ABSTRACT
Eswatini has a high HIV prevalence but has made progress towards improving HIV-status awareness, ART uptake and viral suppression. However, there is still a delay in ART initiation, which could partly be attributed to positive HIV-retesting. This study examines reasons for, and factors associated with, positive HIV-retesting among MaxART participants in Eswatini. Data from 601 participants is included in this cross-sectional study. Descriptive statistics and logistic regressions were used. Of the participants, 32.8% has ever retested after a previous positive result. Most participants who retested did this because they could not accept their results (61.9% of all retesters). Other main reasons are related to external influences, gender or the progression of their HIV infection (respectively 18.3%, 10.2%, and 6.1% of all retesters). Participants without a current partner and participants with less time since their first positive test have lower odds of retesting. To decrease retesting and reduce the delay in ART initiation resulting from it, efforts could be made on increasing the acceptance of positive HIV results. Providing more information on the process of testing and importance of early ART initiation, could be part of the solution.
Introduction
Progress has been made in the reduction of transmission, morbidity and mortality of HIV and AIDS, however additional gains are possible with earlier viral suppression (Cohen et al., Citation2011; Hoffmann & Chaisson, Citation2013; Lawn et al., Citation2005, Citation2006; Lundgren et al., Citation2015; Tanser et al., Citation2013). Given the benefits of early ART initiation, the WHO issue guidance in 2015 that ART should be initiated directly after an HIV diagnosis regardless of a person’s CD4-cell count, denoted as “test-and-treat” (World Health Organization, Citation2015). Because of this, it is important to identify which factors hamper early ART initiation.
The Kingdom of Eswatini has one of the highest HIV prevalence estimates in the world, with 27.0% in 2017 (Government of the Kingdom of Eswatini, Citation2019). The ART coverage among people aware of their HIV-status was 74.1% in that year (Government of the Kingdom of Eswatini, Citation2019). The threshold to initiate ART in Eswatini was <200 CD4-cells/mm³ in 2003 and was changed to <350 CD4-cells/mm³ in 2010 and to <500 CD4-cells/mm³ in 2015. In 2016, Eswatini lifted the CD4-cell threshold for ART initiation (Government of the Kingdom of Eswatini, Citation2019).
The MaxART trial was initiated in 2014 in Eswatini with the aim to examine the effect of the test-and-treat strategy. It was found that the retention in care and viral suppression was higher among people in the test-and-treat group than in the standard of care group, while the adherence to ART remained the same (Khan et al., Citation2020; Molemans et al., Citation2019). However, not all HIV-positive people in Eswatini are on ART, which indicates a delay in ART initiation (Dlamini-Simelane & Moyer, Citation2017; Government of the Kingdom of Eswatini, Citation2019).
An important cause of delays in ART initiation is positive HIV-retesting, that is, retesting after having tested positive at an earlier occasion (Giguère et al., Citation2021; Grimsrud et al., Citation2020; Horter et al., Citation2017; Kulkarni et al., Citation2017), hereinafter referred to as “retesting”. This indicates an earlier missed opportunity for ART initiation and subsequent delay. In the setting of the MaxART study, it was shown that among the patients who delay ART initiation, there are patients who have tested positive multiple times and they indicate that this was a way of coming to terms with their diagnosis (Pell et al., Citation2018).
Even though positive HIV-retesting is an obstacle in ART initiation, research on it is still scarce (Giguère et al., Citation2021; Grimsrud et al., Citation2020; Horter et al., Citation2017; Kulkarni et al., Citation2017). This study examines the reasons for, and the factors associated with, positive HIV-retesting among MaxART participants in Eswatini.
Method
Study setting
The MaxART trial was set in the Hhohho region of Eswatini, and started in 2014. The goal was to examine the implementation of the test-and-treat approach in a government-managed health system (Khan et al., Citation2020; Walsh et al., Citation2017). The MaxART trial also contained a social science component, which included qualitative research, as well as a cross-sectional survey. The objective was to explore the social and behavioural effects of starting ART early for HIV-positive people within the MaxART implementation study at nine out of the fourteen clinics (Molemans et al., Citation2019; Vernooij et al., Citation2016). The survey data from this social science component was used for the current study.
Study population
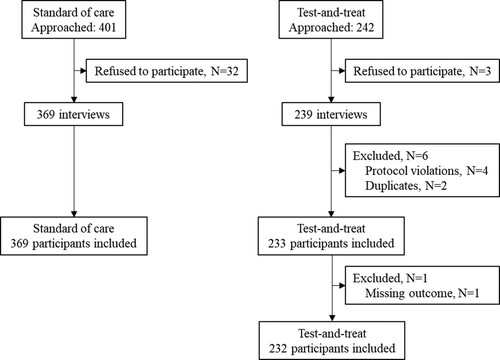
This social science substudy included 602 HIV-positive people aged 18 years and older from the initial MaxART trial, consisting of two groups, namely the test-and-treat group and standard of care group. In the test-and-treat group, there were 239 interview records, six were excluded because of protocol violations or duplication, which resulted in 233 test-and-treat participants. These participants started ART in a facility that adopted the test-and-treat intervention at least three months before the interview. The participants had a CD4 count of >350 CD4-cells/mm³ and WHO clinical stage one or two. The 369 participants in the standard of care arm, started ART less than 12 months ago. These participants were treated following the national ART guidelines, with an ART initiation threshold of <350 CD4-cells/mm³. One additional participant was excluded due to a missing value on the outcome, retesting, resulting in a final sample size of 601 (). Exclusion criteria for the MaxART trial were: participants being pregnant or breastfeeding at enrolment, having a mental illness, or having start ART before enrolment, as described in the protocol (Walsh et al., Citation2017). There were no additional in and exclusion criteria for the social science substudy. However, due to the timing of the interviews being after trial enrolment, everyone was on ART.
Data collection
The data from the social science component were collected face to face by trained Swati researchers using semi-structured questionnaires, which were based on the WHO’s manual HIV Testing, Treatment and Prevention: Generic Tools for Operational Research (Health Organization & Council, Citation2009). The questionnaires were in SiSwati and translated to English after the interviews by the interviewers themselves. The questionnaire contained both closed and open-ended questions.
Variables
For the analysis, the main outcome was “retesting”, defined as a dichotomous variable. The outcome was self-reported. Participants had retested when they had tested positive on HIV on a previous occasion and the repeated test was not part of the standard confirmation test. Based on previous studies on retesting and delays in ART initiation (Giguère et al., Citation2021; Grimsrud et al., Citation2020; Kulkarni et al., Citation2017), the following variables were included: gender, age, educational level, religion, feeling guilty about one’s HIV-status, marital status, HIV-status of the partner, requiring permission to go to health facility from another member of their household, being the head of the household, having children, time since first positive test, and ART initiation guidelines.
The variables gender, feeling guilty, requiring permission to go to health facility, being the head of the household, having children, and ART initiation guidelines, were all dichotomous variables. Age, educational level, religion, marital status, HIV-status of the partner, and time since first positive test were all categorical variables.
Data analysis
The data analysis was carried out with IBM SPSS version 25. We used descriptive statistics to describe frequencies across demographic characteristics and the reasons for retesting. We used logistic regressions to analyse the associations between the predefined variables and retesting in bivariable and multivariable approaches. The multivariable model contained all identified variables as this fits the theoretical framework underlying the analysis. We assumed a two-sided p-value <0.05 as statistically significant. We conducted a thematic qualitative analysis to the answers to the question on the reason for retesting.
Ethics
The MaxART trial was approved by the Eswatini National Health Research Review Board in July 2014 under reference Number: MH/599C/FWA 000 15267. All participants gave oral consent to be included in the MaxART trial and gave written consent to be interviewed for the social science survey study. In the records of these interviews identifiers were used instead of names.
Results
Demographic characteristics
The demographic characteristics of the 601 participants are described in . The mean age was 37, with most participants falling in the category 26–35 and 36–45 (respectively 38.7% and 25.7%). Most participants were female (77.1%). Of the 601 participants, 32.8% (N = 197) had ever retested. When the participants were stratified on whether they had ever retested, the percentages of female participants differed (82.7% of the retesters are female versus 74.3% of the non-retesters are female).
Table 1. Demographic characteristics stratified on retesting (N = 601).
Most participants only attended primary school (34.8%), were in a relationship (86.2%), had children (88.9%), and had partners who are HIV-positive too (48.8%). People who had retested were more often in a relationship (93.4% versus 82.9% of the non-retesters) and did more often have a HIV-positive partner (57.4% versus 44.8% of the non-retesters). Among those who did practice a religion, African Healing Churches were the most frequent (53.3%). Furthermore, almost three out of four participants did not consider themselves head of their household (73.7%), while one out of four stated that they needed permission to go to the health facility (27.3%).
Reasons for retesting
The answers to the open-ended question regarding the reason for retesting were coded and then categorised into eighteen categories. These categories were further organised in five overarching themes; results acceptance, external influences, gender related, disease progression and other/unclear reasons. The overarching themes and the corresponding reasons for retesting can be found in .
Table 2. Reasons for retesting (N = 197).
Results acceptance
The most frequent reasons for retesting were those regarding the acceptance of the results (61.9% of all retesters). The most reported one was that participants wanted to confirm their results (40.1% of all retesters). Other participants stated that they did not believe or trust the results they got (respectively 13.7% and 5.1% of all retesters). Three participants did not trust their results because they used self-tests which gave inconsistent or unclear answers. A few said they needed time to process their outcome (2.0% of all retesters). Two participants hoped that they would get a negative outcome this time (1.0% of all retesters).
External influences
Reasons related to external influences were given by 18.3% of all retesters. Participants were either advised to retest or had no choice but to retest. They had to retest when they changed health facilities, when they were tested a long time ago or when there were practical issues during the earlier test (respectively 3.0%, 1.5% and 4.1% of all retesters). These practical issues included situations such as having been misinformed by health care workers, and not receiving or losing their testing papers. The most frequent reason within this theme was that participants were advised or obliged to retest by a health care worker at the health facility (8.6% of all retesters). Two participants had not been advised at the health facility, but by others at work and at church (1.0% of all retesters).
Gender related
Two of the reasons for retesting were only reported by female participants (10.2% of all retesters). Most women within this theme stated that they were pregnant (6.6% of all retesters), with some being retested as a routine procedure during antenatal care. The other reason was that the participants retested because of their husband or partner (3.6% of all retesters). Hereby some participants stated that their husband did not believe that they were HIV-positive. Others stated that they were afraid to tell their husband themselves and therefore went together to the health facility to (re)test.
Disease progression
A small group of twelve participants stated reasons related to the progression of the disease (6.1% of all retesters). Two participants explicitly stated that they had retested because they wanted to start with ART (1.5% of all retesters). The most frequent reason was that participants wanted to know their CD4-cell count (3.0% of all retesters). Other people stated that they started to feel ill or that they were afraid to die (respectively 1.5% and 0.5% of all retesters).
Other/Unclear
Seven reasons could either not be classified in one of the previous themes or were unclear (3.6% of all retesters).
Factors associated with retesting
The results of the logistic regression for factors associated with retesting are shown in . In the bivariable analyses men had a significantly lower odds of retesting than women (OR = 0.6, CI 95% = 0.4–0.9). With regards to relationship status, single/never married persons (OR = 0.1, CI 95% = 0.0–0.5), or those being divorced/widowed/separated (OR = 0.5, CI 95% = 0.3–1.1) had a lower odds of being retested than participants who were in a relationship. With religion, only a significantly higher odds of retesting compared to non-religious participants was found for participants who have an evangelical religion (OR = 2.3, CI 95% = 1.2–4.7). People who had their first positive test between one to five years ago (OR = 3.3, CI 95% = 2.2–5.1) and those who had it more than five years ago (OR = 7.6, CI 95% = 4.7–12.4) had a higher odds of retesting than people who had it less than one year ago.
Table 3. Factors associated with retesting.
In the multivariable regression model, adjusted for the other variables, marital status and time since first positive test were associated with a higher odds of retesting. The adjusted odds of participants who were single or never married on retesting compared to participants who were in a relationship was 0.1 (CI 95% = 0.0–0.6). People who had their first positive test between one to five years ago (AOR = 3.4, CI 95% = 2.1–5.4) and those who had it more than five years ago (AOR = 8.0, CI 95% = 4.6–13.9) had a higher odds of retesting than people who had it less than one year ago. We found no association between retesting and any other of our predefined variables.
Discussion
This study examined what the reasons are for, and the factors associated with, positive HIV-retesting among MaxART participants in Eswatini. The results show that 32.8% of the participants had retested. Almost two-thirds of them did this because they could not fully accept their previous positive results. The other participants who have retested did this because of external influences, gender-related reasons or reasons regarding the progression of their HIV infection. Furthermore, marital status and time since first positive test were identified as a factors that are associated with retesting.
Participants who are single possibly retested less as there was no spouse that requested an HIV test result at the time of cohabitation. Qualitative research in Eswatini also showed that delays in ART initiation can be due to relational dynamics that women have to navigate to access ART, by acquiring permission and/or financial means from their husband (Dlamini-Simelane & Moyer, Citation2017). Furthermore, the findings that participants who have a longer time since their first positive test are more likely to retest, can be explained by the fact that they had more opportunities to retest.
The acceptance of the results was reported to be an important reason for retesting in other studies as well (Giguère et al., Citation2021; Horter et al., Citation2017). The acceptance of the results and coming to terms with the diagnosis was also found in qualitative interviews with patients that delayed ART initiation in the MaxART study (Pell et al., Citation2018).
However, previous studies found significant associations between retesting and factors for which no significant association was found in this study, such as for education (Hakim et al., Citation2019) and having children (Kulkarni et al., Citation2017). Of all participants, 32.8% have retested in this study, while in other studies this ranges from 13.2% to 75% (Grimsrud et al., Citation2020; Kulkarni et al., Citation2017). The differences in prevalence indicate that the proportion of people retesting is setting specific.
Our results show that there is a large group in Eswatini who could be prioritised for interventions to decrease the delay in ART initiation due to retesting. Outside Eswatini, this study contributes to the currently scarce body of evidence on retesting.
A limitation is that there might have been a social desirability bias, because the data was collected through in-person interviews. There could have occurred some recall bias, including with the outcome, and non-response bias. However, both are expected to be low in this study as most questionnaire questions were about the participants’ current situation and only 5% (N = 35) of the approached people refused to participate in the study (). Additionally, a small group of 19 participants (3.2% of all participants) were not included in the multivariable model because they had a missing value in one or more variables (), which could have caused some bias. Finally, residual confounding could remain. Because studies on retesting are scarce, there are possibly potential confounders that are still unknown.
Based on these findings, policy makers and health care providers could look further into measures to improve the acceptance of positive HIV results. These could potentially lie in other approaches to counselling, possibly couple-focused counselling, which includes more information explaining the process of HIV-testing and the importance of early ART initiation. During counselling, people could be made more aware that a confirmation test already took place before they got the results and the distrust of test results could be made a topic of conversation. If people still want to retest for confirmation, they could be offered one immediately at the health facility. In order to tackle several external influences that cause retesting, efforts could be made to implement a nationwide digital medical registration. Situations such as participants changing health facilities, and losing or not receiving testing papers would no longer cause retests. Such a system would be beneficial for other mobility related issues, such as loss to follow-up (Shabalala et al., Citation2018) and more in general for the management of all chronic conditions requiring regular health care visits. When looking for measures and interventions to decrease retesting, extra attention should be given to people in a relationship.
To conclude, the most important reason for retesting among was that participants could not fully accept their previous results. Marital status and time since first positive test were found to be associated with retesting. Retesting and subsequent delays in ART initiation remain a barrier to achieving additional gains in HIV prevention and control. This study provides insights into the prevalence and reasons for positive HIV retesting in Eswatini.
Acknowledgements
We thank everyone who contributed to the execution and data collection of the MaxART trial and the social science component. We also thank the MaxART partners, study team, healthcare providers and patients at study sites for their cooperation during the study.
Disclosure statement
The MaxART consortium received support of the Dutch Postcode Lottery in the Netherlands, the Embassy of the Kingdom of the Netherlands in South Africa/Mozambique, British Colombia Centre of Excellence in HIV/AIDS in Canada, Mylan and Médecins Sans Frontières. The findings and analysis presented are those of the authors and do not reflect those of any funders.
Additional information
Funding
References
- Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., Hakim, J. G., Kumwenda, J., Grinsztejn, B., Pilotto, J. H. S., Godbole, S. v., Mehendale, S., Chariyalertsak, S., Santos, B. R., Mayer, K. H., Hoffman, I. F., Eshleman, S. H., Piwowar-Manning, E., Wang, L., … Fleming, T. R. (2011). Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine, 365(6), 493–505. https://doi.org/10.1056/NEJMoa1105243
- Dlamini-Simelane, T. T. T., & Moyer, E. (2017). ‘Lost to follow up’: Rethinking delayed and interrupted HIV treatment among married swazi women. Health Policy and Planning, 32(2), 248–256. https://doi.org/10.1093/HEAPOL/CZW117
- Giguère, K., Eaton, J. W., Marsh, K., Johnson, L. F., Johnson, C. C., Ehui, E., Jahn, A., Wanyeki, I., Mbofana, F., Bakiono, F., Mahy, M., & Maheu-Giroux, M. (2021). Trends in knowledge of HIV status and efficiency of HIV testing services in sub-saharan Africa, 2000–20: A modelling study using survey and HIV testing programme data. The Lancet HIV, 8(5), e284–e293. https://doi.org/10.1016/s2352-3018(20)30315-5
- Government of the Kingdom of Eswatini. (2019). Swaziland HIV incidence measurement survey 2 (SHIMS2) 2016-2017. Final report. https://phia.icap.columbia.edu/wp-content/uploads/2019/05/SHIMS2_Final-Report_05.03.2019_forWEB.pdf
- Grimsrud, A., Wilkinson, L., Eshun-Wilson, I., Holmes, C., & Sikazwe, I. (2020). Understanding engagement in HIV programmes: How health services Can adapt to ensure no one Is left behind. Current HIV/AIDS Reports, 17(5), 458–466. https://doi.org/10.1007/2Fs11904-020-00522-1
- Hakim, A. J., Mukasa, B., Hundley, L., Odiit, M., Ogwal, M., Sendagala, S., Karamagi, Y., Sande, E., & Hladik, W. (2019). Correlates of undiagnosed HIV infection and retesting among voluntary HIV testing clients at mildmay clinic, Uganda. AIDS and Behavior, 23(4), 820–834. https://doi.org/10.1007/s10461-018-2274-3
- Health Organization & Council (2009). HIV testing, treatment and prevention: Generic tools for operational research. https://www.popcouncil.org/uploads/pdfs/2009HIV_WHOPCGenericTools.pdf
- Hoffmann, C. J., & Chaisson, R. E. (2013). Mortality associated with delays between clinic entry and ART initiation in resource-limited-settings: Results of a transition-state model. JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(2), 105–111. https://doi.org/10.1097/QAI.0b013e3182893fb4
- Horter, S., Thabede, Z., Dlamini, V., Bernays, S., Stringer, B., Mazibuko, S., Dube, L., Rusch, B., & Jobanputra, K. (2017). “Life is so easy on ART, once you accept it”: Acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Social Science & Medicine, 176, 52–59. https://doi.org/10.1016/j.socscimed.2017.01.006
- Khan, S., Spiegelman, D., Walsh, F., Mazibuko, S., Pasipamire, M., Chai, B., Reis, R., Mlambo, K., Delva, W., Khumalo, G., Zwane, M., Fleming, Y., Mafara, E., Hettema, A., Lejeune, C., Chao, A., Bärnighausen, T., & Okello, V. (2020). Early access to antiretroviral therapy versus standard of care among HIV-positive participants in eswatini in the public health sector: The MaxART stepped-wedge randomized controlled trial. Journal of the International AIDS Society, 23, e25310. https://doi.org/10.1002/jia2.25610
- Kulkarni, S., Tymejczyk, O., Gadisa, T., Lahuerta, M., Remien, R. H., Melaku, Z., El-Sadr, W., Elul, B., Nash, D., & Hoffman, S. (2017). “Testing, testing”: Multiple HIV-positive tests among patients initiating antiretroviral therapy in Ethiopia. Journal of the International Association of Providers of AIDS Care (JIAPAC), 16(6), 546–554. https://doi.org/10.1177/2325957417737840
- Lawn, S. D., Myer, L., Bekker, L. G., & Wood, R. (2006). Burden of tuberculosis in an antiretroviral treatment programme in sub-saharan Africa: Impact on treatment outcomes and implications for tuberculosis control. Aids (london, England), 20(12), 1605–1612. https://doi.org/10.1097/01.aids.0000238406.93249.cd
- Lawn, S. D., Myer, L., Orrell, C., Bekker, L. G., & Wood, R. (2005). Early mortality among adults accessing a community-based antiretroviral service in South Africa: Implications for programme design. Aids (london, England), 19(18), 2141–2148. https://doi.org/10.1097/01.aids.0000194802.89540.e1
- Lundgren, J. D., Babiker, A. G., Gordin, F., Emery, S., Grund, B., Sharma, S., Avihingsanon, A.-C., Cooper, D. A., Fätkenheuer, G., Llibre, J. M., Moli-Na, J.-M., Munderi, P., Schechter, M., Wood, R., Klingman, K. L., Collins, S., Clifford Lane, H., Phil-Lips, A. N., & Neaton, J. D. (2015). Initiation of antiretroviral therapy in early asymptomatic HIV infection. New England Journal of Medicine, 373(9), 795–807. https://doi.org/10.1056/NEJMoa1506816
- Molemans, M., Vernooij, E., Dlamini, N., Shabalala, F. S., Khan, S., van Leth, F., Gomez, G. B., & Reis, R. (2019). Changes in disclosure, adherence and healthcare interactions after the introduction of immediate ART initiation: An analysis of patient experiences in Swaziland. Tropical Medicine and International Health, 24(5), 563–570. https://doi.org/10.1111/tmi.13214
- Pell, C., Vernooij, E., Masilela, N., Simelane, N., Shabalala, F., & Reis, R. (2018). False starts in “test and start”: A qualitative study of reasons for delayed antiretroviral therapy in Swaziland. International Health, 10(2), 78–83. https://doi.org/10.1093/inthealth/ihx065
- Shabalala, F. S., Vernooij, E., Pell, C., Simelane, N., Masilela, N., Spiegelman, D., Chai, B., Khan, S., & Reis, R. (2018). Understanding reasons for discontinued antiretroviral treatment among clients in test and treat: A qualitative study in Swaziland. Journal of the International AIDS Society, 21(S4), e25120. https://doi.org/10.1002/JIA2.25120
- Tanser, F., Bärnighausen, T., Grapsa, E., Zaidi, J., & Newell, M.-L. (2013). High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-natal, South Africa. Science, 339(6122), 966–971. https://doi.org/10.1126/science.1228160
- Vernooij, E., Mehlo, M., Hardon, A., & Reis, R. (2016). Access for all: Contextualising HIV treatment as prevention in Swaziland. AIDS Care, 28(sup3), 7–13. https://doi.org/10.1080/09540121.2016.1178954
- Walsh, F. J., Bärnighausen, T., Delva, W., Fleming, Y., Khumalo, G., Lejeune, C. L., Mazibuko, S., Mlambo, C. K., Reis, R., Spiegelman, D., Zwane, M., & Okello, V. (2017). Impact of early initiation versus national standard of care of antiretroviral therapy in Swaziland’s public sector health system: Study protocol for a stepped-wedge randomized trial. https://doi.org/10.1186/s13063-017-2128-8
- World Health Organization. (2015). Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for hiv guidelines. https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_eng.pdf