ABSTRACT
Background: Breastfeeding is not recommended for women living with HIV (WLWH) in Canada. We described the prevalence of breastfeeding and explored experiences of care, support, and stigma related to infant feeding. Setting: Quebec, Ontario, and British Columbia (Canada). Methods: Data were obtained from the HIV Women’s Sexual and Reproductive Health Cohort Study (CHIWOS) surveys, conducted between 2013 and 2018. Results: Breastfeeding was reported by 73.5% of the 786 women who delivered before HIV diagnosis and 7.3% of the 289 women who delivered after HIV diagnosis. Among them, earlier year of delivery, delivery outside of Canada, and African, Caribbean, Black ethnicity were independently associated with increased odds of breastfeeding. Among WLWH who had a live birth during the last year, 77% (40/52) felt that they had received support regarding infant feeding practices, and 77% (23/30) were concerned that not breastfeeding could lead to them being identified as WLWH. Among 71 women within one year postpartum at any one of the study waves, 89% reported having an undetectable viral load. Conclusion: Breastfeeding experiences were common among WLWH, most often prior to HIV diagnosis. Fear of unintentional HIV status disclosure when not breastfeeding and challenges to maintain an undetectable HIV viral load are important issues to address during postpartum care.
KEYWORDS:
Introduction
The success of prevention of perinatal transmission of human immunodeficiency virus type 1 (HIV) is primarily attributed to the use of antiretroviral therapy (ART) during pregnancy. Breastfeeding avoidance can also contribute to a further reduction (Dunn et al., Citation1992). However, in low-resource settings, breastfeeding is recommended despite the potential risk of HIV transmission. This is because morbidity and mortality are significantly higher among infants who are formula fed compared with those who are breastfed, leading to higher overall rates of HIV-free survival of breastfed children in those contexts (WHO Guidelines Approved by the Guidelines Review Committee, Citation2016). Exclusive formula feeding with the avoidance of breastfeeding continues to be the recommendation in Canada (Khan et al., Citation2023), because maternal ART dramatically reduces HIV transmission through breastmilk but whether it eliminates it is unknown (Bispo et al., Citation2017; Bitnun et al., Citation2014). Several studies have described the social and psychological implications of breastfeeding avoidance (Greene et al., Citation2015; Tariq et al., Citation2016), but recent quantitative data on the frequency of breastfeeding and support for infant feeding practices in high-resource settings is lacking. In the context of the evidence supporting the undetectable = untransmittable campaign regarding sexual transmission of HIV, and of the 2016 WHO recommendations for breastfeeding in low-resource countries (WHO Guidelines Approved by the Guidelines Review Committee, Citation2016), some physicians, scientists and women living with HIV question whether the current recommendation against breastfeeding in high-resource countries remains justified (Kahlert et al., Citation2018; Waitt et al., Citation2018). Furthermore, several cases of breastfeeding among women living with HIV have been reported in these settings (Levison et al., Citation2014; Nashid et al., Citation2020; Portman MP et al., Citation2013; Tuthill et al., Citation2019).
The risk of HIV transmission through breastfeeding is highly linked to maternal viral load, which is dependent on engagement and retention in care (i.e., The cascade of care). The HIV cascade of care refers to the series of steps required for people with HIV to reach an undetectable HIV viral load, and includes diagnosis, linkage to care, retention in care, receiving ART and having an undetectable viral load (Government of Canada, Citation2016). Thus, a better knowledge of the rate of viral load suppression and the cascade of care in the postpartum period are essential sources of data to inform a broader discussion in Canada and other high-resource countries about the need and/or possibility of formulating current, evidence-based guidelines regarding breastfeeding in women living with HIV in these settings.
As such, this study uses cross-sectional survey data collected at three time-points from the Canadian HIV Women's Sexual and Reproductive Health Cohort Study (CHIWOS, www.chiwos.ca) to determine how frequently breastfeeding is reported by Canadian women living with HIV before and after HIV diagnosis and its risk factors (objective 1), to describe the care and support they received regarding infant feeding during and following pregnancy after HIV diagnosis, as well as any stigma they experienced related to feeding practice (objective 2), and to describe the HIV cascade of care among pregnant and postpartum women living with HIV (objective 3).
Methods
Study design and population
CHIWOS is a multicenter prospective cohort study that enrolled women living with HIV in British Columbia (BC), Ontario, and Quebec, conducted under community-based research principles. Participants were eligible if they self-identified as women (including cisgender and transgender women), were living with HIV, and were aged 16 years or older. Participants were recruited by trained peer research associates through HIV clinics, AIDS service organizations, website and social networks (Webster et al., Citation2018). Online questionnaires were administered in person or by phone/SKYPETM by trained peer research associates using FluidSurveys and Oracle software (Kaida et al., Citationn.d).
A total of 1,422 women completed the wave 1 CHIWOS questionnaire (2013–2015), 1252 the wave 2 questionnaire (2015–2017) and 1151 the wave 3 questionnaire (2017–2018). Women who had never been pregnant were excluded from the current analyses. For objective 1, participants were included in the analysis if they reported at least one previous pregnancy resulting in a live birth (before or after HIV diagnosis) and had available data on breastfeeding. For objective 2, only women who reported at least one live birth between waves 1 and 2 or between waves 2 and 3 were included. For objective 3, analyses were restricted to women who either had a live birth in the year prior to answering one of CHIWOS questionnaires or were currently pregnant at the time of completing one of the questionnaires.
The wave 1 questionnaire collected a retrospective lifetime history of pregnancy up to a maximum of 8 pregnancies. The waves 2 and 3 questionnaires included questions regarding HIV care as well as support and stigma/experience related to infant feeding (see Table 1 in supplementary material). Covariates of interest were age at delivery, country of birth, immigration status, country of delivery (Canada vs other), race/ethnicity, education, unplanned pregnancy, employment, education level achieved, preterm delivery, previous breastfeeding experience, province of residence, parity (first child yes/no) and intentions for future pregnancy.
Ethical approval was obtained from Simon Fraser University, University of British Columbia/Providence Health Care, Women’s College Hospital, and McGill University Health Centre, as well as at partnering hospitals and AIDS Service Organizations where required. This sub-study was also approved by the CHU Sainte-Justine Ethics Review Board.
Statistical analyses
Objective 1: Frequency of breastfeeding was assessed as well as its confidence interval. To explore predictors of breastfeeding, generalized estimating equation models were used, considering the correlation between multiple pregnancies for one woman, and stratifying by live births occurring before or after HIV diagnosis. Bivariate analyses between breastfeeding and each predictive factor were first carried out. Predictors were selected based on prior knowledge and review of preliminary summaries. For the multivariate analysis, groups of variables were formed as follows: sociodemographic characteristics (group 1), conception variables (group 2), and delivery variables (group 3) (Dunn et al., Citation1992). Within each group, breastfeeding was modelled using all variables from that group, and the variables with a p-value higher than 0.05 in the resulting model were dropped. The final model was constructed by adding all remaining variables one at a time and the one with most significant improvement of goodness of fit for model, quasilikelihood under the independence model criterion (QIC) was kept at each step, until the improvement is less than 1%.
Objective 2: For each care, support, and/or stigma outcome of interest, proportions for each answer were computed. Potential associations between those outcomes and the exploratory factors were assessed using Fisher’s Exact tests. Due to the exploratory nature of this analysis, no adjustments were made for the multiplicity of the tests.
Objective 3: No formal comparisons were made between groups as a number of women were in both groups at the same time (i.e., Currently pregnant while having delivered a previous child less than one year before) and/or appearing more than once in the same group, especially in the currently pregnant group. Covariates of interest were compared between postpartum women currently on ART with an undetectable viral load and the rest of the postpartum women using Wilcoxon’s rank sum tests for continuous variables and Fisher’s Exact tests for categorical variables. Due to the exploratory nature of the analyses, no adjustments were made for the multiplicity of the tests.
All analyses were made using version 9.4 of the SAS System (Copyright © [2013] SAS Institute Inc.)
Results
Breastfeeding practices before and after HIV-diagnosis
At wave 1, a total of 925 women reported at least one live birth before or after HIV diagnosis and were included in objective 1 analyses. While 1786 deliveries in 786 women occurred before diagnosis of HIV infection (up to 8 deliveries per woman), 409 deliveries in 289 women occurred after HIV infection diagnosis (up to 5 deliveries per woman). Among women who delivered before HIV diagnosis, 73.5% (578/786, 95% CI 70.4–76.6) reported at least one experience of breastfeeding, whereas among women who delivered after receiving their HIV diagnosis, 7.3% (21/289, 95% CI 4.1–10.5) reported an experience of breastfeeding, including 6 who delivered their child in Canada (all these infants tested negative for HIV). Predictive factors of breastfeeding per deliveries are reported in and . Among deliveries before HIV diagnosis, the main factor associated with a lower likelihood of breastfeeding was education lower than high school, while increased odds of breastfeeding were associated with later year of delivery, African, Caribbean, Black ethnicities and delivery outside of Canada. Among women who delivered after HIV diagnosis, earlier year of delivery, delivery outside of Canada, and African, Caribbean, Black ethnicities were independently associated with increased odds of breastfeeding.
Figure 1 . Predictive factors of breastfeeding according to timing of HIV diagnosis (Odds ratio), ART: antiretroviral therapy
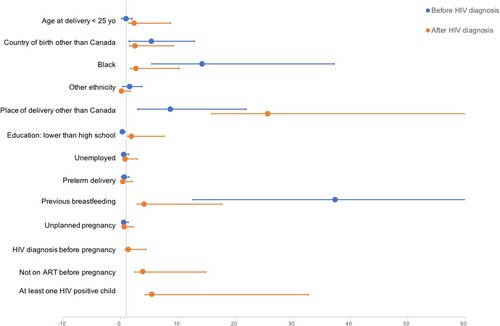
Table 1 . Risk factors for breastfeeding per live birth before and after HIV diagnosis.
Care, support and stigma around feeding practices
Among the CHIWOS cohort, 40 women had pregnancies between waves 1 and 2, and 26 between waves 2 and 3. Their answers to questions related to the care and support they received and their experience regarding infant feeding practices are reported in , by pregnancies. Feeling that they had received support regarding infant feeding practices was reported by 77% (40/52) of the women who provided an answer, and 96% (22/23) of the women who received specific counseling on these practices were satisfied with it. Among the 66 pregnancies, 26% were not offered a medication for lactation inhibition. Access to free formula programs was more frequent in BC and Ontario than in Quebec (respectively, 92%, 90% and 14%, p < 0.001).
Table 2. Care, support and experience regarding infant feeding practice in the CHIWOS cohort (55 women with 66 pregnancies in total).
HIV cascade of care among pregnant and post-partum women living with HIV
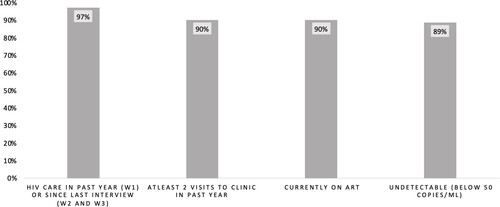
Seventy-one women were within one year postpartum at any one of the study waves. The characteristics of their HIV cascade of care are described in . Ninety percent [95%CI: 81–96] of postpartum women reported being currently on ART, and 89% [95%CI: 79–95] of them reported having an undetectable viral load. In bivariate analyses among postpartum women, being on ART and undetectable was significantly associated with high school education and higher, planned pregnancy and ART initiation before pregnancy (data not shown). Multivariate analyses could not be conducted because of the low number of events.
Figure 2 . HIV cascade of care of women of the Canadian HIV Women's Sexual and Reproductive Health Cohort Study (CHIWOS) who were within one year after delivery at any one of the study waves (n = 71). CHIWOS: W1. Wave 1 (2013–2015), W2. Wave 2 (2015–2017), W3. Wave 3 (2017–2018). ART: antiretroviral therapy
Discussion
This study demonstrates that among a cohort of women living with HIV, living in a resource-rich country, who have been pregnant, most women living with HIV had previous experience of breastfeeding, mainly before their HIV infection diagnosis or before moving to Canada. It also shows that although most women felt supported for their infant feeding practice, 23% did not receive counselling or were unsatisfied with the counselling received, 26% were not offered a medication for lactation inhibition, and 27% did not have access to a free formula program for their infants. Concern with the impact of not breastfeeding on their role and identity as a mother, experiences of social and cultural pressures to breastfeed and concerns about HIV status disclosure if they didn’t breastfeed were common. Among women within one year postpartum, 10% reported not taking ART.
The rate of breastfeeding in women before their HIV diagnosis (73.5%) is lower than the rate of breastfeeding initiation in the general population in Canada (90% in 2015–2016 Public Health Agency of Canada, Citation2018), likely reflecting infant feeding practice in other countries and in earlier years (Cai et al., Citation2012; United Nations Children’s Fund (UNICEF), Citation2018). Indeed breastfeeding rates have increased in Canada and around the world (Cai et al., Citation2012) but are still higher in low and middle resource countries than in high resource countries. Lower education was found to correlate with having not breastfed before HIV diagnosis, which is consistent with previous reports (Acharya & Khanal, Citation2015; Ladomenou et al., Citation2007; Tang et al., Citation2019).
In women who delivered after their HIV diagnosis, breastfeeding was rare and associated with delivery outside of Canada, as well as in earlier years and African, Caribbean, Black ethnicity which is consistent with the evolution of the international guidelines regarding infant feeding practice for women living with HIV (WHO Guidelines Approved by the Guidelines Review Committee, Citation2016; World Heath Organization, Citation2010; Young et al., Citation2011). Breastfeeding is a social construction perceived to be fundamental to many women but importantly by women living with HIV, who in resource-rich settings are encouraged to formula feed (Tuthill et al., Citation2014). Recommendations for women living with HIV to avoid breastfeeding challenge these social expectations. Concern with the impact of not breastfeeding on their role and identity as a mother was raised by the majority of our study participants as well as in previous qualitative studies of WLWH (Greene et al., Citation2015; Tariq et al., Citation2016). The high number of women living with HIV who reported social and cultural pressures to breastfeed in this study is also consistent with previous studies (Greene et al., Citation2015; Tariq et al., Citation2016). Ongoing consideration by care providers of how this might inform decision making about infant feeding practices and contribute to role strain in early motherhood is important to providing optimal pregnancy and postpartum care for mothers and their infants. The stigma associated with avoidance of breastfeeding which can suggest a woman’s HIV infection status is commonly reported (Doherty et al., Citation2006; Ion, Citation2019; Ion et al., Citation2017). Similar to the 77% of women in our study who reported concern about being identified as a women living with HIV by not breastfeeding, health care providers in the US reported that their patients’ primary concern regarding not breastfeeding was likewise stigma from potential HIV disclosure (Tuthill et al., Citation2019).
A the time of the study, free formula programs for infants born to women living with HIV were available in most provinces in Canada except Quebec – this explains why in our study 27% of women didn’t have access to such a program. Several qualitative studies have reported barriers to alternative feeding including cost and availability of formula(Ramara et al., Citation2010; Sibeko et al., Citation2009) and noted the importance of financial assistance with replacement feeding (Tariq et al., Citation2016). Only 74% of women reported that a medication for lactation inhibition was offered to them, likely because this practice is not discussed in most guidelines regarding HIV perinatal management (Tulloch et al., Citation2019). However, cabergoline appears to be safe and effective to decrease pain and discomfort from breast engorgement in women living with HIV when given within 48 hours after delivery (Tulloch et al., Citation2019) and is covered by some provincial health insurance programs in Canada.
The Canadian Perinatal HIV Surveillance Program data shows that the proportion of pregnant women not on suppressive antiretroviral therapy at delivery has gone down from 78% in 1998 to 14% in 2008 to 4.7% in 2018 (Sauve et al., Citation2019). Our data shows a lower rate of viral load control in the first year postpartum (90%). This rate is however much higher than the one reported in a meta-analysis, where postpartum adherence was achieved only by 62% of women living with HIV in high-resource countries (Nachega et al., Citation2012). Our relatively reassuring result should be confirmed in larger Canadian cohorts of post-partum women.
The study has some limitations. The analysis of background data regarding predictive factors for breastfeeding includes pregnancies from a prolonged time period (1961–2015), during which practices and guidelines regarding infant feeding have dramatically evolved. However, the results regarding support for infant feeding, stigma related to feeding practice and postpartum HIV care were collected prospectively during the 2013–2018 period and are therefore more representative of the current situation. In particular, the CHIWOS study took place in a period where guidelines regarding infant feeding in Canada were standardized and after the shift from short-term antenatal treatment for prevention of vertical transmission to the recommendation of life long ART for all adults with HIV regardless of their CD4 count. Additional limitation is that some of the variables were measured at the time of the survey, whereas the pregnancy outcomes were retrospective. Social desirability could also affect our results, as women aware of the recommendation against breastfeeding might have preferred not to disclose that they breastfed after HIV diagnosis during the interview, even if the interviews were conducted by a peer. Lastly, considering the recruitment strategy, women in our study do not represent all Canadian women living with HIV. As such, complementary research should focus both on quantitative data regarding the postpartum cascade of care and qualitative data regarding barriers and facilitators to postpartum retention in care in relation to infant feeding support services.
Conclusion
Most previous publications regarding care, support and experience related to infant feeding practices are from low-resource countries. This study provides new data that should be integrated into infant feeding guidelines for women living with HIV, especially the need to support women regarding social and cultural pressures and expectations to breastfeed, managing the stigma they face, and the impact on their perception of their role as a mother. New interventions should be evaluated to support infant feeding choices, to maximize retention in HIV care, ART adherence, and viral load suppression of postpartum women living with HIV.
CHIWOS Research Team
British Columbia: Aranka Anema (University of British Columbia, Vancouver), Denise Becker (Positive Living Society of British Columbia, Vancouver), Lori Brotto (University of British Columbia, Vancouver), Allison Carter (British Columbia Centre for Excellence in HIV/AIDS, Vancouver, and Simon Fraser University, Burnaby), Claudette Cardinal (Simon Fraser University, Burnaby), Guillaume Colley (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Erin Ding (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Janice Duddy (Pacific AIDS Network, Vancouver), Nada Gataric (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Robert S. Hogg (British Columbia Centre for Excellence in HIV/AIDS, Vancouver, and Simon Fraser University, Burnaby), Terry Howard (Positive Living Society of British Columbia, Vancouver), Shahab Jabbari (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Evin Jones (Pacific AIDS Network, Vancouver), Mary Kestler (Oak Tree Clinic, BC Women’s Hospital and Health Centre, Vancouver), Andrea Langlois (Pacific AIDS Network, Vancouver), Viviane Lima (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Elisa Lloyd-Smith (Providence Health Care Elisa Lloyd-Smith), Melissa Medjuck (Positive Women’s Network, Vancouver), Cari Miller (Simon Fraser University, Burnaby), Deborah Money (Women’s Health Research Institute, Vancouver), Valerie Nicholson (Simon Fraser University, Burnaby), Gina Ogilvie (British Columbia Centre for Disease Control, Vancouver), Sophie Patterson (Simon Fraser University, Burnaby), Neora Pick (Oak Tree Clinic, BC Women’s Hospital and Health Centre, Vancouver), Eric Roth (University of Victoria, Victoria), Kate Salters (Simon Fraser University, Burnaby), Margarite Sanchez (ViVA, Positive Living Society of British Columbia, Vancouver), Jacquie Sas (CIHR Canadian HIV Trials Network, Vancouver), Paul Sereda (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Marcie Summers (Positive Women’s Network, Vancouver), Christina Tom (Simon Fraser University, Burnaby), Clara Wang (British Columbia Centre for Excellence in HIV/AIDS, Vancouver), Kath Webster (Simon Fraser University, Burnaby), Wendy Zhang (British Columbia Centre for Excellence in HIV/AIDS, Vancouver).
Ontario: Rahma Abdul-Noor (Women’s College Research Institute, Toronto), Jonathan Angel (Ottawa Hospital Research Institute, Ottawa), Fatimatou Barry (Women’s College Research Institute, Toronto), Greta Bauer (University of Western Ontario, London), Kerrigan Beaver (Women’s College Research Institute, Toronto), Anita Benoit (Women’s College Research Institute, Toronto), Breklyn Bertozzi (Women’s College Research Institute, Toronto), Sheila Borton (Women’s College Research Institute,Toronto), Tammy Bourque (Women’s College Research Institute, Toronto), Jason Brophy (Children’s Hospital of Eastern Ontario, Ottawa), Ann Burchell (University of Toronto, Toronto), Allison Carlson (Women’s College Research Institute, Toronto), Lynne Cioppa (Women’s College Research Institute, Toronto), Jeffrey Cohen (Windsor Regional Hospital, Windsor), Tracey Conway (Women’s College Research Institute, Toronto), Curtis Cooper (Ottawa Hospital Research Institute, Ottawa), Jasmine Cotnam (Women’s College Research Institute, Toronto), Janette Cousineau (Women’s College Research Institute, Toronto), Marisol Desbiens (Women’s College Research Institute, Toronto), Annette Fraleigh (Women’s College Research Institute, Toronto), Brenda Gagnier (Women’s College Research Institute, Toronto), Claudine Gasingirwa (Women’s College Research Institute, Toronto), Saara Greene (McMaster University, Hamilton), Trevor Hart (Ryerson University, Toronto), Shazia Islam (Women’s College Research Institute, Toronto), Charu Kaushic (McMaster University, Hamilton), Logan Kennedy (Women’s College Research Institute, Toronto), Desiree Kerr (Women’s College Research Institute, Toronto), Gladys Kwaramba (Women’s College Research Institute, Toronto), Lynne Leonard (University of Ottawa, Ottawa), Johanna Lewis (Women’s College Research Institute, Toronto), Carmen Logie (University of Toronto, Toronto), Shari Margolese (Women’s College Research Institute, Toronto), Marvelous Muchenje (Women’s Health in Women’s Hands, Toronto), Mary (Muthoni) Ndung’u (Women’s College Research Institute, Toronto), Kelly O’Brien (University of Toronto, Toronto), Charlene Ouellette (Women’s College Research Institute, Toronto), Je Powis (Toronto East General Hospital, Toronto), Corinna Quan (Windsor Regional Hospital, Windsor), Janet Raboud (Ontario HIV Treatment Network, Toronto), Anita Rachlis (Sunnybrook Health Sciences Centre, Toronto), Edward Ralph (St. Joseph’s Health Care, London), Sean Rourke (Ontario HIV Treatment Network, Toronto), Sergio Rueda (Ontario HIV Treatment Network, Toronto), Roger Sandre (Haven Clinic, Sudbury), Fiona Smaill (McMaster University, Hamilton), Stephanie Smith (Women’s College Research Institute, Toronto), Tsitsi Tigere (Women’s College Research Institute, Toronto), Wangari Tharao (Women’s Health in Women’s Hands, Toronto), Sharon Walmsley (Toronto General Hospital Research Institute, Toronto), Wendy Wobeser (Queen’s University, Kingston), Jessica Yee (Native Youth Sexual Health Network, Toronto), Mark Yudin (St. Michael’s Hospital, Toronto).
Quebec: Dada Mamvula Bakombo (McGill University Health Centre, Montréal), Jean-Guy Baril (Université de Montréal, Montréal), Marc Boucher (Centre Hospitalier Universitaire Ste-Justine, Montréal), Isabelle Boucoiran (Centre Hospitalier Universitaire Sainte-Justine, Montréal), Nora Butler Burke (Concordia University, Montréal), José Côté (Centre Hospitalier de l’Université de Montréal, Montréal), Janice Dayle (McGill University Health Centre, Montréal), Danièle Dubuc, (McGill University Health Centre, Montréal), Mylène Fernet (Université du Québec à Montréal, Montréal), Marilou Gagnon (University of Ottawa, Ottawa), Fatima Kakkar (Centre Hospitalier Universitaire Sainte-Justine, Montréal), Maxime Kiboyogo (McGill University Health Centre, Montréal), Marina Klein (McGill University Health Centre, Montréal), Gary Lacasse (Canadian AIDS Society, Ottawa), Valérie Lamarre (Centre Hospitalier Universitaire Ste-Justine, Montr.al), Carrie Martin (Native Women’s Shelter of Montreal, Montréal), Lyne Massie, (Université de Québec à Montréal, Montréal), Brigitte Ménard, (McGill University Health Centre, Montréal), Ken Monteith (COCQ-SIDA, Montréal), Nadia O’Brien (McGill University, Montréal), Joanne Otis (Université du Québec à Montréal, Montréal), Doris Peltier (Canadian Aboriginal AIDS Network, Montr.al), Alie Pierre (McGill University Health Centre, Montr.al), Karène Proulx-Boucher (McGill University Health Centre, Montr.al), Danielle Rouleau (Centre Hospitalier de l’Université de Montréal, Montréal), Geneviève Rouleau (Centre Hospitalier de l’Universit. de Montr.al, Montr.al), Édénia Savoie (McGill University Health Centre, Montréal), Cécile Tremblay (Centre Hospitalier de l’Université de Montréal, Montr.al), Benoit Trottier (Clinique Médicale Urbaine du Quartier Latin, Montréal), Jason Szabo (Clinique l’Actuel, Montréal), Sylvie Trottier (Centre Hospitalier Universitaire de Québec, Quebec City), Christos Tsoukas (McGill University Health Centre, Montréal).
Other Canadian provinces or international jurisdictions:
Jacqueline Gahagan (Dalhousie University, Halifax), Catherine Hankins (University of Amsterdam, Amsterdam), Renee Masching (Canadian Aboriginal AIDS Network, Dartmouth), Susanna Ogunnaike-Cooke (Public Health Agency of Canada, Ottawa). All other CHIWOS Research Team members wish to remain anonymous.
Conflicts of Interest and Source of Funding
This work was supported by a Canadian Institutes of Health Research (CIHR) operating grant (MOP-111041), the CIHR Canadian HIV Trials Network (CTN 262), the Ontario HIV Treatment Network and the Academic Health Science Centres (AHSC) Alternative Funding Plans (AFP) Innovation Fund. IB and ADP received salary support from the Fonds de la recherche en santé du Québec (FRQS). Angela Kaida received salary support from CIHR.
Supplemental Material
Download MS Word (14.9 KB)Acknowledgements
The members of the CHIWOS Research Team thank all of the women living with HIV who participated in the research and entrusted CHIWOS with their experiences of HIV treatment, care and support. They also thank the entire national team of co-investigators, collaborators and peer research associates. They acknowledge the three provincial community advisory boards, the national CHIWOS Aboriginal advisory board and their partnering organizations for supporting the study. They also acknowledge the BC Centre for Excellence in HIV/ AIDS for in-kind data management and analytic support.
Additional information
Funding
References
- Acharya, P., & Khanal, V. (2015). The effect of mother's educational status on early initiation of breastfeeding: Further analysis of three consecutive Nepal demographic and health surveys. BMC Public Health, 15(1), 1069–1069. https://doi.org/10.1186/s12889-015-2405-y
- Bispo, S., Chikhungu, L., Rollins, N., Siegfried, N., & Newell, M. L. (2017). Postnatal HIV transmission in breastfed infants of HIV-infected women on ART: A systematic review and meta-analysis. Journal of the International AIDS Society, 20(1), 21251. https://doi.org/10.7448/IAS.20.1.21251
- Bitnun, A., Brophy, J., Samson, L., Alimenti, A., Kakkar, F., Lamarre, V., Moore, D., Karatzios, C., Seigel, S., Sauve, L., Vaudry, W., Yudin, M. H., & Money, D. (2014). Prevention of vertical HIV transmission and management of the HIV-exposed infant in Canada in 2014. Canadian Journal of Infectious Diseases and Medical Microbiology, 25(2), 75–77. https://doi.org/10.1155/2014/526019
- Cai, X., Wardlaw, T., & Brown, D. W. (2012). Global trends in exclusive breastfeeding. International Breastfeeding Journal, 7(1), 12. https://doi.org/10.1186/1746-4358-7-12
- Doherty, T., Chopra, M., Nkonki, L., Jackson, D., & Greiner, T. (2006). HIV epidemic and infant feeding in South Africa. Bulletin of the World Health Organization, 84(2), 90–96. https://doi.org/10.2471/BLT.04.019448
- Dunn, D. T., Newell, M. L., Ades, A. E., & Peckham, C. S. (1992). Risk of human immunodeficiency virus type 1 transmission through breastfeeding. The Lancet, 340(8819), 585–588. https://doi.org/10.1016/0140-6736(92)92115-V
- Government of Canada. (2016). Measuring Canada's progress on the 90-90-90 HIV Targets. http://healthycanadians.gc.ca/publications/diseases-conditions-maladies-affections/hiv-90-90-90-vih/index-eng.php Published 2016. Accessed.
- Greene, S., Ion, A., Elston, D., Kwaramba, G., Smith, S., Carvalhal, A., and Loutfy, M. (2015). “Why aren't You breastfeeding?”: How mothers living With HIV talk about infant feeding in a “breast Is best” world. Health Care for Women International, 36(8), 883–901. https://doi.org/10.1080/07399332.2014.888720
- Ion, A. (2019). Keeping secrets, disclosing health information: An institutional ethnography of the social organisation of perinatal care for women living with HIV in Canada. Culture, Health & Sexuality, 1–15.
- Ion, A., Wagner, A. C., Greene, S., & Loutfy, M. R. (2017). HIV-related stigma in pregnancy and early postpartum of mothers living with HIV in Ontario, Canada. AIDS Care, 29(2), 137–144. https://doi.org/10.1080/09540121.2016.1211608
- Kahlert, C., Aebi-Popp, K., Bernasconi, E., Martinez de Tejada, B., Nadal, D., Paioni, P., Rudin, C., Staehelin, C., Wagner, N., & Vernazza, P. (2018). Is breastfeeding an equipoise option in effectively treated HIV-infected mothers in a high-income setting? Swiss Medical Weekly, 148, w14648.
- Kaida, A.-O., Carter, A., Nicholson, V., Lemay, J., O'Brien, N., Greene, S., Tharao, W., Proulx-Boucher, K., Gormley, R., Benoit, A., Bernier, M., Thomas-Pavanel, J., Lewis, J., de Pokomandy, A., Loutfy, M., & On behalf of the CHIWOS Research Team. (n.d). Hiring, training, and supporting Peer Research Associates: Operationalizing community-based research principles within epidemiological studies by, with, and for women living with HIV. (1477-7517 (Electronic)).
- Khan, S., Tsang, K. K., Brophy, J., Kakkar, F., Logan Kennedy, V., Boucoiran, I., Yudin, M. H., Money, D., Read, S., & Bitnun, A. (2023). Canadian Paediatric and Perinatal HIV/AIDS Research Group consensus recommendations for infant feeding in the HIV context. Journal of the Association of Medical Microbiology and Infectious Disease Canada. https://doi.org/10.3138/jammi-2022-11-03
- Ladomenou, F., Kafatos, A., & Galanakis, E. (2007). Risk factors related to intention to breastfeed, early weaning and suboptimal duration of breastfeeding. Acta Paediatrica, 96(10), 1441–1444. https://doi.org/10.1111/j.1651-2227.2007.00472.x
- Levison, J., Weber, S., & Cohan, D. (2014). Breastfeeding and HIV-infected women in the United States: Harm reduction counseling strategies. Clinical Infectious Diseases, 59(2), 304–309. https://doi.org/10.1093/cid/ciu272
- Nachega, J. B., Uthman, O. A., Anderson, J., Peltzer, K., Wampold, S., Cotton, M., F., Mills, E., J., Ho, Y-S., Stringer, J, S. A., McIntyre, J., A., Mofenson, L., M., (2012). Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries. Aids (london, England), 26(16), 2039–2052. https://doi.org/10.1097/QAD.0b013e328359590f
- Nashid, N., Khan, S., Loutfy, M., MacGillivray, J., Yudin, M. H., Campbell, D. M., Barozzino, T., Baqi, M., Read, S. E., & Bitnun, A. (2020). Breastfeeding by women living With human immunodeficiency virus in a resource-rich setting: A case series of maternal and infant management and outcomes. Journal of the Pediatric Infectious Diseases Society, 9(2), 228–231. https://doi.org/10.1093/jpids/piz003
- Portman MP, H., Poole, O., & Wilson, J. (2013). Two HIV-positive breastfeeding mothers in the UK – their story. 9th Annual Conference of the British HIV Association (BHIVA), Manchester UK.
- Public Health Agency of Canada. (2018). Breastfeeding in Canada. https://www.canada.ca/en/public-health/services/publications/healthy-living/breastfeeding-infographic.html Published 2018. Accessed.
- Ramara, N. S., Maputle, M. S., & Lekhuleni, M. E. (2010). Infant feeding and HIV positive mothers in the capricorn district of Limpopo province. Curationis, 33(1), 5–16. https://doi.org/10.4102/curationis.v33i1.1000
- Sauve, LJSJ, Kakkar, F., Lee, T., Brophy, J., Money, D., Alimenti, A., Vaudry, W., Boucoiran, I., Comeau, J., Wong, A., & Bitnun, A., Canadian Perinatal HIV Surveillance Program (CPHSP) (2019). Prevention of vertical HIV transmission in Canada: A Canadian perinatal HIV surveillance program update. Paper presented at: Annual Canadian Conference of HIV Research, Saskatoon (Canada).
- Sibeko, L., Coutsoudis, A., Nzuza, S., & Gray-Donald, K. (2009). Mothers’ infant feeding experiences: Constraints and supports for optimal feeding in an HIV-impacted urban community in South Africa. Public Health Nutrition, 12(11), 1983–1990. https://doi.org/10.1017/S1368980009005199
- Tang, K., Wang, H., Tan, S. H., Xin, Y., Qu, X., Tang, T., Wang, Y., Liu, Y., & Gaoshan, J. (2019). Association between maternal education and breast feeding practices in China: A population-based cross-sectional study. BMJ Open, 9(8), e028485–e028485. https://doi.org/10.1136/bmjopen-2018-028485
- Tariq, S., Elford, J., Tookey, P., Anderson, J., de Ruiter, A., O'Connell, R., & Pillen, A. (2016). ““It pains me because as a woman you have to breastfeed your baby”: decision-making about infant feeding among African women living with HIV in the UK. Sexually Transmitted Infections, 92(5), 331–336. https://doi.org/10.1136/sextrans-2015-052224
- Tulloch, K. J., Dodin, P., Tremblay-Racine, F., Elwood, C., Money, D., & Boucoiran, I. (2019). Cabergoline: A review of its use in the inhibition of lactation for women living with HIV. Journal of the International AIDS Society, 22(6), e25322. https://doi.org/10.1002/jia2.25322
- Tuthill, E., McGrath, J., & Young, S. (2014). Commonalities and differences in infant feeding attitudes and practices in the context of HIV in sub-saharan Africa: A metasynthesis. AIDS Care, 26(2), 214–225. https://doi.org/10.1080/09540121.2013.813625
- Tuthill, E. L., Tomori, C., Van Natta, M., & Coleman, J. S. (2019). ““In the United States, we say, ‘No breastfeeding,’ but that is no longer realistic”: provider perspectives towards infant feeding among women living with HIV in the United States. Journal of the International AIDS Society, 22(1), e25224–e25224. https://doi.org/10.1002/jia2.25224
- United Nations Children’s Fund (UNICEF). (2018). Breastfeeding, A Mother’s Gift, for every child. https://www.unicef.org/publications/files/UNICEF_Breastfeeding_A_Mothers_Gift_for_Every_Child.pdf Published 2018. Accessed 2019/12/30.
- Waitt, C., Low, N., Van de Perre, P., Lyons, F., Loutfy, M., & Aebi-Popp, K. (2018). Does U=U for breastfeeding mothers and infants? Breastfeeding by mothers on effective treatment for HIV infection in high-income settings. The Lancet HIV, 5(9), e531–e536. https://doi.org/10.1016/S2352-3018(18)30098-5
- Webster, K., Carter, A., Proulx-Boucher, K., Dubuc, D., Nicholson, V., Beaver, K., Gasingirwa, C., Menard, B., O'Brien, N., Mitchell, K., Bajard, M. P., Ding, E., de Pokomandy, A., Loutfy, M., & Kaida, A. (2018). Strategies for recruiting women living with human immunodeficiency virus in community-based research: Lessons from Canada. Progress in Community Health Partnerships: Research, Education, and Action, 12(1), 21–34. https://doi.org/10.1353/cpr.2018.0003
- World Health Organization, United Nations Children’s Fund. (2016). Guideline: Updates on HIV and infant feeding: The duration of breastfeeding, and support from health services to improve feeding practices Among mothers living with HIV. World Health Organization 2016.
- World Heath Organization. (2010). Guidelines on HIV and infant feeding. Principles and recommendations for infant feeding in the context of HIV and a summary of evidence. http://apps.who.int/iris/bitstream/10665/44345/1/9789241599535_eng.pdf Published 2010. Accessed.
- Young, S. L., Mbuya, M. N. N., Chantry, C. J., Geubbels, E. P., Israel-Ballard, K., Cohan, D., Vosti, S. A., & Latham, M. C. (2011). Current knowledge and future research on infant feeding in the context of HIV: Basic, clinical, behavioral, and programmatic perspectives. Advances in Nutrition, 2(3), 225–243. https://doi.org/10.3945/an.110.000224
