ABSTRACT
Women living with HIV are reaching older age and experiencing menopause and age-related comorbidities. Data suggest that women living with HIV experience earlier menopause and more menopausal symptoms and age-related comorbidities compared to women without HIV. However, there are no guidelines on the screening for and management of age-related comorbidities and events in women living with HIV. Moreover, little is known about provision of care to this population across Europe. We surveyed 121 HIV healthcare providers in 25 World Health Organization European countries to ascertain screening practices for, and management of, menopause, psychosocial and sexual well-being and age-related comorbidities in women with HIV. Most respondents screened for diabetes, cardiovascular disease (CVD) risk factors and poor mental health at least annually. Low bone mineral density (BMD) was regularly checked but less than once a year. Fewer regularly screened for sexual well-being and intimate partner violence. Menstrual pattern and menopausal symptoms in women aged 45–54 were assessed by 67% and 59% of respondents. 44% stated that they were not confident assessing menopausal status and/or symptoms. CVD, diabetes, low BMD and poor mental health were managed mainly within HIV clinics, whereas menopause care was mainly provided by gynaecology or primary care. Most respondents stated a need for HIV and menopause guidelines. In conclusion, we found that whilst metabolic risk factors and poor mental health are regularly screened for, psychosocial and sexual well-being and menopausal symptoms could be improved. This highlights the need for international recommendations and clinician training to ensure the health of this population.
Introduction
Antiretroviral therapy (ART) has reduced HIV-associated morbidity and mortality and improved life expectancy (Antiretroviral Therapy Cohort Collaboration, Citation2008; Marcus et al., Citation2016). The proportion of people living with HIV who are aged over 50 years has increased, consequently leading to an increase in the incidence of age-related non-AIDS comorbidities and events (UNAIDS, Citation2013).
Women, who represent 53% of people living with HIV worldwide (UNAIDS, Citation2021), experience ageing differently to men both biologically and socially. According to the literature, there is a higher burden of cardiovascular, bone and neurocognitive disease in women living with HIV compared with HIV negative women. Traditional risk factors, such as hypertension, diabetes and dyslipidaemia, are common and often poorly managed (Raffe et al, Citation2022).
Estrogen depletion, a result of menopause, increases the risk of cardiovascular disease (CVD) and low bone mineral density (BMD) (Maas et al., Citation2021; Raisz, Citation2005). This is of particular significance in women living with HIV, who are at increased risk of CVD and low BMD compared to age-matched HIV-negative women and similarly aged men living with HIV (Chow et al., Citation2018; Collins et al., Citation2021; Cortés et al., Citation2015; Frazier et al., Citation2019). Furthermore, some studies suggest that women with HIV are more likely to experience menopause at an earlier age (Andany et al., Citation2020; Van Ommen et al., Citation2021), and that they have a high prevalence of menopausal symptoms such as vasomotor symptoms, sexual dysfunction and mood changes (Marcus et al., Citation2016; Pathak et al., Citation2019; Raisz, Citation2005; Toorabally et al., Citation2020). Recent research among women living with HIV has highlighted that severe menopausal symptoms are associated with reduced quality of life, poorer mental health, and poorer engagement in HIV care (Haag et al., Citation2022; Okhai et al., Citation2022; Solomon et al., Citation2021).
However, despite the increasing number of older women living with HIV and their documented increased risk of comorbidities and menopause-related symptoms, there is no European guideline on the screening for and management of age-related comorbidities and events in women living with HIV. Moreover, little is known about provision of care to this population in Europe. We aimed to describe current screening practices and management of menopause, psychosocial well-being and age-related comorbidities in women living with HIV among HIV healthcare providers (HCPs) in the World Health Organization (WHO) European Region.
Methods
Survey
We designed an online survey in English using the free and open source LimeSurvey tool (https://www.limesurvey.org/pt). Questions were developed by the Women Against Viruses in Europe (WAVE) comorbidities and ageing working group, which is part of the European AIDS Clinical Society (EACS) (Kowalska et al., Citation2018).
The questions were grouped into five sections: (1) demographic and work place characteristics of the responding HCPs; (2) screening and management of general health (blood pressure, weight, cardiovascular risk, diabetes risk, renal function, lipids, BMD) and psychosocial and sexual wellbeing; (3) cancer screening; (4) screening for and management of menopause; and (5) future recommendations (see supplementary information).
Screening frequency was assessed in two ways. Participants were asked if they performed routine screenings, defined as asking every woman, or every woman within specific age group, on a regular basis (e.g., once a year), regardless of clinical history. Participants were also asked to define screening frequency as: at every visit, at least once a year, regularly but less often than once a year, only if there are reasons for concern or not at all.
Recruitment
In June–August 2021, we disseminated the online survey link by email to all WAVE members, to potential participants in the authors’ clinical HIV networks. Anyone self-identifying as a healthcare provider managing people living with HIV in either private or public healthcare systems was eligible to participate. Responses were anonymous, and no personal identifying information was collected. Ethical approval was not required.
Data analysis
Descriptive data analysis was performed with R, version 4.2.0 (R Core Team, Citation2021). Frequency distributions were obtained using the “epiDisplay” package.
Results
Respondent and work place characteristics
This analysis is based on data from 121 respondents from 25 countries in the WHO European Region. The majority of HCPs were female (76%), doctors (97%), specializing in infectious diseases or genitourinary medicine (85%), with over ten years of experience post-qualification (80%) (). The most represented countries were United Kingdom (n = 19, 16%), Portugal (n = 17, 14%) and Italy (n = 11, 9%).
Table 1. Characteristics of participants.
Most respondents worked in HIV/sexual health/infectious diseases outpatient clinics (n = 105, 87%) in large cities (n = 93, 77%) with HIV clinic cohorts of >500 patients (n = 86, 71%). Women represented 26-50% of the clinic cohorts of 48% (n = 58) of respondents and 10-25% of the clinic cohorts of 37% (n = 45) of respondents. Importantly, 40% (n = 48) of respondents reported that 50% of women in their HIV clinic cohorts were aged 40 or above.
General health screening
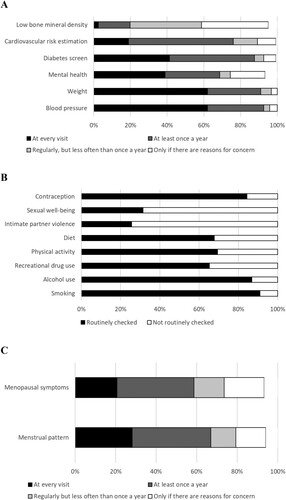
Blood pressure, weight and diabetes screening were performed by approximately 90% of participants (n = 112, 110 and 106, respectively) at every visit or at least once a year. CVD risk was assessed by 76% (n = 92) and mental health by 69% (n = 83). BMD was regularly checked but less than once a year by 39% (n = 47) or only if there were reasons to concern by 36% (n = 44) ((A)).
Figure 1. Proportions of respondents reporting routine screenings of general health (A) psychosocial and sexual wellbeing (B), menopausal status and menopausal symptoms in women aged 45–54 (C).
When participants were asked from what age they would routinely check for diabetes, cardiovascular risk and low BMD in women with HIV with no other risk factors, a relevant percentage of participants did not answer (41%, 37% and 35%, respectively). Most participants who answered would screen for diabetes and CVD risk in women aged ≥40 years (60% and 84% of 72 and 76 respondents, respectively), and for low BMD from 50 years old (58% of 79 respondents).
Fasting glucose (n = 70, 63%) and HbA1c (n = 62, 55%) were the most commonly used screening method for diabetes, Framingham CVD 5- and 10-year score (n = 63, 58%) for CVD risk, FRAX risk estimation tool and central DEXA (n = 34, 48% for both) for low BMD, and symptom enquiry (n = 77, 86%) for mental health.
Cervical screening was mainly performed within either HIV (n = 55, 46%) or gynecology clinics (n = 34, 28%), whereas breast cancer screening was largely undertaken as part of specific screening programs (n = 42, 35%) or in gynaecology clinics (n = 34, 28%).
Screening for psychosocial and sexual well-being
Respondents reported routinely enquiring about smoking, alcohol intake, recreational drug use, physical activity, diet, contraception and fertility intentions (all >65%). In contrast, routine enquiry of intimate partner violence (IPV) and sexual well-being were less common at 26% and 31%, respectively ((B)).
Screening for menopause
Two-thirds of respondents (n = 81) stated that they enquired about menstrual pattern at every visit or at least once a year in women aged 45–54 years (the expected age range for menopause) ((C)); 51% (n = 62) in those under 40, 60% (n = 73) in those aged 40–44 and 50% (n = 60) in those aged ≥55.
Almost 60% (n = 71) reported asking women aged 45–54 about menopausal symptoms at every year visit or at least once a year ((C)); whereas 24% (n = 29) enquired in women aged <40, 36% (n = 44) in those aged 40-44, and 50% (n = 60) in those aged ≥55.
Nearly half of the participants (44%, n = 53) reported not being confident in ascertaining menopausal status whilst 36% (n = 43) weren’t confident in assessing menopausal symptoms.
Menopausal status was mainly determined by symptoms and/or menstrual history by 79% (n = 96) of respondents for women aged ≥ 45 years, and by 59% (n = 71) of respondents for women aged <45 years. Laboratory tests were performed less frequently with Follicle stimulating hormone (FSH) levels being checked by 25% (n = 30) and 31% (n = 37) of respondents in women ≥ 45 and < 45 years-old, respectively, and Anti-Müllerian hormone (AMH) levels evaluated by 4% (n = 5) and 5% (n = 6) of respondents in women ≥ 45 and < 45 years-old, respectively. Two-fifths of respondents (n = 50) and 54% (n = 65) chose to refer to another clinician to confirm menopausal status in women aged ≥ 45 and < 45, respectively.
Management of comorbidities and menopause
Mental health conditions (n = 57, 47%), CVD (n = 54, 45%), low BMD (n = 53, 44%) and diabetes (n = 43, 36%) were mainly managed within HIV services or joint HIV/specialist clinics (). However, women living with HIV with menopausal symptoms were rarely managed within the HIV service (n = 8, 7%) or a joint HIV/specialist service (n = 19, 16%). Instead, women with HIV were mainly referred to mainly either specialist services (n = 62, 51%) or primary care (n = 27, 22%) for management of menopausal symptoms (). Of note, only 35% (n = 42) of respondents reported that their HIV services provided dedicated gynaecology services for women living with HIV; an even smaller number (n = 13, 11%) had specific HIV and menopause services they could refer into. The majority of respondents said that their clinics provided information to women living with HIV who had menopausal symptoms (n = 91, 75%), although few provided psychological or peer/community support (n = 43, 36% and n = 20, 17%, respectively). Only 15% (n = 18) routinely provided medical treatment for menopause symptoms (i.e., menopausal hormone therapy (MHT)).
Figure 2. Proportions of respondents reporting different arrangements for managing comorbidities and menopausal symptoms in women living with HIV.
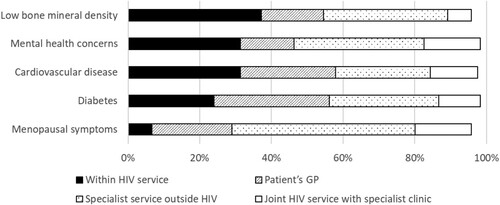
Respondents reported being more aware of women self-referring to private healthcare providers for mental health concerns (n = 29, 24%) and menopause (n = 20, 17%), but less so for age-related comorbidities such as diabetes (n = 7, 6%), CVD (n = 8, 7%) or low BMD (n = 9, 7%).
Approximately half of all respondents followed national or local/institutional guidelines for menopause screening (n = 60, 50%) and managing menopausal symptoms (n = 57, 47%); fewer used guidelines specifically mentioning women living with HIV (n = 34, 28% for menopause screening; n = 29, 24% for menopause symptoms management). Specific guidance on use of systemic MHT and topical vaginal estrogen in women living with HIV was limited; 15% (n = 18) and 7% (n = 9) of respondents reported that guidelines covered these treatment modalities, respectively.
The overwhelming majority of respondents (n = 107, 88%) stated that they would welcome specific European menopause guidelines or recommendations for women living with HIV.
Discussion
In this survey of 121 HIV HCPs in 25 WHO European countries, we have found that age-related comorbidities such as diabetes and CVD, and mental health were routinely screened at least once a year in women living with HIV. Bone mineral density was also regularly screened but less than once a year. Enquiry rates for partner violence and sexual wellbeing were lower than those for smoking, alcohol, recreational drugs, physical activity, diet and contraception/plans for parenthood. Menopausal status and symptoms were routinely assessed by most respondents; however, a significant proportion of HCPs did not feel confident in this.
The EACS guidelines dedicates a brief section to menopause and general health risk assessment (cancer, BMD, CVD risk, mental health) in women aged > 40 (European AIDS Clinical Society, Citation2021). In agreement with EACS recommendations, CVD risk was assessed at least once a year using the Framingham risk score by most of respondents. Likewise, low BMD was mainly evaluated using the FRAX tool although it has been reported that FRAX might underestimate fracture risk in people living with HIV (Mazzitelli et al., Citation2022). Most participants assessed low BMD from 50 years old. EACS recommends screening from age 40 and the British HIVA Association (BIHVA) from 50 years of age onwards (British HIV Association, Citation2017). Mental health was mainly assessed through symptom enquiry rather than validated questionnaires (i.e., patient health questionnaire, general health questionnaire, hospital anxiety and depression scale). Since the use of such surveys requires specialist guidance, our results might reflect the lack of integrated psychiatry services in HIV clinics.
EACS guideline recommends screening for menopause yearly in women aged > 40 using a validated menopause symptom questionnaire (i.e., Menopause Rating Scale, Greene Climacteric Scale) (European AIDS Clinical Society, Citation2021). Accordingly, most respondents assessed symptoms rather than biochemical parameters. However, one-in-four respondents reported using serum FSH to diagnose menopause in women aged >45; guidance in the general population is that menopause in women aged >45 does not recommend FSH testing (National Institute for Health and Care Excellence, Citation2015). A recent study in women living with HIV provides evidence that FSH testing is unnecessary in women living with HIV aged >45 with an undetectable HIV viral load who are amenorrhoeic (Tariq et al., Citation2022).
There appears to be a significant gap in provision of dedicated HIV and menopause services, psychological support, peer support and menopausal hormone therapy to women living with HIV transitioning through the menopause, despite the increase in numbers of women in this age group. Age-related comorbidities and poor mental health were mainly managed within HIV clinics (including in dedicated HIV/specialist services). In contrast, menopause care was rarely provided within HIV services, with patients instead being referred to gynaecology or primary care. Despite the fact that UK HIV guidelines recommend that menopausal women with HIV are managed in primary care (as it is in the general population), general practitioners have little experience of managing menopause in women living with HIV. Many are concerned about potential drug–drug interactions and the possibility of missing an HIV-related diagnosis (Chirwa et al., Citation2017). With HIV clinics not routinely providing menopause care and instead directing women to primary care who may also feel ill-equipped to provide management, it is likely that menopausal women living with HIV may not have their healthcare needs addressed.
The EACS guidelines recommends topical (vaginal) estrogen in all women given the positive effects on sexual health and urogenital symptoms but there is no guidance on when to prescribe systemic hormone therapy or specifically what to prescribe. The British HIV Association (BHIVA) guidelines (British HIV Association, Citation2017) recommends use of MHT as per UK National Institute of Health and Care Excellence (NICE) guidelines (National Institute for Health and Care Excellence, Citation2015). In this study, 14% of respondents routinely provided medical treatment for menopause to women with HIV (i.e., MHT). Previous studies have reported low rates of MHT use among women living with HIV (Fantry et al., Citation2005; Okhai et al., Citation2021; Samuel et al., Citation2014); improving provision of MHT within HIV services is likely to result in more women accessing treatment.
Almost all HCPs in our study stated a need for European HIV and menopause guidelines or recommendations. EACS (European AIDS Clinical Society, Citation2021) and the BHIVA (British HIV Association, Citation2017) include brief sections on menopause, and the British Menopause Society has produced a clinician toolkit to support primary care in managing menopause in women living with HIV (Tariq, Citation2019). However, these guidelines are limited in scope and could be strengthened by providing more detail on management of menopausal symptoms i.e., specific guidance on what MHT to start and when, and how to manage drug interactions. It is important to note that guidelines on screening and management of age-related co-morbidities in HIV exist. Our findings suggest that it is important to raise awareness of the importance of screening women for comorbid conditions such as low BMD and CVD, and psychosocial and sexual factors to ensure they benefit from timely assessment and appropriate management.
This is one of the first studies to ascertain current practice in screening and management of co-morbidities, psychosocial wellbeing and menopause in women living with HIV, among HCPs across WHO European region. We have representation from 25 of the 53 WHO European countries and have taken a holistic approach to women’s health including comorbidity risk, psychosocial well-being and post-reproductive health. However, the study is limited by its small size and potential selection bias. Participants were recruited through WAVE (a small group of HCPs with an interest in women and HIV) and their colleagues, which is likely to have led to sampling bias. Furthermore, those with experience or interest in managing women living with HIV may have been more likely to participate. Also, participants were mainly urban practitioners from large clinical centers, which likely have more specialties than other clinics. Therefore, our findings are likely not to be representative of the wider group of HCPs working in HIV in the whole WHO European region, and instead is potentially a “best case scenario” overestimated. There is also likely to be clustering of responses; respondent driven sampling would have led to respondents recruiting colleagues who are likely to have similar practices.
However, this survey study provides some important insights into current practices in management of women living with HIV and identifies likely unmet need. It emphasizes the importance of developing comprehensive guidelines on management of menopause in this population, as well as highlighting the need for training of HCPs in screening and management of low BMD, menopause and psychosocial and sexual wellbeing. It is imperative that HCPs work across Europe in partnership with women living with HIV to generate guidance and training in order to ensure the fourth 90 of UNAIDS targets in this population across the life-course (Webster, Citation2019).
Acknowledgements
We would like to thank Hilary Curtis (Independent consultant) for her work developing and analysing the survey. We are also grateful to our participants for providing the data this analysis is based on.
Disclosure statement
AH’s institution has received travel grants, congress and advisory fees from MSD, Viiv and Gilead, unrelated to this work. GL received speaker and advisory honoraria from Gilead Sciences, ViiV Healthcare and MSD, unrelated to this publication. NN is an employee of ViiV Healthcare and holds GSK stock and stock options. ST received speaker honoraria and funding for preparation of educational materials from Gilead Sciences. UC received congress and advisory fees from Gilead and Jansen, unrelated to this work. No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Andany, N., Kaida, A., De Pokomandy, A., Yudin, M. H., Wang, L., Kennedy, V. L., Webster, K., & Loutfy, M. (2020). Prevalence and correlates of early-onset menopause among women living with HIV in Canada. Menopause, 27(1), 66–75. https://doi.org/10.1097/GME.0000000000001423
- Antiretroviral Therapy Cohort Collaboration. (2008). Life expectancy of individuals on combination antiretroviral therapy in high-income countries: A collaborative analysis of 14 cohort studies. The Lancet, 372(9635), 293–299. https://doi.org/10.1016/S0140-6736(08)61113-7.
- British HIV Association. (2017). BHIVA/BASHH/FSRH guidelines for the sexual & reproductive health of people living with HIV. https://www.bhiva.org/srh-guidelines
- Chirwa, M., Ma, R., Guallar, C., & Tariq, S. (2017). Managing menopause in women living with HIV: A survey of primary care practitioners. Post Reproductive Health, 23(3), 111–115. https://doi.org/10.1177/2053369117712181
- Chow, F. C., Regan, S., Zanni, M. V., Looby, S. E., Bushnell, C. D., Meigs, J. B., Grinspoon, S. K., Feske, S. K., & Triant, V. A. (2018). Elevated ischemic stroke risk among women living with HIV infection. AIDS, 32(1), 59–67. https://doi.org/10.1097/QAD.0000000000001650
- Collins, L. F., Sheth, A. N., Mehta, C. C., Naggie, S., Golub, E. T., Anastos, K., French, A. L., Kassaye, S., Taylor, T. N., Fischl, M. A., Adimora, A. A., Kempf, M. C., Palella, F. J., Tien, P. C., & Ofotokun, I. (2021). Incident Non-AIDS comorbidity burden Among women With or at risk for human immunodeficiency virus in the United States. Clinical Infectious Diseases, 73(7), e2059–e2069. https://doi.org/10.1093/cid/ciaa1928
- Cortés, Y. I., Yin, M. T., & Reame, N. K. (2015). Bone density and fractures in HIV-infected postmenopausal women: A systematic review. Journal of the Association of Nurses in AIDS Care, 26(4), 387–398. https://doi.org/10.1016/j.jana.2015.03.005
- European AIDS Clinical Society. (2021). EACS guidelines version 11.0.
- Fantry, L. E., Zhan, M., Taylor, G. H., Sill, A. M., & Flaws, J. A. (2005). Age of menopause and menopausal symptoms in HIV-infected women. AIDS Patient Care and STDs, 19(11), 703–711. https://doi.org/10.1089/apc.2005.19.703
- Frazier, E. L., Sutton, M. Y., Tie, Y., Fagan, J., & Fanfair, R. N. (2019). Differences by Sex in cardiovascular comorbid conditions among older adults (aged 50–64 or ≥65 years) receiving care for human immunodeficiency virus. Clinical Infectious Diseases, 69(12), 2091–2100. https://doi.org/10.1093/cid/ciz126
- Haag, K., Tariq, S., Dhairyawan, R., Sabin, C., Okhai, H., Gilson, R., Burns, F., & Sherr, L. (2022). Patterns of mental health symptoms among women living with HIV ages 45-60 in England: Associations with demographic and clinical factors. Menopause, 29(4), 421–429. https://doi.org/10.1097/GME.0000000000001931
- Kowalska, J. D., Aebi-Popp, K., Loutfy, M., Post, F. A., Perez-Elias, M. J., Johnson, M., & Mulcahy, F. (2018). Promoting high standards of care for women living with HIV: Position statement from the Women Against Viruses in Europe Working Group. HIV Medicine, 19(2), 167–173. https://doi.org/10.1111/hiv.12565
- Maas, A. H. E. M., Rosano, G., Cifkova, R., Chieffo, A., van Dijken, D., Hamoda, H., Kunadian, V., Laan, E., Lambrinoudaki, I., Maclaran, K., Panay, N., Stevenson, J. C., van Trotsenburg, M., & Collins, P. (2021). Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: A consensus document from European cardiologists, gynaecologists, and endocrinologists. European Heart Journal, 42(10), 967–984. https://doi.org/10.1093/eurheartj/ehaa1044
- Marcus, J. L., Chao, C. R., Leyden, W. A., Xu, L., Quesenberry, C. P., Klein, D. B., Towner, W. J., Horberg, M. A., & Silverberg, M. J. (2016). Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. JAIDS Journal of Acquired Immune Deficiency Syndromes, 73(1), 39–46. https://doi.org/10.1097/QAI.0000000000001014
- Mazzitelli, M., Branca Isabel, P., Muramatsu, T., Chirwa, M., Mandalia, S., Moyle, G., Marta, B., & Milinkovic, A. (2022). FRAX assessment in people ageing with HIV. HIV Medicine, 23(1), 103–108. https://doi.org/10.1111/hiv.13170
- National Institute for Health and Care Excellence. (2015). Menopause: Diagnosis and management. www.nice.org.uk/guidance/ng23
- Okhai, H., Dragomir, L., Pool, E. R., Sabin, C. A., Miners, A., Sherr, L., Haag, K., Dhairyawan, R., Vora, N., Sultan, B., Gilson, R., Burns, F., Gilleece, Y., Jones, R., Post, F., Ross, J., Ustianowski, A., & Tariq, S. (2022). Association between health-related quality of life and menopausal status and symptoms in women living with HIV aged 45–60 years in England: An analysis of the PRIME study. Women’s Health, 18. https://doi.org/10.1177/17455065211068722
- Okhai, H., Sabin, C. A., Haag, K., Sherr, L., Dhairyawan, R., Burns, F., Gilson, R., Post, F., Ross, J., Mackie, N., Sullivan, A., Shepherd, J., Tariq, A., Jones, R., Fox, J., Rosenvinge, M., & Tariq, S. (2021). Menopausal status, age and management among women living with HIV in the UK. HIV Medicine, 22(9), 834–842. https://doi.org/10.1111/hiv.13138
- Pathak, N., Dhairyawan, R., & Tariq, S. (2019). The experience of intimate partner violence among older women: A narrative review. Maturitas, 121, 63–75. https://doi.org/10.1016/j.maturitas.2018.12.011
- Raffe, S., Sabin, C., & Gilleece, Y. (2022). Comorbidities in women living with HIV: A systematic review. HIV Medicine, 23(4), 331–361. https://doi.org/10.1111/hiv.13240
- Raisz, L. G. (2005). Pathogenesis of osteoporosis: Concepts, conflicts, and prospects. Journal of Clinical Investigation, 115(12), 3318–3325. https://doi.org/10.1172/JCI27071
- R Core Team. (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.r-project.org/
- Samuel, M., Welch, J., Tenant-Flowers, M., Poulton, M., Campbell, L., & Taylor, C. (2014). Care of HIV-positive women aged 50 and over – Can we do better? International Journal of STD & AIDS, 25(4), 303–305. https://doi.org/10.1177/0956462413504553
- Solomon, D., Sabin, C. A., Burns, F., Gilson, R., Allan, S., de Ruiter, A., Dhairyawan, R., Fox, J., Gilleece, Y., Jones, R., Post, F., Reeves, I., Ross, J., Ustianowski, A., Shepherd, J., & Tariq, S. (2021). The association between severe menopausal symptoms and engagement with HIV care and treatment in women living with HIV. AIDS Care, 33(1), 101–108. https://doi.org/10.1080/09540121.2020.1748559
- Tariq, S. (2019). British menopause society tools for clinicians: HIV and the menopause. Post Reproductive Health, 25(1), 38–39. https://doi.org/10.1177/2053369119833884
- Tariq, S., Okhai, H., Severn, A., Sabin, C. A., Burns, F., Gilson, R., Fox, J., Gilleece, Y., Mackie, N. E., Post, F. A., Reeves, I., Rosenvinge, M., Sullivan, A., Ustianowski, A., & Miller, R. F. (2022). Follicle-stimulating hormone in postmenopausal women living with HIV: A prevalence study. HIV Medicine, 23(4), 434–440. https://doi.org/10.1111/hiv.13205
- Toorabally, N., Mercer, C. H., Mitchell, K. R., Blell, M., Burns, F., Gilson, R., McGregor-Read, J., Allan, S., De Ruiter, A., Dhairyawan, R., Fox, J., Gilleece, Y., Jones, R., Mackie, N., Obeyesekera, S., Post, F., Reeves, I., Rosenvinge, M., Ross, J., … Tariq, S. (2020). Association of HIV status with sexual function in women aged 45–60 in England: Results from two national surveys. AIDS Care, 32(3), 286–295. https://doi.org/10.1080/09540121.2019.1653436
- UNAIDS. (2013). HIV and aging: UNAIDS. https://www.unaids.org/sites/default/files/web_story/20131101_PR_HIV_and_Aging_en_0.pdf
- UNAIDS. (2021). UNAIDS data 2021. In UNAIDS. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
- Van Ommen, C. E., King, E. M., & Murray, M. C. M. (2021). Age at menopause in women living with HIV: A systematic review. Menopause, 28(12), 1428–1436. https://doi.org/10.1097/GME.0000000000001871
- Webster, P. (2019). UNAIDS survey aligns with so-called fourth 90 for HIV/AIDS. The Lancet, 393(10187), 2188. https://doi.org/10.1016/S0140-6736(19)31231-0
