ABSTRACT
HIV prevalence has increased continuously, and the age groups most afflicted by the epidemic have also shifted to people aged above 50 years. Informed by the theory of HBM, we aimed to investigate related factors associated with regular HIV testing behavior. Cross-sectional data were collected using online questionnaire from geosocial networking (GSN) mobile application (apps) for MSM during May 2020 (N = 1259). Data were analyzed by univariate and multivariate logistic regression. Around 62.0% (n = 781) had received HIV testing before. Participants being divorced/widowed (AOR = 1.5,95%CI:1.1–2.0), being aware of HIV/AIDS-related knowledge (AOR = 1.8,95%CI:1.4–2.3), having disclosed sexual orientation (AOR = 1.9,95%CI:1.5–2.5), ever had sexually transmitted infections symptoms (STIs)before (AOR = 2.4,95%CI:1.8–3.2), having had≥2 sexual partners (AOR = 1.8,95%CI:1.4–2.3) and with high self-efficacy (AOR = 1.1,95%CI:1.0–1.1) were more likely to receive HIV testing. Findings suggest that many Chinses MSM aged 50 and above have not been tested for HIV. Interventions for promoting HIV testing should focus on expanding scales of HIV/STIs screening, providing HIV/AIDS-related knowledge, creating a more supportive social environment and improving self-efficacy of HIV testing.
KEYWORDS:
Introduction
Recent reports suggest that the number of HIV prevalence among men who have sex with men (MSM) aged 50 and above is increasing, the rate has increased from 1.6% to 13.6% over the period of 2000–2011 (Chen et al., Citation2019).
The prevalence of HIV in the elderly MSM group was higher than that in the young group (Dong et al., Citation2019), but the HIV testing rate was lower than in the young age group (Dalrymple et al., Citation2019). The older MSM was proved to be more vulnerable to HIV than young MSM due to a lack of HIV/AIDS-related knowledge (Dalrymple et al., Citation2019; Dowson et al., Citation2012; Stannah et al., Citation2019). Furthermore, because of the difference in lifestyle, the older populations potentially have different social and clinical needs than young age groups.
HIV testing service is the primary component of HIV treatment and prevention strategies. According to WHO, sexual active MSM should receive HIV testing annually, and for persons with multiple risk factors should be tested more frequently (Sexually Transmitted Diseases Treatment Guidelines, Citation2006). However relevant research reported that only 62.3% MSM aged 50 and above have ever tested lifetime (Ning et al., Citation2018). And there are limited studies focused on HIV testing among MSM aged 50 and above in China. This study aims to estimate the HIV testing rates and identify related factors, hence to promote accessibility and motivation for HIV testing among Chinese MSM aged 50 and above.
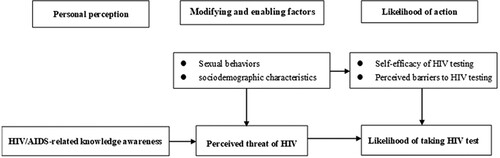
The study was guided by the Health Belief Model (HBM), which explains the relationship between health behaviors and service utilization. The model contains six domains: perceived susceptibility, perceived severity, perceived barriers to taking actions, perceived benefits to taking actions, self-efficacy and cues to action (Rosenstock et al., Citation1988). George Chidi Anwuri ever used HBM to explore the determinants of Voluntary HIV Counseling and Testing among Community College Students in the USA. The results of study underscore the important factors that predict intention to screen for HIV among college students. (Anwuri et al., Citation2017).
illustrates the HBM model and showed how study variables fit into the model (modified from Kabiru et al. (Citation2011)).
Methods
Study design and population
This study was a cross-sectional survey using online convenience sampling during May 2020. We recruited participants from Blued in China by sending study advertisements to users age 50 and above nationwide. Blued is the largest MSM GSN app worldwide, with over 40 million users, especially in the Asia–Pacific region. After reading the advertisement, interested MSM was taken to an internet-based survey webpage. Before the formal questionnaire survey, participants had to fill in an online informed consent and eligibility screening. Eligibility criteria included being biologically male, 50 years and older, and having oral or anal sex with men in the last year. Ethical approval was granted by the Institutional Review Board of Jining Medical College. We sent recruitment messages to 100,000 registered users, and 2411 of them accomplished the questionnaire. Fourour conflicting descriptive questions were used as a quality test. After quality control, the final sample size was 1259.
Measures
Explanatory factors
Based on the HBM framework, potential predictors of HIV testing focused on: HIV/AIDS-related knowledge, perceived barriers, self-efficacy and modifying/enabling factors.
HIV/AIDS-related knowledge was measured by eight items routinely used in national HIV sentinel surveillance among Chinese MSM. Participants who correctly answered six items or above were considered being aware of HIV/AIDS-related knowledge.
Lack of social support, depression and HIV-related stigma were considered to be barriers to HIV testing. Social support was measured by two items (Li et al., Citation2017). Responses were rated on scales that from 0 (“none”) to 10 (“tremendous”), the total score ranged from 0 to 20, 0 indicated they can’t obtain support (Cronbach’s α = 0.68). Depression was measured with The Chinese version 10-item CES-D depression scales (Yu et al., Citation2013). Scores of the CES-D 10 ranged from 0 to 30, participants with a score above 20 were classified as having moderate-to-severe depression (Cronbach’s α = 0.86). Anticipated HIV stigma was assessed by a 7-item scale (Golub & Gamarel, Citation2013). All the items were rated on a 4-point Likert scale ranging from 1 (“strongly disagree”) to 4 (“strongly agree”). The mean score is the average score of seven items ranging from 1 to 4, high score indicated a high level of stigma (Cronbach’s α = 0.78).
Self efficacy was measured with 6-item scale (Zhao et al., Citation2018). All items were rated by 4-point Likert-type response options ranged from 1 (“strongly disagree”) to 4 (“strongly agree”). For each participant, a mean score was calculated with 4 as the highest possible score and 1 as the possible lowest score. High scores indicated high HIV testing self-efficacy (Cronbach’s α = 0.88).
The dimensions of modifying and enabling factors included sexual behaviors and socio-demographic characteristics. Sexual behaviors including disclosure of sexual orientation to the Health-Care Providers, number of sexual partners in previous year, ever had STIs before and substance use. Socio-demopgraphics include age, race, marital stuatu, education, employment and sexual orientation.
Outcome variable
Participants’ HIV testing status was based on the response to the question, “have you ever received HIV testing before?”(0 = no,1 = yes).
Statistical analysis
Descriptive analyses were performed to examine the numbers and frequencies of socio-demographics, history of substance use and ever had STIs before, the number of sexual partners, HIV/AIDS-related knowledge, social support, depression and HIV testing behaviors. Means, median, IQR and standard deviations were used to describe variables such as anticipated HIV stigma and self-efficacy. Multivariate logistic regression was used to analyze factors related to HIV testing behaviors. All data were analyzed by SPSS 21, the dependent variable is HIV testing status, and the independent variables are explanatory factors. The significance level is 0.05.
Results
62.0% (781) had received HIV testing among the participants. HIV testing rate (times≥1) is 43.2% (544) in the previous year. Most of the participants (81.7%, n = 1029) were 50–59 years old, 95.2% (n = 1198) were Han ethnicity, 65.1% (n = 820) were married, 76.9% (n = 968) had a senior high school degree or above and 70.0% (n = 881) were currently employed. More than half of the participants (63.6%,n = 801) were self-identified as gay, and 37.1% (n = 467) had disclosed their sexual orientation. Meanwhile, 61.7% (n = 777) reported≥2 sexual partners, 29.5% (n = 372) reported ever had STIs symptoms before and 22.1% (n = 278) reported a history of ever using substances, 70.3% (n = 885) were aware of HIV/AIDS-related knowledge, 42.7% (n = 538) reported that they couldn’t obtain support and 12.3% (n = 155) experienced moderate-to-severe depression symptoms. In addition, the median score of anticipated HIV stigma was 3.1 (IQR 2.7–3.6), the mean of self-efficacy was 17.6 (S.D. = 4.4)().
Table 1. Characteristics of the participants and univariate analysis on HIVtesting (n = 1259).
In addition, reporting being divorced/widowed, self-identified as gay, being aware of HIV/AIDS-related knowledge, higher level of social support, ever had STIs before and substances use, disclosure of sexual orientation,≥2 sexual partners, a lower level of anticipated HIV stigma, and higher HIV testing self-efficacy were associated with HIV test uptake among MSM aged 50 and above.
In multivariable analysis (), participants who got divorced/widowed were more likely to receive HIV testing compared to those who married (AOR = 1.5;95%CI:1.1–2.0). Participants who were aware of HIV/AIDS-related knowledge (AOR = 1.8;95%CI:1.4–2.3), ever disclosed sexual orientation (AOR = 1.9;95%CI:1.5–2.5), ever had STIs before (AOR = 2.4;95%CI:1.8–3.2) and with high self-efficacy (AOR = 1.1;95%CI:1.0–1.1) were more likely to receive HIV testing. Participants had≥2 sexual partners were more likely to receive HIV testing than those who had one or none (AOR = 1.8;95%CI:1.4–2.3).
Table 2. Multivariate factors associated with HIV testing among 50 and older MSM in China (n = 1259).
Discussion
The current study indicated the rate of HIV testing among Chinese MSM aged 50 and older is 62.0%. The rate is slightly higher than that among MSM aged 16 and older in China but much lower than that in developed countries such as the U.S. and the U.K.(Clark et al., Citation2019; Han et al., Citation2017; Witzel et al., Citation2016).
The study results revealed the theoretically-expected association between HIV testing behaviors and the HBM-based constructs of HIV/AIDS-knowledge, self-efficacy and modifying/enabling factors. As suggested by existing studies, self-efficacy is important in predicting and explaining intention to seek HIV testing, which implied that it is essential to improve self-efficacy of HIV testing by raising perceived susceptibility of HIV infection and essentiality for testing (Jin et al., Citation2017; Pham et al., Citation2019). However, compared to the whole MSM population (88.4%) (Huang et al., Citation2015), it was found that MSM age 50 and older in China had limited HIV/AIDS-related knowledge according to our study.
Sexual orientation disclosure to the Health-Care Provider, number of sexual partners and ever had STIs before were proved associated with HIV testing behavior in our study. Dislosure of MSM’s sexual behaviors can help health providers realize individual’s needs for HIV prevention and care, including routine screenings of HIV (Qiao et al., Citation2018). MSM ever had STIs before were more likely to receive HIV testing, this might be motivated by experiencing illness and forced to seek diagnosis and health care services (Okal et al., Citation2020). Participants with multiple sexual partners may receive HIV testing as prevention practices because of their high-risk sexual behaviors (Mitchell & Petroll, Citation2012). In addition, compared to divorced/widowed individuals, MSM in marriage are always under disclosure pressure, which may explain why they are less likely to have HIV tests in our study.Tailored interventions to identify MSM staying in marriage and offer appropriate health care services might be applicable if the MSM GSN apps can function in this way.
While perceived barriers such as anticipated HIV stigma, depression and lack of social support, were not significant in explaining intention to uptake HIV testing, it might also be mediators through which disclosure affects the HIV testing behavior (Wei et al., Citation2016). Therefore development of a HIV-prevention interventions considering mental health should be adopted among Chinese MSM aged 50 and above.
This study had several limitations. First, the survey was a cross-sectional study, and it is hard to determine the causal connections between the proposed factors and the outcome variables. Second, participants were asked to recall information from the past year, allowing for recall bias and inaccuracy. The third is selection bias. Our findings are based on MSM who have cellphones and use Blued apps. However, older MSM may be more accessible in gay venues like bars, parks, and public baths, not only on the internet. Although we successfully reached over 1200 MSM via an online survey, online studies are not probabilistic sampling strategies, thus precluding the generalizability of the findings in certain extent.
In conclusion, our study suggests that Chinese MSM aged 50 and above have significant rates of not been tested for HIV, which highlights tailored interventions should take into account demographics and behavioral characteristic in a more supportive social environment, hence to promote HIV testing uptake and follow-up treatment and care among this population.
Ethics approval
This study has been approved by the Institutional Review Board of Jining Medical College in March 2020 (approval number: JNMC-2020-KY-002).
Acknowledgements
The authors would like to thank all the persons who contributed to this research: all the professors and lecturers at the Chinese Academy of Medical Science and Peking Union Medical College for their instructive suggestions and helpful comments and all the men who participated in this survey, as they contributed to something useful for their community.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Additional information
Funding
References
- Anwuri, G. C., Dunn, M. S., & Schulze, F. (2017). Determinants of voluntary HIV/AIDS counseling and testing among community college students in the United States. International Journal of MCH and AIDS (IJMA), 6(2), 109–120. https://doi.org/10.21106/ijma.212
- Chen, H., Luo, L., Pan, S. W., Lan, G., Zhu, Q., Li, J., Zhu, J., Chen, Y., Shen, Z., Ge, X., Tang, Z., Xing, H., Shao, Y., Ruan, Y., & Yang, W. (2019). HIV epidemiology and prevention in southwestern China: Trends from 1996-2017. Current HIV Research, 17(2), 85–93. https://doi.org/10.2174/1570162X17666190703163838
- Clark, H. A., Oraka, E., DiNenno, E. A., Wesolowski, L. G., Chavez, P. R., Pitasi, M. A., & Delaney, K. P. (2019). Men who have sex with men (MSM) who have not previously tested for HIV: Results from the MSM testing initiative, United States (2012-2015). AIDS and Behavior, 23(2), 359–365. https://doi.org/10.1007/s10461-018-2266-3
- Dalrymple, J., McAloney-Kocaman, K., Flowers, P., McDaid, L. M., & Frankis, J. S. (2019). Age-related factors influence HIV testing within subpopulations: A cross-sectional survey of MSM within the celtic nations. Sexually Transmitted Infections, 95(5), 351–357. https://doi.org/10.1136/sextrans-2018-053935
- Dong, M.-J., Peng, B., Liu, Z.-F., Ye, Q.-n., Liu, H., Lu, X.-L., Zhang, B., & Chen, J.-J. (2019). The prevalence of HIV among MSM in China: A large-scale systematic analysis. BMC Infectious Diseases, 19(1), 1000. https://doi.org/10.1186/s12879-019-4559-1
- Dowson, L., Kober, C., Perry, N., Fisher, M., & Richardson, D. (2012). Why some MSM present late for HIV testing: A qualitative analysis. AIDS Care, 24(2), 204–209. https://doi.org/10.1080/09540121.2011.597711
- Golub, S. A., & Gamarel, K. E. (2013). The impact of anticipated HIV stigma on delays in HIV testing behaviors: Findings from a community-based sample of men who have sex with men and transgender women in New York city. AIDS Patient Care and STDs, 27(11), 621–627. https://doi.org/10.1089/apc.2013.0245
- Han, L., Wei, C., Muessig, K. E., Bien, C. H., Meng, G., Emch, M. E., & Tucker, J. D. (2017). HIV test uptake among MSM in China: Implications for enhanced HIV test promotion campaigns among key populations. Global Public Health, 12(1), 31–44. https://doi.org/10.1080/17441692.2015.1134612
- Huang, Q., Li, Q., Li, Y., Zeng, G., Cui, X., Yan, P., … Luan, R. (2015). [Prevalence of HIV infection and syphilis, sexual behaviors and awareness of HIV/AIDS related knowledge among men who have sex with men in China: A meta-analysis of data collected from 2010 to 2013]. Zhonghua Liu Xing Bing Xue Za Zhi, 36(11), 1297–1304.
- Jin, S. S., Bu, K., Chen, F. F., Xu, H. F., Li, Y., Zhao, D. H., … Wang, L. (2017). Correlates of condom-use self-efficacy on the EPPM-based integrated model among Chinese College students. Biomedical and Environmental Sciences, 30(2), 97–105. https://doi.org/10.3967/bes2017.013
- Kabiru, C. W., Beguy, D., Crichton, J., & Zulu, E. M. (2011). HIV/AIDS among youth in urban informal (slum) settlements in Kenya: What are the correlates of and motivations for HIV testing? BMC Public Health, 11(1), 685. https://doi.org/10.1186/1471-2458-11-685
- Li, J., Mo, P. K. H., Wu, A. M. S., & Lau, J. T. F. (2017). Roles of self-stigma, social support, and positive and negative affects as determinants of depressive symptoms among HIV infected men who have sex with men in China. AIDS and Behavior, 21(1), 261–273. https://doi.org/10.1007/s10461-016-1321-1
- Mitchell, J. W., & Petroll, A. E. (2012). HIV testing rates and factors associated with recent HIV testing among male couples. Sexually Transmitted Diseases, 39(5), 379–381. https://doi.org/10.1097/OLQ.0b013e3182479108
- Ning, Z., Fu, J., Zhuang, M., Park, J. A., Ibragimov, U., He, N., & Wong, F. Y. (2018). HIV and syphilis epidemic among MSM and non-MSM aged 50 and above in Shanghai, China: A yearly cross-sectional study, 2008-2014. Global Public Health, 13(11), 1625–1633. https://doi.org/10.1080/17441692.2018.1427271
- Okal, J., Lango, D., Matheka, J., Obare, F., Ngunu-Gituathi, C., Mugambi, M., & Sarna, A. (2020). “It is always better for a man to know his HIV status” - A qualitative study exploring the context, barriers and facilitators of HIV testing among men in Nairobi, Kenya. PLoS ONE, 15(4), e0231645. https://doi.org/10.1371/journal.pone.0231645
- Pham, M. D., Aung, P. P., Agius, P. A., Pasricha, N., Oo, S. M., Tun, W., Bajracharya, A., & Luchters, S. (2019). Relationship between self-efficacy and HIV testing uptake among young men who have sex with men in Myanmar: A cross-sectional analysis. International Journal of STD & AIDS, 30(1), 20–28. https://doi.org/10.1177/0956462418.791945
- Qiao, S., Zhou, G., & Li, X. (2018). Disclosure of same-sex behaviors to health-care providers and uptake of HIV testing for men who have sex with men: A systematic review. American Journal of Men's Health, 12(5), 1197–1214. https://doi.org/10.1177/1557988318784149
- Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175–183. https://doi.org/10.1177/109019818801500203
- Sexually Transmitted Diseases Treatment Guidelines. (2006). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5511a1.htm
- Stannah, J., Dale, E., Elmes, J., Staunton, R., Beyrer, C., Mitchell, K. M., & Boily, M. C. (2019). HIV testing and engagement with the HIV treatment cascade among men who have sex with men in Africa: A systematic review and meta-analysis. The Lancet HIV, 6(11), e769–e787. https://doi.org/10.1016/s2352-3018(19)30239-5
- Wei, C., Cheung, D. H., Yan, H., Li, J., Shi, L. E., & Raymond, H. F. (2016). The impact of homophobia and HIV stigma on HIV testing uptake among Chinese men who have sex with men: A mediation analysis. JAIDS Journal of Acquired Immune Deficiency Syndromes, 71(1), 87–93. https://doi.org/10.1097/qai.0000000000000815
- Witzel, T. C., Melendez-Torres, G. J., Hickson, F., & Weatherburn, P. (2016). HIV testing history and preferences for future tests among gay men, bisexual men and other MSM in England: Results from a cross-sectional study. BMJ Open, 6(9), e011372–e011372. https://doi.org/10.1136/bmjopen-2016-011372
- Yu, S.-C., Lin, Y.-H., & Hsu, W.-H. (2013). Applying structural equation modeling to report psychometric properties of Chinese version 10-item CES-D depression scale. Quality & Quantity, 47(3), 1511–1518. https://doi.org/10.1007/s11135-011-9604-0
- Zhao, P., Liu, L., Zhang, Y., Cheng, H., Cao, B., Liu, C., Wang, C., Yang, B., Wei, C., Tucker, J. D., & Tang, W. (2018). The interaction between HIV testing social norms and self-efficacy on HIV testing among Chinese men who have sex with men: Results from an online cross-sectional study. BMC Infectious Diseases, 18(1), 541. https://doi.org/10.1186/s12879-018-3454-5