ABSTRACT
With an annual incidence of about 1.5 million new infections, HIV is an ongoing public health concern. Sexual transmission risk behavior (STRB) is a main driver of the HIV epidemic in most Western countries, particularly among specific populations such as men who have sex with men (MSM). This quasi-experimental pilot study examined the effectiveness of a ten-session group intervention, aiming to reduce STRB among a high-risk subpopulation of MSM living with HIV. Self-reported STRB, impulsivity, mental health symptoms, and functional impairment were compared between the intervention group (n = 12) and a control group (n = 16). At baseline, participants in the intervention group had higher levels of STRB, impulsivity, mental health problems, and functional impairment, compared to the control group. A significant time-by-group interaction effect revealed that after the intervention, STRB, impulsivity, and functional impairment reduced in the intervention group to levels comparable to the control group. These findings suggest that a targeted behavioral intervention might be an effective strategy to reduce persistent STRB and related factors in MSM living with HIV. Future studies should confirm these findings in larger samples, using randomized designs.
KEYWORDS:
Introduction
HIV continues to be a major public health concern (UNAIDS, Citation2019a). Every year around 1.5 million people become infected worldwide and approximately 680.000 people die due to HIV-related causes (UNAIDS, Citation2021). Although the incidence of HIV infections is declining in many countries, prevalence rates among specific key populations are still expanding, comprising 93% of all new infections outside sub-Saharan Africa (UNAIDS, Citation2021). One of those key populations are men who have sex with men (MSM), who have a 25 times higher risk of HIV infection compared to the general population and account for the largest proportion of new HIV infections in Western/Central Europe and North America (UNAIDS, Citation2019b).
Engaging in sexual transmission risk behavior (STRB) is the main driver of HIV transmission among various key populations such as MSM (UNAIDS, Citation2016). STRB includes for instance condomless sex, more concurrent sexual partners, and engaging in sex parties or “chemsex” (having sex under the influence of drugs) (Edmundson et al., Citation2018; Parsons et al., Citation2017). When not fully viral suppressed, STRB can cause transmission of HIV (Rodger et al., Citation2019). A subpopulation of MSM living with HIV persistently show STRB after their HIV diagnosis (around 25–40%) (Crepaz et al., Citation2009; Van Kesteren et al., Citation2007) and is, therefore, particularly relevant given their increased risk to transmit HIV (Bradshaw et al., Citation2013; Kumar et al., Citation2015).
Engaging in STRB, also among MSM living with HIV, has been associated with several psychological factors including impulsivity traits (Arends et al., Citation2019; Danko et al., Citation2016; Jemmott et al., Citation2015) and mental health problems (Bakker & Knoops, Citation2018; Safren et al., Citation2010). Aspects of trait-impulsivity associated with higher chances to engage in STRB among MSM living with HIV include high sensation seeking (Kalichman et al., Citation2008; McCoul & Haslam, Citation2001) and reward-sensitivity (Hahn et al., Citation2019; Shuper et al., Citation2014), and low cognitive inhibition (Margolin et al., Citation2007). It has to be acknowledged that the term STRB does not refer to deliberate conscious behavior aimed to transmit HIV (Todd, Citation2008), but to behaviors that may increase the risk of HIV transmission given the above-mentioned circumstances. Mental health problems often associated with STRB in MSM living with HIV include depression, anxiety, and substance abuse (Batchelder et al., Citation2017; Safren et al., Citation2011). Many factors contribute to mental health problems among populations of MSM and people living with HIV, including minority stress and societal stigma (Safren et al., Citation2011). Mental health issues can in turn also fuel impulsive behavior and impair consistently engaging in healthy behaviors such as sexual risk reduction and treatment adherence (Rogers et al., Citation2010; Safren et al., Citation2011).
Several researchers, therefore, stress the importance of developing tailored behavioral interventions to address maladaptive psychological processes, reduce STRB, and improve mental health among MSM living with HIV (Brown et al., Citation2019; Johnson et al., Citation2008; Pedlow & Carey, Citation2004; Safren et al., Citation2011). Various studies show that behavioral interventions might be effective in reducing STRB in MSM (Berg, Citation2009; Johnson et al., Citation2008; Lorimer et al., Citation2013; Pérez et al., Citation2018). However, these studies are mostly not conducted in MSM living with HIV (Johnson et al., Citation2008; Maulsby et al., Citation2013; Pérez et al., Citation2018), commonly lack details concerning their intervention protocol, do not apply validated questionnaires to measure STRB or lack a control group (Herbst et al., Citation2005a; Higa et al., Citation2013; Johnson et al., Citation2008; Pérez et al., Citation2018).
In this study, we tested the effectiveness of a well-defined behavioral intervention aiming to reduce STRB in a Dutch subpopulation of MSM living with HIV, who persistently engage in STRB, using validated tools in a quasi-experimental design. Furthermore, we explored the potential effects of the intervention on impulsivity and mental health beyond STRB. We hypothesized that compared to a control group, participants who received the behavioral intervention would show a pre–post reduction in levels of (a) sexual transmission risk behavior, (b) impulsivity, (c) general mental health symptoms and (d) functional impairment.
Materials and methods
Design
In this open-label, quasi-experimental pilot study in MSM living with HIV the effects of a ten-session behavioral group intervention aiming to reduce STRB were compared with a control group receiving treatment as usual (TAU) with a baseline and six-month follow-up measurement. Given the developmental stage of the intervention, an explorative quasi-experimental design was chosen. The study was conducted in line with the Helsinki Declaration (WMA, Citation2008) and was approved by the local ethical committee (protocol number: 2016-3103).
Setting & participants
Adult MSM living with HIV were recruited by convenience sampling from two Dutch regional HIV centers located in Nijmegen (Radboudumc) and Arnhem (Rijnstate). Inclusion criteria were: male sex assigned at birth, age between 18 and 65 years, having sex with (cisgender) men, and evidence for STRB (indexed by multiple STI diagnoses in the year prior to the study). Excluded were patients with acute psychiatric conditions requiring immediate treatment and patients unable to fill in self-report questionnaires (e.g., due to language issues).
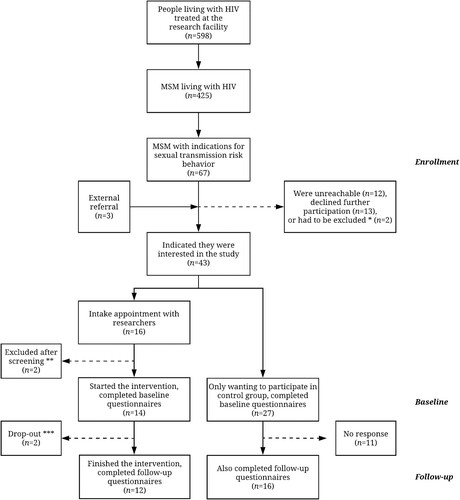
HIV nurse practitioners invited patients meeting the inclusion criteria (n = 70). Patients who wanted to participate were assigned to the intervention group (n = 14) or control group (n = 27), depending on their preference. There were no additional incentives for participants. A total of 28 participants completed follow-up at six months (intervention group: n = 12; control group: n = 16). See for further details on the selection procedure.
Figure 1. Participant inclusion flowchart.
Note. MSM = men who have sex with men. *Excluded as they did not speak/understand Dutch fluently. **One person was excluded as his IQ was indicated to be too low to properly follow the intervention content, another was excluded as he mentioned not being able to attend most of the intervention sessions. ***Both participants dropped out as they were not able to attend the intervention sessions anymore due to planning issues.
Intervention
The behavioral intervention consisted of ten weekly sessions of 2.5 h and homework assignments in between. The intervention was based on principles of Dialectical Behavioral Therapy (DBT). This is a type of cognitive behavioral therapy that includes elements of psychoeducation, motivational interviewing, and skills-training concerning impulse and emotion regulation, as commonly provided in mental health and addiction care facilities (Shoptaw et al., Citation2005; Zapolski & Smith, Citation2017). Topics were standardized per session in a treatment manual adjusted on MSM and HIV/STI (transmission)-related subjects (for the list of treatment components see Supplementary Table 1). The intervention was provided by two trained psychologists (EF & RA), weekly supervised by a specialized psychotherapist (TH) and psychiatrist (AFAS), at the Department of Psychiatry of the Radboudumc. The intervention was on top of treatment as usual (TAU), which consisted of standard pharmacotherapy for HIV and health advice consultations by physicians and nurse practitioners.
Measurements
Baseline sample characteristics
Demographic information (age, level of education, current occupation, marital status, and sexual orientation) was collected using a standard short questionnaire. Medical information was derived from electronic patient records. This included information regarding the years of HIV diagnosis, latest CD4 count (white blood cells), duration of antiretroviral treatment (ART), use of psychiatric medication during the study period, and the amount and results of STI screenings over the past year.
Substance use was assessed by using the Measurements in the Addictions for Triage and Evaluation (MATE 2.1) (Schippers et al., Citation2010). The first module of the measurement was used, consisting of 4 questions regarding lifetime and past-month substance use. The MATE 2.1 was shown to be a reliable measurement with good inter-rater reliability scores in various populations (Schippers et al., Citation2010). STRB, impulsivity, mental health symptoms, and functional impairment were measured with eight questionnaires (specified below).
Sexual transmission risk behavior
The Sexual Risk Survey (SRS) was used to assess the frequency of STRB over the past six months (Turchik & Garske, Citation2009). The 23-item (scale) questionnaire includes one total scale and five subscales, including having various sexual partners, engaging in condomless sex in general, condomless anal sex, impulsiveness regarding sexual behaviors, and the intentions to engage in STRB. Note that the questionnaire does not account for viral suppression. As shown in a youth population, it is a reliable measure to comprehensively assess STRB (Turchik & Garske, Citation2009).
Sexual compulsivity was assessed using the Sexual Compulsivity Scale (SCS). This is a 10-item questionnaire, scored on a 4-point Likert scale (Kalichman & Rompa, Citation1995). One total score is calculated and items encompass compulsive sexual behavior, sexual preoccupations and intrusive thoughts, and lack of sexual impulse control (Kalichman & Cain, Citation2004). The SCS is a valid measurement to assess sexual compulsivity in people living with HIV (Kalichman & Rompa, Citation1995, Citation2001).
The Sexual Sensation Seeking Scale (SSSS) was used to measure the propensity to seek risky sexual stimulation with one total score summing up 17 items, scored on a 4-point Likert scale (Kalichman et al., Citation1994). The SSSS has shown good psychometric characteristics, also among MSM (Kalichman & Rompa, Citation1995).
Impulsivity
The Barrat Impulsiveness Scale 11 (BIS-11) was used to measure impulsivity traits. The BIS-11 is a self-report measure of impulsive behaviors and preferences (Patton & Stanford, Citation1995), consisting of 30 statements with a 4-point Likert scale. It includes three subscales (attentional impulsivity: 8 items, motor impulsivity: 11 items, and non-planning impulsivity: 11 items). The BIS-11 was shown to be a reliable measure, also in clinical samples (Stanford et al., Citation2009).
Impulsive personality was assessed using the Behavioral Inhibition System/Behavioral Activation System scales (BIS/BAS) (Carver & White, Citation1994). It has 24 items with a 4-point Likert scale to examine tendencies towards inhibition and activation of behavior. In this study, the behavioral activation system (BAS) was included, which has three subscales (fun-seeking behavior: 4 items, persistent pursuit of goals: 4 items, and reward responsiveness: 5 items). The BIS/BAS was shown to be a reliable instrument to measure impulsivity traits in various populations (Demianczyk et al., Citation2014).
Reward-related impulsivity was assessed using the Sensitivity to Punishment & Sensitivity to Reward Questionnaire (SPSRQ) (Torrubia et al., Citation2001). It consists of 48 dichotomous items, divided into two scales of 24 items: sensitivity to reward (related to impulsivity traits) and sensitivity to punishment (related to anxiety traits). Only sensitivity to reward was included in this study. The SPSRQ is a reliable measurement of reward sensitivity independent of personality factors (Torrubia et al., Citation2001).
General mental health symptoms and functional impairment
The Depression Anxiety and Stress Scale (DASS-21) was used to assess general mental health symptoms (Norton, Citation2007). The DASS-21 is a self-report questionnaire measuring negative affect using 21 items, scored on a 4-point Likert scale. It is divided into three subscales: depression, anxiety, and stress; with each subscale including a sum score of seven items. The DASS has good internal consistency and reliability of the subscale scores in clinical and non-clinical settings (Osman et al., Citation2012).
The Outcome Questionnaire 45 (OQ-45) was used to assess symptoms of functional impairment. This questionnaire consists of 45 items, scored on a 5-point Likert scale, covering three domains (symptomatic distress: 25 items, interpersonal functioning: 11 items, and social role performance: 9 items). It is a valid and reliable instrument to evaluate impairment in clinical and non-clinical samples (de Jong et al., Citation2007; Lambert et al., Citation1996).
Data analysis
First, baseline characteristics of the intervention and control group were compared using descriptive statistics. Single imputation (stochastic regression) was used for two individual missing item scores, and four unreliable outliers on the SRS (Donders et al., Citation2006).
Second, we analyzed the effects of the intervention using four repeated measures multivariate analyses of variance. The dependent variables in the primary analysis were the three STRB measures (SRS, SCS, and SSSS). In three secondary analyses, the following secondary outcome measures were included: impulsivity (BIS-11, BIS/BAS, and SPSRQ), general mental health symptoms (DASS-21), and functional impairment (OQ-45). Group (behavioral intervention vs. TAU) was the between-subject factor and time (baseline to six months follow-up) the within-subject factor. Age was used as a covariate, as it is assumed to be related to impulsivity and risk behavior (Steinberg et al., Citation2008). An alpha of 0.05 was considered statistically significant, Wilks’ Lambda (multivariate) and Huynh-Feldt (univariate) statistics were reported. All analyzes were performed using IBM SPSS Statistics Version 25.
Results
The groups did not differ on demographic characteristics. However, the intervention participants used more psychiatric medication compared to the control group (X2 = 4.48, p = .034), see .
Table 1. Descriptives of intervention (n = 12) and control (n = 16) participants at baseline.
Primary outcome measures
Multivariate analyses showed a main effect of group on the primary outcome measures of STRB (F(3,23) = 7.72, p = .001, eta2 = .502), with higher levels of STRB reported in the intervention group compared to the control group. Post hoc analysis showed that overall the intervention group reported higher levels of sexual compulsivity (F(1,25) = 23.86, p < .001, eta2 = .488) and sexual sensation seeking (F(1,25) = 11.37, p = .002, eta2 = .313).
Furthermore, multivariate analyses showed a significant interaction effect between group and time on STRB (F(3,23) = 15.08, p < .001, eta2 = .663). Post hoc analysis showed stronger decreases of sexual risk behavior (F(1,25) = 4.57, p = .043, eta2 = .154), sexual compulsivity (F(1,25) = 38.90, p < .001, eta2 = .609), and sexual sensation seeking (F(1,25) = 16.00, p < .001, eta2 = .390) within the intervention group, compared to the control group ( and ).
Figure 2. Comparison of sexual transmission risk behavior between the intervention group and the control group.
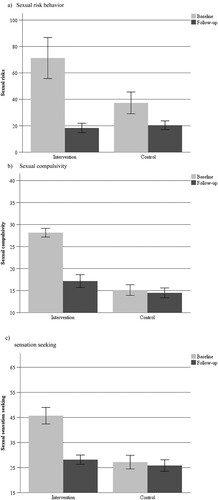
Table 2. Changes in sexual transmission risk behavior, impulsivity, mental health, and functional impairment among groups over time.
Secondary outcome measures
The intervention group reported higher levels of impulsivity compared to the control group (F(7,19) = 8.20, p < .001, eta2 = .751). Post hoc analysis showed overall higher levels of attentional impulsivity (F(1,25) = 29.29, p < .001, eta2 = .540) and motor impulsivity (F(1,25) = 24.69, p < .001, eta2 = .497) in the intervention group compared to the control group. Furthermore, the intervention group reported more mental health symptoms (F(3,23) = 6.64, p = .002, eta2 = .464), specifically higher levels of stress symptoms (F(1,25) = 7.19, p = .013, eta2 = .223). Finally, the intervention group also reported higher levels of functional impairment compared to the control group (F(3,23) = 4.15, p = .017, eta2 = .351), including more impairment related to symptomatic distress, interpersonal functioning, and social role performance (respectively F(1,25) = 6.99, p = .014, eta2 = .218, F(1,25) = 13.18, p = .001, eta2 = .345, and F(1,25) = 6.64, p = .016, eta2 = .210).
There was also a significant interaction effect between group and time for impulsivity (F(7,19) = 6.84, p < .001, eta2 = .716). Post hoc analysis showed that this effect was mainly driven by decreased attention-related and motor-related impulsivity in the intervention group (respectively F(1,25) = 13.75, p = .001, eta2 = .355 and F(1,25) = 29.87, p < .001, eta2 = .544). Furthermore, reward-related impulsivity showed opposite changes in both groups, with an increase in the intervention group compared to a decrease in the control group (reward responsiveness on BAS: F(1,25) = 6.19, p = .020, eta2 = .198 and sensitivity to reward on SPSRQ: F(1,25) = 6.13, p = .020, eta2 = .197).
There was no significant interaction effect between group and time for general mental health symptoms, but there was for functional impairment (F(3,23) = 7.64, p = .001, eta2 = .499). In the intervention group, there was a stronger decrease of impairment in interpersonal functioning (F(1,25) = 16.47, p < .001, eta2 = .397), compared to the control group. See for further details.
Discussion
In this quasi-experimental study, we examined the effectiveness of a behavioral group intervention aiming to reduce STRB in MSM living with HIV and persistent STRB. Compared to the control group, participants in the behavioral intervention reported higher levels of STRB, impulsivity, general mental health symptoms, and functional impairment. Participants of the behavioral intervention reduced their STRB to levels comparable to the control group at follow-up. Furthermore, the intervention showed an effect on attentional and reward impulsivity, as well as functional impairment regarding interpersonal relations.
At baseline participants of the intervention group showed higher levels of STRB, impulsivity, general mental health problems, and functional impairment. This suggests a selection bias, which can be related to the quasi-experimental study design. People with higher levels of experienced problems might have had more intrinsic motivation to participate in the behavioral intervention or they possibly have been more motivated by healthcare workers for behavioral change. Moreover, the severity of mental health problems and functional impairment observed in the intervention group were at a clinical level (de Jong et al., Citation2007; Lovibond & Lovibond, Citation1996). Previous research showed that mental health issues can be related to more impulsive behavior and impair engaging in healthy behaviors such as sex- or drugs-related risk reduction, and reduce effectiveness of prevention programs (Rogers et al., Citation2010; Safren et al., Citation2011). Furthermore, in our study, over 90% of the participants reported illicit drug use in the previous month. The combination of these findings emphasize the importance to pay attention to impulsivity, mental health, and substance use (including their interactions) when studying STRB among MSM living with HIV (Batchelder et al., Citation2017; Safren et al., Citation2010).
The observed reductions in STRB after the behavioral intervention are in line with previous uncontrolled studies suggesting that behavioral interventions for MSM can be effective in reducing STRB (Herbst et al., Citation2005b; Higa et al., Citation2013; Johnson et al., Citation2008). It is tempting to assume that the observed reductions in STRB are a direct result of the behavioral intervention. However, several other explanations should be taken into account, especially given the baseline differences between groups.
First, reductions in STRB in the intervention group might be related to non-specific effects of being in the intervention group (McCarney et al., Citation2007). For example, meeting other people once a week might have had an impact on participants’ behavior and well-being. Moreover, expectations concerning the effects of the intervention, or increased awareness of their behavior by participating in the study, might affected their behavior.
Furthermore, reductions in STRB in the intervention group might have occurred due to spontaneous remission or natural fluctuations over time. Such spontaneous change can be questioned, given the long history of STRB in these participants, and the higher severity profile of participants in the intervention group. Previous studies indeed indicate that spontaneous remission of STRB is often unlikely (Herrick et al., Citation2011; McKirnan et al., Citation2001).
Finally, effects of regression to the mean or biased participant reports cannot be fully ruled out with the current quasi-experimental study design (Miller & Kaptchuk, Citation2008; Peiris et al., Citation2018). Future research should include a randomized design with substantially large samples, to avoid baseline group differences, as well as a placebo group intervention, in order to draw firm conclusions concerning effectiveness.
The reductions in motor and attentional impulsivity among participants of the behavioral intervention further suggest that participants in the intervention group may have developed coping skills to better regulate impulses, and subsequently reduce their STRB. These findings are in line with previous studies, suggesting that the development of alternative coping skills can reduce STRB (Puckett et al., Citation2017). Indeed, specifically higher levels of motor and attentional impulsivity have been related to lower self-regulatory abilities (Meule et al., Citation2017) and STRB (Arends et al., Citation2019; Horvath & Zuckerman, Citation1993; Semple et al., Citation2006).
The observed small but significant opposing effects between groups on reward sensitivity over time are not in line with the other impulsivity findings. Although, reward sensitivity has previously been linked to (transmission) risk behavior (Loxton, Citation2018; Peeters et al., Citation2017), there is also evidence that increased reward-sensitivity is associated with goal achievement, engagement in healthy rewarding behaviors, and reduced levels of depression (Telzer, Citation2016). This suggests that increased levels of reward sensitivity may represent either a vulnerability or an opportunity depending on the motivational context (Telzer, Citation2016). As the current intervention focused on increasing motivation and development of skills to engage in health-promoting behaviors, the observed effects on reward sensitivity might reflect the desired behavioral change among intervention participants (Linke & Wessa, Citation2017). Future studies should further explore the role of reward sensitivity in behavioral change. Furthermore, in this study we only focused on MSM living with HIV. Future studies might explore whether this intervention might also support behavioral change and improve mental health in other populations of people engaging in STRB.
The results of current study should also be seen in the light of some study limitations. First, the study consisted of a small-scale pilot with a quasi-experimental design. We deliberately chose a pilot approach given the explorative nature of testing a new behavioral intervention in a specific population. The selection of participants at an HIV clinic having had multiple positive STI screenings might have created a selection bias of people motivated to engage in health promotion interventions. However, in line with previous intervention studies on STRB among MSM, we encountered difficulties recruiting participants (Jenkins, Citation2012; Johnson et al., Citation2008). Since people frequently mentioned privacy issues related to the group intervention, more anonymous treatment options like eHealth might be of interest. Indeed, a recent review showed preliminary evidence that eHealth interventions can contribute to behavioral change related to HIV/STI prevention among MSM (Nguyen et al., Citation2019).
Furthermore, this pilot study into the effectiveness of a cognitive-dialectical based intervention did not shed light on the most effective ingredients and the mechanisms of action of the intervention. Though it has been shown that cognitive and dialectical behavioral therapy can increase impulse and emotion regulation and reduce risky behaviors such as sex- and substance-related risk behavior (Covey et al., Citation2016; Crepaz et al., Citation2008; Maffei et al., Citation2018), future studies might further explore which elements of the intervention are related to which behavioral outcomes. Given the study limitations outlined above, future studies should replicate current findings in sufficiently large samples, in and outside a hospital setting, and employ randomization.
Conclusion
This pilot work suggests that a ten-session behavioral intervention can reduce STRB in MSM living with HIV. Though these data need replication in substantially large samples, using more rigorous study designs, our findings warrant interdisciplinary collaboration of mental and somatic health professionals to improve quality of life in MSM living with HIV and reduce transmission of HIV.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
- Arends, R. M., Nelwan, E. J., Soediro, R., Van Crevel, R., Alisjahbana, B., Pohan, H. T., & Schellekens, A. F. (2019). Associations between impulsivity, risk behavior and HIV, HBV, HCV and syphilis seroprevalence among female prisoners in Indonesia: A cross-sectional study. PLoS One, 14(2), e0207970. https://doi.org/10.1371/journal.pone.0207970
- Bakker, I., & Knoops, L. (2018). Towards a continuum of care concerning chemsex issues. Sexual Health, 15(2), 173–175. https://doi.org/10.1071/SH17139
- Batchelder, A. W., Safren, S., Mitchell, A. D., Ivardic, I., & O’Cleirigh, C. (2017). Mental health in 2020 for men who have sex with men in the United States. Sexual Health, 14(1), 59–71. https://doi.org/10.1071/SH16083
- Berg, R. (2009). The effectiveness of behavioural and psychosocial HIV/STI prevention interventions for MSM in Europe: A systematic review. Eurosurveillance, 14(48), 19430. https://doi.org/10.2807/ese.14.48.19430-en
- Bradshaw, D., Matthews, G., & Danta, M. J. (2013). Sexually transmitted hepatitis C infection: The new epidemic in MSM? Current Opinion in Infectious Diseases, 26(1), 66–72. https://doi.org/10.1097/QCO.0b013e32835c2120
- Brown, J. L., Vanable, P. A., Bostwick, R. A., & Carey, M. P. J. A. (2019). A pilot intervention trial to promote sexual health and stress management among HIV-infected men who have Sex with Men. Behavior, 23(1), 48–59. https://doi.org/10.1007/s10461-018-2234-y
- Carver, C. S., & White, T. L. (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology, 67(2), 319–333. https://doi.org/10.1037/0022-3514.67.2.319
- Covey, J., Rosenthal-Stott, H. E., & Howell, S. J. (2016). A synthesis of meta-analytic evidence of behavioral interventions to reduce HIV/STIs. Journal of Behavioral Medicine, 39(3), 371–385. https://doi.org/10.1007/s10865-016-9714-1
- Crepaz, N., Marks, G., Liau, A., Mullins, M. M., Aupont, L. W., & Marshall, K. J. (2009). Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: A meta-analysis. AIDS, 23(13), 1617–1629. https://doi.org/10.1097/QAD.0b013e32832effae
- Crepaz, N., Passin, W. F., Herbst, J. H., Rama, S. M., Malow, R. M., Purcell, D. W., & Wolitski, R. J. (2008). Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychology, 27(1), 4. https://doi.org/10.1037/0278-6133.27.1.4
- Danko, M., Buzwell, S., & Earle, M. J. S. A. (2016). Men at risk of HIV: Sexual sensation seeking, sexual compulsivity and sexual risk behavior among Australian MSM who frequently present for post-exposure prophylaxis. Compulsivity, 23(4), 324–341. https://doi.org/10.1080/10720162.2016.1140605
- de Jong, K., Nugter, M. A., Polak, M. G., Wagenborg, J. E., Spinhoven, P., & Heiser, W. J. (2007). The Outcome Questionnaire (OQ-45) in a Dutch population: A cross-cultural validation. Clinical Psychology & Psychotherapy, 14(4), 288–301. https://doi.org/10.1002/cpp.529
- Demianczyk, A. C., Jenkins, A. L., Henson, J. M., & Conner, B. T. (2014). Psychometric evaluation and revision of Carver and White’s BIS/BAS scales in a diverse sample of young adults. Journal of Personality Assessment, 96(5), 485–494. https://doi.org/10.1080/00223891.2013.870570
- Donders, A. R. T., Van Der Heijden, G. J., Stijnen, T., & Moons, K. G. (2006). A gentle introduction to imputation of missing values. Journal of Clinical Epidemiology, 59(10), 1087–1091. https://doi.org/10.1016/j.jclinepi.2006.01.014
- Edmundson, C., Heinsbroek, E., Glass, R., Hope, V., Mohammed, H., White, M., & Desai, M. (2018). Sexualised drug use in the United Kingdom (UK): A review of the literature. International Journal of Drug Policy, 55, 131–148. https://doi.org/10.1016/j.drugpo.2018.02.002
- Hahn, H., Kalnitsky, S., Haines, N., Thamotharan, S., Beauchaine, T. P., & Ahn, W.-Y. (2019). Delay discounting of protected sex: Relationship type and sexual orientation influence sexual risk behavior. Archives of Sexual Behavior, 48(7), 2089–2102. https://doi.org/10.1007/s10508-019-1450-5
- Herbst, J. H., Sherba, R. T., Crepaz, N., DeLuca, J. B., Zohrabyan, L., & Stall, R. D. (2005a). A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 39(2), 228–241. https://doi.org/10.1097/01.qai.0000151077.88193.15
- Herbst, J. H., Sherba, R. T., Crepaz, N., DeLuca, J. B., Zohrabyan, L., & Stall, R. D. (2005b). A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. JAIDS, 39(2), 228–241. https://doi.org/10.1097/00126334-200501010-00012
- Herrick, A. L., Lim, S. H., Wei, C., Smith, H., Guadamuz, T., Friedman, M. S., & Stall, R. (2011). Resilience as an untapped resource in behavioral intervention design for gay men. AIDS and Behavior, 15(1), 25–29. https://doi.org/10.1007/s10461-011-9895-0
- Higa, D. H., Crepaz, N., Marshall, K. J., Kay, L., Vosburgh, H. W., Spikes, P., & Purcell, D. W. (2013). A systematic review to identify challenges of demonstrating efficacy of HIV behavioral interventions for gay, bisexual, and other men who have sex with men (MSM). AIDS and Behavior, 17(4), 1231–1244. https://doi.org/10.1007/s10461-013-0418-z
- Horvath, P., & Zuckerman, M. (1993). Sensation seeking, risk appraisal, and risky behavior. Personality and Individual Differences, 14(1), 41–52. https://doi.org/10.1016/0191-8869(93)90173-Z
- Jemmott, J. B., Jemmott, L. S., O’Leary, A., Icard, L. D., Rutledge, S. E., Stevens, R., & Stephens, A. J. (2015). On the efficacy and mediation of a one-on-one HIV risk-reduction intervention for African American men who have sex with men: A randomized controlled trial. AIDS and Behavior, 19(7), 1247–1262. https://doi.org/10.1007/s10461-014-0961-2
- Jenkins, R. A. J. A. (2012). Recruiting substance-using men who have sex with men into HIV prevention research: Current status and future directions. AIDS and Behavior, 16(6), 1411–1419. https://doi.org/10.1007/s10461-011-0037-5
- Johnson, W. D., Diaz, R. M., Flanders, W. D., Goodman, M., Hill, A. N., Holtgrave, D., & McClellan, W. M. (2008). Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews, (3), CD001230. https://doi.org/10.1002/14651858.CD001230.pub2
- Kalichman, S. C., & Cain, D. (2004). The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. Journal of Sex Research, 41(3), 235–241. https://doi.org/10.1080/00224490409552231
- Kalichman, S. C., Johnson, J. R., Adair, V., Rompa, D., Multhauf, K., & Kelly, J. A. (1994). Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment, 62(3), 385–397. https://doi.org/10.1207/s15327752jpa6203_1
- Kalichman, S. C., & Rompa, D. (1995). Sexual sensation seeking and sexual compulsivity scales: Validity, and predicting HIV risk behavior. Journal of Personality Assessment, 65(3), 586–601. https://doi.org/10.1207/s15327752jpa6503_16
- Kalichman, S. C., & Rompa, D. (2001). The Sexual Compulsivity Scale: Further development and use with HIV-positive persons. Journal of Personality Assessment, 76(3), 379–395. https://doi.org/10.1207/S15327752JPA7603_02
- Kalichman, S. C., Simbayi, L., Jooste, S., Vermaak, R., & Cain, D. (2008). Sensation seeking and alcohol use predict HIV transmission risks: Prospective study of sexually transmitted infection clinic patients, Cape Town, South Africa. Addictive Behaviors, 33(12), 1630–1633. https://doi.org/10.1016/j.addbeh.2008.07.020
- Kumar, S., Rao, P., Earla, R., & Kumar, A. J. (2015). Drug–drug interactions between anti-retroviral therapies and drugs of abuse in HIV systems. Expert Opinion on Drug Metabolism & Toxicology, 11(3), 343–355. https://doi.org/10.1517/17425255.2015.996546
- Lambert, M. J., Hansen, N., Umpress, V., Lunnen, K., Okiishi, J., Burlingame, G., & Reisinger, C. (1996). Administration and scoring manual for the OQ-45.2. American Professional Credentialing Services.
- Linke, J., & Wessa, M. (2017). Mental imagery training increases wanting of rewards and reward sensitivity and reduces depressive symptoms. Behavior Therapy, 48(5), 695–706. https://doi.org/10.1016/j.beth.2017.04.002
- Lorimer, K., Kidd, L., Lawrence, M., McPherson, K., Cayless, S., & Cornish, F. (2013). Systematic review of reviews of behavioural HIV prevention interventions among men who have sex with men. AIDS Care, 25(2), 133–150. https://doi.org/10.1080/09540121.2012.699672
- Lovibond, S. H., & Lovibond, P. F. (1996). Manual for the depression anxiety stress scales. Psychology Foundation of Australia.
- Loxton, N. J. (2018). The role of reward sensitivity and impulsivity in overeating and food addiction. Current Addiction Reports, 5(2), 212–222. https://doi.org/10.1007/s40429-018-0206-y
- Maffei, C., Cavicchioli, M., Movalli, M., Cavallaro, R., & Fossati, A. (2018). Dialectical behavior therapy skills training in alcohol dependence treatment: Findings based on an open trial. Substance Use & Misuse, 53(14), 2368–2385. https://doi.org/10.1080/10826084.2018.1480035
- Margolin, A., Schuman-Olivier, Z., Beitel, M., Arnold, R. M., Fulwiler, C. E., & Avants, S. K. (2007). A preliminary study of spiritual self-schema (3-S+) therapy for reducing impulsivity in HIV-positive drug users. Journal of Clinical Psychology, 63(10), 979–999. https://doi.org/10.1002/jclp.20407
- Maulsby, C., Millett, G., Lindsey, K., Kelley, R., Johnson, K., Montoya, D., & Holtgrave, D. (2013). A systematic review of HIV interventions for black men who have sex with men (MSM). BMC Public Health, 13(1), 625. https://doi.org/10.1186/1471-2458-13-625
- McCarney, R., Warner, J., Iliffe, S., Van Haselen, R., Griffin, M., & Fisher, P. (2007). The Hawthorne effect: A randomised, controlled trial. BMC Medical Research Methodology, 7(1), 30. https://doi.org/10.1186/1471-2288-7-30
- McCoul, M. D., & Haslam, N. (2001). Predicting high risk sexual behaviour in heterosexual and homosexual men: The roles of impulsivity and sensation seeking. Personality and Individual Differences, 31(8), 1303–1310. https://doi.org/10.1016/S0191-8869(00)00222-1
- McKirnan, D. J., Vanable, P. A., Ostrow, D. G., & Hope, B. (2001). Expectancies of sexual “escape” and sexual risk among drug-and alcohol-involved gay and bisexual men. Journal of Substance Abuse, 13(1-2), 137–154. https://doi.org/10.1016/S0899-3289(01)00063-3
- Meule, A., de Zwaan, M., & Müller, A. (2017). Attentional and motor impulsivity interactively predict ‘food addiction’ in obese individuals. Comprehensive Psychiatry, 72, 83–87. https://doi.org/10.1016/j.comppsych.2016.10.001
- Miller, F. G., & Kaptchuk, T. J. (2008). The power of context: Reconceptualizing the placebo effect. Journal of the Royal Society of Medicine, 101(5), 222–225. https://doi.org/10.1258/jrsm.2008.070466
- Nguyen, L. H., Tran, B. X., Rocha, L. E., Nguyen, H. L. T., Yang, C., Latkin, C. A., & Strömdahl, S. (2019). A systematic review of eHealth interventions addressing HIV/STI prevention among men who have sex with men. AIDS and Behavior, 23(9), 2253–2272. https://doi.org/10.1007/s10461-019-02626-1
- Norton, P. J. (2007). Depression Anxiety and Stress scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress & Coping, 20(3), 253–265. https://doi.org/10.1080/10615800701309279
- Osman, A., Wong, J. L., Bagge, C. L., Freedenthal, S., Gutierrez, P. M., & Lozano, G. (2012). The depression anxiety stress scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. Journal of Clinical Psychology, 68(12), 1322–1338. https://doi.org/10.1002/jclp.21908
- Parsons, J. T., Rendina, H. J., Moody, R. L., Gurung, S., Starks, T. J., & Pachankis, J. E. (2017). Feasibility of an emotion regulation intervention to improve mental health and reduce HIV transmission risk behaviors for HIV-positive gay and bisexual men with sexual compulsivity. AIDS and Behavior, 21(6), 1540–1549. https://doi.org/10.1007/s10461-016-1533-4
- Patton, J. H., & Stanford, M. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. https://doi.org/10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
- Pedlow, C. T., & Carey, M. P. (2004). Developmentally appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Annals of Behavioral Medicine, 27(3), 172. https://doi.org/10.1207/s15324796abm2703_5
- Peeters, M., Oldehinkel, T., & Vollebergh, W. (2017). Behavioral control and reward sensitivity in adolescents’ risk taking behavior: A longitudinal TRAILS study. Frontiers in Psychology, 8, 231. https://doi.org/10.3389/fpsyg.2017.00231
- Peiris, N., Blasini, M., Wright, T., & Colloca, L. (2018). The placebo phenomenon: A narrow focus on psychological models. Perspectives in Biology and Medicine, 61(3), 388. https://doi.org/10.1353/pbm.2018.0051
- Pérez, A., Santamaria, E. K., & Operario, D. (2018). A systematic review of behavioral interventions to reduce condomless sex and increase HIV testing for Latino MSM. Journal of Immigrant and Minority Health, 20(5), 1261–1276. https://doi.org/10.1007/s10903-017-0682-5
- Puckett, J. A., Newcomb, M. E., Garofalo, R., & Mustanski, B. (2017). Examining the conditions under which internalized homophobia is associated with substance use and condomless sex in young MSM: The moderating role of impulsivity. Annals of Behavioral Medicine, 51(4), 567–577. https://doi.org/10.1007/s12160-017-9878-0
- Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., Degen, O., & Beloukas, A. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): Final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428–2438. https://doi.org/10.1016/S0140-6736(19)30418-0
- Rogers, R. D., Moeller, F. G., Swann, A. C., & Clark, L. (2010). Recent research on impulsivity in individuals with drug use and mental health disorders: Implications for alcoholism. Alcoholism: Clinical Experimental Research, 34(8), 1319–1333. https://doi.org/10.1111/j.1530-0277.2010.01216.x
- Safren, S. A., Blashill, A. J., & O’Cleirigh, C. M. (2011). Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior, 15(1), 30–34. https://doi.org/10.1007/s10461-011-9898-x
- Safren, S. A., Reisner, S. L., Herrick, A., Mimiaga, M. J., & Stall, R. (2010). Mental health and HIV risk in men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 55(Suppl. 2), S74. https://doi.org/10.1097/QAI.0b013e3181fbc939
- Schippers, G. M., Broekman, T. G., Buchholz, A., Koeter, M. W., & Van Den Brink, W. (2010). Measurements in the Addictions for Triage and Evaluation (MATE): An instrument based on the World Health Organization family of international classifications. Addiction, 105(5), 862–871. https://doi.org/10.1111/j.1360-0443.2009.02889.x
- Semple, S. J., Zians, J., Grant, I., & Patterson, T. L. (2006). Methamphetamine use, impulsivity, and sexual risk behavior among HIV-positive men who have sex with men. Journal of Addictive Diseases, 25(4), 105–114. https://doi.org/10.1300/J069v25n04_10
- Shoptaw, S., Reback, C. J., Peck, J. A., Yang, X., Rotheram-Fuller, E., Larkins, S., & Hucks-Ortiz, C. (2005). Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug and Alcohol Dependence, 78(2), 125–134. https://doi.org/10.1016/j.drugalcdep.2004.10.004
- Shuper, P. A., Joharchi, N., & Rehm, J. (2014). Personality as a predictor of unprotected sexual behavior among people living with HIV/AIDS: A systematic review. AIDS and Behavior, 18(2), 398–410. https://doi.org/10.1007/s10461-013-0554-5
- Stanford, M. S., Mathias, C. W., Dougherty, D. M., Lake, S. L., Anderson, N. E., & Patton, J. H. (2009). Fifty years of the Barratt impulsiveness scale: An update and review. Personality and Individual Differences, 47(5), 385–395. https://doi.org/10.1016/j.paid.2009.04.008
- Steinberg, L., Albert, D., Cauffman, E., Banich, M., Graham, S., & Woolard, J. (2008). Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology, 44(6), 1764. https://doi.org/10.1037/a0012955
- Telzer, E. H. (2016). Dopaminergic reward sensitivity can promote adolescent health: A new perspective on the mechanism of ventral striatum activation. Developmental Cognitive Neuroscience, 17, 57–67. https://doi.org/10.1016/j.dcn.2015.10.010
- Todd, P. (2008). Unconscious mental factors in HIV infection. Mind and Matter, 6(2), 193–206.
- Torrubia, R., Avila, C., Moltó, J., & Caseras, X. (2001). The Sensitivity to Punishment and Sensitivity to Reward Questionnaire (SPSRQ) as a measure of Gray’s anxiety and impulsivity dimensions. Personality and Individual Differences, 31(6), 837–862. https://doi.org/10.1016/S0191-8869(00)00183-5
- Turchik, J. A., & Garske, J. P. (2009). Measurement of sexual risk taking among college students. Archives of Sexual Behavior, 38(6), 936–948. https://doi.org/10.1007/s10508-008-9388-z
- UNAIDS. (2016). Prevention gap report. http://www.unaids.org/en/resources/documents/2016/prevention-gap
- UNAIDS. (2019a). Global AIDS update.
- UNAIDS. (2019b). UNAIDS DATA 2019. http://rstesa.unaids.org/documents/publications/77-2019-unaids-data-en/file
- UNAIDS. (2021). Global HIV & AIDS statistics –- 2021 fact sheet. https://www.unaids.org/en/resources/fact-sheet
- Van Kesteren, N. M., Hospers, H. J., & Kok, G. (2007). Sexual risk behavior among HIV-positive men who have sex with men: A literature review. Patient Education and Counseling, 65(1), 5–20. https://doi.org/10.1016/j.pec.2006.09.003
- WMA. (2008). Declaration of Helsinki: Ethical principles for medical research involving human subjects. https://www.wma.net/wp-content/uploads/2016/11/DoH-Oct2008.pdf
- Zapolski, T. C., & Smith, G. T. (2017). Pilot study: Implementing a brief DBT skills program in schools to reduce health risk behaviors among early adolescents. The Journal of School Nursing, 33(3), 198–204. https://doi.org/10.1177/1059840516673188
