Abstract
People with severe mental illness (SMI) have high prevalence of lifetime victimization, but little is known about the extent and risk of recent domestic/sexual violence. The objective was to synthesize evidence on prevalence, odds, and risk factors for recent violence against people with SMI, with a focus on domestic and sexual violence. Relevant studies were identified through literature searches in Medline, Psychinf, Embase (for studies published in 2010–2015), and through existing systematic reviews (for studies published in 2000–2014). The review included 30 studies (with 16 140 SMI participants), including six on domestic violence and 11 on sexual violence. Prevalence of recent domestic violence ranged from 15–22% among women and from 4–10% among men/mixed samples; with little evidence on risk compared with the general population. Median prevalence of sexual violence was 9.9% (IQR = 5.9–18.1%) in women and 3.1% (IQR = 2.5–6.7%) in men; with 6-fold higher odds of victimization compared with the general population. There was little evidence on risk factors for domestic or sexual violence. In conclusion, people with SMI have a high prevalence of recent domestic and sexual violence, but little is known about risk factors for these violence types, or extent of domestic violence victimization compared to the general population.
Introduction
Domestic and sexual violence are important public health problems, with well-established associations with mental ill health (Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, Citation2008; World Health Organization, Citation2013). Evidence from longitudinal studies suggests that the relationship is likely to be bi-directional, with intimate partner violence (IPV) being associated with incident depression, and conversely depression being associated with incident IPV (Devries et al., Citation2013). The extent and correlates of recent violence against people with pre-existing mental disorders are important from public health and clinical perspectives, since victimization is associated with poorer quality-of-life and greater treatment resistance among psychiatric patients (Mueser, Rosenberg, Goodman, & Trumbetta, Citation2002; Neria, Bromet, Carlson, & Naz, Citation2005); and health professionals are well placed to detect and address victimization (Howard et al., Citation2010; NICE, Citation2014). This review focuses on recent physical and sexual violence against people with severe mental illness (SMI), including violence perpetrated by partner or family members (domestic violence) as well as violence perpetrated by strangers or acquaintances (community violence). People with SMI may be particularly vulnerable to victimization (Hiday, Swartz, Swanson, Borum, & Wagner, Citation1999; Khalifeh, Johnson, et al., Citation2015; Latalova, Kamaradova, & Prasko, Citation2014; Maniglio, Citation2009; Teplin, McClelland, Abram, & Weiner, Citation2005) and their contact with psychiatric services provides a window of opportunity for intervention (Howard et al., Citation2010).
A recent systematic review on violence against people with diagnosed psychiatric disorders found a high prevalence and increased odds of adulthood and recent domestic violence against people with depressive disorders, anxiety and PTSD, with limited evidence for other diagnoses (Trevillion, Oram, Feder, & Howard, Citation2012). A systematic review on domestic violence against psychiatric patients estimated that a third of patients had been victims of adulthood domestic violence, but there was limited evidence for male patients and for recent victimization, and no comparative studies were identified (Oram, Trevillion, Feder, & Howard, Citation2013). Hughes et al. (Citation2012) systematically reviewed the evidence on prevalence and risk of past-year physical or sexual violence by any perpetrator against people with disabilities—including people with common mental disorder or severe mental illness (SMI)—and estimated that around a quarter of people with mental illness had experienced recent physical violence—a 4-fold increased risk compared to those without mental illness—around 6% had experienced recent sexual violence and nearly 40% had experienced recent IPV. However, the above reviews had a number of limitations. They did not examine risk factors for victimization, and, due to data limitations, they did not examine victimization stratified by gender. These are important gaps, since a better understanding of victimization risk by gender and of the relative importance of different risk factor domains (e.g. socio-demographic vs clinical) is needed for developing effective, gender-sensitive interventions.
This systematic review aims to address the evidence gaps outlined above. The study objectives were: (1) to synthesize the evidence on the prevalence and relative odds of recent violence against people with SMI, stratified by gender; including (a) physical or sexual violence by any perpetrator; (b) physical or sexual domestic violence; and (2) to synthesize the evidence on risk factors for violence victimization among people with SMI (with a focus on risk factors for domestic or sexual violence). Relevant studies published in 2000–2015 were identified from published systematic reviews, and from a primary search of the literature for studies published in the period 2010–2015.
Methods
PRISMA and STROBE guidelines were followed (Liberati et al., Citation2009; Vandenbroucke et al., Citation2007).
Definitions of SMI and violence
Severe mental illness (SMI) was defined as either (a) having a psychotic disorder (i.e. schizophrenia, schizoaffective disorder, bipolar disorder, or depressive disorder with psychotic symptoms); measured using a validated diagnostic instrument or from clinical records; or (b) being under the care of secondary mental health services.
Violence was defined as any physical or sexual violence by any perpetrator, including (a) violence perpetrated by partners/ex-partner/family members (domestic violence) or (b) violence perpetrated by strangers or acquaintances (community violence). Sexual violence was defined as sexual harassment, unwanted sexual touching, rape or attempted rape by any perpetrator.
Recent violence was defined as violence occurring within the past 3 years. This was guided by the definition of ‘recent violence’ in relevant published studies, with most studies including violence occurring within the past 12 months, but a few studies including violence occurring within a longer time period of up to 3 years.
Study selection criteria
Study inclusion criteria were: (1) Randomized controlled trial (RCT), case-control, cross-sectional, or cohort study published in a peer-reviewed journal; (2) reported on prevalence or risk factors for recent physical or sexual violence against people with SMI (occurring within the past 3 years); (3) reported on experiences of people aged over 18; (4) written in English; and (5) published in the period 1 January 2000–17 February 2015. For odds estimates, an additional inclusion criterion was that the study reported on relative risk or odds of being a victim of recent violence among adults with vs those without SMI (or reported data from which this could be estimated). Studies were excluded if they (a) reported on any criminal victimization without separately reporting on violence, (b) included people with any mental illness (e.g. common mental disorders), without separately reporting on people with SMI, (c) did not specify whether violence was experienced in childhood (aged <16) or adulthood (age >16), (d) focused on selected populations (e.g. prisoners, homeless people, immigrants, forensic population, domestic violence shelter attendees, women with perinatal psychiatric disorders), or (e) would result in duplication of included data (for studies with multiple reports we included the study with the largest sample size).
Search strategy, data extraction, and quality measures
Studies were identified using two methods: (1) from a search of the primary literature for studies published in 2010–2015 (using the methods detailed below); (2) from five published systematic reviews on violence against people with SMI for studies published from 2000–2014 (Hughes et al., Citation2012; Latalova et al., Citation2014; Maniglio, Citation2009; Oram et al., Citation2013; Trevillion et al., Citation2012) This was supplemented by screening reference lists of retrieved studies.
Medline, Embase, and Psychinfo were searched for primary research studies published between 1 January 2010 and 17 February 2015 that reported on prevalence or relative odds/risk of violence against people with SMI in adulthood. A search strategy was developed and adapted for each database, including free text and index terms (see Appendix). Search terms were developed for the two categories of ‘severe mental illness’ ((mental* or psychiatric*) adj2 (ill or illness* or disorder* or patient*)) or (schiz* or bipolar or psychos* or psychot*) and ‘violence victimization’ ((viol* or assault* or abus* or agressi* or maltreat* or rape*) and (victim* or against)).
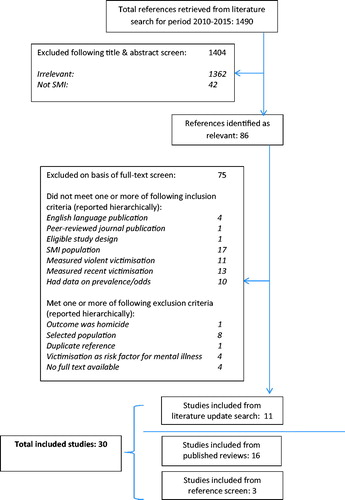
References were managed using Endnote. One reviewer screened the titles/abstracts of all references for potential relevance and excluded studies which were clearly irrelevant or which clearly met one or more exclusion criteria. The reason for study exclusion was recorded, using a hierarchical list of inclusion/exclusion criteria (see ). A second reviewer assessed 10% of excluded studies and any disagreements re-exclusion were resolved by consensus. Two reviewers assessed the remaining references for eligibility for inclusion using full-text screening. A standard electronic form was used to extract data on all included studies, including data on study design and methods, population, outcomes (prevalence and risk), risk factors and quality-related measures.
Study quality was based on international standards, with an emphasis on standards to assess for bias and confounding in observational studies (Vandenbroucke et al., Citation2007). Six quality criteria were used for prevalence studies, and a further six criteria for comparative studies, with a maximum score of 12 for each (see Table S2). Studies which provided both prevalence and comparative data were assigned two separate quality scores. Study quality was assessed by two reviewers (with disagreements resolved by consensus). Study quality was used in the analysis by stratifying on total quality score and on individual quality measures in sub-group meta-analyses (since the total score can be biased and may fail to reflect the global quality of a study) (Higgins & Green, Citation2011).
Risk factor analyses
Risk factors were grouped into the following six domains: demographic, social, clinical, substance misuse, violence perpetration and childhood abuse. This was based on the World Health Organization’s violence conceptual framework (Krug, Citation2002), and on past research on key risk factors for violence in the general population and among people with SMI (Abramsky et al., Citation2011; Maniglio, Citation2009; Witt, van Dorn, & Fazel, Citation2013). For each study, information was extracted about risk factors reported in univariate and multivariate analyses, including: (a) total number and number victimized among those with and without a given risk factor; (b) reported crude and adjusted ORs (with 95% confidence intervals/standard errors); and (c) risk factor domains included in the multivariate analyses. Where ORs were not reported, information was extracted on whether a given factor was reported as being associated or not with victimization, and the related p-value. For odds ratios reported in the text, the following qualitative descriptions were used: weak (OR = 1.2–1.5), moderate (OR = 1.6–2.5), and strong (OR >2.5).
Heterogeneity analyses
The factors that could explain heterogeneity in the estimates of victimization prevalence/risk were grouped into the following four domains: (a) study design & setting: design, country, clinical setting (inpatient vs outpatient); (b) study population: gender (operationalized as percentage male) and diagnosis (operationalized as percentage with schizophrenia); (c) violence measures: violence timeframe, type (physical or sexual vs physical only) and measure (long structured questionnaire vs brief questionnaire); and (d) study quality: sampling method, response rate, total number of participants, and total quality score.
Statistical analysis
Victimization prevalence was estimated using raw data. Exact binomial confidence intervals were calculated using the Clopper-Pearson method (a standard method for estimating confidence intervals based on proportions, using the binomial distribution) (Clopper & Pearson, Citation1934). Crude odds ratios (for victimization in people with vs without SMI (and for victimization among SMI people with vs without a given risk factor) were estimated using raw data where possible. Confidence intervals were calculated using Woolf’s formula (a standard method for calculating confidence intervals based on ln(OR)) (Kirkwood & Sterne, Citation2003a). Where raw data was not available, the published ORs and their confidence intervals (CIs)/standard errors (SEs) were used. Where CIs/SEs were not reported but p-values were given, the SEs were calculated by converting p-values to z-values and then calculating the standard errors (Deeks, Higgins, & Altman, Citation2011). Meta-analyses were conducted using STATA version 12. Pooled prevalence and pooled ORs (with 95% CI) were estimated using a random effects model. This model was used since there was wide variation in the settings, populations and measures of SMI/violence in the included studies—such that the true effect was likely to vary between studies (Kirkwood & Sterne, Citation2003a). The Stata metan command was used, which employs the DerSimonian and Laird method (DerSimonian & Laird, Citation1986). Meta-analyses were only conducted where three or more studies reported a given estimate. Forest plots were used to graphically display study and pooled estimates, with 95% CIs. Based on past reviews, it was anticipated that the meta-analyses would show a high degree of heterogeneity (Hughes et al., Citation2012). In this review, meta-analyses were carried out and presented even where heterogeneity was high—in order to describe the extent of heterogeneity and to explore its potential sources. Heterogeneity for prevalence/risk estimates was tested using the I2 statistic (reported with 95% CI). This estimates the proportion of variation across studies due to heterogeneity between study effect estimates rather than chance (Deeks et al., Citation2011). Potential sources of heterogeneity were explored using random-effects meta-analyses stratified by relevant sub-groups and by inspection of related forest plots. It is recognized that, where heterogeneity is high, the pooled estimate is unlikely to be a valid summary of individual study findings and that the individual study estimates need to be inspected.
Risk of publication bias was assessed using funnel plots and Peter’s test for odds ratio estimates (Peters, Sutton, Jones, Abrams, & Rushton, Citation2006).
Results
Included studies
shows the study selection flowchart. Thirty studies on recent violence by any perpetrator against people with SMI were identified, with a total of 16 140 participants with SMI. Details of all included studies are given in , and their characteristics are summarized in . Of these 30 studies, six studies reported on recent domestic violence (DV); including three studies that reported exclusively on intimate partner violence (Chang et al., Citation2011; McPherson, Delva, & Cranford, Citation2007; Morgan, Zolese, McNulty, & Gebhardt, Citation2010) and three studies that reported separately on domestic and community (see ) (Bengtsson-Tops & Ehliasson, Citation2012; Katsikidou et al., Citation2013; Khalifeh, Moran, et al., Citation2015).
Table 1. Details of all included studies.
Table 2. Summary of characteristics of prevalence studies.
Table 4. Prevalence of recent domestic violence (partner violence (PV) or family violence (FV)).
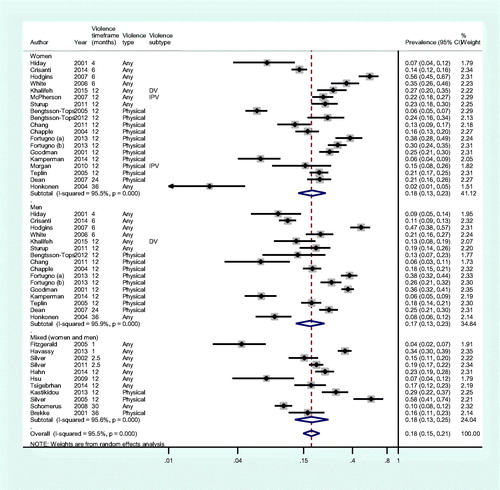
Prevalence and odds of any or physical violence(all perpetrators)
For this analysis where data were reported separately for physical and sexual violence we used prevalence for physical violence, otherwise we used prevalence for any (physical or sexual) violence. Thirty studies reported on prevalence of any/physical violence (regardless of perpetrator). The results are shown in and in , stratified by patient gender where this data were available. The 30 studies included a total of 16 140 participants, 2702 (16.7%) of whom reported being a victim of any/physical violence (median prevalence = 18.6%, interquartile range (IQR) = 10.9–26.2%). The median prevalence of any/physical victimization was 20.7% in women (IQR = 12.6–27.1%) and 17.8% in men (IQR = 9.9–25.6%). Pooled prevalence is shown in , but heterogeneity was high so this was unlikely to be a valid summary of individual study estimates. There was no evidence that any of the variables examined (relating to study design & setting, population, violence measures and study quality) accounted for the heterogeneity in prevalence estimates. The pooled crude OR of any/physical victimization in women compared with men was 1.1 (CI = 0.90–1.4, p = .31; I2 = 72%; n = 16 studies), suggesting a lack of association with gender.
Figure 2. Meta-analysis: prevalence of any or physical violence, stratified by gender where data available.
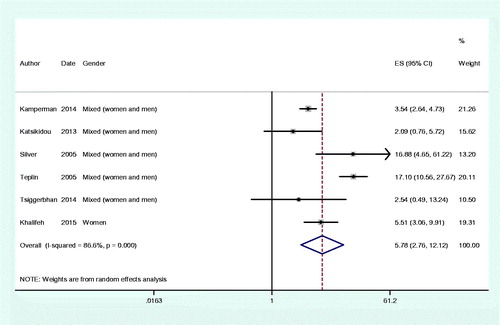
Nine studies reported odds for any/physical victimization in people with vs without SMI. Results are shown in and (in the latter stratified by gender where data were available). These studies included a total of 3403 people with SMI and 106 328 people without SMI. All studies showed increased crude odds of victimization among people with vs those without SMI; including studies of women with vs without SMI (pooled crude OR = 9.2, CI = 3.2–26.7, I2 = 95%; n = 3 studies), of men with vs without SMI (pooled crude OR = 5.4, CI = 2.2–13.1, I2 = 92%; n = 3 studies) and of men or women with vs without SMI (pooled crude OR = 5.6, CI = 3.7–8.6, I2 = 74%; n = 6 studies).
Figure 3. Meta-analysis: crude OR for any or physical victimization in people with compared with those without SMI.
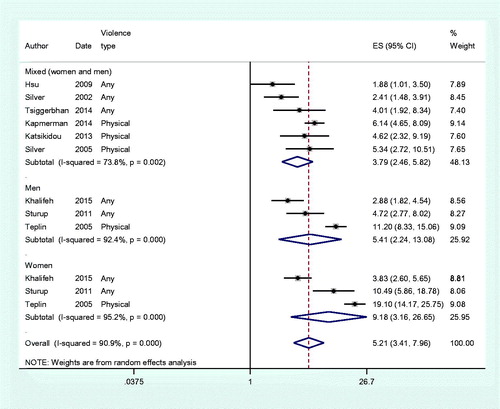
Table 3. Details of comparative studies (on victimization among people with vs without SMI).
Prevalence and odds of any or physical domestic violence
Six studies reported on past-year violence perpetrated by family members and/or partners (see and ). The results are difficult to synthesize quantitatively due to heterogeneity in violence definitions and victim gender. Three studies reported the prevalence of DV against women (prevalence range = 15–22%) (Khalifeh, Moran, et al., Citation2015; McPherson et al., Citation2007; Morgan et al., Citation2010); three studies reported the prevalence of DV against men or women (prevalence range = 3–15%) (Bengtsson-Tops & Ehliasson, Citation2012; Chang et al., Citation2011; Katsikidou et al., Citation2013) and only one study reported prevalence of DV against men (6% for family violence and 9% for partner violence) (Khalifeh, Moran, et al., Citation2015). Two studies reported findings separately for partner and family violence, and found similar prevalence for these violence sub-types (Bengtsson-Tops & Ehliasson, Citation2012; Khalifeh, Moran, et al., Citation2015).
Figure 4. Meta-analysis: prevalence of any or physical domestic violence (perpetrated by partner or family member).
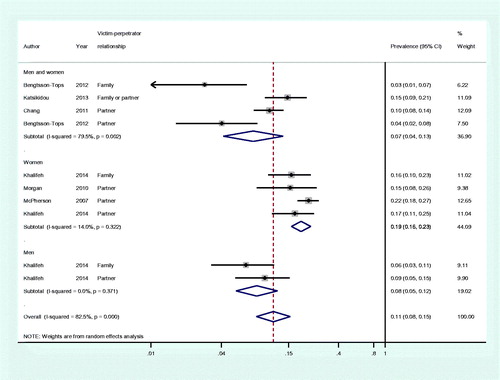
Only two studies reported odds of DV in people with SMI compared with the general population; with one UK study reporting 3–7-fold higher odds (Khalifeh, Moran, et al., Citation2015); and one Greek study reporting 22-fold higher odds (Katsikidou et al., Citation2013).
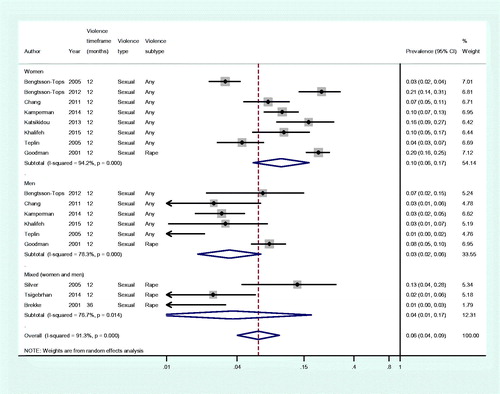
Prevalence and odds of sexual violence(all perpetrators)
The prevalence of sexual victimization (regardless of perpetrator) is shown in and in , stratified by gender where this data were available. A sub-set of 11 prevalence studies provided estimates for recent sexual violence victimization. These studies included 5427 participants, 310 (5.7%) of whom reported being a victim of recent sexual violence. The median prevalence of sexual victimization was 9.9% (IQR = 5.9–18.2%) in women and 3.1% in men (IQR = 2.5–6.7%). Pooled prevalence is shown in , but heterogeneity was high so this was unlikely to be a valid summary of individual study estimates. The pooled crude OR of sexual victimization was 3-fold higher in women compared with men (pooled crude OR = 3.4, CI = 2.5–4.6, p < .001; I2 = 0; n = 6 studies). Six studies reported odds for sexual victimization in people with vs without SMI (see ), with pooled crude ORs ranging from 5-fold to 17-fold higher odds (pooled OR = 5.8, CI = 2.8–12.1; I2 = 87%).
Prevalence of sexual domestic violence
Two studies reported on recent sexual victimization by partners or family members. In Sweden, Bengtsson-Tops and Ehliasson (Citation2012) estimated that 1–3% of male or female patients had been recently sexually assaulted by each of a partner, an ex-partner, or a family member—with 18% of all sexual assault victims being assaulted by an ex-partner. In Greece, Katsikidou et al. (Citation2013) estimated that 0.7% of male or female patients had been recently sexually assaulted by a family member (including partners), with 7% of all sexual assault victims being assaulted by a family member. Results were not reported disaggregated by gender.
Risk factors for violence (all perpetrators)
Eighteen studies reported associations between risk factors and recent violent victimization (by any perpetrator) (see ). Meta-analyses of crude odds ratios showed that victimization was strongly associated with homelessness (pooled OR = 2.6, CI = 2.1–3.2, I2 = 15%), substance misuse (pooled OR = 2.4, CI = 1.8–3.0, I2 = 63%) and violence perpetration (OR = 4.4, CI = 2.5–7.6, I2 = 84%). Victimization was moderately associated with illness severity (e.g. as measured by impaired function, young illness onset, and the number of admissions) and weakly associated with symptom cluster. Victimization was not associated with any demographic factors (gender, ethnicity, or age), diagnosis, or socio-economic status at the 5% significance level (see ).
Table 5. Meta-analyses of crude ORs for the association between risk factors and victimization.
Risk factors for domestic violence
Only one study reported risk factors for recent IPV (McPherson et al., Citation2007), and two studies reported risk factors for adulthood (but not recent) IPV (Chang et al., Citation2011; Morgan et al., Citation2010). McPherson et al. (Citation2007) reported correlates of past-year physical or sexual partner violence among 379 mothers with SMI who were followed up prospectively. Victimization was associated with younger age, but not with other socio-demographics (ethnicity, marital status, and education). Clinically it was associated with alcohol or drug misuse and some markers of illness severity (number of hospitalizations, number of symptoms), but not with illness duration or diagnosis. Chang et al. (Citation2011) reported correlates of adulthood (not recent) physical and sexual IPV among 428 male and female psychiatric patients. Physical IPV was commoner among women (OR = 4.7, CI = 2.7–8.2) and patients with a diagnosis of substance misuse or PTSD. Sexual IPV was commoner among women (OR = 12.4, CI = 4.9–31.1) and patients with a diagnosis of substance misuse or anxiety. Morgan et al. (Citation2010) reported correlates of adulthood (not recent) physical partner violence among 70 female psychiatric outpatients. They found that victimization was associated with having children, a history of overdose, and sexual abuse since the age of 16; but it was not associated with age, ethnicity, employment, or hospital admission history.
Discussion
Key findings
The review identified 30 studies on recent violence by any perpetrator against people with severe mental illness (SMI), with a total of 16 140 participants with SMI. However, only six studies reported on recent domestic violence and 11 on recent sexual violence. The median prevalence of recent physical violence by any perpetrator was 20.7% (IQR = 12.6–27.1%), with no difference in odds of victimization by gender (OR = 1.1, CI = 0.9–1.4, p = .31). The prevalence of past-year domestic violence ranged from 15–22% for violence against women, with very limited data on violence against men. The median prevalence of recent sexual violence was 9.9% (IQR = 5.9–18.1%) in women and 3.1% (IQR = 2.5–6.7%) in men; with 3-fold higher odds in women than in men (OR = 3.4, CI = 2.5–4.6, p < .001; I2 = 0). When comparing people with SMI vs those without SMI, the odds of physical, sexual, and domestic violence were elevated in all comparative studies, with a range of 2–22-fold higher odds (with most studies reporting elevated odds of 3–6-fold); with very limited evidence for relative odds of domestic violence. Overall victimization (i.e. regardless of perpetrator) was strongly associated with homelessness (pooled crude OR = 2.6, CI = 2.1–3.2; I2 = 15%), substance misuse (pooled crude OR = 2.4, CI = 1.8–3.0, I2 = 63%), and violence perpetration (pooled crude OR = 4.4, CI = 2.5–7.6; I2 = 84%). There was no association between victimization and demographic factors, socioeconomic status, or diagnosis. There was very limited evidence for risk factors specifically for domestic or sexual violence.
Findings in context of past evidence
This review provides an updated gender-specific synthesis on the prevalence and risk of victimization among people with SMI, and the first quantitative synthesis of risk factors for victimization in this population. The findings of previous related systematic reviews are summarized in Supplementary Table S1. Oram et al. (Citation2013) estimated that a third of women in contact with psychiatric inpatients or outpatients had a history of adulthood IPV. In this review, we found that around one in five women with SMI experienced recent DV—so the abuse for many patients was ongoing whilst under psychiatric care. Limited evidence suggested that family violence was as common as partner violence, but there was little evidence on its nature or impact. For sexual violence, Hughes et al. (Citation2012) previously estimated that ∼5% of people with any mental illness (including common mental disorder or SMI) experienced recent sexual violence, but did not report prevalence by gender. We estimated that around one in ten women (and 3% of men) with SMI experienced recent sexual violence.
In the general population men are at higher risk of physical violence and women are at much higher risk of sexual and domestic violence (Krug, Citation2002; World Health Organization, Citation2013). This review found that men and women with SMI had a similarly high prevalence of physical violence victimization—such that the protective effect of female gender in the general population was lost in the SMI population. Data on domestic violence against men were too limited to allow a gender comparison. For sexual violence, and like in the general population, women with SMI had a higher prevalence of sexual victimization than men with SMI. However, the protective effect of being male was less pronounced in the SMI population than in the general population—with some studies reporting a similar prevalence of sexual violence against men with SMI to that against women in the general population (Khalifeh, Moran, et al., Citation2015). Overall, people with SMI were at greater risk of both physical and sexual violence than the general population, with a narrowing of the gender gap found in the general population for both types of violence.
The pooled estimate of 5-fold relative odds for any physical violence in people with SMI compared to those without mental illness found in this review is in line with the 4-fold risk reported in the systematic review by Hughes et al. (Citation2012) (which mainly related to people with common mental disorders), and somewhat higher than the 3-fold risk of domestic violence in the review by Trevillion et al. (Citation2012). In all studies the elevated risk persisted after taking into account socio-demographic differences, so this effect is unlikely to be due to confounding.
This review provides the first quantitative synthesis of risk factors for victimization among people with SMI. Due to the lack of primary data, however, it was not possible to consider risk factors separately by gender or by type of violence, and the extent to which risk factors are relevant to violence experienced by both men and women and for domestic and sexual violence is unclear. The odds of any victimization were 4-fold higher among those with a history of violence perpetration, 3-fold higher among those with a history of substance misuse or homelessness, and 2-fold higher among those with greater illness severity. This reflects the findings by Maniglio (Citation2009), who identified the same key risk factors, but did not quantify their effects. The finding that violence perpetration and substance misuse are key risk factors for being a victim is not surprising. There are well-established links between victimization and perpetration in the general population and among people with SMI, although their relevance to women’s experiences of domestic and sexual violence are less well understood (Hiday, Swanson, Swartz, Borum, Wagner, Hiday, et al., Citation2001; Krug, Citation2002; Silver, Piquero, Jennings, Piquero, & Leiber, Citation2011). A recent systematic review on violence perpetration by people with psychosis found that being a victim of violence was associated with 6-fold higher odds of being a perpetrator (Witt et al., Citation2013). Several mechanisms have been suggested to explain this association, some of which apply to those without mental illness; for example, living in socially deprived neighbourhoods, where social and economic conditions foster violence norms (Sampson & Groves, Citation1989) or involvement in a violent sub-culture, especially one involving drug misuse (Goldstein, Citation1985; Krug, Citation2002; Sampson, Morenoff, & Gannon-Rowley, Citation2002). Other proposed mechanisms are specific to mental illness, for example acutely ill patients displaying disturbed or psychotic behaviour, which may evoke hostile reactions and attempts at social control from others, leading in turn to conflict and mutual violence (Silver, Citation2002). However, in this review there was greater support for risk factors shared with the general population than for illness-specific factors. In contrast to the strong associations found with substance misuse, homelessness and violence perpetration, diagnosis and positive symptoms were not associated with the risk of victimization.
Interestingly, key factors which are associated with victimization in the general population, such as gender, age, and social deprivation, were not associated with victimization in the SMI population. In the general population, young men are at highest risk of physical violence, in part due to lifestyle and socialization with delinquent peers (Krug, Citation2002). The risk decreases with age as men acquire employment and move to independent living with family responsibilities (Coid & Yang, Citation2010). Therefore, older age and employment are protective. It could be argued that the lack of meaningful social roles and social integration for the majority of people with SMI could leave them vulnerable to victimization, regardless of age or gender.
Only two of the included studies assessed childhood abuse, and both found an association with victimization risk. In the general population childhood abuse is associated with greater victimization risk in adulthood (Coid et al., Citation2001; Widom, Czaja, & Dutton, Citation2008). People with SMI have high rates of childhood abuse (Varese et al., Citation2012), and this may be an important risk factor in their vulnerability to violence as adults. There is a need for greater understanding of the mechanisms linking early abuse to later vulnerability; which are likely to include long-term effects of insecure attachment, poor self-esteem, and inter-personal difficulties in forming trusting relationships, setting boundaries, and managing conflict (Fonagy, Citation2003). These mechanisms are likely to be present in any victims of childhood abuse, but those who develop SMI have additional challenges in forming and maintaining supportive relationships, due to the direct and indirect effects of their illness (Thornicroft, Brohan, Rose, Sartorius, & Leese, Citation2009). This may compound the psychological and social effects of childhood abuse.
Whether the above findings are specifically applicable to DV is uncertain. DV advocates and mental health service users, however, have long been critical of ‘biomedical’ treatment models that emphasize diagnosis and individualize what is a social problem (Humphreys & Thiara, Citation2003; Trevillion et al., Citation2014). Echoing this, the review findings suggest that treatment approaches that focus only on psychiatric symptoms are likely to be insufficient in reducing risk of violent victimization. We found that there was very limited evidence on risk factors specifically for domestic or sexual violence against people with SMI. In the general population, factors associated with domestic or sexual victimization include younger age, witnessing DV as a child, substance misuse, poverty, and childhood sexual abuse (Krug, Citation2002). These factors are more prevalent among people with SMI and may in part account for the excess risk. The evidence reviewed here suggests that illness severity and substance misuse are important correlates; these factors could both precede and follow victimization. A more recent study found a strong association between childhood abuse and adulthood domestic and sexual violence among both men and women with SMI—with emotional childhood abuse having particularly strong associations with adulthood victimization (Anderson, Howard, Dean, Moran, & Khalifeh, Citation2016). However, aetiological factors also occur at the level of the relationship (e.g. having a partner who misuses substances or who was a victim of childhood abuse), community (e.g. high population density, unemployment, and social isolation), and society or culture (e.g. gender and social inequalities, and health, economic, and social policies) (Krug, Citation2002; Oram, Khalifeh, & Howard, Citation2016) There was a lack of evidence on risk factors operating at these levels, but they are likely to be key in this population.
The findings highlight the importance of improving mental health service responses to domestic, sexual, and other forms of violence victimization. Mental health professionals are accustomed to assessing what risk their patients pose to others, but are less practiced in asking about patients experiences of violence; it is estimated that only 10–30% of cases of domestic violence are identified and that sexual violence is similarly under-detected (Chapman & Monk, Citation2015; Howard et al., Citation2010; Oram et al., Citation2016) Several countries now require that mental health professionals routinely enquire about violence victimization (Agar & Read, Citation2002; Department of Health, Citation2010; Eilenberg, Fullilove, Goldman, & Mellman, Citation1996). In order to do so safely, mental health professionals should be trained in identifying and responding to violence victimization, including awareness of the increased risk of being a victim of violence compared to the general population and of the gender differences in the types of violence experienced. Clear referral pathways to specialist support and advice for people who have experienced violence should be implemented. However, efforts to improve the identification and response to violent victimization among mental health service users, including the refinement of risk assessments and implementation of prevention strategies, would benefit from research to elucidate whether and how risk factors differ for men and women and for different forms of abuse.
Strengths and limitations
Strengths of this review include a gender-specific focus (lacking in previous reviews), new quantitative synthesis of evidence on risk factors and rigorous evaluation of study quality, and potential sources of heterogeneity. Due to time and resource limitations, the literature search was conducted for studies published over a limited time period, with identification of earlier studies relying on published systematic reviews. Therefore, it is possible that some earlier studies may have been missed. This is likely to be mitigated by screening of reference lists from more recent studies. Authors and experts were not contacted. The review only included studies published in English, so may have missed some relevant studies published in other languages. The study settings, populations, and methods were highly varied. In this review SMI was defined as having either a psychotic illness or being under the care of psychiatric services. This was in part a pragmatic choice, based on the populations included in the relevant published studies. The definition is potentially problematic, as those under the care of secondary services might well include patients with a range of non-psychotic disorders, but there is no widely agreed definition of SMI, with inconsistency in whether SMI is restricted to certain diagnoses or is defined by illness severity, functional impairment, and the need for secondary care (Charlwood, Mason, Goldacre, Cleary, & Wilkinson, Citation1999). The pooled prevalence estimates had high levels of statistical heterogeneity, where the findings from individual studies were more different from each other than would be expected by chance. Therefore, the pooled prevalence estimates may not be a valid summary of individual study findings, and the individual study estimates need to be inspected. Although a broad range of potential sources of heterogeneity were explored (related to study setting, design, methods, and quality), none explained the heterogeneity in violence prevalence estimates. This might be either because the true prevalence varies across settings and populations, or because there were multiple differences in design, methods, and quality across studies that could not be adequately accounted for in the heterogeneity analyses. The risk factor meta-analyses had little or moderate heterogeneity, so these meta-analyses have greater validity.
The quality of many included studies was limited by non-random recruitment, low response rates, and brief, poorly validated violence measures. Many had a primary focus other than victimization, with victimization included in a battery of measures on quality-of-life, or investigated as a risk factor for violence perpetration. None of the studies reported correlates of sexual violence only; but rather reported risk factors for either physical violence only, or physical and sexual violence combined. Therefore, it was not possible to compare risk factors for physical and sexual violence. Future research should acknowledge domestic, sexual, and other forms of violence as public mental health problems and seek to understand risk pathways for different types of violence at the individual, inter-personal, community, and societal levels, within a lifespan or developmental framework. Given the high burden and excess risk of victimization among people with SMI, future research should evaluate complex interventions for improving detection of and response to victimization experiences within mental health services.
Conclusion
The review synthesized evidence from 30 studies and found that around a fifth of people with severe mental illness had experienced recent violence, regardless of their age, gender, socio-economic position, or diagnosis. More limited evidence suggested that 15–20% of women with SMI experienced recent domestic violence (with a similar burden of partner and family violence) and one in 10 experienced recent sexual violence. Men and women with SMI were at higher risk of physical and sexual violence than the general population, with a narrowing of the gender gap. Many of the risk factors for victimization among people with SMI were shared with the general population rather than being illness-specific, and included violence perpetration, substance misuse, and homelessness. There was a lack of evidence on risk factors specifically for domestic and sexual violence, and on the extent of domestic and sexual violence against men with SMI. Future studies should address these evidence gaps, in order to guide clinical practice and policy on gender-sensitive violence prevention measures in this group.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Abramsky, T., Watts, C., Garcia Moreno, C., Devries, K., Kiss, L., Ellsberg, M., …. Heise, L. (2011). What factors are associated with recent intimate partner violence? findings from the WHO multi-country study on women's health and domestic violence. BMC Public Health, 11, 109. doi: 10.1186/1471-2458-11-109.
- Agar, K., & Read, J. (2002). What happens when people disclose sexual or physical abuse to staff at a community mental health centre? International Journal of Mental Health Nursing, 11, 70–79. doi: 10.1046/j.1440-0979.2002.00230.x.
- Anderson, F., Howard, L., Dean, K., Moran, P., & Khalifeh, H. (2016). Childhood maltreatment and adulthood domestic and sexual violence victimisation among people with severe mental illness. Social Psychiatry and Psychiatric Epidemiology, 51, 961–970. doi: 10.1007/s00127-016-1244-1.
- Bengtsson-Tops, A., & Ehliasson, K. (2012). Victimization in individuals suffering from psychosis: A Swedish cross-sectional study. Journal of Psychiatric and Mental Health Nursing, 19, 23–30. doi: 10.1111/j.1365-2850.2011.01749.x.
- Bengtsson-Tops, A., Markstrom, U., & Lewin, B. (2005). The prevalence of abuse in Swedish female psychiatric users, the perpetrators and places where abuse occurred. Nordic Journal of Psychiatry, 59, 504–510. doi: 10.1080/08039480500360732.
- Brekke, J.S., Prindle, C., Bae, S.W., & Long, J.D. (2001). Risks for individuals with schizophrenia who are living in the community. Psychiatric Services, 52, 1358–1366. doi: 10.1176/appi.ps.52.10.1358.
- Chang, J.C., Cluss, P.A., Burke, J.G., Hawker, L., Dado, D., Goldstrohm, S., …. Scholle, S.H. (2011). Partner violence screening in mental health. General Hospital Psychiatry, 33, 58–65. doi: 10.1016/j.genhosppsych.2010.11.009.
- Chapman, A., & Monk, C. (2015). Domestic violence awareness. American Journal of Psychiatry, 172, 944–945. doi: 10.1176/appi.ajp.2015.15070853.
- Chapple, B., Chant, D., Nolan, P., Cardy, S., Whiteford, H., & McGrath, J. (2004). Correlates of victimisation amongst people with psychosis. Social Psychiatry and Psychiatric Epidemiology, 39, 836–840. doi: 10.1007/s00127-004-0819-4.
- Charlwood, P., Mason, A., Goldacre, M., Cleary, R., & Wilkinson, E. (1999). Health outcome indicators: Severe mental illness. Report of a working group to the department of health. Oxford: National Centre for Health Outcomes Development.
- Clopper, C., & Pearson, S. (1934). The use of confidence or fiducial limits illustrated in the case of the Binomial. Biometrika, 26, 404–413. doi: 10.1093/biomet/26.4.404.
- Coid, J., Petruckevitch, A., Feder, G., Chung, W.S., Richardson, J., & Moorey, S. (2001). Relation between childhood sexual and physical abuse and risk of revictimisation in women: A cross-sectional survey. The Lancet, 358, 450–454. doi: http://dx.doi.org/10.1016/S0140-6736(01)05622-7.
- Coid, J., & Yang, M. (2010). Violence and delayed social independence among young adult British men. Social Psychiatry and Psychiatric Epidemiology, 45, 301–308. doi: 10.1007/s00127-009-0077-6.
- Crisanti, A.S., Frueh, B.C., Crisanti, A.S., & Frueh, B.C. (2014). Risk of trauma exposure among persons with mental illness in jails and prisons: What do we really know? Current Opinion in Psychiatry, 24, 431–435. doi: 10.1097/YCO.0b013e328349bbb8.
- Dean, K., Moran, P., Fahy, T., Tyrer, P., Leese, M., Creed, F., …. Walsh, E. (2007). Predictors of violent victimization amongst those with psychosis. Acta Psychiatrica Scandinavica, 116, 345–353. doi: 10.1111/j.1600-0447.2007.01078.x.
- Deeks, J.J., Higgins, J.P., & Altman, D.G. (2011). Analysing data and undertaking meta-analyses. In J. Higgins & S. Green (Eds.), Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration.
- Department of Health. (2010). Responding to violence against women and children – the role of the NHS. London: HMSO.
- DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7, 177–188. doi: 10.1016/0197-2456(86)90046-2.
- Devries, K.M., Mak, J.Y., Bacchus, L.J., Child, J.C., Falder, G., Petzold, M., …. Watts, C.H. (2013). Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. Plos Medicine, 10, 11. doi: 10.1371/journal.pmed.1001439.
- Eilenberg, J., Fullilove, M.T., Goldman, R.G., & Mellman, L. (1996). Quality and use of trauma histories obtained from psychiatric outpatients through mandated inquiry. Psychiatric Services, 47, 165–169. doi: 10.1176/ps.47.2.165.
- Ellsberg, M., Jansen, H.A.F.M., Heise, L., Watts, C.H., & Garcia-Moreno, C. (2008). Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: An observational study. The Lancet, 371, 1165–1172. doi: 10.1016/S0140-6736(08)60522-X.
- Fitzgerald, P.B., de Castella, A.R., Filia, K.M., Filia, S.L., Benitez, J., & Kulkarni, J. (2005). Victimization of patients with schizophrenia and related disorders. Australian and New Zealand Journal of Psychiatry, 39, 169–174. doi: 10.1111/j.1440-1614.2005.01539.x.
- Fonagy, P. (2003). Towards a developmental understanding of violence. The British Journal of Psychiatry, 183, 190–192. doi: 10.1192/02-514.
- Fortugno, F., Katsakou, C., Bremner, S., Kiejna, A., Kjellin, L., Nawka, P., …. Priebe, S. (2013). Symptoms associated with victimization in patients with schizophrenia and related disorders. PLoS One [Electronic Resource], 8, e58142. doi: 10.1371/journal.pone.0058142.
- Goldstein, P.J. (1985). The drugs/violence nexus: A tripartite conceptual framework. Journal of Durg Issues, 15, 493–506. doi: 10.1177/002204268501500406.
- Goodman, L.A., Salyers, M.P., Mueser, K.T., Rosenberg, S.D., Swartz, M., Essock, S.M. … Site Health and Risk Study Research. (2001). Recent victimization in women and men with severe mental illness: Prevalence and correlates. Journal of Traumatic Stress, 14, 615–632. doi: 10.1023/a:1013026318450.
- Hahn, L., Rigby, A., & Galletly, C. (2014). Determinants of high rates of smoking among people with psychosis living in a socially disadvantaged region in South Australia. Australian and New Zealand Journal of Psychiatry, 48, 70–79. doi: 10.1177/0004867413491158.
- Havassy, B.E., & Mericle, A.A. (2013). Recent violence among persons entering short-term residential mental health and substance abuse treatment. Journal of Dual Diagnosis, 9, 222–227. doi: 10.1080/15504263.2013.804773.
- Hiday, V.A., Swanson, J.W., Swartz, M.S., Borum, R., Wagner, H.R., Hiday, V.A., …. Wagner, H.R. (2001). Victimization: A link between mental illness and violence? [Erratum appears in Int J Law Psychiatry.2002 Sep-Oct;25(5):533-6.]. International Journal of Law & Psychiatry, 24, 559–572. doi: 10.1016/S0160-2527(01)00091-7.
- Hiday, V.A., Swartz, M.S., Swanson, J.W., Borum, R., & Wagner, H.R. (1999). Criminal victimization of persons with severe mental illness. Psychiatric Services, 50, 62–68. doi: 10.1176/ps.50.1.62.
- Higgins, J.P., & Green, S. (2011). Cochrane handbook for systematic reviews of interventions. London: The Cochrane Collaboration.
- Hodgins, S., Alderton, J., Cree, A., Aboud, A., & Mak, T. (2007). Aggressive behaviour, victimisation and crime among severely mentally ill patients requiring hospitalisation. British Journal of Psychiatry, 191, 343–350. doi: 10.1192/bjp.bp.106.029587.
- Honkonen, T., Henriksson, M., Koivisto, A.M., Stengard, E., & Salokangas, R.K.R. (2004). Violent victimization in schizophrenia. Social Psychiatry and Psychiatric Epidemiology, 39, 606–612. doi: 10.1007/s00127-004-0805-x.
- Howard, L., Trevillion, K., Khalifeh, H., Woodall, A., Agnew-Davies, R., & Feder, G. (2010). Domestic violence and severe psychiatric disorders: prevalence and interventions. Psychological Medicine, 40, 881–893. doi: 10.1017/S0033291709991589.
- Hsu, C.C., Sheu, C.J., Liu, S.I., Sun, Y.W., Wu, S.I., & Lin, Y. (2009). Crime victimization of persons with severe mental illness in Taiwan. Australian and New Zealand Journal of Psychiatry, 43, 460–466. doi: 10.1080/00048670902817737.
- Hughes, K., Bellis, M.A., Jones, L., Wood, S., Bates, G., Eckley, L., …. Officer, A. (2012). Prevalence and risk of violence against adults with disabilities: A systematic review and meta-analysis of observational studies. The Lancet, 379, 1621–1629. doi: http://dx.doi.org/10.1016/S0140-6736(11)61851-5.
- Humphreys, C., & Thiara, R. (2003). Mental health and domestic violence: ‘I call it symptoms of abuse’. British Journal of Social Work, 33, 209–226. doi: 10.1093/bjsw/33.2.209.
- Kamperman, A.M., Henrichs, J., Bogaerts, S., Lesaffre, E.M., Wierdsma, A.I., Ghauharali, R.R., …. Mulder, C.L. (2014). Criminal victimisation in people with severe mental illness: A multi-site prevalence and incidence survey in the Netherlands. PLoS One, 9, e91029. doi: 10.1371/journal.pone.0091029.
- Katsikidou, M., Samakouri, M., Fotiadou, M., Arvaniti, A., Vorvolakos, T., Xenitidis, K., & Livaditis, M. (2013). Victimization of the severely mentally ill in Greece: The extent of the problem. International Journal of Social Psychiatry, 59, 706–715. doi: 10.1177/0020764012448782.
- Khalifeh, H., Johnson, S., Howard, L.M., Borschmann, R., Osborn, D., Dean, K., … Moran, P. (2015). Violent and non-violent crime against adults with severe mental illness. Br J Psychiatry, 206, 275–282. doi: 10.1192/bjp.bp.114.147843.
- Khalifeh, H., Moran, P., Borschmann, R., Dean, K., Hart, C., Hogg, J., …. Howard, L. (2015). Domestic and sexual violence against patients with severe mental illness. Psychological Medicine, 45, 875–886. doi: http://dx.doi.org/10.1017/S0033291714001962.
- Kirkwood, B.R., & Sterne, J.A.C. (2003a). Medical statistics. Oxford: Blackwell Publishing.
- Kirkwood, B.R., & Sterne, J.S. (2003b). Comparing two proportions. In B. R. Kirkwood & J. S. Sterne (Eds.), Medical Statistics (pp. 148–164). Oxford: Blackwell Science Ltd.
- Krug, E.G. (2002). World report on violence and health. Geneva: World Health Organization.
- Latalova, K., Kamaradova, D., & Prasko, J. (2014). Violent victimization of adult patients with severe mental illness: A systematic review. Neuropsychiatric Disease and Treatment, 10, 1925–1939. doi: 10.2147/ndt.s68321.
- Liberati, A., Altman, D.G., Tetzlaff, J., Mulrow, C., Gotzsche, P.C., Tzsche, P., …. Moher, D., (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Plos Medicine, 6, e1000100. doi: 10.1371/journal.pmed.1000100.
- Maniglio, R. (2009). Severe mental illness and criminal victimization: A systematic review. Acta Psychiatrica Scandinavica, 119, 180–191. doi: 10.1111/j.1600-0447.2008.01300.x.
- McPherson, M.D., Delva, J., & Cranford, J.A. (2007). A longitudinal investigation of intimate partner violence among mothers with mental illness. 58, 675–680. doi: 10.1176/appi.ps.58.5.675.
- Morgan, J.F., Zolese, G., McNulty, J., & Gebhardt, S. (2010). Domestic violence among female psychiatric patients: Corss-sectional survey. The Psychiatrist, 34, 461–464. doi: 10.1001/archpsyc.62.8.911.
- Mueser, K.T., Rosenberg, S.D., Goodman, L.A., & Trumbetta, S.L. (2002). Trauma, PTSD, and the course of severe mental illness: An interactive model. Schizophrenia Research, 53, 123–143. doi: http://dx.doi.org/10.1016/S0920-9964(01)00173-6.
- Neria, Y., Bromet, E.J., Carlson, G.A., & Naz, B. (2005). Assaultive trauma and illness course in psychotic bipolar disorder: Findings from the suffolk county mental health project. Acta Psychiatrica Scandinavica, 111, 380–383. doi: 10.1111/j.1600-0447.2005.0530.x.
- NICE. (2014). Domestic violence and abuse: How health services, social care and the organisations they work with can respond effectively. London: National Institute for health and Care Excellence.
- Oram, S., Khalifeh, H., & Howard, L.M. (2016). Violence against women and mental health. The Lancet Psychiatry. (In press).
- Oram, S., Trevillion, K., Feder, G., & Howard, L.M. (2013). Prevalence of experiences of domestic violence among psychiatric patients: Systematic review. The British Journal of Psychiatry, 202, 94–99. doi: 10.1192/bjp.bp.112.109934.
- Peters, J.L., Sutton, A.J., Jones, D.R., Abrams, K.R., & Rushton, L. (2006). Comparison of two methods to detect publication bias in meta-analysis. JAMA, 295, 676–680. doi: 10.1001/jama.295.6.676.
- Sampson, R.J., & Groves, W.B. (1989). Community structure and crime – testing social-disorganization theory. American Journal of Sociology, 94, 774–802. doi: http://dx.doi.org/10.1086/229068.
- Sampson, R.J., Morenoff, J.D., & Gannon-Rowley, T. (2002). Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology, 28, 443–478. doi: 10.1146/annurev.soc.28.110601.141114.
- Schomerus, G., Heider, D., Angermeyer, M.C., Bebbington, P.E., Azorin, J.M., Brugha, T., & Toumi, M. (2008). Urban residence, victimhood and the appraisal of personal safety in people with schizophrenia: Results from the European schizophrenia cohort (EuroSC). Psychological Medicine, 38, 591–597. doi: 10.1017/s0033291707001778.
- Silver, E. (2002). Mental disorder and violent victimization: The mediating role of involvement in conflicted social relationships. Criminology, 40, 191–212. doi: 10.1111/j.1745-9125.2002.tb00954.x.
- Silver, E., Arseneault, L., Langley, J., Caspi, A., & Moffitt, T.E. (2005). Mental disorder and violent victimization in a total birth cohort. American Journal of Public Health, 95, 2015–2021. doi: 10.2105/ajph.2003.021436.
- Silver, E., Piquero, A.R., Jennings, W.G., Piquero, N.L., & Leiber, M. (2011). Assessing the violent offending and violent victimization overlap among discharged psychiatric patients. Law and Human Behavior, 35, 49–59. doi: 10.1007/s10979-009-9206-8.
- Sturup, J., Sorman, K., Lindqvist, P., & Kristiansson, M. (2011). Violent victimization of psychiatric patients: A Swedish case-control study. Social Psychiatry and Psychiatric Epidemiology, 46, 29–34. doi: 10.1007/s00127-009-0167-5.
- Teplin, L.A., McClelland, G.M., Abram, K.M., & Weiner, D.A. (2005). Crime victimization in adults with severe mental illness – Comparison with the national crime victimization survey. Archives of General Psychiatry, 62, 911–921. doi: 10.1001/archpsyc.62.8.911.
- Thornicroft, G., Brohan, E., Rose, D., Sartorius, N., & Leese, M. (2009). Global pattern of experienced and anticipated discrimination against people with schizophrenia: A cross-sectional survey. The Lancet, 373, 408–415. doi: 10.1016/S0140-6736(08)61817-6.
- Trevillion, K., Hughes, B., Feder, G., Borschmann, R., Oram, S., & Howard, L.M. (2014). Disclosure of domestic violence in mental health settings: a qualitative meta-synthesis. International Review of Psychiatry, 26, 430–444. doi: 10.3109/09540261.2014.924095.
- Trevillion, K., Oram, S., Feder, G., & Howard, L.M. (2012). Experiences of domestic violence and mental disorders: A systematic review and meta-analysis. PLoS One, 7, e51740. doi: 10.1371/journal.pone.0051740.
- Tsigebrhan, R., Shibre, T., Medhin, G., Fekadu, A., & Hanlon, C. (2014). Violence and violent victimization in people with severe mental illness in a rural low-income country setting: A comparative cross-sectional community study. Schizophrenia Research, 152, 275–282. doi: 10.1016/j.schres.2013.10.032.
- Vandenbroucke, J., von Elm, E., Altman, D., Gotzsche, P., Mulrow, C., G.¸Tzsche, P., …. Egger, M. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. PLos Medicine, 4, e297–e1654. doi: http://dx.doi.org/10.1371/journal.pmed.0040297.
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., … Bentall, R.P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin, 38, 661–671. doi: 10.1093/schbul/sbs050.
- White, M.C., Chafetz, L., Collins-Bride, G., & Nickens, J. (2006). History of arrest, incarceration and victimization in community-based severely mentally ill. Journal of Community Health, 31, 123–135. doi: 10.1007/s10900-005-9005-1.
- Widom, C.S., Czaja, S.J., & Dutton, M.A. (2008). Childhood victimization and lifetime revictimization. Child Abuse and Neglect, 32, 785–796. doi: http://dx.doi.org/10.1016/j.chiabu.2007.12.006
- Witt, K., van Dorn, R., & Fazel, S. (2013). Risk factors for violence in psychosis: Systematic review and meta-regression analysis of 110 studies. PLoS One, 8, e55942. doi: 10.1371/journal.pone.0055942.
- World Health Organization. (2013). Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO.