Abstract
Depression has a large burden, but the development of new drugs for its treatment has proved difficult. Progresses in neuroscience have highlighted several physiopathological pathways, notably inflammatory and metabolic ones, likely involved in the genesis of depressive symptoms. A novel strategy proposes to repurpose established medical treatments of known safety and to investigate their potential antidepressant activity. Among numerous candidates, growing evidence suggests that statins may have a positive role in the treatment of depressive disorders, although some have raised concerns about possible depressogenic effects of these widely prescribed medications. This narrative review summarises relevant findings from translational studies implicating many interconnected neurobiological and neuropsychological, cardiovascular, endocrine-metabolic, and immunological mechanisms by which statins could influence mood. Also, the most recent clinical investigations on the effects of statins in depression are presented. Overall, the use of statins for the treatment of depressive symptoms cannot be recommended based on the available literature, though this might change as several larger, methodologically robust studies are being conducted. Nevertheless, statins can already be acknowledged as a driver of innovation in mental health, as they provide a novel perspective to the physical health of people with depression and for the development of more precise antidepressant treatments.
Introduction
Depression is a common disabling disorder (Demyttenaere & Van Duppen, Citation2019; James et al., Citation2018) for which current management strategies, including psychotherapy and pharmacotherapy (Cuijpers et al., Citation2020; Furukawa et al., Citation2021), are not satisfactory (Malhi et al., Citation2020). While about half of patients with depressive illness respond to first-line antidepressant medication, one-third still suffer from impairing symptoms after four treatment steps over one year (Rush et al., Citation2006). Concordance with treatment is a further significant issue (Solmi et al., Citation2021), with more than one-quarter discontinuing antidepressants due to any cause or because of intolerable side-effects (Cipriani et al., Citation2018).
Most licenced antidepressants, which work in the main by modulating monoaminergic neurotransmission, are characterised by a delayed therapeutic onset (Harmer et al., Citation2017), further complicating the effective management of this condition (Malhi et al., Citation2020). Overall, there is a compelling need to identify novel molecular targets in depression and thus new antidepressants that can act on them (Jarończyk & Walory, Citation2022), particularly with a view to tailoring treatment to the individual patient (Maj et al., Citation2020). Regrettably, clinical research and drug development in this area is challenging (Rush et al., Citation2022), and indeed several pharmaceutical companies have disinvested from it (Ciccocioppo, Citation2017). An innovative and promising approach proposes instead to repurpose existing medications with a well-defined safety profile and capable of targeting emerging physiopathological pathways implicated in depression (Berk & Nierenberg, Citation2015; Ebada, Citation2017; Mohammad Sadeghi et al., Citation2021), similarly to what has been recently advocated for bipolar illness (Bartoli et al., Citation2021).
Currently, the conceptual neurobiological framework surrounding depressive disorders encompasses a variety of mechanisms including deeply interconnected neurobiological and neuropsychological, endocrine-metabolic, cardiovascular, and immunological systems (Bot et al., Citation2020; Caspani et al., Citation2021; Chavez-Castillo et al., Citation2020; Guerreiro Costa et al., Citation2022; Jones et al., Citation2021; Kokkeler et al., Citation2022). In this context, pre-clinical and clinical studies consistently show that the 3-hydroxy-3-methylglutaryl-Coenzyme A (HMG-CoA) reductase inhibitors, or statins, are intriguing candidates for repurposing in neuropsychiatric disorders (Avan et al., Citation2021; Fernandes et al., Citation2021; Fracassi et al., Citation2019; Rahola, Citation2012; Tao et al., Citation2021), and especially in depression (Covington et al., Citation2010; Fabbri et al., Citation2021; Le-Niculescu et al., Citation2021; Maes et al., Citation2012; Mohammad Sadeghi et al., Citation2021; So et al., Citation2019).
Statins are a class of lipid-lowering drugs, among the most widely prescribed worldwide (Simons, Citation2003), which have been used for several decades to treat and prevent cardiovascular, cerebrovascular, and metabolic disorders (Sizar et al., Citation2022). Their primary mechanism of action involves the competitive, reversible antagonism of liver HMG-CoA reductase, the rate-limiting enzyme in cholesterol biosynthesis (Endo et al., Citation1976). However, statins are described as possessing “pleiotropic effects” (Yu & Liao, Citation2022), of which the anti-inflammatory actions are best characterised today (Zeiser, Citation2018).
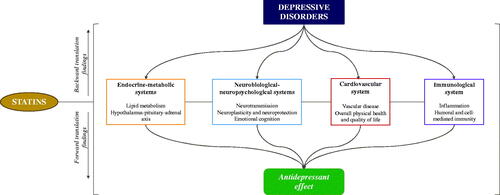
Statins express their pleiotropic activities differentially, based on both their potency and lipophilicity/hydrophilicity (Irwin et al., Citation2020): their variable strength and neural entry/efflux emphasise the need for these molecules to be considered individually with respect to their pharmacological activity in the central nervous system (CNS) (McFarland et al., Citation2014). Statins can affect brain function both directly, via local neurobiological and neuropsychological effects, and indirectly, by influencing deeply interconnected systems (i.e. endocrine-metabolic, cardiovascular, immunological) that ultimately have an impact on mental processes (Farooqui et al., Citation2007; Fracassi et al., Citation2019). The most recent evidence from basic science (Walker et al., Citation2021) and clinical research (Hayes et al., Citation2019; Kim et al., Citation2019) indicates that statins may play a role in the treatment of neuropsychiatric syndromes, particularly in the context of affective disorders such as depression (Bortolato et al., Citation2016; De Giorgi et al., Citation2021).
Translational evidence for statins in depression
It has been shown that statin administration can improve depressive-like behaviour in animals (Kilic et al., Citation2010). More intriguingly, several lines of evidence from translational investigations in vitro, animal, and human models have provided valuable information not only about the putative antidepressant effect of statins (i.e. forward findings), but also on some of those neurobiological and neuropsychological, cardiovascular, endocrine-metabolic, and immunological processes underpinning the physiopathology of depressive disorders (i.e. backward findings) ().
Statins can affect brain biology through their activity on neurotransmission and neurogenesis/neuroprotective processes. Though several neurotransmitters have been involved (Kosowski et al., Citation2021), most of the evidence concerns serotonin (5-HT) transmission, suggesting that antidepressant effect of statins may be due to their capacity to increase availability of the serotonin precursor, tryptophan (Kilic et al., Citation2012) and overall hippocampal serotonin levels (ElBatsh, Citation2015), while also showing 5-hydroxytryptamine receptor (5HT1A, 5HT2A/C, and 5HT3) antagonism (Ludka et al., Citation2014; Nothdurfter et al., Citation2010; Shrivastava et al., Citation2010). Further, selective serotonin reuptake inhibitors (SSRIs) pharmacodynamics (Kilic et al., Citation2012; Ludka et al., Citation2014; Renshaw et al., Citation2009; Santos et al., Citation2012) and pharmacokinetics (Al-Asmari et al., Citation2017; Bhattarai et al., Citation2017; Li et al., Citation2017) appear modulated by statin administration.
Statins also affect non-monoaminergic pathways, including N-methyl-D-aspartate (NMDA) receptor antagonism (da Cruz et al., Citation2017; Kilic et al., Citation2012; Ludka et al., Citation2013; Wang et al., Citation2009; Yan et al., Citation2011), which is implicated in the effects of ketamine on mood (Zanos & Gould, Citation2018). The antidepressant effects of statins have also been associated with induction of neuroprotective pathways (Eisel et al., Citation2010; Ludka et al., Citation2016) and decreased neuronal damage due to glutamate excitotoxicity, inflammation, and oxidative stress (Ludka et al., Citation2013, Citation2017b), as well as increased neurogenesis through brain-derived neurotrophic factor (BDNF) (Binder et al., Citation2015; Ludka et al., Citation2013, Citation2017a; Tang et al., Citation2020; Tsai, Citation2007). Besides these diverse neurobiological actions, recent human studies have shown that statins can influence neuropsychological functions such as emotional processing (De Giorgi et al., Citation2021, Citation2022; Gillespie et al., Citation2022), which have been robustly linked to depression and its treatment (Godlewska & Harmer, Citation2021).
As mentioned, statins are primarily used in the context of cardiovascular disorders: it has been proposed that their ability to reduce thrombogenesis and improve cerebral blood flow in animals (Sheets et al., Citation2016) and humans (Massardo et al., Citation2020; Citation2022; van Agtmaal et al., Citation2017) might lead to an improvement in cognitive and emotional functioning, as well as in patients’ overall physical health and quality of life (Downs et al., Citation1993; Yang et al., Citation2003) – all elements associated with fewer depressive onsets, especially in the elderly (Taylor et al., Citation2013).
The metabolic effect of statins on systemic lipids are well established, but their consequences on mood regulation less so. Some studies have found that cholesterol and related metabolites can modulate statins’ reduction of depressive- and anxiety-like behaviour in rats (Can et al., Citation2012; Segatto et al., Citation2014), while others have failed to identify such association (Citraro et al., Citation2014). In humans, excessively low concentrations of blood cholesterol correlate with the onset of depressive episodes, but when cholesterol-lowering is achieved via statins, such association does not persist (Persons et al., Citation2016). On the other hand, certain antidepressants and antipsychotics with antidepressant activity have been associated with higher lipid levels (Vancampfort et al., Citation2014). Statins are also capable of expressing an endocrine effect on the hypothalamic-pituitary-adrenal (HPA) axis and cortisol, thus controlling stress (Kumar et al., Citation2012; Lin et al., Citation2014) and immune responses (ElBatsh, Citation2015; Sheets et al., Citation2016) that seem to play a significant role in depression (Pellosmaa et al., Citation2015; Pellosmaa & Dougall, Citation2016).
Indeed, the immunological effects of statins in depression, especially via anti-inflammatory mechanisms, are the most investigated, since exaggerated or overactive inflammation appears crucial in at least certain subtypes of depressive disorders (Miller et al., Citation2017). Numerous studies have shown that statins can reduce circulating pro-inflammatory cytokines, such as interleukins (IL), tumour necrosis factor (TNF)-α, and C-reactive protein (CRP) in both animals (Hai-Na et al., Citation2020; Lim et al., Citation2017; Menze et al., Citation2021; Sheets et al., Citation2016; Wu et al., Citation2019; Yu et al., Citation2019; Zhang et al., Citation2017) and humans (Kang et al., Citation2016; Kim et al., Citation2018; Lesperance et al., Citation2004; Ma et al., Citation2016), and this anti-inflammatory effect also correlates with their antidepressant activity. Non-inflammatory mechanisms, pertaining to humoral and cellular immunity, preliminarily indicate that statins might affect tryptophan metabolism through these less studied processes (Neurauter et al., Citation2003; Wirleitner et al., Citation2003, Citation2004).
Overall, translational evidence that uses statins as a probe for depression and its treatment highlights intriguing avenues for further research on largely interconnected neurobiological and neuropsychological, cardiovascular, endocrine-metabolic, and immunological systems. However, translation of findings from in vitro, animal, and indeed human studies to medical practice remains particularly challenging in psychiatry (Nestler & Hyman, Citation2010); therefore we now provide an overview of the latest studies exploring the clinical effects of statins in depression.
Clinical evidence for statins in depression
Early evidence had raised concerns about potential connections between statin use, low cholesterol, increased mortality due to suicide, and depressive symptoms (Muldoon et al., Citation1990; Shin et al., Citation2008). Consistently, meta-analytic data suggested a possible relationship between lower lipid levels and suicidality in depression (Wu et al., Citation2016), though not in bipolar depression (Bartoli et al., Citation2017), perhaps suggesting a possible role of clinical and biochemical confounding factors underlying such associations (Bartoli et al., Citation2017).
More recently, many clinical studies have directly investigated the potential effect of statins on depressive symptoms. Previous work from our group had summarised the existing evidence for this topic (De Giorgi et al., Citation2021); an updated search on the 8th of April 2022 (i.e. one year later) has retrieved further 16 records, for a current total of 88 studies. A graphic display of the beneficial, null, or harmful outcomes on depression observed for statin use, according to study design, is in . The most recent, largest studies are described below.
Table 1. Clinical studies investigating the effect of statins in depression.
Clinical trials and their meta-analyses
The majority of the twenty-two clinical trials have been variably included in the eight available meta-analyses. Two pair-wise meta-analyses published in the same year (Köhler-Forsberg et al., Citation2019; Yatham et al., Citation2019) comprised distinct subsets of randomised controlled trials (RCTs), despite similar inclusion criteria, yet reached the same conclusion: statins appeared to have a small to moderate positive effect on depressive symptoms [Nrange = 1,576–2,517; standardised mean difference (SMD)range = −0.31 to −0.26; 95% confidence interval (CI)range = −0.52 to −0.09].
Two network meta-analyses, also containing a pair-wise component, respectively compared statins against each other (Lee et al., Citation2021a) and against other drugs with anti-inflammatory properties (Hang et al., Citation2021). The former involved thirteen RCTs (N = 2,479) and showed that statins were on the whole better than placebo in reducing depressive symptoms [mean difference (MD) = −0.35; 95%CI = −0.59 to −0.11], with atorvastatin seemingly the most efficacious (MDvs placebo = −3.46; 95%CI −5.26 to −1.67) (Lee et al., Citation2021a). The second only included three RCTs (N = not reported) and did not identify any effect on depression [relative risk (RR) = 0.68; 95%CI = 0.38–1.18] (Hang et al., Citation2021).
Two more recent pair-wise meta-analyses, which expand on a subgroup analysis of the earlier work by Yatham et al. (Citation2019), may explain the reason behind these discrepancies: pooled results from trials that had administered statins in add-on to antidepressants in patients diagnosed with a depressive disorder showed a moderate beneficial effect (four RCTs; N = 238; SMD = −0.48; 95%CI = −0.74 to −0.22) of this intervention compared to antidepressants alone (De Giorgi et al., Citation2021), whereas statins used in monotherapy versus placebo in trials including people experiencing depressive symptoms, without a formal diagnosis of depression, appeared ineffective (eleven RCTs; N = 2,712; SMD = −0.18; 95%CI = −0.41 to 0.04) (De Giorgi et al., Citation2022).
Some clinical trials could not be entered in the quantitative synthesis of the meta-analyses above for a variety of reasons, including lack of usable data or a non-randomised and/or non-controlled design. Notably, these included the only negative crossover RCT, conducted on 120 hyperlipidaemic men aged 35–64 years, for whom simvastatin dispensed for 24 weeks led to a small increase in scores on the Beck Depression Inventory (BDI) (MD = 0.06; 95%CI = 0.01–0.12) compared to placebo (Hyyppä et al., Citation2003). A trial comparing simvastatin versus atorvastatin (i.e. without a placebo arm) in 46 post-coronary artery bypass patients with comorbid mild-to-moderate depression showed that depression scores measured on the Hamilton Depression Rating Scale (HDRS) at 6 weeks were significantly lower in the simvastatin group (MD = 3.63; 95%CI = 0.44–6.51) (Abbasi et al., Citation2015). A small (N = 10), recent RCT randomised participants to either rosuvastatin or placebo plus SSRI: improvements on depression scales (BDI and HDRS) were observed in both groups, and were reportedly larger in those treated with a statin on the BDI (placebo p = 0.038; rosuvastatin p < 0.001) but not on the HDRS (placebo p < 0.002; rosuvastatin p < 0.001) (Massardo et al., Citation2022); however, no test for directly comparing the two groups was performed
Observational studies and their meta-analyses
Several observational studies and their meta-analyses are available, showing more variable results for the effects of statins in depression (positive = 25, none = 20, negative = 7), likely due to different designs and populations, exposures/comparisons, and outcomes of interest. However, compared to interventional trials, observational data retains great value as it can benefit from oftentimes larger unselected study populations and longer follow-ups (Kennedy-Martin et al., Citation2015).
Neither of the two most recent meta-analyses of observational studies could identify an effect of statins in depression. The larger one included thirteen observational studies over 5,035,070 participants and initially found a positive effect on the odds of depression for statin users [odds ratio (OR) = 0.85; 95%CI = 0.72–0.99], but no association (OR = 0.87; 95%CI = 0.74–1.02) was eventually confirmed when a trim-and-fill analysis, which corrects for publication bias, was employed (Lee et al., Citation2021b). The other meta-analysis investigated several cardiovascular medications and comprised nineteen observational studies over 178,278 participants on statins, again not finding any association between these drugs and depression (OR = 0.78; 95%CI = 0.57–1.06) (Zhang et al., Citation2022).
Some recent observational studies were not included in the previous meta-analyses. A historical cohort study over 21 years of prescription data from 497,080 statin users found that these medications decreased the rate of incident depression (trend test for statin prescription = 0.92; 95%CI = 0.92–0.95) (Kessing et al., Citation2019). Similar results for a larger sample of 1,149,384 statin users followed for 8 years were seen in an epidemiological investigation using a within-subject design, which showed that presentations to mental health services for depressive episodes were less frequent during periods on statins compared to periods off them [hazard ratio (HR)= 0.91; 95%CI 0.88–0.94] (Molero et al., Citation2020).
In contrast, two studies highlighted a harmful association between statins and depression. One was conducted on a large nationwide database (N = 7,481,168) and observed an overrepresentation of depressive disorders in statin users compared to non-users (OR = 1.22; 95%CI 1.20–1.25), though this association appeared reversed when considering low doses of statins, and worsened in high-dose users (Leutner et al., Citation2021). Another used a Mendelian randomisation methodology and likewise noted a 12% increase in the odds of depression for people taking statins (N = 188,000; 95%CI = 1.04–1.18) (Alghamdi et al., Citation2018). Interestingly, a propensity-score matched analysis of 193,977 statin users and 193,977 non-users also revealed higher hazards of depression diagnosis in the exposed group (HR = 1.33; 95%CI = 1.31–1.35) followed for a mean 6.8-year, but such association became non-significant when controlled for antidepressant use (Köhler-Forsberg et al., Citation2019).
Only one earlier study on a cohort of SSRIs users had specifically focussed on the issue of concurrent statin and antidepressant use, yet it reported lower hazards for psychiatric hospital contacts due to depression (N = 872,216; HR = 0.64; 95%CI = 0.55–0.75] among those using statins plus SSRIs versus SSRIs-only (Köhler et al., Citation2016). We are currently working on a real-world, primary care-based study comparing statin use against non-use in two cohorts of patients diagnosed with first-episode depression: one including only people initiating for the first time an antidepressant therapy (i.e. statin plus antidepressant versus antidepressant alone); the other encompassing all statin users versus non-users (De Giorgi et al., Citation2022). Preliminary analyses show a more positive profile for the combined strategy of statins and antidepressants (unpublished material), which is in line with findings from meta-analyses of clinical trials (De Giorgi et al., Citation2021, Citation2022; Yatham et al., Citation2019), but more definitive evidence is required before drawing any conclusion on the potential augmentative effects of statins on antidepressants.
Statins as a tool for innovation in psychiatry
Based on the translational and clinical findings presented above, the repurposing of statins for depressive disorders seems particularly tempting. These “old-school” drugs are safe (Collins et al., Citation2016) and commonly used in today medical practice (Urquhart, Citation2019), but for mental health researchers and psychiatrists they are novel because they can target underexplored biological pathways implicated in depression while also showing promising signs of efficacy, or at least no harm, in patients with depressive illness. Naturally, the available evidence remains preliminary, and these exciting perspectives must be taken with caution and further investigated (Köhler-Forsberg et al., Citation2020). While statins may not be the next ‘breakthrough’ in antidepressant development, nevertheless some interesting implications for research and clinical practice can already be argued.
Implications for research: approaching “precision” in depression
From a translational, “backward” perspective (), statins have pleiotropic actions (Yu & Liao, Citation2022) on a very large number of neurobiological and neuropsychological, endocrine-metabolic, cardiovascular, and immunological processes: the relationship between all these factors and their exact consequences in terms of antidepressant or depressogenic effect may have not been unravelled, but their relevance to depression is strengthened and expands beyond the classic monoamine hypothesis to explain it (Hirschfeld, Citation2000).
In other words, statins can be used as a dependable, if somewhat unselective probe into the role of factors such as dyslipidaemia (Can et al., Citation2012; Citraro et al., Citation2014; Persons et al., Citation2016; Segatto et al., Citation2014), HPA axis abnormalities (ElBatsh, Citation2015; Kumar et al., Citation2012; Lin et al., Citation2014; Pellosmaa et al., Citation2015; Pellosmaa & Dougall, Citation2016; Sheets et al., Citation2016), changes in emotional processing (De Giorgi et al., Citation2021; Citation2022; Gillespie et al., Citation2022), or inflammation (Hai-Na et al., Citation2020; Kang et al., Citation2016; Kim et al., Citation2018; Lesperance et al., Citation2004; Lim et al., Citation2017; Ma et al., Citation2016; Menze et al., Citation2021; Sheets et al., Citation2016; Wu et al., Citation2019; Yu et al., Citation2019; Zhang et al., Citation2017), as well as some of their interactions, in the physiopathology of depressive disorders. This list is hardly exhaustive: for example, statin therapy has recently been associated with a reduction of gut microbiota dysbiosis and thus systemic inflammation (Vieira-Silva et al., Citation2020), which in turn seem involved in the onset of depressive symptoms (Eltokhi & Sommer, Citation2022) and could mediate antidepressant response (McGovern et al., Citation2019) via the gut-brain axis.
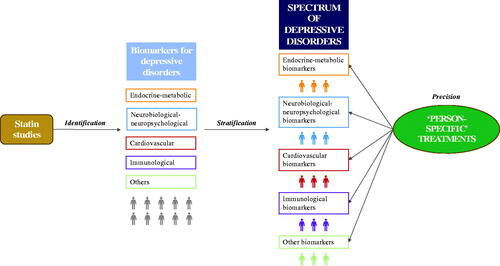
From a translational, “forward” perspective (), these factors may become useful, oftentimes easily measurable (e.g. lipid profile, cortisol levels, negative emotional bias, or CRP and other peripheral cytokines) biomarkers that can be utilised in the design of more precise studies for developing new antidepressants or repurposing other medications as such. It is likely that either a deficit or an exaggeration of some, but not all the above mechanisms at the same time would characterise different clinical presentations on a spectrum of depressive disorders requiring treatment(s) addressing those specific dysfunctions (Maj et al., Citation2020).
Here, statins widespread activities are double-edged, as in practice they would turn into altering certain physiological functions that are not necessarily helpful, or are in fact plainly unhelpful, for eliciting an antidepressant response. An example of this is perhaps observable by comparing the results of those meta-analyses that had suggested a positive effect of statins in people formally diagnosed with a depressive disorder (De Giorgi et al., Citation2021; Yatham et al., Citation2019) against those that had found no overall effect of statins on depressive symptoms in heterogenous populations with subclinical depressive symptoms and a variety of underlying medical disorders (De Giorgi et al., Citation2022; Yatham et al., Citation2019).
Several physical comorbidities such as hyperlipidaemia (Wee et al., Citation2016), cardiovascular (Wium-Andersen et al., Citation2017b) or cerebrovascular (Wium-Andersen et al., Citation2017a) diseases, neurodegenerative (Sparks et al., Citation2005) and inflammatory (Kang et al., Citation2016; Kim et al., Citation2018) disorders, as well as demographic variables such as age (Berk et al., Citation2020; Kim et al., Citation2019; Redlich et al., Citation2014) and sex (Feng et al., Citation2010; Pasco et al., Citation2010; Williams et al., Citation2016) can likewise present with an array of risk factors for depression, which would relate to a variable antidepressant efficacy for statins. In this respect, statins would not be used directly as a “precision” treatment for individual patients with depression. However, statin studies () may help approaching that by identifying biomarkers that can stratify these subjects according to different subtypes of depressive disorders (Arns et al., Citation2022).
Then, for example, people whose depression presents with a prominently immunological component, as observed via biomarkers such as elevated peripheral cytokines (Miller et al., Citation2017), could be targeted with more selective immunomodulatory drugs (Drevets et al., Citation2022), while others whose symptoms seem associated with interconnected inflammatory and endocrine-metabolic abnormalities, such as obesity, lipid dysregulation, and insulin resistance (Jones et al., Citation2021; Qiu et al., Citation2021), may benefit from broader approaches ranging from conventional treatments including diet and exercise (Jacka & Berk, Citation2013) and statins themselves (De Giorgi et al., Citation2021), to newer drugs such as glucagon‐like peptide‐1 (GLP1) receptor agonists (Detka & Głombik, Citation2021). Ultimately, an integration of advanced data from sources such as multi-omics, neuroimaging, artificial intelligence, and molecular epidemiology and physiology studies will converge towards recognising specific clusters of biomarkers that can lead to precise, person-specific treatments (Fernandes et al., Citation2017).
Implications for clinical practice: physical health in depression
The scandal of the “mortality gap,” mostly due to comorbid physical illness(Momen et al., Citation2022; Weye et al., Citation2020), in people with mental disorders including depression is a notorious, much debated topic (Fiorillo & Sartorius, Citation2021), which has become even more relevant in the context of the Covid-19 pandemic and its aftermath (Fiorillo & Gorwood, Citation2020). Lifestyle psychosocial interventions have proved useful for improving physical health (Luciano et al., Citation2021) and reducing mortality (Fiorillo et al., Citation2019), but several barriers, including concordance with treatment, may hinder their immediate application to patients suffering from depressive symptoms. Adherence to pharmacological treatment, especially antidepressants, is another significant issue (Dell’Osso et al., Citation2020) that has been associated with ill-health and mortality in depression (Krivoy et al., Citation2016).
Overall, interventions aimed at improving the physical health of patients with depressive disorders are under researched and even less frequently applied to clinical practice, but if psychiatry is to fully integrate with modern medicine, it becomes paramount that psychiatrists work confidently at the interplay between physical and mental illness (Fiorillo & Maj, Citation2018). Here, the use of statins in depression can already provide a clinically meaningful opportunity.
Firstly, in spite of the established physical health benefits (Yebyo et al., Citation2019) and decrease in all-cause mortality (Gitsels et al., Citation2021) associated with statin therapy, there are reports of systematic underuse of these medications in patients with depression (Ljung et al., Citation2021) – precisely those individuals who might benefit the most from their positive cardiometabolic effects (Vancampfort et al., Citation2017). Secondly, new research has found that statin adherence, concordance with antidepressant treatment, and lower mortality rates independently correlate with each other (Avrahamy et al., Citation2021). In line with this, preliminary analyses (unpublished material) of our ongoing study (De Giorgi et al., Citation2022) show that statin use can be associated with both lower antidepressant discontinuations and all-cause mortality, in the absence of any significant adverse events. Nevertheless, it remains possible that a spurious association between the use of medications such as statins and antidepressant efficacy might be partly explained by overall depression severity and related treatment adherence – despite more recent observational studies having controlled for these potential confounders.
In summary, emerging evidence advises that statin treatment may become a safe and viable strategy to improve both mental and physical health outcomes in patients with depressive disorders, but once again these suggestions must be corroborated by further studies before finding an application to clinical practice.
Conclusion
In this article, we have narratively reviewed the translational and clinical evidence for the effects of statins in depression. On these bases, we have argued that statins may be an instrument that brings novelty to psychiatry research and practice, including some potential implications for developing more precise antidepressant treatments and for better managing the physical health of patients with depressive disorders.
Several clinical and research questions remain unanswered. Do different populations likewise show an antidepressant response to statins? For example, healthy subjects, individuals at-risk for depression, patients with first-episode or treatment-resistant depressive disorders, people with heightened risk due to clinical-demographic characteristics associated to inflammation and dyslipidaemia might be more or less prone to respond to statins (De Giorgi et al., Citation2021).
Are individual statins capable of expressing distinct influences on mood and anxiety, and at which dosage and length of treatment? In this case, simvastatin’s profiling is emerging as superior to other statins (Abbasi et al., Citation2015; De Giorgi et al., Citation2021, Citation2022; Molero et al., Citation2020; Redlich et al., Citation2014), but dose- and time-response relationships remain ambiguous. Do statins work better as adjunct to conventional antidepressant, rather than a standalone treatment? The clinical evidence above seems to suggest so (De Giorgi et al., Citation2021, Citation2022; Yatham et al., Citation2019), but the biological and psychological (Al-Asmari et al., Citation2017; Bhattarai et al., Citation2017; Kilic et al., Citation2012; Li et al., Citation2017; Ludka et al., Citation2014; Renshaw et al., Citation2009; Santos et al., Citation2012) underpinnings of such augmentative effect must be better defined before having any meaningful medical application.
Are the existing outcome measures adequate for detecting the favourable or detrimental consequences of statin use in depression? Scales measuring depressive or anxiety symptoms, neuropsychological tasks, hard outcomes such as mortality, suicidality, and psychiatric hospitalisations: all have the potential to provide clinically and translationally useful insights, but it remains uncertain which one is better tailored to gauge the effects of statins in the context of depressive illness (De Giorgi et al., Citation2021). Overall, it is likely that many further investigations involving a variety of research designs (i.e. clinical and experimental medicine trials, observational studies) will be required before finding an answer to all these lingering queries.
Disclosure statement
CJH received consultancy fees from P1vital, Lundbeck, Servier, UCB, Zogenix, J&J, and Syndesi outside of the current work. The other authors declare that they have no conflict of interest.
References
- Abbasi, S. H., Mohammadinejad, P., Shahmansouri, N., Salehiomran, A., Beglar, A. A., Zeinoddini, A., Forghani, S., & Akhondzadeh, S. (2015). Simvastatin versus atorvastatin for improving mild to moderate depression in post-coronary artery bypass graft patients: A double-blind, placebo-controlled, randomized trial. Journal of Affective Disorders, 183, 149–155. https://doi.org/10.1016/j.jad.2015.04.049
- Al-Asmari, A. K., Ullah, Z., Al Masoudi, A. S., & Ahmad, I. (2017). Simultaneous administration of fluoxetine and simvastatin ameliorates lipid profile, improves brain level of neurotransmitters, and increases bioavailability of simvastatin. Journal of Experimental Pharmacology, ume 9, 47–57. https://doi.org/10.2147/JEP.S128696
- Alghamdi, J., Matou-Nasri, S., Alghamdi, F., Alghamdi, S., Alfadhel, M., & Padmanabhan, S. (2018). Risk of neuropsychiatric adverse effects of lipid-lowering drugs: A mendelian randomization study. International Journal of Neuropsychopharmacology, 21(12), 1067–1075. https://doi.org/10.1093/ijnp/pyy060
- Arns, M., van Dijk, H., Luykx, J. J., van Wingen, G., & Olbrich, S. (2022). Stratified psychiatry: Tomorrow's precision psychiatry? European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 55, 14–19. https://doi.org/10.1016/j.euroneuro.2021.10.863
- Avan, R., Sahebnasagh, A., Hashemi, J., Monajati, M., Faramarzi, F., Henney, N. C., Montecucco, F., Jamialahmadi, T., & Sahebkar, A. (2021). Update on statin treatment in patients with neuropsychiatric disorders. Life, 11(12), 1365. https://doi.org/10.3390/life11121365
- Avrahamy, H., Shoval, G., Hoshen, M., Balicer, R. D., Kamhi-Nesher, S., Zalsman, G., Weizman, A., & Krivoy, A. (2021). Association between adherence to SSRI treatment and mortality among individuals with metabolic syndrome components. Pharmacopsychiatry, 54(05), 232–239. https://doi.org/10.1055/a-1425-7246
- Bartoli, F., Cavaleri, D., Bachi, B., Moretti, F., Riboldi, I., Crocamo, C., & Carrà, G. (2021). Repurposed drugs as adjunctive treatments for mania and bipolar depression: A meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials. Journal of Psychiatric Research, 143, 230–238. https://doi.org/10.1016/j.jpsychires.2021.09.018
- Bartoli, F., Crocamo, C., Dakanalis, A., Riboldi, I., Miotto, A., Brosio, E., Clerici, M., & Carrà, G. (2017). Association between total serum cholesterol and suicide attempts in subjects with major depressive disorder: Exploring the role of clinical and biochemical confounding factors. Clinical Biochemistry, 50(6), 274–278. https://doi.org/10.1016/j.clinbiochem.2016.11.035
- Bartoli, F., Di Brita, C., Crocamo, C., Clerici, M., & Carrà, G. (2017). Lipid profile and suicide attempt in bipolar disorder: A meta-analysis of published and unpublished data. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 79(Pt B), 90–95. https://doi.org/10.1016/j.pnpbp.2017.06.008
- Berk, M., & Nierenberg, A. A. (2015). Three paths to drug discovery in psychiatry. The American Journal of Psychiatry, 172(5), 412–414. https://doi.org/10.1176/appi.ajp.2014.14070858
- Berk, M., Mohebbi, M., Dean, O. M., Cotton, S. M., Chanen, A. M., Dodd, S., Ratheesh, A., Amminger, G. P., Phelan, M., Weller, A., Mackinnon, A., Giorlando, F., Baird, S., Incerti, L., Brodie, R. E., Ferguson, N. O., Rice, S., Schäfer, M. R., Mullen, E., … Davey, C. G. (2020). Youth Depression Alleviation with Anti-inflammatory Agents (YoDA-A): A randomised clinical trial of rosuvastatin and aspirin. BMC Medicine, 18(1), 16. https://doi.org/10.1186/s12916-019-1475-6
- Bhattarai, B., Swamy, S., Baral, S. R., & Acharya, C. P. (2017). A study on the effect of atorvastatin on the pharmacokinetic and antidepressant activity of fluoxetine. National Journal of Physiology, Pharmacy and Pharmacology, 7(11), 1–1229. https://doi.org/10.5455/njppp.2017.7.0622519072017
- Binder, L. B., Ludka, F. K., Cunha, M. P., Dal-Cim, T., Constantino, L. C., Massari, C., Martins, W. C., Rodrigues, A. L. S., & Tasca, C. I. (2015). Atorvastatin prevents cell death and depressive-like behaviour induced by Abeta1-40 peptide via BDNF cleavage. Journal of Neurochemistry, 134(SUPPL. 1), 332–333. https://doi.org/10.1111/jnc.13189
- Bortolato, B., Miskowiak, K. W., Köhler, C. A., Maes, M., Fernandes, B. S., Berk, M., & Carvalho, A. F. (2016). Cognitive remission: A novel objective for the treatment of major depression? BMC Medicine, 14, 9. https://doi.org/10.1186/s12916-016-0560-3
- Bot, M., Milaneschi, Y., Al-Shehri, T., Amin, N., Garmaeva, S., Onderwater, G. L., Pool, R., Thesing, C. S., Vijfhuizen, L. S., Vogelzangs, N., Arts, I. C., Demirkan, A., van Duijn, C., van Greevenbroek, M., van der Kallen, C. J., Köhler, S., Ligthart, L., van den Maagdenberg, A. M., Mook-Kanamori, D. O., … Sattar, N. (2020). Metabolomics profile in depression: A pooled analysis of 230 metabolic markers in 5283 cases with depression and 10,145 controls. Biological Psychiatry. 87(5), 409–418. https://doi.org/10.1016/j.biopsych.2019.08.016
- Can, Ö. D., Ulupinar, E., Özkay, Ü. D., Yegin, B., & Öztürk, Y. (2012). The effect of simvastatin treatment on behavioral parameters, cognitive performance, and hippocampal morphology in rats fed a standard or a high-fat diet. Behavioural Pharmacology, 23(5–6), 582–592. https://doi.org/10.1097/FBP.0b013e328356c3f2
- Caspani, G., Turecki, G., Lam, R. W., Milev, R. V., Frey, B. N., MacQueen, G. M., Müller, D. J., Rotzinger, S., Kennedy, S. H., Foster, J. A., & Swann, J. R. (2021). Metabolomic signatures associated with depression and predictors of antidepressant response in humans: A CAN-BIND-1 report. Communications Biology, 4(1), 903. https://doi.org/10.1038/s42003-021-02421-6
- Chavez-Castillo, M., Nava, M., Ortega, A., Rojas, M., Nunez, V., Salazar, J., Bermudez, V., & Rojas-Quintero, J. (2020). Depression as an immunometabolic disorder: Exploring shared pharma-cotherapeutics with cardiovascular disease. Current Neuropharmacology, 18(11), 1138–1153. https://doi.org/10.2174/1570159X18666200413144401
- Ciccocioppo, R. (2017). Grand challenge in psychopharmacology: Setting priorities to shape a bright future. Frontiers in Psychiatry, 8, 15. https://doi.org/10.3389/fpsyt.2017.00015
- Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357–1366. https://doi.org/10.1016/S0140-6736(17)32802-7
- Citraro, R., Chimirri, S., Aiello, R., Gallelli, L., Trimboli, F., Britti, D., De Sarro, G., & Russo, E. (2014). Protective effects of some statins on epileptogenesis and depressive-like behavior in WAG/Rij rats, a genetic animal model of absence epilepsy. Epilepsia, 55(8), 1284–1291. https://doi.org/10.1111/epi.12686
- Collins, R., Reith, C., Emberson, J., Armitage, J., Baigent, C., Blackwell, L., Blumenthal, R., Danesh, J., Smith, G. D., DeMets, D., Evans, S., Law, M., MacMahon, S., Martin, S., Neal, B., Poulter, N., Preiss, D., Ridker, P., Roberts, I., … Peto, R. (2016). Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet, 388(10059), 2532–2561. https://doi.org/10.1016/S0140-6736(16)31357-5
- Covington, H. E., Vialou, V., & Nestler, E. J. (2010). From synapse to nucleus: Novel targets for treating depression. Neuropharmacology, 58(4–5), 683–693. https://doi.org/10.1016/j.neuropharm.2009.12.004
- Cuijpers, P., Noma, H., Karyotaki, E., Vinkers, C. H., Cipriani, A., & Furukawa, T. A. (2020). A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry, 19(1), 92–107. https://doi.org/10.1002/wps.20701
- da Cruz, J. N., Dal Magro, D. D., de Lima, D. D., & da Cruz, J. G. P. (2017). Simvastatin treatment reduces the cholesterol content of membrane/lipid rafts, implicating the N-methyl-D-aspartate receptor in anxiety: A literature review. Brazilian Journal of Pharmaceutical Sciences, 53(1), e16102. https://doi.org/10.1590/s2175-97902017000116102
- De Giorgi, R., De Crescenzo, F., Cowen, P. J., Harmer, C. J., & Cipriani, A. (2022). STAT-QResearch. OSF.
- De Giorgi, R., De Crescenzo, F., Rizzo Pesci, N., Martens, M., Howard, W., Cowen, P. J., & Harmer, C. J. (2021). Statins for major depressive disorder: A systematic review and meta-analysis of randomized controlled trials. PLOS One, 16(3), e0249409. https://doi.org/10.1371/journal.pone.0249409
- De Giorgi, R., Martens, M., Rizzo Pesci, N., Cowen, P. J., & Harmer, C. J. (2021). The effects of atorvastatin on emotional processing, reward learning, verbal memory and inflammation in healthy volunteers: An experimental medicine study. Journal of Psychopharmacology, 35(12), 1479–1487. https://ovidsp.ovid.com/ovidweb.cgi?T = JS&CSC = Y&NEWS = N&PAGE = fulltext&D = emexb&AN=2014417489
- De Giorgi, R., Quinton, A. G. M., Waters, S., Cowen, P. J., & Harmer, C. J. (2022). An experimental medicine study of the effects of simvastatin on emotional processing, reward learning, verbal memory, and inflammation in healthy volunteers. Psychopharmacology, 239(8), 2635–2645. https://doi.org/10.1007/s00213-022-06156-y
- De Giorgi, R., Rizzo Pesci, N., Quinton, A., De Crescenzo, F., Cowen, P. J., & Harmer, C. J. (2021). Statins in depression: An evidence-based overview of mechanisms and clinical studies. Frontiers in Psychiatry, 12, 702617. https://doi.org/10.3389/fpsyt.2021.702617
- De Giorgi, R., Waters, S., Pesci, N. R., Rosso, G., Cowen, P. J., & Harmer, C. J. (2022). The effects of statin monotherapy on depressive symptoms: A systematic review and meta-analysis. Journal of Affective Disorders, 311, 336–343. https://doi.org/10.1016/j.jad.2022.05.113
- Dell’Osso, B., Albert, U., Carrà, G., Pompili, M., Nanni, M. G., Pasquini, M., Poloni, N., Raballo, A., Sambataro, F., Serafini, G., Viganò, C., Demyttenaere, K., McIntyre, R. S., & Fiorillo, A. (2020). How to improve adherence to antidepressant treatments in patients with major depression: A psychoeducational consensus checklist. Annals of General Psychiatry, 19(1), 61. https://doi.org/10.1186/s12991-020-00306-2
- Demyttenaere, K., & Van Duppen, Z. (2019). The impact of (the concept of) treatment-resistant depression: An opinion review. The International Journal of Neuropsychopharmacology, 22(2), 85–92. https://doi.org/10.1093/ijnp/pyy052
- Detka, J., & Głombik, K. (2021). Insights into a possible role of glucagon-like peptide-1 receptor agonists in the treatment of depression. Pharmacological Reports, 73(4), 1020–1032. https://doi.org/10.1007/s43440-021-00274-8
- Downs, J. R., Oster, G., & Santanello, N. C. (1993). HMG CoA reductase inhibitors and quality of life. JAMA, 269(24), 3107–3108. https://doi.org/10.1001/jama.269.24.3107
- Drevets, W. C., Wittenberg, G. M., Bullmore, E. T., & Manji, H. K. (2022). Immune targets for therapeutic development in depression: Towards precision medicine. Nature Reviews. Drug Discovery, 21(3), 224–244. https://doi.org/10.1038/s41573-021-00368-1
- Ebada, M. E. (2017). Drug repurposing may generate novel approaches to treating depression. The Journal of Pharmacy and Pharmacology, 69(11), 1428–1436. https://doi.org/10.1111/jphp.12815
- Eisel, U. L. M., Dolga, A., Granic, I., Dobos, N., Naude, P., Nyakas, C., & Luiten, P. G. M. (2010). Inflammation as a target in neurodegenerative disease and related depression. Acta Physiologica Hungarica, 97(4), 437–438. https://doi.org/10.1556/APhysiol.97.2010.4.7
- ElBatsh, M. M. (2015). Antidepressant-like effect of simvastatin in diabetic rats. Canadian Journal of Physiology and Pharmacology, 93(8), 649–656. https://doi.org/10.1139/cjpp-2014-0560
- Eltokhi, A., & Sommer, I. E. (2022). A reciprocal link between gut microbiota, inflammation and depression: A place for probiotics? Frontiers in Neuroscience, 16, 852506. https://doi.org/10.3389/fnins.2022.852506
- Endo, A., Kuroda, M., & Tanzawa, K. (1976). Competitive inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase by ML-236A and ML-236B fungal metabolites, having hypocholesterolemic activity. FEBS Letters, 72(2), 323–326. https://doi.org/10.1016/0014-5793(76)80996-9
- Fabbri, C., Kasper, S., Zohar, J., Souery, D., Montgomery, S., Albani, D., Forloni, G., Ferentinos, P., Rujescu, D., Mendlewicz, J., De Ronchi, D., Riva, M. A., Lewis, C. M., & Serretti, A. (2021). Drug repositioning for treatment-resistant depression: Hypotheses from a pharmacogenomic study. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 104, 110050. https://doi.org/10.1016/j.pnpbp.2020.110050
- Farooqui, A. A., Ong, W. Y., Horrocks, L. A., Chen, P., & Farooqui, T. (2007). Comparison of biochemical effects of statins and fish oil in brain: The battle of the titans. Brain Research Reviews, 56(2), 443–471. https://doi.org/10.1016/j.brainresrev.2007.09.004
- Feng, L., Yap, K. B., Kua, E. H., & Ng, T. P. (2010). Statin use and depressive symptoms in a prospective study of community-living older persons. Pharmacoepidemiology and Drug Safety, 19(9), 942–948. https://doi.org/10.1002/pds.1993
- Fernandes, B. S., Williams, L. M., Steiner, J., Leboyer, M., Carvalho, A. F., & Berk, M. (2017). The new field of 'precision psychiatry. BMC Medicine, 15(1), 80. https://doi.org/10.1186/s12916-017-0849-x
- Fernandes, B., Dai, Y., Jia, P., & Zhao, Z. (2021). Charting the proteome landscape in major psychiatric disorders: from biomarkers to biological pathways for precision psychiatry. European Neuropsychopharmacology, 51, e171–e172. https://doi.org/10.1016/j.euroneuro.2021.08.137
- Fiorillo, A., & Gorwood, P. (2020). The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry: The Journal of the Association of European Psychiatrists, 63(1), e32. https://doi.org/10.1192/j.eurpsy.2020.35
- Fiorillo, A., & Maj, M. (2018). The role of psychiatry in modern medicine. International Review of Psychiatry, 30(2), 169–175. https://doi.org/10.1080/09540261.2018.1436675
- Fiorillo, A., & Sartorius, N. (2021). Mortality gap and physical comorbidity of people with severe mental disorders: The public health scandal. Annals of General Psychiatry, 20(1), 52. https://doi.org/10.1186/s12991-021-00374-y
- Fiorillo, A., Luciano, M., Pompili, M., & Sartorius, N. (2019). Editorial: Reducing the mortality gap in people with severe mental disorders: The role of lifestyle psychosocial interventions. Frontiers in Psychiatry, 10, 434. https://doi.org/10.3389/fpsyt.2019.00434
- Fracassi, A., Marangoni, M., Rosso, P., Pallottini, V., Fioramonti, M., Siteni, S., & Segatto, M. (2019). Statins and the brain: More than lipid lowering agents? Current Neuropharmacology, 17(1), 59–83. https://doi.org/10.2174/1570159x15666170703101816
- Furukawa, T. A., Shinohara, K., Sahker, E., Karyotaki, E., Miguel, C., Ciharova, M., Bockting, C. L. H., Breedvelt, J. J. F., Tajika, A., Imai, H., Ostinelli, E. G., Sakata, M., Toyomoto, R., Kishimoto, S., Ito, M., Furukawa, Y., Cipriani, A., Hollon, S. D., & Cuijpers, P. (2021). Initial treatment choices to achieve sustained response in major depression: A systematic review and network meta-analysis. World Psychiatry, 20(3), 387–396. https://doi.org/10.1002/wps.20906
- Gillespie, A. L., Wigg, C., van Assche, I., Murphy, S. E., & Harmer, C. J. (2022). Associations between statin use and negative affective bias during COVID-19: An observational, longitudinal UK study investigating depression vulnerability. Biological Psychiatry, S0006-3223(22)01126-X. https://doi.org/10.1016/j.biopsych.2022.03.009
- Gitsels, L. A., Bakbergenuly, I., Steel, N., & Kulinskaya, E. (2021). Do statins reduce mortality in older people? Findings from a longitudinal study using primary care records. A Family Medicine, Public and Community Health, 9(2):e000780. https://doi.org/10.1136/fmch-2020-000780
- Godlewska, B. R., & Harmer, C. J. (2021). Cognitive neuropsychological theory of antidepressant action: A modern-day approach to depression and its treatment. Psychopharmacology, 238(5), 1265–1278. https://doi.org/10.1007/s00213-019-05448-0
- Guerreiro Costa, F. L. N., Carneiro, B. A., Alves, G. S., Lins Silva, D. H., Faria Guimaraes, D., Souza, L. S., Bandeira, I. D., Beanes, G., Miranda Scippa, A., & Quarantini, L. C. (2022). Metabolomics of major depressive disorder: A systematic review of clinical studies. Cureus, 14(3), e23009. https://doi.org/10.7759/cureus.23009
- Hai-Na, Z., Xu-Ben, Y., Cong-Rong, T., Yan-Cheng, C., Fan, Y., Lei-Mei, X., Ruo-Lan, S., Ye-Zi, W., Liang, J., Ye-Zi , Ye-Xuan, W., & Jing, L. (2020). Atorvastatin ameliorates depressive behaviors and neuroinflammatory in streptozotocin-induced diabetic mice. Psychopharmacology, 237(3), 695–705. https://doi.org/10.1007/s00213-019-05406-w
- Hang, X., Zhang, Y., Li, J., Li, Z., Zhang, Y., Ye, X., Tang, Q., & Sun, W. (2021). Comparative efficacy and acceptability of anti-inflammatory agents on major depressive disorder: A network meta-analysis. Frontiers in Pharmacology, 12, 691200. https://doi.org/10.3389/fphar.2021.691200
- Harmer, C. J., Duman, R. S., & Cowen, P. J. (2017). How do antidepressants work? New perspectives for refining future treatment approaches. The Lancet Psychiatry, 4(5), 409–418. https://doi.org/10.1016/S2215-0366(17)30015-9
- Hayes, J. F., Lundin, A., Wicks, S., Lewis, G., Wong, I. C. K., Osborn, D. P. J., & Dalman, C. (2019). Association of hydroxylmethyl glutaryl coenzyme a reductase inhibitors, L-Type calcium channel antagonists, and biguanides with rates of psychiatric hospitalization and self-harm in individuals with serious mental illness. JAMA Psychiatry, 76(4), 382–390. https://doi.org/10.1001/jamapsychiatry.2018.3907
- Hirschfeld, R. M. (2000). History and evolution of the monoamine hypothesis of depression. The Journal of Clinical Psychiatry, 61 (Suppl 6), 4–6.
- Hyyppä, M. T., Kronholm, E., Virtanen, A., Leino, A., & Jula, A. (2003). Does simvastatin affect mood and steroid hormone levels in hypercholesterolemic men? A randomized double-blind trial. Psychoneuroendocrinology, 28(2), 181–194. https://doi.org/10.1016/S0306-4530(02)00014-8
- Irwin, J. C., Fenning, A. S., & Vella, R. K. (2020). Statins with different lipophilic indices exert distinct effects on skeletal, cardiac and vascular smooth muscle. Life Sciences, 242, 117225. https://doi.org/10.1016/j.lfs.2019.117225
- Jacka, F. N., & Berk, M. (2013). Depression, diet and exercise. The Medical Journal of Australia, 199(S6), S21–S23. https://doi.org/10.5694/mja12.10508
- James, S. L., Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N., Abbastabar, H., Abd-Allah, F., Abdela, J., Abdelalim, A., Abdollahpour, I., Abdulkader, R. S., Abebe, Z., Abera, S. F., Abil, O. Z., Abraha, H. N., Abu-Raddad, L. J., Abu-Rmeileh, N. M. E., Accrombessi, M. M. K., … Murray, C. J. L. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392(10159), 1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7
- Jarończyk, M., & Walory, J. (2022). Novel molecular targets of antidepressants. Molecules, 27(2), 533. https://doi.org/10.3390/molecules27020533
- Jones, B. D. M., Farooqui, S., Kloiber, S., Husain, M. O., Mulsant, B. H., & Husain, M. I. (2021). Targeting metabolic dysfunction for the treatment of mood disorders: Review of the evidence. Life, 11(8), 819. https://doi.org/10.3390/life11080819
- Kang, H. J., Bae, K. Y., Kim, S. W., Kim, J. T., Park, M. S., Cho, K. H., & Kim, J. M. (2016). Effects of interleukin-6, interleukin-18, and statin use, evaluated at acute stroke, on post-stroke depression during 1-year follow-up. Psychoneuroendocrinology, 72, 156–160. https://doi.org/10.1016/j.psyneuen.2016.07.001
- Kennedy-Martin, T., Curtis, S., Faries, D., Robinson, S., & Johnston, J. (2015). A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials, 16, 495. https://doi.org/10.1186/s13063-015-1023-4
- Kessing, L. V., Rytgaard, H. C., Gerds, T. A., Berk, M., Ekstrøm, C. T., & Andersen, P. K. (2019). New drug candidates for depression – a nationwide population-based study. Acta Psychiatrica Scandinavica, 139(1), 68–77. https://doi.org/10.1111/acps.12957
- Kilic, F. S., Ozatik, Y., Kaygisiz, B., Baydemir, C., & Erol, K. (2012). Acute antidepressant and anxiolytic effects of simvastatin and its mechanisms in rats. Neurosciences, 17(1), 39–43.
- Kilic, F. S., Ozatyk, Y., Kaygisiz, B., Baydemyr, C., & Erol, K. (2010). Focused Conference Group: P17 – Newapproaches and targets in psychiatry investigation of antidepressant and anxiolytic effects of simvastatine in rats. Basic and Clinical Pharmacology and Toxicology, 107(SUPPL. 1), 374. https://doi.org/10.1111/j.1742-7843.2010.00600.x
- Kim, S. W., Kang, H. J., Jhon, M., Kim, J. W., Lee, J. Y., Walker, A. J., Agustini, B., Kim, J. M., & Berk, M. (2019). Statins and inflammation: New therapeutic opportunities in psychiatry. Frontiers in Psychiatry, 10, 103. https://doi.org/10.3389/fpsyt.2019.00103
- Kim, S.-W., Kang, H.-J., Bae, K.-Y., Shin, I.-S., Hong, Y. J., Ahn, Y.-K., Jeong, M. H., Berk, M., Yoon, J.-S., & Kim, J.-M. (2018). Interactions between pro-inflammatory cytokines and statins on depression in patients with acute coronary syndrome. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 80(Pt C), 250–254. https://doi.org/10.1016/j.pnpbp.2017.07.003
- Köhler, O., Gasse, C., Petersen, L., Ingstrup, K. G., Nierenberg, A. A., Mors, O., & Østergaard, S. D. (2016). The effect of concomitant treatment with SSRIs and statins: A population-based study. The American Journal of Psychiatry, 173(8), 807–815. https://doi.org/10.1176/appi.ajp.2016.15040463
- Köhler-Forsberg, O., C, N. L., Hjorthøj, C., Nordentoft, M., Mors, O., & Benros, M. E. (2019). Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: Meta-analysis of clinical trials. Acta Psychiatrica Scandinavica, 139(5), 404–419. https://doi.org/10.1111/acps.13016
- Köhler-Forsberg, O., Gasse, C., Petersen, L., Nierenberg, A. A., Mors, O., & Østergaard, S. D. (2019). Statin treatment and the risk of depression. Journal of Affective Disorders, 246, 706–715. https://doi.org/10.1016/j.jad.2018.12.110
- Köhler-Forsberg, O., Otte, C., Gold, S. M., & Østergaard, S. D. (2020). Statins in the treatment of depression: Hype or hope? Pharmacology & Therapeutics, 215, 107625. https://doi.org/10.1016/j.pharmthera.2020.107625
- Kokkeler, K. J. E., Marijnissen, R. M., Wardenaar, K. J., Rhebergen, D., van den Brink, R. H. S., van der Mast, R. C., & Oude Voshaar, R. C. (2022). Subtyping late-life depression according to inflammatory and metabolic dysregulation: A prospective study. Psychological Medicine, 52(3), 515–525. https://doi.org/10.1017/s0033291720002159
- Kosowski, M., Smolarczyk-Kosowska, J., Hachuła, M., Maligłówka, M., Basiak, M., Machnik, G., Pudlo, R., & Okopień, B. (2021). The effects of statins on neurotransmission and their neuroprotective role in neurological and psychiatric disorders. Molecules, 26(10), 2838. https://doi.org/10.3390/molecules26102838
- Krivoy, A., Balicer, R. D., Feldman, B., Hoshen, M., Zalsman, G., Weizman, A., & Shoval, G. (2016). Adherence to antidepressants is associated with lower mortality: A 4-year population-based cohort study. The Journal of Clinical Psychiatry, 77(5), e566-572–e572. https://doi.org/10.4088/JCP.14m09531
- Kumar, A., Vashist, A., Kumar, P., Kalonia, H., & Mishra, J. (2012). Protective effect of HMG CoA reductase inhibitors against running wheel activity induced fatigue, anxiety like behavior, oxidative stress and mitochondrial dysfunction in mice. Pharmacological Reports, 64(6), 1326–1336. https://doi.org/10.1016/S1734-1140(12)70930-1
- Lee, M. C., Peng, T. R., Chen, B. L., Lee, C. H., Wang, J. Y., Lai, C. P., Lee, J. A., Chen, S. M., & Shiang, J. C. (2021a). Effects of various statins on depressive symptoms: A network meta-analysis. Journal of Affective Disorders, 293, 205–213. https://doi.org/10.1016/j.jad.2021.06.034
- Lee, M. C., Peng, T. R., Lee, C. H., Wang, J. Y., Lee, J. A., Chen, S. M., & Shiang, J. C. (2021b). Statin use and depression risk: A systematic review and meta-analysis. Journal of Affective Disorders, 282, 308–315. https://doi.org/10.1016/j.jad.2020.12.164
- Le-Niculescu, H., Roseberry, K., Gill, S. S., Levey, D. F., Phalen, P. L., Mullen, J., Williams, A., Bhairo, S., Voegtline, T., Davis, H., Shekhar, A., Kurian, S. M., & Niculescu, A. B. (2021). Precision medicine for mood disorders: Objective assessment, risk prediction, pharmacogenomics, and repurposed drugs. Molecular Psychiatry, 26(7), 2776–2804. doi:https://doi.org/10.1038/s41380-021-01061-w
- Lesperance, F., Frasure-Smith, N., Theroux, P., & Irwin, M. (2004). The association between major depression and levels of soluble intercellular adhesion molecule 1, lnterleukin-6, and C-reactive protein in patients with recent acute coronary syndromes. The American Journal of Psychiatry, 161(2), 271–277. doi:https://doi.org/10.1176/appi.ajp.161.2.271
- Leutner, M., Matzhold, C., Kautzky, A., Kaleta, M., Thurner, S., Klimek, P., & Kautzky-Willer, A. (2021). Major Depressive Disorder (MDD) and antidepressant medication are overrepresented in high-dose statin treatment. Frontiers in Medicine, 8, 608083. https://doi.org/10.3389/fmed.2021.608083
- Li, F., Ling, Z. L., Wang, Z. J., Zhong, Z. Y., Shu, N., Zhang, M., Liu, C., Liu, L., & Liu, X. D. (2017). Differential effects of pravastatin on the pharmacokinetics of paroxetine in normal and diabetic rats. Xenobiotica; The Fate of Foreign Compounds in Biological Systems, 47(1), 20–30. https://doi.org/10.3109/00498254.2016.1154999
- Lim, S.-W., Shiue, Y.-L., Liao, J.-C., Wee, H.-Y., Wang, C.-C., Chio, C.-C., Chang, C.-H., Hu, C.-Y., & Kuo, J.-R. (2017). Simvastatin therapy in the acute stage of traumatic brain injury attenuates brain trauma-induced depression-like behavior in rats by reducing neuroinflammation in the hippocampus. Neurocritical Care, 26(1), 122–132. https://doi.org/10.1007/s12028-016-0290-6
- Lin, P.-Y., Chang, A. Y. W., & Lin, T.-K. (2014). Simvastatin treatment exerts antidepressant-like effect in rats exposed to chronic mild stress. Pharmacology, Biochemistry, and Behavior, 124, 174–179. https://doi.org/10.1016/j.pbb.2014.06.006
- Ljung, R., Köster, M., Björkenstam, E., & Salmi, P. (2021). Associations between statin use and suicidality, depression, anxiety, and seizures. The Lancet. Psychiatry, 8(2), e2. https://doi.org/10.1016/s2215-0366(20)30512-5
- Luciano, M., Sampogna, G., Amore, M., Andriola, I., Calcagno, P., Carmassi, C., Del Vecchio, V., Dell'Osso, L., Di Lorenzo, G., Gelao, B., Giallonardo, V., Rossi, A., Rossi, R., Siracusano, A., & Fiorillo, A. (2021). How to improve the physical health of people with severe mental illness? A multicentric randomized controlled trial on the efficacy of a lifestyle group intervention. European Psychiatry, 64(1), e72. https://doi.org/10.1192/j.eurpsy.2021.2253
- Ludka, F. K., Constantino, L. C., Dal-Cim, T., Binder, L. B., Zomkowski, A., Rodrigues, A. L. S., & Tasca, C. I. (2016). Involvement of PI3K/Akt/GSK-3β and mTOR in the antidepressant-like effect of atorvastatin in mice. Journal of Psychiatric Research, 82, 50–57. https://doi.org/10.1016/j.jpsychires.2016.07.004
- Ludka, F. K., Constantino, L. C., Kuminek, G., Binder, L. B., Zomkowski, A. D. E., Cunha, M. P., Dal-Cim, T., Rodrigues, A. L. S., & Tasca, C. I. (2014). Atorvastatin evokes a serotonergic system-dependent antidepressant-like effect in mice. Pharmacology, Biochemistry, and Behavior, 122, 253–260. https://doi.org/10.1016/J.PBB.2014.04.005
- Ludka, F. K., Cunha, M. P., Dal-Cim, T., Binder, L. B., Constantino, L. C., Massari, C. M., Martins, W. C., Rodrigues, A. L. S., & Tasca, C. I. (2017a). Atorvastatin protects from Aβ1–40-induced cell damage and depressive-like behavior via ProBDNF cleavage (Vol. 54, pp.6163–6173): Springer.
- Ludka, F. K., Cunha, M. P., Dal-Cim, T., Binder, L. B., Constantino, L. C., Massari, C. M., Martins, W. C., Rodrigues, A. L. S., & Tasca, C. I. (2017b). Atorvastatin and fluoxetine prevent oxidative stress and mitochondrial dysfunction evoked by glutamate toxicity in hippocampal slices. Molecular Neurobiology, 54(8), 6163–6173. https://doi.org/10.1007/s12035-016-0134-6
- Ludka, F. K., Zomkowski, A. D., Cunha, M. P., Dal-Cim, T., Zeni, A. L., Rodrigues, A. L., & Tasca, C. I. (2013). Acute atorvastatin treatment exerts antidepressant-like effect in mice via the L-arginine-nitric oxide-cyclic guanosine monophosphate pathway and increases BDNF levels. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 23(5), 400–412. https://doi.org/10.1016/j.euroneuro.2012.05.005
- Ma, W., Shen, D., Liu, J., Pan, J., Yu, L., Shi, W., Deng, L., Zhu, L., Yang, F., Liu, J., Cai, W., Yang, J., Luo, Y., Cui, H., & Liu, S. (2016). Statin function as an anti-inflammation therapy for depression in patients with coronary artery disease by downregulating interleukin-1beta. Journal of Cardiovascular Pharmacology, 67(2), 129–135. https://doi.org/10.1097/FJC.0000000000000323
- Maes, M., Fisar, Z., Medina, M., Scapagnini, G., Nowak, G., & Berk, M. (2012). New drug targets in depression: Inflammatory, cell-mediate immune, oxidative and nitrosative stress, mitochondrial, antioxidant, and neuroprogressive pathways. and new drug candidates-Nrf2 activators and GSK-3 inhibitors. Inflammopharmacology, 20(3), 127–150. https://doi.org/10.1007/s10787-011-0111-7
- Maj, M., Stein, D. J., Parker, G., Zimmerman, M., Fava, G. A., De Hert, M., Demyttenaere, K., McIntyre, R. S., Widiger, T., & Wittchen, H. U. (2020). The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry, 19(3), 269–293. https://doi.org/10.1002/wps.20771
- Malhi, G. S., Bell, E., Morris, G., & Hamilton, A. (2020). The delay in response to antidepressant therapy: A window of opportunity? The Australian and New Zealand Journal of Psychiatry, 54(2), 127–129. https://doi.org/10.1177/0004867419900313
- Massardo, T., Quintana, J. C., Risco, L., Corral, S., Spuler, J., Vicentini, D., Castro-Muñoz, G., Riedel, B., Villa, C., & Pereira, J. I. (2022). Effect of low-dose statins in addition to standard therapy on brain perfusion and neurocognitive performance in patients with major depressive disorder. Neuropsychobiology, 81(4), 215–271. https://doi.org/10.1159/000521104
- Massardo, T., Quintana, J., Pereira, J., Saez, C., Risco, L., Corral, S., Olivares, N., Spuler, J., Castro, G., Vicentini, D., Riedel, B., Valenzuela, G., & Villa, C. (2020). Effect of statins on brain perfusion in major depression as an addition to standard therapy. SPM analysis of inflammation, platelet activation, endothelial dysfunction and neurocognitive parameters. European Journal of Nuclear Medicine and Molecular Imaging, 47(SUPPL 1), S446–S447. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed22&AN=634255459
- McFarland, A. J., Anoopkumar-Dukie, S., Arora, D. S., Grant, G. D., McDermott, C. M., Perkins, A. V., & Davey, A. K. (2014). Molecular mechanisms underlying the effects of statins in the central nervous system. International Journal of Molecular Sciences, 15(11), 20607–20637. https://doi.org/10.3390/ijms151120607
- McGovern, A. S., Hamlin, A. S., & Winter, G. (2019). A review of the antimicrobial side of antidepressants and its putative implications on the gut microbiome. The Australian and New Zealand Journal of Psychiatry, 53(12), 1151–1166. https://doi.org/10.1177/0004867419877954
- Menze, E. T., Ezzat, H., Shawky, S., Sami, M., Selim, E. H., Ahmed, S., Maged, N., Nadeem, N., Eldash, S., & Michel, H. E. (2021). Simvastatin mitigates depressive-like behavior in ovariectomized rats: Possible role of NLRP3 inflammasome and Estrogen receptors' modulation. International Immunopharmacology, 95, 107582. https://doi.org/10.1016/j.intimp.2021.107582
- Miller, A. H., Haroon, E., & Felger, J. C. (2017). Therapeutic implications of brain-immune interactions: Treatment in translation. Neuropsychopharmacology, 42(1), 334–359. https://doi.org/10.1038/npp.2016.167
- Mohammad Sadeghi, H., Adeli, I., Mousavi, T., Daniali, M., Nikfar, S., & Abdollahi, M. (2021). Drug repurposing for the management of depression: Where do we stand currently? Life, 11(8), 774. https://doi.org/10.3390/life11080774
- Molero, Y., Cipriani, A., Larsson, H., Lichtenstein, P., D'Onofrio, B. M., & Fazel, S. (2020). Associations between statin use and suicidality, depression, anxiety, and seizures: A Swedish total-population cohort study. The Lancet. Psychiatry, 7(11), 982–990. https://doi.org/10.1016/S2215-0366(20)30311-4
- Momen, N. C., Plana-Ripoll, O., Agerbo, E., Christensen, M. K., Iburg, K. M., Laursen, T. M., Mortensen, P. B., Pedersen, C. B., Prior, A., Weye, N., & McGrath, J. J. (2022). Mortality associated with mental disorders and comorbid general medical conditions. JAMA Psychiatry, 79(5), 444–453. https://doi.org/10.1001/jamapsychiatry.2022.0347
- Muldoon, M. F., Manuck, S. B., & Matthews, K. A. (1990). Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ, 301(6747), 309–314. https://doi.org/10.1136/bmj.301.6747.309
- Nestler, E. J., & Hyman, S. E. (2010). Animal models of neuropsychiatric disorders. Nature Neuroscience, 13(10), 1161–1169. https://doi.org/10.1038/nn.2647
- Neurauter, G., Wirleitner, B., Laich, A., Schennach, H., Weiss, G., & Fuchs, D. (2003). Atorvastatin suppresses interferon-gamma -induced neopterin formation and tryptophan degradation in human peripheral blood mononuclear cells and in monocytic cell lines. Clinical and Experimental Immunology, 131(2), 264–267. https://doi.org/10.1046/j.1365-2249.2003.02021.x
- Nothdurfter, C., Tanasic, S., Di Benedetto, B., Rammes, G., Wagner, E. M., Kirmeier, T., Ganal, V., Kessler, J. S., Rein, T., Holsboer, F., & Rupprecht, R. (2010). Impact of lipid raft integrity on 5-HT3 receptor function and its modulation by antidepressants. Neuropsychopharmacology, 35(7), 1510–1519. https://doi.org/10.1038/npp.2010.20
- Pasco, J. A., Jacka, F. N., Williams, L. J., Henry, M. J., Nicholson, G. C., Kotowicz, M. A., & Berk, M. (2010). Clinical implications of the cytokine hypothesis of depression: The association between use of statins and aspirin and the risk of major depression. Psychotherapy and Psychosomatics, 79(5), 323–325. https://doi.org/10.1159/000319530
- Pellosmaa, H., & Dougall, A. L. (2016). Examining the role of statins and mood on plasma lipids and health outcomes: A systematic review. Psychosomatic Medicine, 78(3), A94. https://doi.org/10.1097/PSY.0000000000000343
- Pellosmaa, H., Orsak, G., Tebbe, D., Jenney, C., Das, S., Thompson, J., Carroll, J., Feldman, M., Vecchio, M., & Dougall, A. L. (2015). Managing high cholesterol: Relationships among stress, depression, adherence and inflammatory markers. Psychosomatic Medicine, 77(3), A136. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed16&NEWS=N&AN=71869347
- Persons, J. E., Robinson, J. G., Coryell, W. H., Payne, M. E., & Fiedorowicz, J. G. (2016). Longitudinal study of low serum LDL cholesterol and depressive symptom onset in postmenopause. The Journal of Clinical Psychiatry, 77(02), 212–220. https://doi.org/10.4088/JCP.14m09505
- Qiu, W., Cai, X., Zheng, C., Qiu, S., Ke, H., & Huang, Y. (2021). Update on the relationship between depression and neuroendocrine metabolism. Frontiers in Neuroscience, 15, 728810. https://doi.org/10.3389/fnins.2021.728810
- Rahola, J. G. (2012). Somatic drugs for psychiatric diseases: Aspirin or simvastatin for depression? Current Neuropharmacology, 10(2), 139–158. https://doi.org/10.2174/157015912800604533
- Redlich, C., Berk, M., Williams, L. J., Sundquist, J., Sundquist, K., & Li, X. (2014). Statin use and risk of depression: A Swedish National Cohort Study. BMC Psychiatry, 14(1), 348. https://doi.org/10.1186/s12888-014-0348-y
- Renshaw, P. F., Parsegian, A., Yang, C. K., Novero, A., Yoon, S. J., Lyoo, I. K., Cohen, B. M., & Carlezon, W. A. Jr, (2009). Lovastatin potentiates the antidepressant efficacy of fluoxetine in rats. Pharmacology, Biochemistry, and Behavior, 92(1), 88–92. https://doi.org/10.1016/j.pbb.2008.10.017
- Rush, A. J., Sackeim, H. A., Conway, C. R., Bunker, M. T., Hollon, S. D., Demyttenaere, K., Young, A. H., Aaronson, S. T., Dibué, M., Thase, M. E., & McAllister-Williams, R. H. (2022). Clinical research challenges posed by difficult-to-treat depression. Psychological Medicine, 52(3), 419–432. https://doi.org/10.1017/s0033291721004943
- Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Stewart, J. W., Warden, D., Niederehe, G., Thase, M. E., Lavori, P. W., Lebowitz, B. D., McGrath, P. J., Rosenbaum, J. F., Sackeim, H. A., Kupfer, D. J., Luther, J., & Fava, M. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. American Journal of Psychiatry, 163(11), 1905–1917. https://doi.org/10.1176/ajp.2006.163.11.1905
- Santos, T., Baungratz, M. M., Haskel, S. P., de Lima, D. D., da Cruz, J. N., Magro, D. D. D., & da Cruz, J. G. P. (2012). Behavioral interactions of simvastatin and fluoxetine in tests of anxiety and depression. Neuropsychiatric Disease and Treatment, 8, 413–422. https://doi.org/10.2147/NDT.S31714
- Segatto, M., Manduca, A., Lecis, C., Rosso, P., Jozwiak, A., Swiezewska, E., Moreno, S., Trezza, V., & Pallottini, V. (2014). Simvastatin treatment highlights a new role for the isoprenoid/cholesterol biosynthetic pathway in the modulation of emotional reactivity and cognitive performance in rats. Neuropsychopharmacology, 39(4), 841–854. https://doi.org/10.1038/npp.2013.284
- Sheets, W. J., Brooks, S. D., Chantler, P., & Frisbee, J. (2016). Interventions blunting systemic inflammation and oxidant stress improve depressive symptoms and vascular function in a model of metabolic syndrome. FASEB Journal. 30, 948. http://www.fasebj.org/content/30/1_Supplement/948.15.abstract?sid=8311572a-92b5-4c61-a93c-7deaa58e0821
- Shin, J. Y., Suls, J., & Martin, R. (2008). Are cholesterol and depression inversely related? A meta-analysis of the association between two cardiac risk factors. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 36(1), 33–43. https://doi.org/10.1007/s12160-008-9045-8
- Shrivastava, S., Pucadyil, T. J., Paila, Y. D., Ganguly, S., & Chattopadhyay, A. (2010). Chronic cholesterol depletion using statin impairs the function and dynamics of human serotonin 1A receptors †. Biochemistry, 49(26), 5426–5435. https://doi.org/10.1021/bi100276b
- Simons, J. (2003). The $10 billion pill. Fortune, 147(1), 58–62.
- Sizar, O., Khare, S., Jamil, R. T., & Talati, R. (2022). Statin medications. In StatPearls. StatPearls Publishing, Copyright © 2022, StatPearls Publishing LLC.
- So, H. C., Chau, C. K., Lau, A., Wong, S. Y., & Zhao, K. (2019). Translating GWAS findings into therapies for depression and anxiety disorders: Gene-set analyses reveal enrichment of psychiatric drug classes and implications for drug repositioning. Psychological Medicine, 49(16), 2692–2708. https://doi.org/10.1017/s0033291718003641
- Solmi, M., Miola, A., Croatto, G., Pigato, G., Favaro, A., Fornaro, M., Berk, M., Smith, L., Quevedo, J., Maes, M., Correll, C. U., & Carvalho, A. F. (2021). How can we improve antidepressant adherence in the management of depression? A targeted review and 10 clinical recommendations. Revista Brasileira de Psiquiatria, 43(2), 189–202. https://doi.org/10.1590/1516-4446-2020-0935
- Sparks, D. L., Sabbagh, M. N., Connor, D. J., Lopez, J., Launer, L. J., Browne, P., Wasser, D., Johnson-Traver, S., Lochhead, J., & Ziolwolski, C. (2005). Atorvastatin for the treatment of mild to moderate Alzheimer disease: Preliminary results. Archives of Neurology, 62(5), 753–757. https://ovidsp.ovid.com/ovidweb.cgi?T = JS&CSC = Y&NEWS = N&PAGE = fulltext&D = emed9&AN=40656090
- Tang, C.-R., Yu, X.-B., Zhang, H.-N., Cao, Y.-C., Yang, F., Xu, L.-M., Sun, R.-L., Ye, Z., Wang, Y.-X., & Liang, J. (2020). Lovastatin prevents depressive behaviors and increased hippocampal neurogenesis in streptozotocin-induced diabetic mice. Pharmacology, 105(5–6), 339–348. https://doi.org/10.1159/000503865
- Tao, S. H., Ren, X. Q., Zhang, L. J., & Liu, M. Y. (2021). Association between common cardiovascular drugs and depression. Chinese Medical Journal, 134(22), 2656–2665. doi:https://doi.org/10.1097/CM9.0000000000001875
- Taylor, W. D., Aizenstein, H. J., & Alexopoulos, G. S. (2013). The vascular depression hypothesis: Mechanisms linking vascular disease with depression. Molecular Psychiatry, 18(9), 963–974. https://doi.org/10.1038/mp.2013.20
- Tsai, S.-J. (2007). Statins may enhance the proteolytic cleavage of proBDNF: Implications for the treatment of depression. Medical Hypotheses, 68(6), 1296–1299. https://doi.org/10.1016/j.mehy.2006.09.043
- Urquhart, L. (2019). Top drugs and companies by sales in 2018. Nature Reviews Drug Discovery, 18, 245. https://doi.org/10.1038/d41573-019-00049-0
- van Agtmaal, M. J. M., Houben, A., Pouwer, F., Stehouwer, C. D. A., & Schram, M. T. (2017). Association of microvascular dysfunction with late-life depression: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 729–739. https://doi.org/10.1001/jamapsychiatry.2017.0984
- Vancampfort, D., Correll, C. U., Wampers, M., Sienaert, P., Mitchell, A. J., De Herdt, A., Probst, M., Scheewe, T. W., & De Hert, M. (2014). Metabolic syndrome and metabolic abnormalities in patients with major depressive disorder: A meta-analysis of prevalences and moderating variables. Psychological Medicine, 44(10), 2017–2028. https://doi.org/10.1017/S0033291713002778
- Vancampfort, D., Firth, J., Schuch, F. B., Rosenbaum, S., Mugisha, J., Hallgren, M., Probst, M., Ward, P. B., Gaughran, F., De Hert, M., Carvalho, A. F., & Stubbs, B. (2017). Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: A global systematic review and meta-analysis. World Psychiatry, 16(3), 308–315. https://doi.org/10.1002/wps.20458
- Vieira-Silva, S., Falony, G., Belda, E., Nielsen, T., Aron-Wisnewsky, J., Chakaroun, R., Forslund, S. K., Assmann, K., Valles-Colomer, M., Nguyen, T. T. D., Proost, S., Prifti, E., Tremaroli, V., Pons, N., Le Chatelier, E., Andreelli, F., Bastard, J.-P., Coelho, L. P., Galleron, N., … Raes, J. (2020). Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature, 581(7808), 310–315. https://doi.org/10.1038/s41586-020-2269-x
- Walker, A. J., Kim, Y., Borissiouk, I., Rehder, R., Dodd, S., Morris, G., Nierenberg, A. A., Maes, M., Fernandes, B. S., Dean, O. M., Williams, L. J., Eyre, H. A., Kim, S. W., Zoungas, S., Carvalho, A. F., & Berk, M. (2021). Statins: Neurobiological underpinnings and mechanisms in mood disorders. Neuroscience and Biobehavioral Reviews, 128, 693–708. https://doi.org/10.1016/j.neubiorev.2021.07.012
- Wang, Q., Zengin, A., Deng, C., Li, Y., Newell, K. A., Yang, G. Y., Lu, Y., Wilder-Smith, E. P., Zhao, H., & Huang, X. F. (2009). High dose of simvastatin induces hyperlocomotive and anxiolytic-like activities: The association with the up-regulation of NMDA receptor binding in the rat brain. Experimental Neurology, 216(1), 132–138. https://doi.org/10.1016/j.expneurol.2008.11.016
- Wee, H.-Y., Ho, C.-H., Fu , Liang, W., Hsieh, K.-Y., Wang, C.-C., Wang, J.-J., Chio, C.-C., Chang, C.-H., & Kuo, J.-R. (2016). Increased risk of new-onset depression in patients with traumatic brain injury and hyperlipidemia: The important role of statin medications. The Journal of Clinical Psychiatry, 77(4), 505–511. https://doi.org/10.4088/JCP.14m09749
- Weye, N., Momen, N. C., Christensen, M. K., Iburg, K. M., Dalsgaard, S., Laursen, T. M., Mortensen, P. B., Santomauro, D. F., Scott, J. G., Whiteford, H. A., McGrath, J. J., & Plana-Ripoll, O. (2020). Association of specific mental disorders with premature mortality in the Danish population using alternative measurement methods. JAMA Network Open, 3(6), e206646. https://doi.org/10.1001/jamanetworkopen.2020.6646
- Williams, L. J., Pasco, J. A., Mohebbi, M., Jacka, F. N., Stuart, A. L., Venugopal, K., O’Neil, A., & Berk, M. (2016). Statin and aspirin use and the risk of mood disorders among men. International Journal of Neuropsychopharmacology, 19(6), pyw008. https://doi.org/10.1093/ijnp/pyw008
- Wirleitner, B., Rudzite, V., Neurauter, G., Murr, C., Kalnins, U., Erglis, A., Trusinskis, K., & Fuchs, D. (2003). Immune activation and degradation of tryptophan in coronary heart disease. European Journal of Clinical Investigation, 33(7), 550–554. https://doi.org/10.1046/j.1365-2362.2003.01186.x
- Wirleitner, B., Sperner-Unterweger, B., & Fuchs, D. (2004). Statins to reduce risk of depression. Journal of the American College of Cardiology, 43(6), 1132–1133. https://doi.org/10.1016/j.jacc.2003.12.029
- Wium-Andersen, I. K., Wium-Andersen, M. K., Jørgensen, M. B., & Osler, M. (2017a). Anti-inflammatory treatment and risk for depression after first-time stroke in a cohort of 147 487 Danish patients. Journal of Psychiatry & Neuroscience, 42(5), 320–330. https://doi.org/10.1503/jpn160244
- Wium-Andersen, I. K., Wium-Andersen, M. K., Jørgensen, M. B., & Osler, M. (2017b). Anti-inflammatory treatment and risk of depression in 91,842 patients with acute coronary syndrome and 91,860 individuals without acute coronary syndrome in Denmark. International Journal of Cardiology, 246, 1–6. https://doi.org/10.1016/j.ijcard.2017.05.105
- Wu, H., Lv, W., Pan, Q., Kalavagunta, P. K., Liu, Q., Qin, G., Cai, M., Zhou, L., Wang, T., Xia, Z., & Shang, J. (2019). Simvastatin therapy in adolescent mice attenuates HFD-induced depression-like behavior by reducing hippocampal neuroinflammation. Journal of Affective Disorders, 243, 83–95. https://doi.org/10.1016/j.jad.2018.09.022
- Wu, S., Ding, Y., Wu, F., Xie, G., Hou, J., & Mao, P. (2016). Serum lipid levels and suicidality: A meta-analysis of 65 epidemiological studies. Journal of Psychiatry & Neuroscience, 41(1), 56–69. https://doi.org/10.1503/jpn.150079
- Yan, J., Xu, Y., Zhu, C., Zhang, L., Wu, A., Yang, Y., Xiong, Z., Deng, C., Huang, X. F., Yenari, M. A., Yang, Y. G., Ying, W., & Wang, Q. (2011). Simvastatin prevents dopaminergic neurodegeneration in experimental parkinsonian models: The association with anti-inflammatory responses. PLOS One, 6(6), e20945. https://doi.org/10.1371/journal.pone.0020945
- Yang, C.-C., Jick, S. S., & Jick, H. (2003). Lipid-lowering drugs and the risk of depression and suicidal behavior. (Vol. 163, pp. 1926): American Medical Association.
- Yatham, M. S., Yatham, K. S., Ravindran, A. V., & Sullivan, F. (2019). Do statins have an effect on depressive symptoms? A systematic review and meta-analysis. Journal of Affective Disorders, 257, 55–63. https://doi.org/10.1016/j.jad.2019.07.002
- Yebyo, H. G., Aschmann, H. E., & Puhan, M. A. (2019). Finding the balance between benefits and harms when using statins for primary prevention of cardiovascular disease: A modeling study. Annals of Internal Medicine, 170(1), 1–10. https://doi.org/10.7326/m18-1279
- Yu, D., & Liao, J. K. (2022). Emerging views of statin pleiotropy and cholesterol lowering. Cardiovascular Research, 118(2), 413–423. https://doi.org/10.1093/cvr/cvab032
- Yu, X.-B., Zhang, H.-N., Dai, Y., Zhou, Z.-Y., Xu, R-a., Hu, L.-F., Zhang, C.-H., Xu, H.-Q., An, Y.-Q., Tang, C.-R., & Lin, G.-Y. (2019). Simvastatin prevents and ameliorates depressive behaviors via neuroinflammatory regulation in mice. Journal of Affective Disorders, 245, 939–949. https://doi.org/10.1016/j.jad.2018.11.086
- Zanos, P., & Gould, T. D. (2018). Mechanisms of ketamine action as an antidepressant. Molecular Psychiatry, 23(4), 801–811. https://doi.org/10.1038/mp.2017.255
- Zeiser, R. (2018). Immune modulatory effects of statins. Immunology, 154(1), 69–75. https://doi.org/10.1111/imm.12902
- Zhang, H. N., Xu, H., Yu, X. B., Wang, C. Z., Xu, Q. Q., Dai, G. X., Hu, L. F., & Zhang, X. H. (2017). Effect of simvastatin on lipopolysaccharides induced depressive behaviors and neuroinflammation in mice. Chinese Pharmacological Bulletin, 33(3), 373–378. https://doi.org/10.3969/j.issn.1001-1978.2017.03.016
- Zhang, L., Bao, Y., Tao, S., Zhao, Y., & Liu, M. (2022). The association between cardiovascular drugs and depression/anxiety in patients with cardiovascular disease: A meta-analysis. Pharmacological Research. 175, 106024. https://doi.org/10.1016/j.phrs.2021.106024