Psoriasis can be debilitating, as even objectively mild cases can have profound impact on a patient’s activities and social interactions. Highly efficacious treatment options are available (Citation1). Despite their high degree of efficacy, however, patients may be hesitant to use treatments due to fear of adverse events, fears which are often exacerbated by risk aversion.
Risk aversion is the tendency to avoid uncertain large risks by choosing another option with a more certain, but less beneficial, expected outcome. For example, a risk averse decision would be an investor electing a lower interest rate savings account instead of a high earning, high risk stock with a higher expected rate of return. Humans are naturally risk averse (Citation2). In a study of patients’ risk attitude regarding their health, 74% were either moderately or decidedly risk averse (Citation3). Risk aversion may lead to poor treatment decisions due to patients being unwilling to accept medication risks, despite the likelihood that the medication would be beneficial.
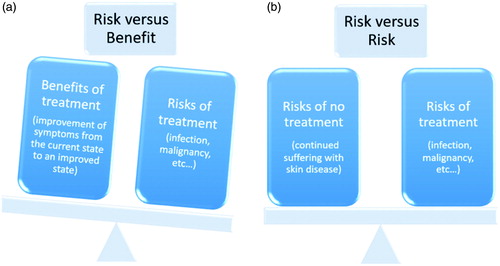
When physicians present treatment information to patients, the benefits of treatment are often presented alongside their risks. The tendency toward risk aversion may lead patients to weigh risks more heavily than benefits and thus lead to poor treatment choices. To neutralize risk aversion, treatment benefits can be reframed in terms of the risk of not taking treatment. While the discussion of risk versus risk may not fully overcome patients’ fears, risk versus benefit makes it even more difficult (Citation4).
Consider a 60-year-old patient with severe psoriasis who has failed treatment with methotrexate. The next step would be the introduction of a biologic, for which the standard risk versus benefit discussion would revolve around data supporting the efficacy of biologics and their potential rare risks of infection, malignancy, etc (Citation5). The benefits of treatment would be presented as the improvement of symptoms from the current state to an improved state. The decision would be framed around how willing the patient would be to accept the potential risks of the drug for potential disease improvement. This framing could very well discourage risk averse patients from the treatments that would help them.
To neutralize the effects of risk aversion and to help patients make a more objective determination, the side effect risks can be compared to the risk of non-treatment. The risk of non-treatment includes continued suffering with skin disease or the development of comorbidities such as cardiac disease or arthritis (Citation6). The patient is no longer presented with one risk and one benefit, but rather, there are now two possible risks being compared. This allows for neutralization of risk aversion and ultimately better positions the patient to make an informed decision regarding their treatment options ().
Figure 1. A treatment decision comparison between a “risk versus benefit” and “risk versus risk” presentation in a psoriasis patient. visually represents the risk versus benefit model. Patients, being naturally risk averse, internally weigh the risks of treatment more heavily than the benefits of treatment. Meanwhile, visually represents the risk versus risk model; two parallel risk structures are presented. In this scenario, the patient does not have a predilection for overweighting risks, and both treatment and non-treatment choices are evaluated on a more equal basis.
Elias Oussedik and Michael S. Anderson Center for Dermatology Research, Department of Dermatology Wake Forest School of Medicine, Winston-Salem, North Carolina Steven R. Feldman Center for Dermatology Research, Department of Dermatology Wake Forest School of Medicine Winston-Salem, North Carolina; Department of Pathology, Wake Forest School of Medicine, Winston-Salem, North Carolina; Department of Public Health Sciences, Wake Forest School of Medicine, Winston-Salem, North Carolina
Disclosure statement
Dr. Feldman is a speaker for Janssen and Taro. He has received research, speaking and/or consulting support from a variety of companies including Galderma, GSK/Stiefel, Almirall, Leo Pharma, Baxter, Boeringer Ingelheim, Mylan, Celgene, Pfizer, Valeant, Abbvie, Cosmederm, Anacor, Astellas, Janssen, Lilly, Merck, Merz, Novartis, Qurient, National Biological Corporation, Caremark, Advance Medical, Suncare Research, Informa, UpToDate and National Psoriasis Foundation. He is the founder and majority owner of www.DrScore.com. He is founder and part owner of Causa Research, a company dedicated to enhancing patients’ adherence to treatment. Michael Anderson and Elias Oussedik have no conflicts of interest to disclose.
Contents of the manuscript have not been previously published and are not currently submitted elsewhere.
References
- Sandoval LF, Pierce A, Feldman SR. Systemic therapies for psoriasis: an evidence-based update. Am J Clin Dermatol. 2014;15:165–80.
- Ortendahl M. Shared decision-making based on different features of risk in the context of diabetes mellitus and rheumatoid arthritis. Ther Clin Risk Manag. 2007;3:1175–80.
- Rosen AB, Tsai JS, Downs SM. Variations in risk attitude across race, gender, and education. Med Decis Mak. 2003;23:511–17.
- Bergus GR, Levin IP, Elstein AS. Presenting risks and benefits to patients. J Gen Intern Med. 2002;17:612–17.
- Lis K, Kuzawińska O, Bałkowiec-Iskra E. State of the art paper tumor necrosis factor inhibitors – state of knowledge. Arch Med Sci. 2014;6:1175–85.
- Saleem MD, Kesty C, Feldman SR. Relative versus absolute risk of comorbidities in patients with psoriasis. J Am Acad Dermatol. 2016:1–7.
