ABSTRACT
Youth living with HIV in sub-Saharan Africa have poor HIV care outcomes. We determined the association of recent significant life-events with HIV antiretroviral treatment (ART) initiation and HIV viral suppression in youth aged 15–24 years living with HIV in rural Kenya and Uganda. This was a cross-sectional analysis of 995 youth enrolled in the SEARCH Youth study. At baseline, providers assessed recent (within 6 months) life-events, defined as changes in schooling/employment, residence, partnerships, sickness, incarceration status, family strife or death, and birth/pregnancy, self-reported alcohol use, being a parent, and HIV-status disclosure. We examined the frequencies of events and their association with ART status and HIV viral suppression (<400 copies/ul). Recent significant life-events were prevalent (57.7%). Having >2 significant life-events (aOR = 0.61, 95% CI:0.45-0.85) and consuming alcohol (aOR = 0.61, 95% CI:0.43-0.87) were associated with a lower odds of HIV viral suppression, while disclosure of HIV-status to partner (aOR = 2.39, 95% CI:1.6-3.5) or to family (aOR = 1.86, 95% CI:1.3-2.7), being a parent (aOR = 1.8, 95% CI:1.2-2.5), and being single (aOR = 1.6, 95% CI:1.3-2.1) had a higher odds. This suggest that two or more recent life-events and alcohol use are key barriers to ART initiation and achievement of viral suppression among youth living with HIV in rural East Africa.
Trial registration: ClinicalTrials.gov identifier: NCT03848728..
Introduction
Adolescents and young adults represent a growing share of people living with HIV. Despite significant gains made across Africa in HIV testing, treatment coverage, and viral suppression overall, youth continue to have lower HIV testing rates, engagement in care, and viral suppression compared to older adults (Brown, Getahun, et al., Citation2019; Nachega et al., Citation2018; Petersen et al., Citation2017; UNAIDS, Citation2019) Critically, adolescents remain the only population in which AIDS death rates have stagnated or are still rising (UNAIDS, Citation2020).
Adolescence and young adulthood represent unique periods in human life with concurrent physical and psychological transitions as well as significant developmental life-events, including completion of or leaving school, start of sexual relations, marriage, and childbearing (Arnett, Citation2014; Fatusi & Hindin, Citation2010; Guan et al., Citation2019). For adolescents and youth living with HIV, who often have multiple social vulnerabilities and must navigate lifelong care, these transitions and life-events can have significant impacts on their ability to access and engage in HIV care and remain adherent to medications.
While there is evidence for the negative effect of stressful life-events and transitions on lifelong care and health behaviors among adults and young people with chronic illness in the United States, (Brown, Harrison, et al., Citation2019; Murphy et al., Citation2000; O'Donnell et al., Citation2017; Oren et al., Citation2017; Pence et al., Citation2010; Walders-Abramson et al., Citation2014; Williams et al., Citation2006) there is a paucity of information on the occurrence of significant life-events among African adolescents and youth living with HIV and how life-events affect HIV care engagement and treatment outcomes (Filiatreau et al., Citation2021; Peer et al., Citation2020). Understanding the impact of significant life-events on care engagement and treatment outcomes in adolescents and youth with HIV may inform models of care that are optimally differentiated for youth’s needs. Therefore, the objective of this research was to describe the frequency of recent significant life-events and to examine the association between recent life-events and ART engagement and HIV viral suppression among youth receiving or starting HIV care in rural African HIV clinics.
Materials and methods
Study design and setting
This was a cross-sectional analysis of baseline data collected as part of the SEARCH Youth study (Strategic Antiretroviral Therapy and HIV Testing for Youth in Rural Africa. ClinicalTrials.gov Identifier: NCT03848728). The SEARCH Youth study is a cluster randomized clinical trial to evaluate the effect on HIV viral suppression of a combination intervention designed to address structural barriers, psychological and social needs, and life-stage events of youth living with HIV and receiving care in 28 rural health facilities, with 14 in southwestern Uganda and 14 in western Kenya. In this setting, HIV prevalence ranges from 3.4% (Uganda) to 18.4% (Kenya) (Chamie et al., Citation2016).
Participants
Youth were eligible if they were aged 15–24 years and were newly diagnosed with HIV, had a prior HIV diagnosis but did not start ART, were already on ART, or were re-engaging with care in the 14 intervention clinics (7 in Uganda and 7 in Kenya) participating in the SEARCH Youth study. The study sample for this analysis includes all participants enrolled between March 2019 through October 2020 and randomized to the SEARCH Youth study intervention arm.
Procedures
Demographic information including age, sex, education attainment, marital status, employment status, and parental status were collected. Participants in the intervention arm were assessed for recent significant life-events through provider checklist assisted interviews asking about any recent (within six months) major life-events: start or stop school or employment, change in residence, divorce/separation or relationship strife, new sexual partners, family death, sickness, incarceration, family strife, and birth or pregnancy. Males were asked the pregnancy/childbirth questions with the context of its occurrence within their primary relationship. The choice of recent life-events measured was informed by a combination of the adolescent development theoretical framework and preliminary qualitative investigations into HIV care barriers for youth that were used to develop the SEARCH-Youth study intervention. The set of life-events measured was chosen to represent the breadth of potential significant life-event issues across the target age range and demographics of HIV-infected youth in Uganda and Kenya. Providers also inquired about alcohol use, mobility (travel away from home > 1 month in a year), and HIV status disclosure to family, friends, and partners in the preceding 6 months. ART history and a baseline viral load test (Cepheid Xpert® HIV-1 Viral Load) were also obtained.
Statistical methods
ART initiation was defined as having initiated ART at least 6 months prior to enrollment into the SEARCH Youth study, and HIV viral suppression defined as having a baseline viral load of <400 copies/ul. Individuals were considered to be re-engaging in HIV care if they had started ART ≥ 6 months prior to enrollment, but had not been seen for HIV care for the past 6 months or otherwise reported dropping out of care.
Composite variables representing participant report of 2 or more, 3 or more recent significant life-events, and the total number of reported recent life-event categories were created. The rationale for examining the total number of recent life-events and the 2+, and 3 + cut-offs was to investigate potential linear and threshold effects of having multiple recent life-events. Summary measures of baseline demographics, life-events, and behaviors were calculated overall, and by gender, age group, and baseline ART status (starting at enrollment, starting <6 months prior, starting ≥ 6 prior and engaged in HIV care, and starting ≥ 6 prior and re-engaging in HIV care). Chi-square or Fisher’s exact tests were used to test for significant difference by sex as appropriate. Univariable and multivariable analyses were conducted to assess the associations between baseline HIV viral suppression and recent life-events, participant demographics, and reported behaviors. Calculation of 95% confidence intervals for the odds ratio associated with individual life-events were obtained from bivariate logistic regression analysis coefficients and standard error using standard formulas. ART status was not included in these analyses as it was hypothesized to be on the causal pathway between the predictors and HIV viral suppression. Multivariable analyses were repeated within the key subgroup of participants who initiated ART ≥ 6 months prior to enrollment and were engaged in care. Among all participants, multivariable analyses were implemented to examine the associations between baseline ART duration (initiated ≥ 6 more prior to enrollment) and recent life-events, demographics, and behaviors. All standard error estimates accounted for clustering by clinic using a sandwich variance estimator. Unless otherwise stated, the respective reference group for reported predictors in the assessment of odds ratios is the natural converse of the predictor (e.g., Disclosure of HIV status to their partner, reference group of those who did not disclose HIV to their partner).
Ethics
The ethical and institutional review boards of Makerere University, the Uganda National Council of Science and technology, the Kenya Medical Research council, and the University of California San Francisco approved this study.
Results
Baseline participants characteristics
A total of 995 participants aged 15–24 years were enrolled into the intervention arm of the SEARCH Youth trial between March 2019 and October 2020 in Kenya and Uganda. Most participants were female (n = 826, 83%). Participants’ demographics and behaviors at enrollment are shown in .
Table 1. Participant demographics, overall and by gender.
The median age was 21 years with males being slightly younger on average (mean 19.9 years for males vs. 20.7 years for females). One hundred fifty-five participants (15.6%) were younger than 18 including 30.8% of all male participants and 12.5% of female participants. Marital status differed meaningfully for males and females with 27.2% of males and 63.2% of females reporting having been ever married. More than half (57.8%) had one or more biological child with two-thirds of females (63.7%) and one-third of males (29%) reporting that they were parents. Overall, 18.8% of participants reported using any alcohol (26.6% among males and 17.2% among females).
HIV disclosure to family members was reported by 74.9% of participants and did not differ by gender. Disclosure of HIV status to partners was lower at 50.8% and differed by gender with 29% for males and 55.2% for females. Disclosure of HIV to status to friends was still lower overall (32.3%) and also differed by gender with 39.6% for males and 30.8% for females.
ART status at enrollment
The majority of participants, 816 (82%), had already started ART prior to enrollment, and 179 (18%) started at enrollment (). Of those who had already started ART, 598 (73%) had been on ART for ≥ 6 months, among which 36 participants (6%) had been out of HIV care for more than 6 months and were re-engaging at the time of study entry. ART status at enrollment did not differ significantly by gender.
Recent significant life-events
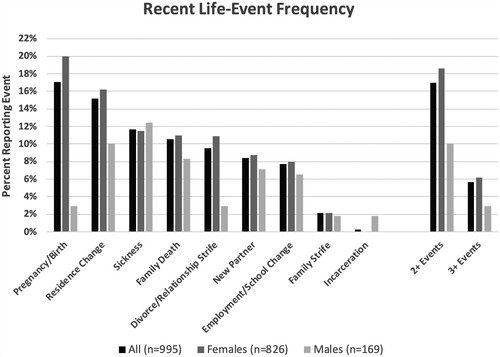
Overall, the percentage of participants reporting at least one recent significant life-event at baseline was 57.7% (95% CI:54.5%–60.8%). Females were significantly more likely to report having any recent major life-event (61.4%, 95% CI:58.0%–64.7%) than males (39.6%, 95% CI:32.2%–47.4%, p < 0.001). shows the frequency of recent major life-events overall and by gender. Overall, the most common life-events were pregnancy or childbirth (17.1%) and change in residence (15.2%), followed by sickness (11.7%), death within the family (10.6%), relationship strife (9.5%), change in sexual partner (8.4%), change in school or employment (7.7%), family strife (2.1%), and incarceration (<1%). The frequency of certain life-events varied by sex. A significantly higher proportion of females than males reported experiencing pregnancy/childbirth (p < 0.001), residence change (p = 0.04), relationship strife (p = 0.001), while males more frequently reported incarceration (p < 0.001).
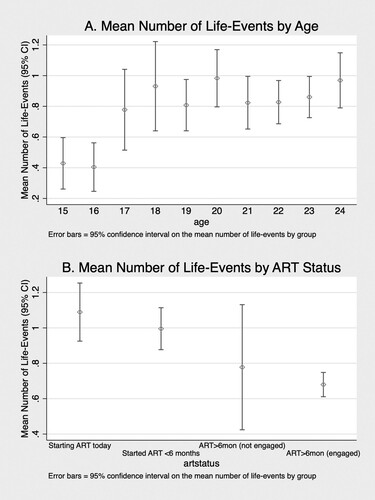
Two or more significant life-events in the prior 6-months (at baseline) were reported by 171 (17.2%) participants with 56 (5.6%) reporting three or more recent major life-events. Two or more recent life-events were significantly more common among females (18.6%) than among males (10.1%, p = 0.007). The maximum number of life-events was 5, reported by 5 participants (0.5%). The average number of recent life-events was .83 and was significantly higher for females 0.88 than for males 0.54 (p < .001).
shows the average number of reported life-events by age and by ART status. As expected, older participants were more likely to have experienced recent major life-events (P < .001 for trend). The average number of life-events was significantly higher for those starting ART at baseline and those who had started ART < 6 months prior, compared to those with engaged in HIV care and on ART for ≥ 6 months at baseline study entry (P < 0.001 for both). An elevated average number of recent life-events was seen for those who had started ART ≥ 6 months prior to baseline but who had dropped out of care (not engaged in HIV care, n = 36) compared to those with ≥ 6 months of ART who were engaged in HIV care, but the difference was not meaningfully different.
Association of recent life-Events, ART engagement, and HIV viral suppression
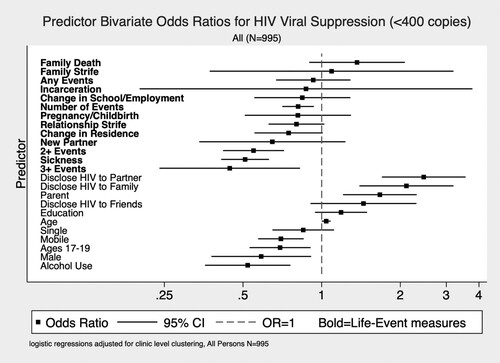
Bivariate odds ratios (OR) for baseline HIV viral suppression (HIV copy number <400) with recent life-events and participant characteristics are shown in . The number of life-events was strongly predictive of viral non-suppression. For each additional recent life-event, the odds of viral suppression were 0.81-times lower (95%CI: 0.71–0.93, p < 0.003). Likewise, having 2 or more recent life-events and having 3 or more recent life-events were associated with 0.55-times lower (95% CI: 0.42–0.72, p < 0.001) and 0.44-times lower (95% CI: 0.24–0.84, p = .01) odds of suppression, respectively. Personal sickness also predicted lower odds of viral suppression (OR = 0.51, 95% CI: 0.41–0.63, p < 0.001). Additionally, being male (OR = 0.59, 95% CI:0.38–0.91, p = 0.18), having a history of mobility (OR = 0.7, 95% CI:0.57–0.85, p < 0.001), consuming alcohol (OR = 0.52, 95% CI:0.36–0.8, p = 0.001), and being aged 17–19 years (OR = 0.69, 95% CI:0.53–0.91, p = 0.008) were associated with a reduced odds of HIV viral suppression. Conversely, having disclosed HIV status to a partner as opposed to not disclosing to a partner (OR = 2.5, 95% CI:1.7–3.6, p < 0.001), disclosed to family (OR = 2.1, 95% CI:1.4–3.2, p < 0.001), and being a parent (OR = 1.7, 95% CI:1.2–2.3, p = 0.002) were associated with an increased odds of HIV viral suppression.
Unsurprisingly, HIV viral suppression was significantly associated with ART status at study baseline with the lower odds of HIV viral suppression seen for those just starting ART at study entry (OR = 0.6, 95% CI:0.03–0.10, p < 0.001), those on ART < 6 months (OR = 0.35, 95% CI:0.23–0.55, p < 0.001), and those on ART for ≥ 6 months but not engaged in HIV care (OR = 0.09, 95% CI:0.05–0.18, p < 0.001), as compared to those on ART for ≥ 6 months and engaged in HIV care.
In multivariable analyses, significant adjusted associations with HIV viral suppression at study baseline were seen for having 2 or more recent life-events (aOR = 0.61, 95% CI:0.45–0.85, p = 0.003) and consuming alcohol (aOR = 0.61, 95% CI:0.43–0.87, p = 0.007) indicating a reduced odds of viral suppression, and disclosure of HIV status to partner (aOR = 2.39, 95% CI:1.6–3.5, p < 0.001), disclosure to family (aOR = 1.86, 95% CI:1.3–2.7, p = 0.002), being a parent (aOR = 1.8, 95% CI:1.2–2.5, p = 0.003), and being single (aOR = 1.6, 95% CI:1.3–2.1, p < 0.001) indicating an increased odds of viral suppression as shown in A (all significant variables shown and adjusted for each other in the model).
Table 2. Multivariable predictors of HIV viral suppression among (A) All participants, (B) HIV viral suppression among participants on ART for 6+ months and engaged in HIV care, and (C) Being on ART for 6+ months at study baseline.
In a sub-group analysis among participants on ART for ≥ 6 months and who were engaged in HIV care, we did not see significant multivariable associations between HIV viral suppression and any measures of recent life-events (B). Nonetheless, among this subgroup, being aged 17–19 years was associated with lower odds of suppression (aOR = 0.52, 95% CI:0.35–0.79, p < 0.002) than being in other age groups. Furthermore, disclosure of HIV status to their partner was associated with higher odds of suppression (aOR = 2.66, 95% CI:1.96–3.61, p < 0.001).
To further understand the observed association between recent life-events and HIV viral suppression, we examined whether recent life-events were associated with being on ART for 6 or more months (regardless of HIV care engagement). In multivariable analysis we saw a significant association between having 2 or more recent life-events (aOR = 0.46, 95% CI:0.36–0.57, p < 0.001) and consuming alcohol (aOR = 0.44, 95% CI:0.31–0.64, p < 0.001) (reduced odds of having an ART duration ≥ 6 months at baseline), and disclosure of HIV status to family (aOR = 3.21, 95% CI:2.25–4.57,p < 0.001), disclosure to friends (aOR = 1.45, 95% CI:1.19–1.77,p < 0.001), and being single (aOR = 1.55, 95% CI:1.07–2.25, p = 0.021) (increased odds of ART duration >6 months at baseline), see C.
Discussion
Among 995 youth ages 15–24 years old living with HIV in rural Kenya and Uganda we found that recent significant life-events were common. In multivariable analyses, having two or more recent life-events and the use of alcohol were associated with lower odds of HIV viral suppression, while being a parent, single, and having disclosed HIV status to partners or family were associated with higher odds of suppression. In subgroup analysis restricted to those on ART for ≥ 6 months and engaged in HIV care, life-events were no longer associated with suppression; however, having two or more recent significant life-events and alcohol use were associated with lower odds of starting ART ≥ 6 months prior while being single and having disclosed HIV status to family or friends were associated with higher odds of virologic suppression. Taken together, these results suggest that the lower odds of HIV viral suppression associated with two or more recent life-events and alcohol use is driven by challenges in linkage to HIV care and initiation of ART.
Youth living with HIV are a not homogenous group with some acquiring HIV perinatally and others through sexual transmission in early adolescence and young adulthood and this diverse group represents different vulnerabilities and life course experiences (Bekker & Hosek, Citation2015; Foundation, Citation2020; Sherr et al., Citation2018). Between the ages of 10–24 years youth go through distinct series of life stages and milestone life-events like pregnancy or child birth and the formation of lifelong habits including alcohol and substance use that can modulate response to HIV care seeking and treatment (Sawyer et al., Citation2012).
Life-events were common in our study with 39.6% and 61.4% males and females, respectively, reporting at least one significant life-event within the last 6 months. Pregnancy or childbirth (17.1%) as well as change in residence (15.2%) were most prevalent. The majority of the study’s participants were female reflecting the gendered nature of the youth HIV epidemic in Sub-Saharan Africa (HIV/AIDS, Citation2018). Women in East Africa marry early and nearly fifty-percent become mothers before the age of twenty (HIV/AIDS, Citation2018). Early marriage or sexual activity increases the risk for acquiring HIV, and young women who often are in age-disparate relationships may not easily access HIV care because of a lack of negotiating ability in such relations (Neal et al., Citation2015; Schaefer et al., Citation2017; Worku et al., Citation2021). Observed differences prevalence of life-events between males and females and the odds of HIV viral suppression by sex warrant further examination in subsequent larger studies.
The impact of significant life-events on health has been studied outside of sub-Saharan Africa among adults, adolescents, and children with stressful and other significant life-events and reported to be associated with health-related quality of life, (Coker et al., Citation2011; O'Donnell et al., Citation2017; Villalonga-Olives et al., Citation2010) cancer, and infectious diseases (Cohen et al., Citation2019). Specific to HIV patients in the west, relationships with significant life-events have been reported to be associated with increased HIV risk taking behaviors, (Pence et al., Citation2010) depression and anxiety, (Glynn et al., Citation2019; Murphy et al., Citation2000; Wong et al., Citation2007) hospital utilization, (Elliott-DeSorbo et al., Citation2009; Leserman et al., Citation2005) and non-adherence to ART medications (Duggal et al., Citation2000; Leserman et al., Citation2008; Mugavero et al., Citation2009; O'Donnell et al., Citation2017).
Our study adds unique data to the literature on the impacts of recent significant life-events on the likelihood of ART initiation and HIV viral suppression among youth ages 15–24 years living with HIV in rural East Africa. Our finding of the high prevalence of two or more recent significant life-events and their adverse association with HIV viral suppression and ART engagement points to the importance of considering developmental life-stages and trajectory in the care and optimization of treatment outcomes for youth living with HIV.
Our additional finding that alcohol use is associated with lower odds of HIV viral suppression and ART engagement of ≥ 6 months are in consistent with prior literature (Hendershot et al., Citation2009). Alcohol consumption is very common in Africa with up to 43% of the adult population reporting alcohol use (Ferreira-Borges et al., Citation2017) and has been associated with poor treatment-seeking behaviors and adherence as well as HIV care outcomes among African adults and key populations (Brown, Getahun, et al., Citation2019; Fatch et al., Citation2017; Kiwanuka et al., Citation2017; Patsis et al., Citation2020; Puryear et al., Citation2020; Santos et al., Citation2014; UNAIDS, Citation2016; Vagenas et al., Citation2015).
Our study also found that disclosure of HIV status was associated with higher odds of HIV viral suppression and ART engagement with the strongest association for disclosure to family members. HIV status disclosure to family, peers and partners is one of the most challenging transitions young people living with HIV have to make (Foundation, Citation2020; Lowenthal et al., Citation2014; Maeri et al., Citation2016; Ministry of Health, Citation2019; Siu et al., Citation2012). In our study, we found high levels of HIV disclosure to family members among both men and. The fact that disclosure to family and partners was independently associated with higher odds of HIV viral suppression and ART engagement suggests in our data suggests that support youth derive from their close social network can buttress against the disruption of major life-events.
Limitations
This study has several limitations. First, this was a cross-sectional analysis of youth and therefore, we can only investigate associations and not evaluate causality. Nonetheless, because of the paucity of information on the relationship between significant life-events and HIV viral suppression and ART engagement among youth living with HIV, a cross-sectional analysis is justified prior to a more comprehensive longitudinal investigation. Second, self-report of recent life-events may have been subject to both social-desirability bias and recall bias on the part of participants. To minimize such bias, all providers were trained on non-judgmental interviewing and the structured checklist was designed to reduce variability in data collection. Given the significant nature of the life-events under study (pregnancy/childbirth, deaths, moves, etc.) Along with the short assessment period (within the last 6 months), recall bias was expected to be minimal. Third, we were unable to directly include ART adherence in our models and empirically describe the pathway between life-events and viral suppression This inclusion was challenged by the heterogeneity of ART engagement among the sample (a mixture of participants on ART, never on ART, and discontinued ART at baseline) and our hypothesis that ART engagement (including starting ART and adherence to medication) is on the causal pathway between life-events and HIV viral suppression. Finally, the study sample size limited our ability to examine the significance of potential gender differences.
Conclusions
From this analysis of youth ages 15–24 years living with HIV in rural Kenya and Uganda, we conclude that recent significant life-events are very common for youth engaged in or about to engage in HIV care. Having 2 or more recent significant life-events and the use of alcohol were associated with lower odds of HIV viral suppression. This relationship appears to be primarily driven by upstream challenges to linkage to HIV care and initiation of ART. Altogether our results suggest that HIV treatment engagement and HIV viral suppression could be optimized for youth by including a regular inquiry about significant life-events and alcohol use and providing adaptations to care to overcome identified challenges. These findings support the UNAIDS call for a life course approach to HIV care for all people living with HIV and especially youth (UNAIDS, Citation2016).
Sponsor conflict of interest
This sponsor (NICHD) had no role in the if any, in the study design, the collection, analysis, and interpretation of data, the writing of the report; and the decision to submit the manuscript for publication.
Author confirmation statement
All author confirm that they meet the criteria for authorship, as defined by the International Committee of Medical Journal Editors.
Author contributions
All authors contributed to design of this analysis and reviewed manuscript.
FM, EC, TR drafted the manuscript; EC performed the statistical analysis.
Acknowledgements
Authors would like to thank the sponsor, study team and participants. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, TR, upon reasonable request.
Additional information
Funding
References
- Arnett, J. J. (2014). Presidential address: The emergence of emerging adulthood. Emerging Adulthood, 2(3), 155–162. https://doi.org/10.1177/2167696814541096
- Bekker, L.-G., & Hosek, S. (2015). HIV and adolescents: Focus on young key populations. Journal of the International AIDS Society, 18(2Suppl 1), 20076. https://doi.org/10.7448/IAS.18.2.20076
- Brown, L. B., Getahun, M., Ayieko, J., Kwarisiima, D., Owaraganise, A., Atukunda, M., Olilo, W., Clark, T., Bukusi, E. A., Cohen, C. R., Kamya, M. R., Petersen, M. L., Charlebois, E. D., Havlir, D. V., Madiba, S., & Camlin, C. S. (2019). Factors predictive of successful retention in care among HIV-infected men in a universal test-and-treat setting in Uganda and Kenya: A mixed methods analysis. PloS One, 14(1), e0210126. https://doi.org/10.1371/journal.pone.0210126
- Brown, M. J., Harrison, S. E., & Li, X. (2019). Gender disparities in traumatic life experiences and antiretroviral therapy adherence Among people living with HIV in South Carolina. AIDS and Behavior, 23(11), 2904–2915. https://doi.org/10.1007/s10461-019-02440-9
- Chamie, G., Clark, T. D., Kabami, J., Kadede, K., Ssemmondo, E., Steinfeld, R., Lavoy, G., Kwarisiima, D., Sang, N., Jain, V., Thirumurthy, H., Liegler, T., Balzer, L. B., Petersen, M. L., Cohen, C. R., Bukusi, E. A., Kamya, M. R., Havlir, D. V., & Charlebois, E. D. (2016). A hybrid mobile approach for population-wide HIV testing in rural east Africa: An observational study. The Lancet HIV, 3(3), e111–e119. https://doi.org/10.1016/S2352-3018(15)00251-9
- Cohen, S., Murphy, M. L. M., & Prather, A. A. (2019). Ten surprising facts about stressful life events and disease risk. Annual Review of Psychology, 70(1), 577–597. https://doi.org/10.1146/annurev-psych-010418-102857
- Coker, T. R., Elliott, M. N., Wallander, J. L., Cuccaro, P., Grunbaum, J. A., Corona, R., Saunders, A. E., & Schuster, M. A. (2011). Association of family stressful life-change events and health-related quality of life in fifth-grade children. Archives of Pediatrics and Adolescent Medicine, 165(4), 354–359. https://doi.org/10.1001/archpediatrics.2011.13
- Duggal, S., Malkoff-Schwartz, S., Birmaher, B., Anderson, B. P., Matty, M. K., Houck, P. R., Bailey-Orr, M., Williamson, D. E., & Frank, E. (2000). Assessment of life stress in adolescents: Self-report versus interview methods. Journal of the American Academy of Child and Adolescent Psychiatry, 39(4), 445–452. https://doi.org/10.1097/00004583-200004000-00013
- Elliott-DeSorbo, D. K., Martin, S., & Wolters, P. L. (2009). Stressful life events and their relationship to psychological and medical functioning in children and adolescents with HIV infection. JAIDS Journal of Acquired Immune Deficiency Syndromes, 52(3), 364–370. https://doi.org/10.1097/QAI.0b013e3181b73568
- Fatch, R., Emenyonu, N. I., Muyindike, W., Kekibiina, A., Woolf-King, S., & Hahn, J. A. (2017). Alcohol interactive toxicity beliefs and ART Non-adherence among HIV-infected current drinkers in Mbarara, Uganda. AIDS and Behavior, 21(7), 1812–1824. https://doi.org/10.1007/s10461-016-1429-3
- Fatusi, A. O., & Hindin, M. J. (2010). Adolescents and youth in developing countries: Health and development issues in context. Journal of Adolescence, 33(4), 499–508. https://doi.org/10.1016/j.adolescence.2010.05.019
- Ferreira-Borges, C., Parry, C. D. H., & Babor, T. F. (2017). Harmful Use of alcohol: A shadow over Sub-Saharan Africa in need of workable solutions. International Journal of Environmental Research and Public Health, 14(4), 4. https://doi.org/10.3390/ijerph14040346
- Filiatreau, L. M., Pettifor, A., Edwards, J. K., Masilela, N., Twine, R., Xavier Gomez-Olive, F., Xavier Gómez-Olivé, F., Haberland, N., Kabudula, C. W., Lippman, S. A., & Kahn, K. (2021). Associations between key psychosocial stressors and viral suppression and retention in care among youth with HIV in rural South Africa. AIDS and Behavior, 25(8), 2358–2368. https://doi.org/10.1007/s10461-021-03198-9
- Foundation, E. G. P. A. (2020). AIDS free generation Z: A call to action for improving youth-focused HIV programming. https://www.pedaids.org/wp-content/uploads/2020/07/2020YouthReport_0706.pdf
- Glynn, T. R., Llabre, M. M., Lee, J. S., Bedoya, C. A., Pinkston, M. M., O'Cleirigh, C., & Safren, S. A. (2019). Pathways to health: An examination of HIV-related stigma, life stressors, depression, and substance Use. International Journal of Behavioral Medicine, 26(3), 286–296. https://doi.org/10.1007/s12529-019-09786-3
- Guan, K., Park, A. L., & Chorpita, B. F. (2019). Emergent life events during youth evidence-based treatment: Impact on future provider adherence and clinical progress. Journal of Clinical Child & Adolescent Psychology, 48(sup1), S202–S214. https://doi.org/10.1080/15374416.2017.1295382
- Hendershot, C. S., Stoner, S. A., Pantalone, D. W., & Simoni, J. M. (2009). Alcohol use and antiretroviral adherence: Review and meta-analysis. JAIDS Journal of Acquired Immune Deficiency Syndromes, 52(2), 180–202. https://doi.org/10.1097/QAI.0b013e3181b18b6e
- HIV/AIDS, U. J. U. N. P. o. (2018). Women and Girls and HIV. https://www.unaids.org/sites/default/files/media_asset/women_girls_hiv_en.pdf
- Kiwanuka, N., Ssetaala, A., Ssekandi, I., Nalutaaya, A., Kitandwe, P. K., Ssempiira, J., Bagaya, B. S., Balyegisawa, A., Kaleebu, P., Hahn, J., Lindan, C., Braitstein, P., & Sewankambo, N. K. (2017). Population attributable fraction of incident HIV infections associated with alcohol consumption in fishing communities around lake Victoria, Uganda. PloS One, 12(2), e0171200. https://doi.org/10.1371/journal.pone.0171200
- Leserman, J., Ironson, G., O'Cleirigh, C., Fordiani, J. M., & Balbin, E. (2008). Stressful life events and adherence in HIV. AIDS Patient Care and STDs, 22(5), 403–411. https://doi.org/10.1089/apc.2007.0175
- Leserman, J., Whetten, K., Lowe, K., Stangl, D., Swartz, M. S., & Thielman, N. M. (2005). How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosomatic Medicine, 67(3), 500–507. https://doi.org/10.1097/01.psy.0000160459.78182.d9
- Lowenthal, E. D., Bakeera-Kitaka, S., Marukutira, T., Chapman, J., Goldrath, K., & Ferrand, R. A. (2014). Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: A review of emerging challenges. The Lancet Infectious Diseases, 14(7), 627–639. https://doi.org/10.1016/s1473-3099(13)70363-3
- Maeri, I., El Ayadi, A., Getahun, M., Charlebois, E., Akatukwasa, C., Tumwebaze, D., Itiakorit, H., Owino, L., Kwarisiima, D., Ssemmondo, E., Sang, N., Kabami, J., Clark, T. D., Petersen, M., Cohen, C. R., Bukusi, E. A., Kamya, M., Havlir, D., Camlin, C. S., & Collaboration, S. (2016). How can I tell?” consequences of HIV status disclosure among couples in eastern African communities in the context of an ongoing HIV “test-and-treat” trial. AIDS Care, 28(Suppl 3), 59–66. https://doi.org/10.1080/09540121.2016.1168917
- Ministry of Health, U. (2019). Uganda Population-based HIV Impact Assessment (UPHIA) 2016-2017: Final Report. https://phia.icap.columbia.edu/wp-content/uploads/2019/07/UPHIA_Final_Report_Revise_07.11.2019_Final_for-web.pdf
- Mugavero, M. J., Raper, J. L., Reif, S., Whetten, K., Leserman, J., Thielman, N. M., & Pence, B. W. (2009). Overload: Impact of incident stressful events on antiretroviral medication adherence and virologic failure in a longitudinal, multisite human immunodeficiency virus cohort study. Psychosomatic Medicine, 71(9), 920–926. https://doi.org/10.1097/PSY.0b013e3181bfe8d2
- Murphy, D. A., Moscicki, A. B., Vermund, S. H., & Muenz, L. R. (2000). Psychological distress among HIV(+) adolescents in the REACH study: Effects of life stress, social support, and coping. The adolescent medicine HIV/AIDS research network. Journal of Adolescent Health, 27(6), 391–398. https://doi.org/10.1016/S1054-139X(00)00158-0
- Nachega, J. B., Sam-Agudu, N. A., Mofenson, L. M., Schechter, M., & Mellors, J. W. (2018). Achieving viral suppression in 90% of people living with human immunodeficiency virus on antiretroviral therapy in Low- and middle-income countries: Progress, challenges, and opportunities. Clinical Infectious Diseases, 66(10), 1487–1491. https://doi.org/10.1093/cid/ciy008
- Neal, S. E., Chandra-Mouli, V., & Chou, D. (2015). Adolescent first births in East Africa: Disaggregating characteristics, trends and determinants. Reproductive Health, 12(1), 13. https://doi.org/10.1186/1742-4755-12-13
- O'Donnell, J. K., Gaynes, B. N., Cole, S. R., Edmonds, A., Thielman, N. M., Quinlivan, E. B., O’Donnell, J. K., Heine, A., Modi, R., & Pence, B. W. (2017). Stressful and traumatic life events as disruptors to antiretroviral therapy adherence. AIDS Care, 29(11), 1378–1385. https://doi.org/10.1080/09540121.2017.1307919
- Oren, E., Gerald, L., Stern, D. A., Martinez, F. D., & Wright, A. L. (2017). Self-Reported stressful life events during adolescence and subsequent asthma: A longitudinal study. Journal of Allergy and Clinical Immunology: In Practice, 5(2), 427–434. https://doi.org/10.1016/j.jaip.2016.09.019. e422.
- Patsis, I., Goodrich, S., Yiannoutsos, C. T., Brown, S. A., Musick, B. S., Diero, L., Kulzer, J. L., Bwana, M. B., Oyaro, P., Francis, J. M., & Wools-Kaloustian, K. K. (2020). Lower rates of ART initiation and decreased retention among ART-naïve patients who consume alcohol enrolling in HIV care and treatment programs in Kenya and Uganda. PLoS One, 15(10), e0240654. https://doi.org/10.1371/journal.pone.0240654
- Peer, N., Lombard, C., Steyn, K., & Levitt, N. (2020). A high burden of adverse life events and poor coping mechanisms experienced by urban-dwelling black South Africans. PLoS One, 15(9), e0238320. https://doi.org/10.1371/journal.pone.0238320
- Pence, B. W., Raper, J. L., Reif, S., Thielman, N. M., Leserman, J., & Mugavero, M. J. (2010). Incident stressful and traumatic life events and human immunodeficiency virus sexual transmission risk behaviors in a longitudinal, multisite cohort study. Psychosomatic Medicine, 72(7), 720–726. https://doi.org/10.1097/PSY.0b013e3181e9eef3
- Petersen, M., Balzer, L., Kwarsiima, D., Sang, N., Chamie, G., Ayieko, J., Kabami, J., Owaraganise, A., Liegler, T., Mwangwa, F., Kadede, K., Jain, V., Plenty, A., Brown, L., Lavoy, G., Schwab, J., Black, D., van der Laan, M., Bukusi, E. A., … Havlir, D. (2017). Association of implementation of a universal testing and treatment intervention with HIV diagnosis, receipt of antiretroviral therapy, and viral suppression in east Africa. JAMA - Journal of the American Medical Association, 317(21), 2196–2206. https://doi.org/10.1001/jama.2017.5705
- Puryear, S. B., Balzer, L. B., Ayieko, J., Kwarisiima, D., Hahn, J. A., Charlebois, E. D., Clark, T. D., Cohen, C. R., Bukusi, E. A., Kamya, M. R., Petersen, M. L., Havlir, D. V., & Chamie, G. (2020). Associations between alcohol use and HIV care cascade outcomes among adults undergoing population-based HIV testing in east Africa. AIDS (London, England), 34(3), 405–413. https://doi.org/10.1097/QAD.0000000000002427
- Santos, G. M., Emenyonu, N. I., Bajunirwe, F., Rain Mocello, A., Martin, J. N., Vittinghoff, E., Bangsberg, D. R., & Hahn, J. A. (2014). Self-reported alcohol abstinence associated with ART initiation among HIV-infected persons in rural Uganda. Drug and Alcohol Dependence, 134, 151–157. https://doi.org/10.1016/j.drugalcdep.2013.09.025
- Sawyer, S. M., Afifi, R. A., Bearinger, L. H., Blakemore, S.-J., Dick, B., Ezeh, A. C., & Patton, G. C. (2012). Adolescence: A foundation for future health. The Lancet, 379(9826), 1630–1640. https://doi.org/10.1016/S0140-6736(12)60072-5
- Schaefer, R., Gregson, S., Eaton, J. W., Mugurungi, O., Rhead, R., Takaruza, A., Maswera, R., & Nyamukapa, C. (2017). Age-disparate relationships and HIV incidence in adolescent girls and young women: Evidence from Zimbabwe. AIDS (London, England), 31(10), 1461–1470. https://doi.org/10.1097/QAD.0000000000001506
- Sherr, L., Cluver, L. D., Toska, E., & He, E. (2018). Differing psychological vulnerabilities among behaviourally and perinatally HIV infected adolescents in South Africa – Implications for targeted health service provision. AIDS Care, 30(sup2), 92–101. https://doi.org/10.1080/09540121.2018.1476664
- Siu, G. E., Bakeera-Kitaka, S., Kennedy, C. E., Dhabangi, A., & Kambugu, A. (2012). HIV serostatus disclosure and lived experiences of adolescents at the transition clinic of the infectious diseases clinic in Kampala, Uganda: A qualitative study. AIDS Care, 24(5), 606–611. https://doi.org/10.1080/09540121.2011.630346
- UNAIDS. (2016). Get on the fast-track: The life-cycle approach to HIV. Geneva, Switzerland. https://www.unaids.org/sites/default/files/media_asset/Get-on-the-Fast-Track_en.pdf
- UNAIDS. (2019). 2019-global-AIDS-update. Retrieved from Communities at the Centre.
- UNAIDS. (2020). Seizing the moment. Global AIDS update 2020. Retrieved from Unaids: https://www.unaids.org/sites/default/files/media_asset/2020_%0Aglobal-aids-report_en.pdf
- Vagenas, P., Azar, M. M., Copenhaver, M. M., Springer, S. A., Molina, P. E., & Altice, F. L. (2015). The impact of alcohol Use and related disorders on the HIV continuum of care: A systematic review: Alcohol and the HIV continuum of care. Current HIV/AIDS Reports, 12(4), 421–436. https://doi.org/10.1007/s11904-015-0285-5
- Villalonga-Olives, E., Rojas-Farreras, S., Vilagut, G., Palacio-Vieira, J. A., Valderas, J. M., Herdman, M., Ferrer, M., Rajmil, L., & Alonso, J. (2010). Impact of recent life events on the health related quality of life of adolescents and youths: The role of gender and life events typologies in a follow-up study. Health and Quality of Life Outcomes, 8(1), 71. https://doi.org/10.1186/1477-7525-8-71
- Walders-Abramson, N., Venditti, E. M., Ievers-Landis, C. E., Anderson, B., El Ghormli, L., Geffner, M., Kaplan, J., Koontz, M. B., Saletsky, R., Payan, M., Yasuda, P., & Youth Study, s. (2014). Relationships among stressful life events and physiological markers, treatment adherence, and psychosocial functioning among youth with type 2 diabetes. The Journal of Pediatrics, 165(3), 504–508. https://doi.org/10.1016/j.jpeds.2014.05.020. e501.
- Williams, P. L., Storm, D., Montepiedra, G., Nichols, S., Kammerer, B., Sirois, P. A., Farley, J., Malee, K., & Team, P. C. (2006). Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics, 118(6), e1745–e1757. https://doi.org/10.1542/peds.2006-0493
- Wong, M. D., Sarkisian, C. A., Davis, C., Kinsler, J., & Cunningham, W. E. (2007). The association between life chaos, health care use, and health status among HIV-infected persons. Journal of General Internal Medicine, 22(9), 1286–1291. https://doi.org/10.1007/s11606-007-0265-6
- Worku, M. G., Tessema, Z. T., Teshale, A. B., Tesema, G. A., & Yeshaw, Y. (2021). Prevalence and associated factors of adolescent pregnancy (15-19 years) in East Africa: A multilevel analysis. BMC Pregnancy and Childbirth, 21(1), 253. https://doi.org/10.1186/s12884-021-03713-9