGYW from 2017 to 2018.
3. Community and young people’s awareness, demand and perceptions of PrEP uptake
Availability: awareness of PrEP
PrEP was available and implemented in this area through a sex-worker peer outreach programme to self-identifying and visible YWSS. Respondents in qualitative interviews were aware of sex-work in the community and many identified FSW hot-spots however, most were not aware of PrEP. Some young people indicated it was their first time to hear about PrEP and could not attach meaning to the term since they did not have an isiZulu word for it. Lack of awareness was heightened by PrEP not being available through public-sector health clinics. Most older community members – including community health champions such as community caregivers were also not aware of PrEP, with some people confusing it with post-exposure prophylaxis.
Acceptability: demand and perceived benefit of PrEP
Whilst generally unaware of PrEP, many respondents could imagine it would benefit young people, often because it could be an alternative to condoms. Condoms were generally seen by young people as unacceptable both for HIV prevention and contraception, as it resulted in “killing your babies” or “eating sweets in a wrapping paper” (group discussion young men). One young person indicated that PrEP would probably be more helpful than condoms because people do not like wearing condoms, but with PrEP “it will be in their system” and hence more likely to be effective as it does not obstruct sex. Older community members liked PrEP because it is taken orally and therefore seen to be easier to use than condoms. Staff at FSW clinics reported that PrEP had only minor side-effects and so FSWs were able to adhere to it, as confirmed by drug-level blood tests. However, teachers and other healthcare providers were more ambivalent about PrEP. While acknowledging PrEP’s effectiveness and usefulness for young people who were “rushing to have sex”, they worried it would lower personal responsibility for sexual health and lead to unprotected sex, promiscuity and increases in already high teenage pregnancy rates.
The perceived benefits of PrEP were strongly gendered. Most young people thought PrEP would be more beneficial to boys or young men than girls or women because men were believed to “love sex more than women” and had multiple partners. Further, PrEP was seen to help keep circumcised men negative for a longer time as they were worried about the 40% residual risk not covered by medical circumcision.
Similarly, an implementing partner from another organisation indicated that PrEP was mainly beneficial for boys because they engaged in unsafe sex when drunk. However, some young people thought girls would have greater access to PrEP because they are more likely to access clinics for other reasons, while boys associate clinics with sick people and so would not uptake PrEP from there.
PrEP was seen as giving hope to people who are in discordant relationships indicating that someone’s HIV status would not need to be a barrier in forming or remaining in sexual relationships:
“those who are in relationships with older people who are infected, they can be able to get treatment beside leaving him because of his HIV status.” (Young person)
Also, young people thought PrEP would benefit women in long-distance relationships with their husbands as “they cannot be certain of their husbands” other relationships while away from home.
Affordability: financial and social cost of taking PrEP
The peer outreach approach used by the organisation delivering PrEP assisted with recruitment as YWSS felt less stigmatised or fearful of being identified. An accompanying mobile unit offered a range of services free of charge, including syndromic screening and treatment of STIs and tuberculosis, HIV testing, ART and PrEP. This approach also meant YWSS incurred little or no transport costs to access PrEP. However, several social barriers were highlighted for uptake of PrEP. One challenge was stigma as a barrier to HIV testing, the entry point for PrEP:
“this disease [HIV] was introduced badly, if you are suffering from it you are sleeping with many people, so that can lead to people not wanting to test and your peers will talk behind your back.” (discussion community caregivers)
Moreover, clinics were seen as stigmatised spaces, places for “gossip” and associated with being HIV-positive, suggesting PrEP delivery to young people through primary health care clinics would be difficult.
Another challenge for PrEP delivery was that some young people were “ashamed of taking pills” and would not use them until “the situation forces” it, i.e., when they get sick. Pill-taking in this setting is associated with being unhealthy, especially in the context of high HIV prevalence. Furthermore, women felt they could not take PrEP for occasional sexual enounters as they were often not in regular partnerships and therefore not having regular sex. Lack of information on PrEP availability, effectiveness and side-effects created ambivalence in some young respondents, “because we don’t have a guarantee of 100% that this thing works.”
Discussion
Introduction of PrEP to YWSS confined to a narrow sex-work focused programme limited the reach and coverage of public-sector PrEP roll-out in this rural South African setting. In this setting where HIV prevalence is high, condoms are undesirable and use remains low, as seen across South Africa (Chimbindi et al., Citation2018; Human Sciences Research Council (HSRC), Citation2018), the introduction of PrEP through a sex-worker programme was feasible. PrEP roll-out was targeted to YWSS and so there was almost no community-based demand creation(Nakasone et al., Citation2020). However, PrEP awareness rose over time because of increase roll-out, and PrEP was seen to be desirable, especially for young men, discordant couples, and women with long distant sex partners. Despite this uptake of PrEP remained low among YWSS. The narrow focus of the PrEP programme, including targeting based on age, gender and risk group, may have contributed to the low uptake. Stigma around HIV testing and PrEP (Golub, Citation2018; Zuma et al., Citation2019) and community norms fearing the permissive effect of PrEP on young people’s sexuality were social costs and potential barriers to PrEP roll-out.
Many of the groups that the community described as potentially wanting PrEP – men and older women in long-distance relationships – are not currently part of the South African PrEP target groups of key populations and women aged 15–24 (South Africa National Department of Health, Citation2017), which could potentially hamper PrEP roll-out (Bekker et al., Citation2015a). Engaging young women at high risk of HIV in clinical PrEP trials in South Africa has been challenging, showing high uptake but poor retention and adherence over time, and therefore failed to show effectiveness (Marrazzo et al., Citation2015; Van Damme et al., Citation2012). In contrast, the Partners demonstration project involving older serodiscordant heterosexual couples proved effective (Baeten et al., Citation2012). Alongside our findings, this suggests that narrow PrEP targeting by demographic or risk group may limit population-level coverage of people at risk for HIV acquisition, and feed into existing stigma. Community-led approaches to delivery that can adapt to the context may overcome some of the challenges of targeted approaches in high HIV-prevalence settings (Cambiano et al., Citation2019; Hatzold et al., Citation2019).
Healthcare providers and key stakeholders acknowledge the effectiveness and importance of PrEP, but worry about young people not taking responsibility of their sexuality (Bekker et al., Citation2015b; Camlin et al., Citation2020). Such attitudes will potentially fuel the internalised and enacted stigma towards PrEP (Bekker et al., Citation2015b; Camlin et al., Citation2020; Golub, Citation2018), much as they have around HIV testing in rural settings (Camlin et al., Citation2020). To minimise such risks, PrEP promotion, particularly amongst gatekeepers such as teachers and healthcare providers should be integrated with a package of adolescent and youth sexual health interventions that include PrEP as part of differentiated HIV prevention alongside contraception (Bekker et al., Citation2015a). Community sensitisation of PrEP as part of sexual well-being maybe key to embedding changes in attitudes and norms amongst these stakeholders.
Conclusion
The targeting of provision to YWSS limited the early effectiveness of a public-sector PrEP programme in this rural setting. Although PrEP awareness increased, uptake was low, even among YWSS. PrEP was widely perceived to be potentially beneficial (acceptable), however the stigma associated with membership of the target group and the lack of availability in primary health clinics reduced accessibility and reach of PrEP amongst young people. Inclusive, community-based PrEP, as part of sexual health provision, and with active engagement of youth and key stakeholders, may help improve demand for and access to PrEP.
Ethics approval and consent to participate
Ethics approval was received from the University of KwaZulu-Natal Biomedical Research Ethics Committee (BFC339/19) and the London School of Hygiene and Tropical Medicine (REF11835). Written informed consent was obtained from all participants prior to data collection.
Authors contributions
NC, MS, NM, JS conceptualised the study, NC,TZ, MS, SN, JD performed the research, MS, IB, SF designed the research study. NM, KB, MS, NC analysed the quantitative data and KB, GH, NMcG, MS critically reviewed it. NC, TZ, MS, SN and IB analysed the qualitative data, and LS and JS critically reviewed it. NC and MS wrote the manuscript. All authors read, critically reviewed, edited and approved the final manuscript.
Acknowledgements
We would like to thank all the participants who contributed data to this study and the data collection teams from AHRI who collected the quantitative and qualitative data.- Miss D Mthethwa, Mr SD Mdluli, Mr KC Mngomezulu, Miss PN Mthethwa, Mr Z Xulu, Mr M Nhlenyama, Ms NL Ntombela, Mr MT Nzuza, Miss Q Shandu, Miss P Khanyile, Mr S Hlongwane, Mrs NC Fakude, Miss TG Dlamini, Miss SQ Ntshangase, Mr S Nsibande, Miss NN Mbatha, Mrs ZB Mathenjwa, Mrs Z Cumbane, Ms K Ngobese, Ms B Mbatha, Miss G Buthelezi, Ms N Buthelezi, and Ms M Myeni.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from corresponding author [MS] upon reasonable request.
Additional information
Funding
References
- Amico, K. R., Wallace, M., Bekker, L.-G., Roux, S., Atujuna, M., Sebastian, E., … Grant, R. M. (2017). Experiences with HPTN 067/ADAPT study-provided open-label PrEP among women in Cape Town: Facilitators and barriers within a mutuality framework. AIDS and Behavior, 21(5), 1361–1375. https://doi.org/https://doi.org/10.1007/s10461-016-1458-y
- Baeten, J. M., Donnell, D., Ndase, P., Mugo, N. R., Campbell, J. D., Wangisi, J., … Partners Pr, E. P. S. T. (2012). Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England Journal of Medicine, 367(5), 399–410. https://doi.org/https://doi.org/10.1056/NEJMoa1108524
- Bekker, L.-G., Gill, K., & Wallace, M. (2015a). Pre-exposure prophylaxis for South African adolescents: What evidence? (Vol. 105).
- Bekker, L.-G., Gill, K., & Wallace, M. (2015b). Pre-exposure prophylaxis for South African adolescents: What evidence? South African Medical Journal, 105(11), 907–911. https://doi.org/https://doi.org/10.7196/SAMJ.2015.v105i11.10222
- Birdthistle, I., Schaffnit, S. B., Kwaro, D., Shahmanesh, M., Ziraba, A., Kabiru, C. W., … Floyd, S. (2018). Evaluating the impact of the DREAMS partnership to reduce HIV incidence among adolescent girls and young women in four settings: A study protocol. BMC Public Health, 18(1), 912. https://doi.org/https://doi.org/10.1186/s12889-018-5789-7
- Cambiano, V., Johnson, C. C., Hatzold, K., Terris-Prestholt, F., Maheswaran, H., Thirumurthy, H., … Phillips, A. (2019). The impact and cost-effectiveness of community-based HIV self-testing in sub-Saharan Africa: A health economic and modelling analysis. Journal of the International AIDS Society, 22(Suppl 1), e25243. https://doi.org/https://doi.org/10.1002/jia2.25243
- Camlin, C. S., Koss, C. A., Getahun, M., Owino, L., Itiakorit, H., Akatukwasa, C., & Havlir, D. V. (2020). Understanding demand for PrEP and early experiences of PrEP Use Among young adults in rural Kenya and Uganda: A qualitative study. AIDS and Behavior, 24, 2149–2169. https://doi.org/https://doi.org/10.1007/s10461-020-02780-x
- Chimbindi, N., Mthiyane, N., Birdthistle, I., Floyd, S., McGrath, N., Pillay, D., & Shahmanesh, M. (2018). Persistently high incidence of HIV and poor service uptake in adolescent girls and young women in rural KwaZulu-Natal, South Africa prior to DREAMS. PLoS One, 13(10), e0203193. https://doi.org/https://doi.org/10.1371/journal.pone.0203193
- Cohen, M. S., McCauley, M., & Gamble, T. R. (2012). HIV treatment as prevention and HPTN 052. Current Opinion in HIV and AIDS, 7(2), 99–105. https://doi.org/https://doi.org/10.1097/COH.0b013e32834f5cf2
- Cowan, F. M., Delany-Moretlwe, S., Sanders, E. J., Mugo, N. R., Guedou, F. A., Alary, M., & Bekker, L.-G. (2016). PrEP implementation research in Africa: What is new? Journal of the International AIDS Society, 19(Suppl 6):21101. https://doi.org/https://doi.org/10.7448/IAS.19.7.21101
- Dunkle, K. L., Jewkes, R. K., Brown, H. C., Gray, G. E., McIntryre, J. A., & Harlow, S. D. (2004). Transactional sex among women in soweto, South Africa: Prevalence, risk factors and association with HIV infection. Social Science & Medicine, 59(8), 1581–1592. https://doi.org/https://doi.org/10.1016/j.socscimed.2004.02.003
- Golub, S. A. (2018). PrEP stigma: Implicit and explicit drivers of disparity. Current HIV/AIDS Reports, 15(2), 190–197. https://doi.org/https://doi.org/10.1007/s11904-018-0385-0
- Hargreaves, J. R., Delany-Moretlwe, S., Hallett, T. B., Johnson, S., Kapiga, S., Bhattacharjee, P., … Garnett, G. P. (2016). The HIV prevention cascade: Integrating theories of epidemiological, behavioural, and social science into programme design and monitoring. The Lancet HIV, 3(7), e318–e322. https://doi.org/https://doi.org/10.1016/S2352-3018(16)30063-7
- Hatzold, K., Gudukeya, S., Mutseta, M. N., Chilongosi, R., Nalubamba, M., Nkhoma, C., … Corbett, E. L. (2019). HIV self-testing: Breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. Journal of the International AIDS Society, 22(Suppl 1), e25244. https://doi.org/https://doi.org/10.1002/jia2.25244
- Herbst, K., Law, M., Geldsetzer, P., Tanser, F., Harling, G., & Barnighausen, T. (2015). Innovations in health and demographic surveillance systems to establish the causal impacts of HIV policies. Current Opinion in HIV and AIDS, 10(6), 483–494. https://doi.org/https://doi.org/10.1097/COH.0000000000000203. PMID: 26371462.
- HSRC. (2017). The fifth South African National HIV prevalence, incidence, behaviour and communication survey. http://www.hsrc.ac.za/uploads/pageContent/9234/SABSSMV_Impact_Assessment_Summary_ZA_ADS_cleared_PDFA4.pdf
- Human Sciences Research Council (HSRC). (2018). The Fifth South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017: HIV Impact Assessment Summary Report. Cape Town.
- Krakower, D. S., & Mayer, K. H. (2016). The role of healthcare providers in the roll out of preexposure prophylaxis. Curr Opin HIV AIDS, 11(1), 418. https://doi.org/https://doi.org/10.1097/COH.0000000000000206
- Marrazzo, J. M., Ramjee, G., Richardson, B. A., Gomez, K., Mgodi, N., Nair, G., & for the VOICE Study Team. (2015). Tenofovir-based Preexposure Prophylaxis for HIV Infection among African women. New England Journal of Medicine, 372(6), 509–518. https://doi.org/https://doi.org/10.1056/NEJMoa1402269
- McCormack, S., Dunn, D. T., Desai, M., Dolling, D. I., Gafos, M., Gilson, R., … Gill, O. N. (2016). Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet, 387(10013), 53–60. https://doi.org/https://doi.org/10.1016/S0140-6736(15)00056-2
- McIntyre, D., Thiede, M., & Birch, S. (2009). Access as a policy-relevant concept in low- and middleincome countries. Health Economics, Policy and Law, 4(2), 179–193. https://doi.org/https://doi.org/10.1017/S1744133109004836
- Nakasone, S. E., Chimbindi, N., Mthiyane, N., Nkosi, B., Zuma, T., Baisley, K., … Shahmanesh, M. (2020). “They have this not care - don’t care attitude:” A mixed methods study evaluating community readiness for oral PrEP in adolescent girls and young women in a rural area of South Africa. AIDS Research and Therapy, 17(1), 55. https://doi.org/https://doi.org/10.1186/s12981-020-00310-2
- QSR International Pty Ltd. (2018). NVIVO version 11. https://www.qsrinternational.com/nvivo/contact-us
- Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., van Lunzen, J., … Group, f. t. P. S. (2016). Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy HIV transmission in serodifferent couples using suppressive ARTHIV transmission in serodifferent couples using suppressive ART. JAMA, 316(2), 171–181. https://doi.org/https://doi.org/10.1001/jama.2016.5148
- South Africa National Department of Health. (2017). PrEP implementation pack: South Africa 2016–2017. https://www.prepwatch.org/wp-content/uploads/2017/07/SA_ImplementationPack.pdf
- StataCorp. (2017). Stata statistical software: Release 15. StataCorp LLC.
- Stoebenau, K., Heise, L., Wamoyi, J., & Bobrova, N. (2016). Revisiting the understanding of “transactional sex” in sub-Saharan Africa: A review and synthesis of the literature. Social Science & Medicine, 168, 186–197. https://doi.org/https://doi.org/10.1016/j.socscimed.2016.09.023
- UNAIDS. (2018). UNAIDS Data 2018. http://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf
- UNAIDS: DREAMS initiative for adolescent girls and young women in South Africa. (2015.
- University, V. (2006). REDCap (Research Electronic Data Capture). 1207 17th Avenue South, Suite 105, Nashville, Tennessee 37212, https://projectredcap.org/about/
- Van Damme, L., Corneli, A., Ahmed, K., Agot, K., Lombaard, J., Kapiga, S., … Taylor, D. (2012). Preexposure prophylaxis for HIV infection among African women. New England Journal of Medicine, 367(5), 411–422. https://doi.org/https://doi.org/10.1056/NEJMoa1202614
- Vandormael, A., Akullian, A., Siedner, M., de Oliveira, T., Bärnighausen, T., & Tanser, F. (2019). Declines in HIV incidence among men and women in a South African population-based cohort. Nature Communications, 10(1), 5482. https://doi.org/https://doi.org/10.1038/s41467-019-13473-y
- Wamoyi, J., Ranganathan, M., Kyegombe, N., & Stoebenau, K. (2019). Improving the measurement of transactional sex in sub-Saharan Africa: A critical review. JAIDS Journal of Acquired Immune Deficiency Syndromes, 80(4), 367–374. https://doi.org/https://doi.org/10.1097/QAI.0000000000001928
- Wamoyi, J., Stobeanau, K., Bobrova, N., Abramsky, T., & Watts, C. (2016). Transactional sex and risk for HIV infection in sub-Saharan Africa: A systematic review and meta-analysis. Journal of the International AIDS Society, 19(1), 20992. https://doi.org/https://doi.org/10.7448/IAS.19.1.20992
- World Health Organization. (2015). Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV.
- Yun, K., Xu, J. J., Zhang, J., Li, J. M., Hu, Q. H., Chu, Z. X., … Wang, N. (2018). Female and younger subjects have lower adherence in PrEP trials: A meta-analysis with implications for the uptake of PrEP service to prevent HIV. Sexually Transmitted Infections, 94(3), 163–168. https://doi.org/https://doi.org/10.1136/sextrans-2017-053217
- Zuma, T., Seeley, J., Sibiya, L. O., Chimbindi, N., Birdthistle, I., Sherr, L., & Shahmanesh, M. (2019). The changing landscape of diverse HIV treatment and prevention interventions: Experiences and perceptions of adolescents and young adults in rural KwaZulu-Natal, South Africa. Frontiers in Public Health, 7(336), https://doi.org/https://doi.org/10.3389/fpubh.2019.00336
