ABSTRACT
The risk of poor antiretroviral therapy (ART) adherence among adolescents is a challenge to controlling HIV. This study aims to provide guidance for geographically focussed public health interventions to improve adherence. Through clinic records, it investigates adolescents’ non-adherence risk and clinic-level differences in regions of Nigeria which were part of PEPFAR’s geographical pivot. Records (n = 26,365) were selected using systematic random sampling from all PEPFAR-supported facilities (n = 175) in targeted Local Government Areas across three regions in Nigeria. Adolescents’ risk of non-adherence was estimated using region-specific random-effects models accounting for clinic-level variation. These were adjusted for sex, whether a patient had to travel to a different region, clinic location (urban/rural), clinic type (primary, secondary, tertiary). Despite regional variations, adolescents were at higher risk of non-adherence compared to adults. A similar, but weaker, association was found for children. Patients attending tertiary facilities for ART in the South-South region exhibited very high risk of non-adherence. Adolescents and children are at an increased risk of poor ART adherence in rural regions of Nigeria. Regional differences and facility type are critical factors. Future public health programmes focused on the risk of poor adherence targeting “high-prevalence areas” should be sensitive to contextual differences and age-appropriate care.
Background
Poor antiretroviral therapy (ART) adherence among adolescents has increasingly been recognized as a pressing public health challenge, particularly in sub-Saharan Africa 6/23/20 9:04:00 PM. Nigeria has the world’s third largest burden of disease, with an estimated 1.6 million persons living with HIV and AIDS (PLHIV) in 2019 (UNAIDS, Citation2020b), an estimated 150,000 children (0–14) living with HIV and AIDS (UNAIDS, Citation2020b), and a consistently high 0.5% HIV prevalence among 15–24-year-olds between 2015 and 2019 (UNAIDS, Citation2020a). Effective management of the disease, particularly in this age group, requires the quantification and understanding of patient loss along the continuum of care (Kranzer et al., Citation2012). Adherence to medication is essential for patient health (Beck & Walensky, Citation2009), and non-adherence leads to viral resistance (Sethi et al., Citation2003), treatment failure, and economic strain among individuals (Rosen et al., Citation2014) and across health systems.
Existing research highlights considerable challenges with retention in care and adherence and a recent systematic review found an average one-year retention rate below 75% across four nationally representative studies in Nigeria (M. P. Fox & Rosen, Citation2015). Although just below the continent-wide average (76%) estimated by the review, only four of the 20 included African countries had lower retention rates. More recent studies from Nigeria note a high rate of loss to follow-up (37%) in the first 12 months before ART initiation (Ahonkhai et al., Citation2015), and generally, low retention rates once enrolled in ART (e.g., 81.2% at 12 months) (Bailey et al., Citation2017, Balogun et al., Citation2019). For children (age <15) a recent study found >50% attrition from a dedicated ART programe in Nigeria (Dayyab et al., Citation2021).
Low rates of retention adherence are particularly problematic among young people living with HIV, leading to poor health outcomes (Enane et al., Citation2018). Evidence on adolescents (aged 10–19) and youths (aged 15–24) highlight considerable unplanned care interruptions of >90 days, particularly in the first year after ART initiation (Ahonkhai et al., Citation2015).
Authors of several recent reviews point to the need for large, high-quality studies centered on adolescents (Bailey et al., Citation2017; Enane et al., Citation2018; Fox & Rosen, Citation2015). Crucially, the 2016 Nigerian National HIV Strategy for Adolescents and Young People 2016–2020 argues that due to the lack of evidence around adolescents and young people (AYP), the “HIV response has not been comprehensive for AYP” (National Agency for the Control of AIDS, Citation2016, p. 14). Moreover, in 2016 the UNAIDS “ALL IN – Strategic framework to end the AIDS epidemic among adolescents” (UNAIDS / UNICEF, Citation2016) posed as key research and programming questions the need to identify those adolescents at greatest risk.
In the Nigerian context, regular clinic visits (Ugwu & Eneh, Citation2013), short travel times (Charurat et al., Citation2010), sex (Agaba et al., Citation2018; Odafe et al., Citation2012), and type of clinic (small, primary care) (Odafa et al. Citation2012) were strong predictors of ART adherence among adults. An emergent body of qualitative research from Nigeria highlights stigma, clinic staff attitudes and communication, as well as long waiting times and stockouts as factors leading to non-adherence (Dibb & Ohanyido, Citation2018; Okonkwoh, Citation2011).
However, little evidence exists on adolescent-specific risks of ART non-adherence, including travel-related, clinic-level, and geographical factors. Geographical factors are of particular importance given the stark regional (National Agency for the Control of AIDS, Citation2017), between-state (National Agency for the Control of AIDS, Citation2014), and urban–rural differences in HIV prevalence found in Nigeria.
Geographical differences in HIV prevalence are central to the 2016 PEPFAR (USAID and CDC) geographical pivot towards a geographical focus on public health intervention. The pivot targets treatment on geographical areas and populations with the highest HIV prevalence in Nigeria (PEPFAR, Citation2018). As a result, 32 Local Government Areas (LGAs) across the North-Central, South-South, and South-West regions with the highest HIV prevalence became the focal point of CDC/USAID support. However, no evidence exists concerning the different levels of adherence risk for adolescents in these regions; consequently, little is known about the need for regionally adapted ART public health provisions.
This study aims to:
estimate the risk for ART non-adherence amongst adolescents supported by clinics of the PEPFAR geographical pivot in Nigeria;
assess the relationship between clinic-level factors and risk of ART non-adherence and;
test associations of age, sex, and geographical location with the risk of ART non-adherence.
Each aim has programming implications: Aim 1 explores the need for differential and age-appropriate treatment provision. Aim 2 examines the context of the PEPFAR regional pivot and its geographical focus, with the potential to highlight regional-specific approaches. Finally, Aim 3 addresses a research and policy gap highlighted in the 2016 Nigerian National Strategic Plan, concerning evidence for girls and young women (National Agency for the Control of AIDS, Citation2016).
Methods
This study is designed as cross-sectional, multi-level analysis of a sample of clinic records. It aims to represent all facilities chosen due to the PEPFAR geographical pivot (note limitations to representativeness below). The key outcome is a proxy measure of non-adherence based on the last pick-up of ARTs. Where clinic records indicate that the last pick-up occurred more than 60 days ago, non-adherence is deemed to be at risk of non-adhence, as pills were provided for a maximum of 2 months at the time of the study.
Clinics as sampling units
Essential to this design is the “standard of care” provided. Structurally, three levels of care provision are present in facilities of the PEPFAR geographical pivot. Primary-level facilities offer HIV counseling and testing, referral to secondary-level facilities for ART initiation, nutritional support, and prevention and treatment of malaria and opportunistic infections. In addition to the services rendered at primary-level facilities, both secondary- and tertiary-level facilities initiate clients on ART; provide routine ART refill; and offer adherence counseling, basic laboratory investigations, CD4+ count estimation, as well as prevention and management of opportunistic infections. More advanced services such as viral load estimation and liver function tests are offered only at tertiary-level facilities.
It is these facilities that are both a key factor in adherence as well as being the first stage of the sampling of the study’s data with patient records being the primary sampling unit.
Sampling and data
The data were collected for the USAID-financed “Health Facility Catchment Area Mapping” study conducted by the Coordinating Comprehensive Care for Children project (4Children)Footnote1 led by Catholic Relief Services (CRS) in Nigeria during 2016. The sampling frame was intended to cover all 32 PEPFAR scale-up LGAs and all 183 comprehensive health facilities within them. A full list of the LGAs is available as part of the appendix.
Eligibility critieria
Within each clinic, records for all adults and children recorded as “currently on ART” were eligible for inclusion, including pregnant women living with HIV initiated on ART for the prevention of mother-to-child transmission of HIV (PMTCT). Records were included if complete information was available for date of birth, sex, HIV treatment information and the patient’s LGA of residence.
Sampling of record within facilities
Samples were drawn from these records, with sample sizes based on the reported numbers for each of the cohorts (age <15, age ≥15, and PMTCT) per clinic in September 2015.Footnote2
Combination of patient- and facility-level data
Patient record data were merged with facility data, facility level, contact information, facility location (urban/rural), geocode, and LGA of facility. The identifier for merging was the facility name recorded with the data collected on patient records. However, information on individual incomplete records or number of incomplete records at the facility level was not collected. Some coding errors were addressed (negative days since the last ART treatment (n = 111) and implausibly large number of days (>10,000, n = 80)).Footnote3
Datacollector training and technology
Patient record data were collected through an Environmental Systems Research Institute (ESRI)-developed Survey123 tool for ArcGIS on Android devices, which was piloted prior to use and adapted in response to enumerators’ feedback. Data collectors were jointly trained by CRS and ESRI and visited once during the exercise. Further details on enumerator training and stakeholder involvement have been previously described (USAID/4Children, Citation2017). Implementation issues of this design are discussed in the limitations section.
Measures
Risk of non-adherence was defined by proxy. Namely, having had the last ART treatment provided (“date of last drug pick-up”) in >60 days (two months) and not being lost to follow-up, transferred to a different facility, or deceased.Age was categorized as child (0–9 years), adolescent (10–19 years), and adult (>19 years).
Distance to the clinic was measured by a binary proxy indicator “traveling to a different LGA”, derived from comparing patients’ LGA of residence with the LGA of their health facility.
Health care facilities are coded according to their three levels: primary, secondary, and tertiary. Primary-level facilities are usually “community health facilities” funded by the local government authorities. Secondary-level facilities are hospitals funded by the state governments that are occasionally staffed by specialist medical practitioners and act as referral sites for primary-level facilities. Tertiary facilities are mostly teaching institutions providing specialist care.
Statistical analyses
Associations were estimated using logit models with random effects for each health care facility. Given the sampling structure, the models were estimated separately for each region. Two regression models are presented: a base model (Model 1), including only the focal variables of interest (age groups), and a full model (Model2) with the key clinic characteristics, and demographic controls. Results are shown as odds ratios and predicted probabilities. Robustness checks were conducted using additional predictors.
All analyses were undertaken in R (R.Core Team, Citation2021, v.4.0.5), using the following packages: lme4 (Bates et al., Citation2015, v.1.1-27), effects (J. Fox & Hong, Citation2009, v.4.2), sjPlot (Luedecke, Citation2017, v.2.8.9), ggplot2 (Wickham, Citation2009, v.3.3.5), and maptools (Bivand & Lewin-Koh, Citation2017, v.1.1-1).
Replication syntax and data are available at https://doi.org//10.17605/OSF.IO/U56R7.
Ethics
Ethical approval, for data collection and processing, was obtained from the National Health Research Ethics Committee of Nigeria: NHREC/01/01/2007 prior to data collection on 16 June 2016. Data were collected without names or unique identifiers, and stored securely.
Results
Geographical context
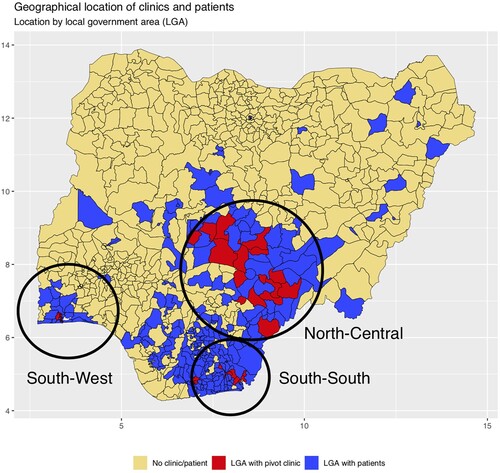
shows the LGAs in which PEPFAR’s geographical pivot clinics are located (red) and the additional LGAs of residence for patients who travel to the PEPFAR clinics (blue).Footnote4 visually indicates that attending a clinic in a different LGA implies significant geographical distance from the place of residence. Patients are drawn from areas considerably beyond the LGAs targeted by the program, and approximately 28% of patients attend a clinic in an LGA different than their LGA of residence. (a detailed list of the states and LGAs can be found in the appendix).
Sample
The study sample () does not include patients who were identified as transferred, passed away, or lost to follow-up, or those for whom case records were incomplete. Death (≤1%) and transferral (≤1%) occurred only rarely, while a large proportion of the sampled records (15–20%) could not be used due to recorded loss to follow-up or being classed as “not on ART”. This occurred despite sampling records being classified as “currently on ART”.
Table 1. Sample flow.
Regional, demographic and clinic-level characteristics
The following analyses are based on a sample of patient records from three regions: North-Central (N–C), South-South (S–S), and South-West (S–W). These regions differ in levels of absolute poverty (N–C 68%, S–S 64%, S–W 59%) their Human Development Index (S–S: HDI = 0.56; S–W = 0.51, N–C = 0.48) (Ibrahim & Ibrahim, Citation2014), and degree of urbanization (S–W: high, S–S and N–C: low).
North-Central and South-South include several districts and hold 67% and 20% of all patients in the study, respectively. Patient demographics across the regions are roughly similar (). Adolescents constitute only 3–8% of all patients in each region, with the South-West/Lagos subsample having the highest proportion of adolescents.
Table 2. Patient numbers, regional and demographic distribution.
Considerable differences exist in facility levels between North-Central and the others, with 19% of patients attending a primary-level facility, compared to 9% in South-South and South-West. Only 13% of patients in North-Central attend a tertiary clinic. As described below, this bears a strong relation to the context of risk of ART non-adherence.
Risk of ART non-adherence (last clinic visit >2 months ago)
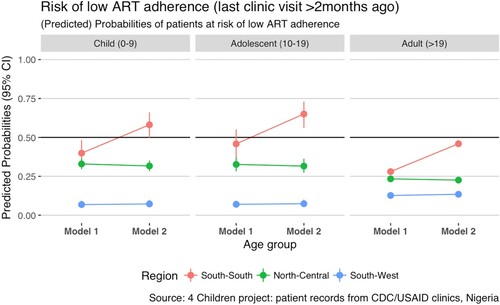
Across the three regions, we observe high incidences of being at risk of non-adherence (N–C: n = 6073 (35.8%), S–S: 3111 (54.6%), S–W: n = 905 (28.3%)). provides the estimated risk of ART non-adherence by region. Model 1 shows that adolescents have considerably higher odds of being at risk of ART non-adherence than adults in both South-South (OR 1.59, 95%CI: 1.50–3.15) and North-Central (OR 2.18, 95%CI: 1.28–1.98). By contrast, in South-West, adolescents and children have substantially lower odds of being at risk of non-adherence than adults (adolescents 0.52, 95%CI: 0.31–0.88). Children in South-South and North-Central have higher odds of being at risk of ART non-adherence than adults (S–S: OR 1.71, 95%CI: 1.21–2.40; N–C: 1.61, 95%CI: 1.36–1.92), whereas in South-West the reverse holds (OR: 0.52, 95%CI: 0.31–0.83).
Table 3. Risk of ART non-adherence (multilevel logit model with random intercepts).
Demographic risk factors for ART non-adherence
We also inspect the risk of non-adherence with respect to attending a clinic in a different LGA. There is a large amount of within-clinic correlation between patients across regions (ICC 0.184–0.423), suggesting considerable clinic-level variation. Model 2 accounts for clinic-level variation and demographic factors, including attendance at a clinic in an LGA different to the patient’s LGA of residence, further differentiating between patients traveling from an LGA of residence with and without a clinic.
Strikingly, the initially observed age relationship with risk of ART non-adherence holds irrespective of these controls, with almost no differences in coefficient sizes. In South-South, male patients were more likely to be at risk of non-adherence (OR 1.27, 95%CI: 1.07–1.49).
Clinic-level risks of ART non-adherence
In South-South, attending a more centralized facility is a risk factor for non-adherence, whether at a secondary-level (OR 3.90, 95%CI: 1.33–11.47) or tertiary-level facility (OR 41.39, 95%CI: 8.86–193.38). Facility level demonstrates the greatest difference in odds among all risk factors. Attending a facility in an urban setting in the largely rural South-South lowers the risk of ART non-adherence (OR 0.21, 95%CI: 0.07–0.64). By contrast, the more urban South-West show no difference in risk by facility level or urban/rural location.
These findings point to clinic-level characteristics having a strong association with the risk of ART non-adherence. Notably, the distance to clinic had no association with the risk of non-adherence.
Regional variation
The findings across both models in suggest very strong regional variations in the demographic and contextual factors for risk of ART non-adherence. South-South and North-Central are more similar regarding the age association; however, the sex and clinic-level association in the former distinguish these regions, too.
presents the predicted probabilitiesFootnote5 of adherence risk for each age group and region. South-West (blue) consistently demonstrates the lowest risk, and South-South (red) the highest, which indicates the regional variation in risk of non-adherence. Importantly, overall probabilities for non-adherence in South-West and North-Central are low, while those for South-South point to the potential for an increased, systematic risk of non-adherence.
As depicted, adults have, on average, a lower probability of risk of ART non-adherence in South-South and North-Central. In South-South, the overall risk across all age groups increases when considering clinic-level and sex differences (Model 2). In this is corroborated by the difference in model-fit.
The overall conclusions are robust against controlling for time on ART and receiving PMTCT treatment (not shown).
Discussion
This study provides robust evidence of a relatively higher risk of ART non-adherence among adolescents in three very different regions of Nigeria characterized by a high prevalence of HIV and AIDS. The findings show that this challenge persists across different levels of clinics (primary, secondary, tertiary) and is independent of sex differences. The albeit coarse indicator of distance to the clinic showed no association. Therefore, the overlap of the age groups’ risk for non-adherence and clinic characteristics appears to be the key focus. This adds to the growing evidence base on the need for “adolescent-friendly health services” and underscores the need to find effective adolescent-focused interventions (Alcon et al., Citation2020; Casale et al., Citation2019; Kim et al., Citation2014; MacPherson et al., Citation2015; Mavegam et al., Citation2017).
Unexpectedly, given the focus of the study, we also observed elevated risks of non-adherence among children, though to a lesser extent than among adolescents. This potentially points to a more general need for age-appropriate and targeted ART provision to increase adherence.
The findings further highlight the considerable differences in risk of ART non-adherence between patients in urban and rural contexts, and between the three regions investigated.Footnote6 Reviews on interventions focused on adolescents increasingly point to more context-sensitive interventions, and the general paucity of these interventions has been cited as a reason for the lack of broadly effective interventions (Casale et al., Citation2019).
While regional and contextual variations are to be expected, it is notable that clinic-level differences and the increased risk of ART non-adherence among adolescents are smaller than the regional differences observed in this study. The regional differences observed could be interpreted with findings from the 2013 Demographic and Health Survey (National Population Commission, Citation2014). These show that problems with accessing clinics (among women) are more prevalent in North-West and South-South than in South-West. Key observed differences in the number of problems mentioned are “getting money for treatment”, the “distance to health facility”, and the “attitude of health workers” (National Population Commission, Citation2014, p.154).
Our findings speak to the growing literature on benefits of health care decentralization that shifts HIV-related services to primary-level facilities (Cobos Muñoz et al., Citation2017). The very large differences in risk of ART non-adherence by facility level further suggest the effectiveness of a more targeted approach to decentralization (Okonkwo et al., Citation2014).
Finally, a focus on clinics, decentralization, and increased awareness of regional differences points to the importance of system-level interventions addressing issues at clinic and regional management for which promising evidence exists (Eluwa et al., Citation2015).
The 2016 PEPFAR guidance highlights HIV prevalence as central for targeting and interventions. According to our study a crucial aspect of making a geographically targetted strategy successful lies in better understanding regional patterns of clinic access, retention and adherence, and their predictors.
Limitations
This study investigates the risk of low ART adherence among adolescents in Nigeria. Yet adherence was measured indirectly via clinic visits, which is problematic since, pills could be picked up by caregivers, and pick-ups could go unrecorded. However, regular clinic visits have been established as an effective proxy for treatment adherence in Nigeria (Ugwu & Eneh, Citation2013). Moreover, the measure chosen is conservative, using a two-month cutoff, and robust, accounting for patient death, transfer, and loss-to-follow-up.
We found no evidence of a relationship between the risk of ART non-adherence and traveling to a clinic in a different LGA than a patient’s LGA of residence. The measurement of “travel” does not measure nor approximate distance. Thus clinics might be close to LGA boundaries and potentially closer than a clinic within a patient’s LGA of residence.
The sample drawn is not representative of Nigeria or all types of clinics. Rather it represents three regions selected for their inclusion in the regional pivot and all participating CDC/USAID-run clinics. LGAs and facilities were sampled due to PEPFAR’s regional pivot (PEPFAR, Citation2018). However, one LGA (Eleme LGA in Rivers State) and thus six facilities (of 182) were not included. Furthermore, only records of patients “currently on ART” were eligible; yet the sample drew a number of records (see above) of patients lost to follow-up or dead. Finally, only complete records were eligible and no information on individual incomplete records or number of incomplete records at the facility level were collected. Consequently, bias from missing observations is also likely. For these reasons, the sample is not the result of a random sampling procedure, and inferences should be made cautiously.
Yet, given the number of records (n = 26,365) and clinics (n = 176) sampled, covering almost all PEPFAR regional pivot clinics, this study is, to the authors’ knowledge, the first to robustly account for clinic context in a sample representative of a clearly defined patient population.
Finally, existing research particularly among adolescents – shows the significance of stigma, clinic staff attitudes, and clinic characteristics such as waiting times (Dibb & Ohanyido, Citation2018; Okonkwoh, Citation2011). Although this study finds a clear effect of facility level and the importance of clinic characteristics (cf ICCs), it does not analyze these specific risk factors for non-adherence.
Directions for future research
Future research should examine the causes of increased risk of ART non-adherence among adolescents and, given these findings, also children. Beyond existing research, greater attention should be paid to specific scontextual factors such as reasons for the observed differences between regions, between urban and rural clinics, and the different levels of facilities. This would directly support the development and optimizatoin of adolescent-friendly services, and may help adapt existing interventions of mixed effectiveness (Casale et al., Citation2019; Mavegam et al., Citation2017).
Conclusion
Implications for practitioners
In 2016 the UNAIDS “ALL IN – Strategic framework to end the AIDS epidemic among adolescents” posed as key research and programming questions the need to identify those adolescents at greatest risk for non-adherence (UNAIDS / UNICEF, Citation2016). This study identified an elevated risk of non-adherence among adolescents in clinics specifically supported by the 2016 PEPFAR pivot, which targeted funding and support for clinics in high-prevalence regions (UNAIDS, Citation2014). In this context, it found type of clinic (tertiary) and regional variations as crucial risk factors in the context of non-adherence.
Future programming should take into account regional differences and acknowledge that the risk of non-adherence is elevated in tertiary-level clinics. Finally, programming to address the elevated risk of non-adherence among children and adolescents should increase the provision of adolescent-friendly (and pediatric) services, for which an emergent body of evidence exists (Mbatia et al., Citation2018).
Funding details
This paper has been made possible by the generous support of the American people through the United States Agency for International Development (USAID) under Cooperative Agreement [AID-OAA-A-14-00061].
Acknowledgements
This paper has been made possible by the generous support of the American people through the United States Agency for International Development (USAID) under Cooperative Agreement AID-OAA-A-14-00061. The contents are the responsibility of the authors and the Coordinating Comprehensive Care for Children (4Children) project and do not necessarily reflect the views of USAID or the United States Government.
The authors are grateful for insightful guidance from Tapfuma Murove, Kelly Bunkers, and Adele Clark (CRS) as well as Franziska Meinck (University of Edinburgh).
Disclosure statement
The corresponding author has been a paid consultant for Catholic Relief Services (CRS) and has received honoraria for teaching statistical programming in R as well as being associate editor for the Journal of Child and Adolescent Mental Health.
Data availability statement
The annoymised data and replication syntax that support the findings of this study are openly available at https://doi.org//10.17605/OSF.IO/U56R7.
Notes
1 4Children was a five-year, USAID-funded project improving the health and well-being of vulnerable children affected by HIV and AIDS and other adversities. 4Children draws on global evidence that illustrates that HIV and other hardships are best prevented and addressed when people have access to both high-quality health and social welfare services. More information can be found at https://www.crs.org/our-work-overseas/program-areas/health/4children.
2 Records were sampled in (random) intervals of five, and the samplesizes were calculated for a 5% margin of error.
3 Negative values were set to 1 and decimal places for exceedingly large values were adjusted by 10.
4 Source: Shapefiles: OCHA ROWCA. Date of dataset: September 26, 2017. Available at: https://data.humdata.org/dataset/west-and-central-africa-administrative-boundaries-levels. Accessed January 17, 2018.
5 For the models presented for detailed probabilities, see appendix.
6 Given the lower degree of urbanization and thus a stronger contrast between urban and rural contexts in access to care, it is to be expected and indeed observed that attending a clinic in an urban setting in South-South reduces the risk of ART non-adherence. By contrast, the more urban South-West shows no such systematic differences between urban and rural contexts or by clinic level.
References
- Agaba, P. A., Genberg, B. L., & Sagay, A. S. (2018). Retention in differentiated care: Multiple measures analysis for a decentralized HIV care and treatment program in North Central Nigeria. Journal of AIDS & Clinical Research, 9(2), https://doi.org/10.4172/2155-6113.1000756
- Ahonkhai, A. A., Banigbe, B., & Adeola, J. (2015). High rates of unplanned interruptions from HIV care early after antiretroviral therapy initiation in Nigeria. BMC Infectious Diseases, 15(1), 397. https://doi.org/10.1186/s12879-015-1137-z
- Alcon, S., Ahmed, B., Sloane, D., Lim, Y. S., & Cervia, J. S. (2020). Interventions to improve medication adherence in adolescents with HIV: A systematic review and meta-analysis. Journal of Investigative Medicine, 68(7), 1217. https://doi.org/10.1136/jim-2020-001295
- Bailey, H., Cruz, M. L. S., Songtaweesin, W. N., & Puthanakit, T. (2017). Adolescents with HIV and transition to adult care in the Caribbean. Journal of the International AIDS Society, 20(Suppl 3):21475. https://doi.org/10.7448/IAS.20.4.21475.
- Balogun, M., Meloni, S. T., Igwilo, U. U., Roberts, A., Okafor, I., & Sekoni, A. (2019). Status of HIV-infected patients classified as lost to follow up from a large antiretroviral program in southwest Nigeria. PLoS ONE 14(7).
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. https://doi.org/10.18637/jss.v067.i01
- Beck, E. J., & Walensky, R. P. (2009). The outcome and impact of 10 years of HAART. In José M. Zuniga, Alan Whiteside, Amin Ghaziani, & John G. Bartlett (Eds.), A decade of HAART (Vol. 10, pp. 45–62). Oxford Scholarship Online.
- Bivand, R., & Lewin-Koh, N. (2017). Maptools: Tools for reading and handling spatial objects.
- Casale, M., Carlqvist, A., & Cluver, L. (2019). Recent interventions to improve retention in HIV care and adherence to antiretroviral treatment among adolescents and youth: A systematic review. AIDS Patient Care and STDs, 33(6), https://doi.org/10.1089/apc.2018.0320
- Charurat, M., Oyegunle, M., & Benjamin, R. (2010). Patient retention and adherence to antiretrovirals in a large antiretroviral therapy program in Nigeria: A longitudinal Analysis for risk factors. PLoS One, 5(5), 10584. https://doi.org/10.1371/journal.pone.0010584
- Cobos Muñoz, D., Merino Amador, P., Monzon Llamas, L., Martinez Hernandez, D., & Santos Sancho, J. (2017). Decentralization of health systems in low and middle income countries: A systematic review. International Journal of Public Health, 62(2), 219–229. https://doi.org/10.1007/s00038-016-0872-2
- Dayyab, F. M., Mukhtar, F., Iliyasu, G., & Habib, A. G. (2021). Determinants of loss to follow-up among people living with HIV on antiretroviral therapy in Nigeria. African Journal of AIDS Research, 20(1), https://doi.org/10.2989/16085906.2021.1874444
- Dibb, Z., & Ohanyido, C. (2018). Listening to the needs and preferences of adolescents living with HIV in Nigeria. Coordinating Comprehensive Care for Children.
- Eluwa, G. I., Adebajo, S., & Idogho, O. (2015). Evaluating the impact of health system strengthening on HIV and sexual risk behaviors in Nigeria. JAIDS Journal of Acquired Immune Deficiency Syndromes, 70(1), 67–74. https://doi.org/10.1097/QAI.0000000000000701
- Enane, L. A., Vreeman, R. C., & Foster, C. (2018). Retention and adherence. Current Opinion in HIV and AIDS, 13(3), 212–219. https://doi.org/10.1097/COH.0000000000000459.
- Fox, J., & Hong, J. (2009). Effect displays in R for multinomial and proportional-odds logit models: Extensions to the effects package. Journal of Statistical Software, 32(1), 1–24. https://doi.org/10.18637/jss.v032.i01
- Fox, M. P., & Rosen, S. (2015). Systematic review of retention of pediatric patients on HIV treatment in low and middle-income countries 2008–2013. Aids (London, England), 29(4), 493–502. https://doi.org/10.1097/QAD.0000000000000559
- Ibrahim, S. S., & Ibrahim, H. (2014). Budgetary allocation dynamics and its impact on poverty spread among the geopolitical zones of Nigeria. American Journal of Economics, 4(2), 124–129. https://doi.org/10.5923/j.economics.20140402.04
- Kim, S.-H., Gerver, S. M., Fidler, S., & Ward, H. (2014). Adherence to antiretroviral therapy in adolescents living with HIV. Aids (london, England), 28(13), https://doi.org/10.1097/QAD.0000000000000316
- Kranzer, K., Govindasamy, D., Ford, N., Johnston, V., & Lawn, S. D. (2012). Quantifying and addressing losses along the continuum of care for people living with HIV infection in sub-Saharan Africa: A systematic review. Journal of the International AIDS Society, 15(2), https://doi.org/10.7448/IAS.15.2.17383
- Luedecke, D. (2017). sjPlot: Data visualization for statistics in social science.
- MacPherson, P., Munthali, C., Ferguson, J., Armstrong, A., Kranzer, K., Ferrand, R. A., & Ross, D. A. (2015). Service delivery interventions to improve adolescents’ linkage, retention and adherence to antiretroviral therapy and HIV care. Tropical Medicine & International Health, 20(8), 1015–1032. https://doi.org/10.1111/tmi.12517
- Mavegam, B. O., Pharr, J. R., Cruz, P., & Ezeanolue, E. E. (2017). Effective interventions to improve young adults’ linkage to HIV care in Sub-Saharan Africa: A systematic review. AIDS Care, 29(10), https://doi.org/10.1080/09540121.2017.1306637
- Mbatia, R., Kikaro, S., & Mgelea, E. (2018). Enhancing HIV retention and clinical outcomes in Tanzania through pediatric and adolescent-friendly services. Working Paper WP 18-204.
- National Agency for the Control of AIDS. (2014). Global AIDS response: Country progress report. National Agency for the Control of AIDS.
- National Agency for the Control of AIDS. (2016). National HIV Strategy for Adolescents and Young People 2016-2020. National Agency for the Control of AIDS.
- National Agency for the Control of AIDS. (2017). National HIV and AIDS Strategic Framework 2017-2021. National Agency for the Control of AIDS, Federal Republic of Nigeria.
- National Population Commission. (2014). Nigeria Demographic and Health Survey 2013. National Population Commission.
- Odafe, S., Torpey, K., & Khamofu, H. (2012). The pattern of attrition from an antiretroviral treatment program in Nigeria. PLoS One, 7(12), 51254. https://doi.org/10.1371/journal.pone.0051254
- Okonkwo, P., Sagay, A. S., & Agaba, P. A. (2014). Treatment outcomes in a decentralized antiretroviral therapy program: A comparison of two levels of care in north central Nigeria. AIDS Research and Treatment, 2014, 560623. https://doi.org/10.1155/2014/560623.
- Okonkwoh, C. (2011). Factors affecting antiretroviral treatment adherence among young adult living with HIV/AIDS in Yaba, Lagos, Nigeria: A qualitative study. Master’s degree thesis. Wageningen University.
- PEPFAR. (2018). Country/Regional Operational Plan (COP/ROP) 2016 Guidance. PEPFAR. 2015. https://www.pepfar.gov/documents/organization/250377.pdf
- R.Core Team. (2021). R: A Language and Environment for Statistical Computing. R Core Team.
- Rosen, S., Larson, B., & Rohr, J. (2014). Effect of antiretroviral therapy on patients’ economic well being. Aids (London, England), 28(3), 417–424. https://doi.org/10.1097/QAD.0000000000000053
- Sethi, A. K., Celentano, D. D., Gange, S. J., Moore, R. D., & Gallant, J. E. (2003). Association between adherence to antiretroviral therapy and human immunodeficiency virus drug resistance. Clinical Infectious Diseases, 37(8), 1112–1118. https://doi.org/10.1086/378301
- Ugwu, R., & Eneh, A. (2013). Factors influencing adherence to paediatric antiretroviral therapy in Portharcourt, South-South Nigeria. Pan African Medical Journal, 16(30). https://doi.org/10.11604/pamj.2013.16.30.1877.
- UNAIDS. (2014). 90-90-90 – An ambitious treatment target to help end the AIDS epidemic. UNAIDS.
- UNAIDS. (2020a). Aidsinfo – Country estimate: “HIV prevalence – young people (15-24).” http://aidsinfo.unaids.org
- UNAIDS. (2020b). Global HIV & AIDS statistics — 2020 fact sheet – HIV estimates with uncertainity bounds 1990-2019. https://www.unaids.org/en/resources/fact-sheet
- UNAIDS / UNICEF. (2016). A progress report: All in to end the adolescent HIV epidemic. UNAIDS/UNICEF HIV.
- USAID/4Children. (2017). New study reveals nearly one third of HIV clients travel outside of their Local Government Area (LGA) for health care in Nigeria. USAID. http://ovcsupport.org/wp-content/uploads/2017/05/Facility-Mapping-Summary_Final.pdf
- Wickham, H. (2009). GGPlot2: Elegant Graphics for Data analysis. Springer-Verlag.
Appendix
(1) Local Governmental Areas in which clinics are situated
(2) Robustness checks
Patient’s facility in same Local Governmental Area of residence – No regions split.
(3) Patient lives in an LGA without a clinic
(4) Predicted probabilities – ART in same LGA
Results displayed in , model statistics and coefficients in .
(5) Predicted probabilities – ART in same LGA individual controls.
The predicted probabilities presented below are the result of models fitting: a base model (Model 1 report), and sequentially adding gender, clinic level, and the binary urban/rural indicator. As such they give some indication of the suppressor effect of individual control variables.