Abstract
Background: Psoriatic lesions in the genital area (GenPs) can cause considerable physical and emotional distress. To increase physician awareness, we estimated the GenPs prevalence among patients with psoriasis.
Methods: An English language literature search was performed. Articles reporting GenPs prevalence met the search criteria and were included. Because GenPs is rarely reported in demographics of prospective clinical trials, GenPs prevalence and baseline demographics of patients with and without GenPs in two prospective randomized phase 3b trials (NCT02561806 and NCT02634801) involving patients with moderate-to-severe psoriasis are reported.
Results: Overall, 600 references were screened. Eighteen articles met the search criteria. Patient populations were highly heterogeneous across articles. Broadly, the presence of GenPs was either physician-reported (physical examinations) or patient-reported (questionnaires). In the literature, GenPs prevalence at the time of reporting ranged from 7% to 42% and the prevalence of GenPs at any time during the course of psoriasis ranged from 33% to 63%. In the two prospective clinical trials, the prevalence of GenPs at the time of enrollment was 35–42%.
Conclusion: A substantial proportion of patients experience genital lesions at some time during the course of psoriasis. Increased awareness of GenPs prevalence may drive improved assessment and treatment.
Introduction
Patients with psoriasis may develop lesions on their genital area (GenPs) during the course of their disease. In the literature, through 2009, estimates of GenPs prevalence based on limited publications ranged from 29% to 46% (Citation1). Patients with GenPs can experience considerable physical and emotional distress. Lesions usually appear as brightly erythematous, thin plaques that frequently lack dry scaling, but may include fissure and can cause pruritus, pain, and burning (Citation1). Patients with GenPs report impaired quality of life and negative impact on sexual health (Citation1,Citation2). Genital psoriasis is not routinely discussed by patients and their health care providers, and physician examinations of psoriasis patients often do not include the genital region (Citation1,Citation3). Increased awareness of GenPs is needed for appropriate diagnosis and treatment.
The objective was to determine the GenPs prevalence based on a broad literature search and in two ongoing randomized phase 3 clinical trials of patients with moderate-to-severe plaque psoriasis. Typically, baseline GenPs in clinical trial populations is not reported. These clinical trials (NCT02561806 [I1F-MC-RHBS; IXORA-S] and NCT02634801 [I1F-EW-RHBZ; IXORA-Z]) (Citation4,Citation5) were included because the presence of GenPs at enrollment was recorded.
Materials and methods
Literature search
A literature search was performed using the following databases and dates: BIOSIS Previews 1989 to 2017 Week 17; Current Contents/All Editions 1998 Week 01 to 2017 Week 13; Embase Classic + Embase 1947 to 2017 March 23; Ovid MEDLINE(R) 1946 to March Week 3 2017; Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations March 23, 2017; Ovid MEDLINE(R) Epub Ahead of Print 23 March 2017, Ovid MEDLINE(R) Versions; PsycINFO 1806 to March Week 3 2017; Google Scholar (accessed 3/24/2017); and Incidence & Prevalence Database (accessed 3/24/2017).
A broad search using both indexing and free-text terms was performed and then focused using limits to titles, abstracts, and indexing. Indexing terms included psoriasis, genital system, genitalia, epidemiology and their narrower terms. Free-text terms included psoriasis, psoriatic, genital*, groin*, hidden psoriasis, concealed psoriasis, vulva*, vulvo*, labia*, clitor*, vestibul*, penis*, penile, testicle*, testicular*, foreskin*, testes, testis, scrotum, scrotal*, erectile, gonad*, epidemiolog*, inciden*, prevalen*, surveillan*, statist*, sampling*, number*, rate or rates, percent*, survey*, and questionnaire*. Terms were limited to major or title or abstract and combined in various ways to focus the results. The search was limited to English-language articles. Articles reporting GenPs prevalence met search criteria and were included. After the search was performed, references that were either listed in bibliographies of other references or found in unrelated searches were added to those found in the search.
Prospective clinical trials
NCT02561806 [I1F-MC-RHBS; IXORA-S] is a phase 3b, multicenter, randomized, double-blinded, double-dummy, parallel-group study comparing ixekizumab to ustekinumab in patients with moderate-to-severe plaque psoriasis who had failure, contraindication, or intolerance to non-biologic systemic treatments (Citation4). NCT02634801 [I1F-EW-RHBZ; IXORA-Z] is a phase 3b, multicenter, randomized, open-label, active-comparator, and parallel-group study with blinded outcomes assessment, examining the effect of treatment with ixekizumab, fumaric acid esters, or methotrexate in patients with moderate-to-severe plaque psoriasis vulgaris who are naïve to systemic therapy (Citation5). The presence of GenPs was determined by an affirmative answer to the following question on the case report form: “Does the patient currently have psoriasis on the genital area?” Genital area included hair-bearing labia majora, labial modified mucous membrane, and perineum in women; and the glans penis, penis shaft, and scrotum in men.
Clinical trials were conducted with the ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines and approved by ethical review boards for each center. Patients provided informed consent. Clinical trials were registered.
Results
Based on the search strategy, 600 articles were reviewed and 75 were deemed of interest. These articles were read by a doctor of philosophy familiar with the subject area; 23 articles were determined to have possibly met the search criteria. These articles were read by two authors (A. P. B. and L. J. K.). Eleven articles were discarded because the GenPs prevalence was not stated or they were reviews. Seven articles that were identified through other means were added. Upon author review, one article was deleted because the study population was duplicated in another article. The final list comprises 18 articles ().
Table 1. Listing of studies from literature search.
Overall, the articles were heterogeneous in reported demographic information including psoriasis type (e.g. plaque, guttate) and severity; sometimes the psoriatic disease characteristics were not reported. Five articles reported results from a single gender () (Citation6–10); of these, three articles reported on men in erectile dysfunction-related studies (Citation6–8) and two articles reported on exclusively female populations (Citation9,Citation10). Only three articles provided specific anatomic descriptions of affected sites within the term “genital “or “genitalia” (Citation2,Citation10,Citation11). The GenPs prevalence was determined by examination in six articles (Citation2,Citation8–12), by patient-reported questionnaire in seven articles (Citation3,Citation6,Citation13–17) and by a combination of medical records and questionnaires in one article (Citation18). Telephone interviews were conducted in one article (Citation19), and in three articles, it could not be determined whether the data were exam-based or self-reported (Citation7,Citation20,Citation21).
Among the six exam-based articles ( ), the prevalence of current (at the time of the exam) GenPs ranged from 12% to 42% (Citation2,Citation8–12). The low end of the range involved a population of Indian (both genders) patients (Citation11). The upper end of the range involved a cohort of sexually active Egyptian women with psoriasis (Citation9). None of the articles mentioned if GenPs was histologically confirmed as psoriasis.
Figure 1. Prevalence of genital psoriasis. Prevalence at time of exam (a); prevalence at time of questionnaire (b), and prevalence at any time during psoriasis course (c) are shown. In three studies, it was unclear whether the reported prevalence was exam-based or self-reported: 18% Alpsoy 2017; 19% Carrera 2017; 27% Cabete 2014. Refer to for study details. F: female; M: male.
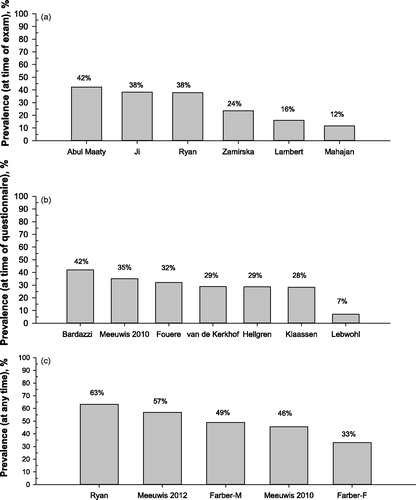
Among patients with psoriasis, the current GenPs prevalence at the time of patient-reporting ranged from 7% to 42% ( ) (Citation3,Citation6,Citation14–16,Citation18,Citation19). The low end of the range was derived from a telephone survey (Citation19) and the high end involved men with and without erectile dysfunction; there was no difference in GenPs prevalence among men with and without erectile dysfunction (Citation6).
The prevalence of GenPs at any time during the course of psoriasis ranged from 33% to 63% (and ) (Citation2,Citation3,Citation13,Citation17). Of these, one article focused on a 277-patient cohort (of 487 respondents with psoriasis [57%]) with GenPs and reported that at the time of questionnaire completion, 62% had current GenPs lesions, and 31% had past GenPs lesions (Citation17).
shows baseline demographics from two prospective randomized phase 3b clinical trials that enrolled patients with moderate-to-severe psoriasis (Citation4,Citation5). At the time of enrollment (randomization), the GenPs prevalence was 35–42%. In both trials, patients with GenPs had higher incidences of scalp and nail psoriasis than patients without GenPs.
Table 2. Baseline characteristics by genital psoriasis status in IXORA-S and IXORA-ZTable Footnotea.
Discussion
There is considerable variation in the prevalence of GenPs as mentioned in the literature: 7–42% at the time of data collection (Citation2,Citation3,Citation6–12,Citation14–16,Citation18–21) and 33–63% at any point during the course of psoriasis (and ) (Citation2,Citation3,Citation13,Citation17). There are likely multiple reasons for this variation, including data collection methodology. The low value (7%) was determined using telephone surveys (Citation19). Respondents may have under-reported GenPs due to embarrassment and privacy concerns: respondents may have worried about discussing their conditions on the telephone with the interviewer, a stranger, who had their phone numbers. Although patients may not have the same anonymity concerns with paper-and computer-based questionnaires, self-reporting is problematic. Patients may mistake genital lesions such as Candida, eczema, vulvar or penile intraepithelial neoplasia, or simple irritation or may believe that their genital lesions are due to other causes, such as sexually transmitted disease, when they are actually psoriasis. Aggregate information obtained from self-reported questionnaires may not reflect the characteristics of the general population with psoriasis because self-selection occurs when patients chose to complete a survey or not. Finally, questionnaire- and phone-based surveys may suffer from a lack of clear definition of GenPs.
Although none of the articles mentioned if histological diagnosis of GenPs was made, prevalence determinations from exam-based studies are likely more accurate than questionnaires, because physicians define and identify GenPs. However, exam-based studies still yielded a wide range of GenPs prevalence ranging from 12% to 42% at the time of examination (Citation2,Citation8–12), perhaps because there was a great deal of heterogeneity across articles in ethnicity, gender (50% of exam-based studies were single-gender), and psoriasis severity, as well as inconsistency in reporting of clinical characteristics and definitions of the genital area. Thus, an overall limitation of this review is substantial between-study heterogeneity. Individual studies may have skewed results towards the low or high spectrums of prevalence due to the severity of GenPs in the study populations.
This work does show that a substantial proportion of patients with psoriasis suffered from genital lesions at any time during the course of their disease, (33–63%) (Citation2,Citation3,Citation13,Citation17) whereas 7–42% of patients had GenPs at the time of data collection (Citation2,Citation3,Citation6–12, Citation14–16,Citation18–21). The proportion of patients with genital lesions at enrollment in IXORA-S and IXORA-Z, which included patients with moderate-to-severe psoriasis, was consistent with numbers reported in the literature. The presence of genital lesions causes substantial physical, personal, and emotional distress. Because a substantial proportion of psoriatic patients experience genital lesions at some time during the course of their disease increased physician awareness is needed so patients can be appropriately treated and educated.
Acknowledgements
The authors thank Kristin Hollister, PhD (Eli Lilly and Company) for assistance with screening the references and Angela Lorio, ELS (Syneos Health) for editorial assistance.
Disclosure statement
Dr Meeuwis has provided consultancy services, has been a speaker, or received honoraria from Eli Lilly and Company and Eucerin, and is on the medical advisory board of Eucerin. Dr van de Kerkhof has provided consultancy services for and/or research/education support from Celgene, Centocor, Allmirall, Amgen, Pfizer, Philips, AbbVie, Eli Lilly and Company, Galderma, Novartis, Jansen Cilag, LEO Pharma, Sandoz, Mitsibishu, and Philips Lighting. Dr. Menter reports consultancy services for and research/educational support from Eli Lilly and Company; otherwise he reports no further personal, commercial, or academic conflict of interests. Drs Potts Bleakman and Dutronc are employees and Eli Lilly and Company own stock. Dr Henneges is an employee of Lilly Deutschland GmbH. Dr Kornberg is an employee of Syneos Health, which is a vendor of Eli Lilly and Company.
Additional information
Funding
References
- Meeuwis KA, de Hullu JA, IntHout J, et al. Genital psoriasis awareness program: physical and psychological care for patients with genital psoriasis. Acta Derm Venerol. 2015;95:211–216.
- Ryan C, Sadlier M, De Vol E, et al. Genital psoriasis is associated with significant impairment in quality of life and sexual functioning. J Am Acad Dermatol. 2015;72:978–983.
- Meeuwis KA, de Hullu JA, de Jager ME, et al. Genital psoriasis: a questionnaire-based survey on a concealed skin disease in the Netherlands. J Eur Acad Dermatol Venereol. 2010;24:1425–1430.
- Reich K, Pinter A, Lacour JP, et al. Comparison of ixekizumab with ustekinumab in moderate-to-severe psoriasis: 24-week results from IXORA-S, a phase III study. Br J Dermatol. 2017;177:1014–1023.
- Clinicaltrials.gov [Internet]. A Study of Ixekizumab (LY2439821) in Participants With Moderate-to-Severe Plaque Psoriasis Naive to Systemic Treatment; [cited 2017 Jul 24]. Available from: https://www.clinicaltrials.gov/ct2/show/NCT02634801
- Bardazzi F, Odorici G, Ferrara F, et al. Sex and the PASI: patients affected by a mild form of psoriasis are more predisposed to have a more severe form of erectile dysfunction. J Eur Acad Dermatol Venereol. 2016;30:1342–1348.
- Cabete J, Torres T, Vilarinho T, et al. Erectile dysfunction in psoriasis patients. Eur J Dermatol. 2014;24:482–486.
- Ji S, Zang Z, Ma H, et al. Erectile dysfunction in patients with plaque psoriasis: the relation of depression and cardiovascular factors. Int J Impot Res. 2016;28:96–100.
- Abul Maaty AS, Gomaa AH, et al. Assessment of female sexual function in patients with psoriasis. J Sex Med. 2013;10:1545–1548.
- Zamirska A, Reich A, Berny-Moreno J, et al. Vulvar pruritus and burning sensation in women with psoriasis. Acta Derm Venereol. 2008;88:132–135.
- Mahajan R, Kumaran MS, Narang T, et al. Genital psoriasis among Indians: a prospective cross-sectional study. Australas J Dermatol. 2015;56:e18–e20.
- Lambert J, Dowlatshahi EA, de la Brassinne, et al. A descriptive study of psoriasis characteristics, severity and impact among 3,269 patients: results of a Belgian cross sectional study (BELPSO). Eur J Dermatol. 2012;22:231–237.
- Farber EM, Nall ML. The natural history of psoriasis in 5,600 patients. Dermatologica. 1974;148:1–18.
- Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19 Suppl 3:2–6.
- Klaassen KM, van de Kerkhof PC, Pasch MC. Nail psoriasis: a questionnaire-based survey. Br J Dermatol. 2013;169:314–319.
- van de Kerkhof PC, de Hoop D, de Korte J, et al. Patient compliance and disease management in the treatment of psoriasis in the Netherlands. Dermatology. 2000;200:292–298.
- Meeuwis KA, van de Kerkhof PC, Massuger LF, et al. Patients' experience of psoriasis in the genital area. Dermatology. 2012;224:271–276.
- Hellgren L. Psoriasis. A statistical, clinical and laboratory investigation of 255 psoriatics and matched healthy controls. Acta Derm Venereol. 1964;44:191–207.
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70:871–881. e1–e30.
- Alpsoy E, Polat M, FettahlioGlu-Karaman B, et al. Internalized stigma in psoriasis: a multicenter study. J Dermatol. 2017;44:885–891.
- Carrera CG, Dapavo P, Malagoli P, et al. PACE study: real-life PASI 100 response with biological agents in moderate-severe psoriasis. J Dermatol Treat. 2017 [Nov 10]; [6 p.]. DOI:10.1080/09546634.2017.1395805
