Abstract
Purpose
Currently, in the treatment of moderate-to-severe psoriasis (PsO) there is a lack of evidence demonstrating optimal biologic treatment response with respect to disease duration. The aim of this post-hoc analysis, using real world data from the Psoriasis Study of Health Outcomes (PSoHO), is to provide evidence if early intervention with biologics is associated with better treatment outcomes and if there is any difference among drug classes or individual biologics.
Materials and methods
For this post-hoc analysis patients were categorised into two subgroups according to shorter (≤2 years) or longer (>2 years) disease duration. Analysis was performed on anti-interleukin (IL)-17A cohort vs other biologics cohort, anti-IL-17A vs other drug classes, and pairwise comparisons of ixekizumab vs individual biologics, provided that the statistical models converged. Analysis investigated the association of disease duration with the proportion of patients achieving 100% improvement in Psoriasis Area Severity Index score (PASI 100) at week 12. Adjusted comparative analyses, reported as odds ratio (OR), were performed using Frequentist Model Averaging (FMA) for each cohort or treatments within each subcategory of the subgroups.
Results
At week 12, anti-IL-17A and other biologics cohorts displayed minimal differences in numerical response rate for PASI 100 with respect to disease duration. The anti-IL-17A cohort showed a higher numerical PASI 100 response rate compared to the other biologic cohort irrespective of disease duration (≤2 years: 36.7% vs 21.8%; >2 years: 35.8% vs 21.9%).
Conclusion
Overall, the results do not clearly indicate that treating patients early is critical in achieving optimal patient outcomes. Furthermore, patients treated with ixekizumab show numerically higher response rates relative to other individual biologics irrespective of disease duration.
Introduction
Over the last number of years, the results of randomized clinical trials have led to the approval of biologics to treat moderate-to-severe psoriasis (PsO). Although biologics have shown superior short- and long-term efficacy and rapid onset of action compared to conventional drugs (Citation1,Citation2), along with significantly greater increase in measures of physical and mental functioning compared to oral therapy (Citation3), they are commonly not prescribed until several years after diagnosis (Citation4). Recent studies have determined that the median disease period before receiving a biologic therapy is 17.1 to 20.5 years (Citation4,Citation5); this delay is arguably a consequence of access to treatment due to socioeconomic factors (Citation6). Additionally, when choosing the optimum treatment for patients with PsO, clinicians need to consider several variables related to the patient, the treatment, and the severity of disease, whereby maximal disease severity rarely presents from the onset (Citation7). Currently, there is a fractured understanding of the natural course of disease and pharmacodynamics, and a lack of evidence showing a significant difference in biologic treatment response with respect to disease duration in patients with PsO. This in turn leads to an absence of clear definitions regarding the most appropriate disease duration cutoffs to be studied. In psoriatic arthritis (PsA), early-stage disease represents <2 years from symptom onset (Citation8,Citation9), with a cutoff of ≤2 years being used to classify shorter disease duration and >2 years used to classify longer disease duration of PsO (Citation10). Therefore, in this analysis, to ensure consistency with other studies performed in PsO, the effects of biologic treatment with respect to disease duration, cutoffs of ≤2 years and >2 years were used. The aim of this post hoc analysis is to provide evidence, if early disease intervention with biologics is associated with better treatment outcomes and if there is a meaningful difference among biologics or drug classes.
Materials and methods
PSoHO is an ongoing 3-year observational cohort study; details of the study including eligibility criteria, clinical characteristics, and all prescribed biologics have been previously published (Citation1,Citation11). For this post-hoc analysis, patients were categorized into two subgroups according to shorter (≤2 years) or longer (>2 years) PsO disease duration. Analysis was performed on anti-interleukin (IL)-17A cohort (ixekizumab [IXE] and secukinumab [SEC]) vs other biologics cohort (brodalumab, guselkumab [GUS], risankizumab [RIS], tildrakizumab, ustekinumab, adalimumab, infliximab, etanercept, and certolizumab), anti-IL-17A versus other drug classes, and pairwise comparisons of IXE vs individual biologics, provided that the statistical models converged. The endpoint of this analysis was the proportion of patients achieving 100% improvement in Psoriasis Area Severity Index score (PASI 100) at week 12. Patients with missing outcomes were imputed as non-responder imputation (NRI). Adjusted comparative analyses, reported as odds ratio (OR), were performed using Frequentist Model Averaging (FMA) for each cohort or treatments within each subcategory of the subgroups, as previously described (Citation1,Citation12,Citation13).
The protocol, amendments, and consent documentation were approved by local institutional review boards (IRB). The study was registered at the European Network of Centers for Pharmacoepidemiology and Pharmacovigilance (ENCEPP24207) and was conducted according to International Conference on Harmonization, Good Clinical Practice guidelines, and the Declaration of Helsinki. All patients were required to give informed consent for participation in the study.
Results
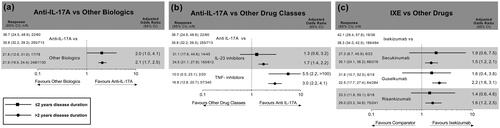
PSoHO enrolled 1981 patients, 7% of patients had a disease duration of ≤2 years. Patient baseline characteristics across the two cohorts stratified by disease duration of ≤2 and >2 years were similar with a few exceptions such as prevalence of patients with PsA, nail PsO and prior exposure to biologics (Table SI and Table SII). At week 12, the anti-IL-17A and other biologics cohort displayed minimal differences in numerical response rate for PASI 100 with respect to disease duration (). The anti-IL-17A cohort showed a higher numerical PASI 100 unadjusted response rate compared to the other biologic cohort irrespective of disease duration (≤2 years: 36.7% vs 21.8%; >2 years: 35.8% vs 21.9%). For >2 years disease duration, the adjusted odds ratio showed a significant difference between the two cohorts (OR 2.1; confidence interval [CI] 1.7, 2.5), with no significant difference being observed for disease duration ≤2 years (). Similarly, irrespective of disease duration, the anti-IL17A cohort had a higher unadjusted response rate compared to IL-23 inhibitors and tumor necrosis factor (TNF) inhibitors (≤2 years: 36.7% vs 31.1% and 10.0%; >2 years: 35.8% vs 24.5% and 16.8% respectively). For a disease duration ≤2, a significantly higher adjusted odds ratio was observed for the anti-IL17A cohort compared to the TNF inhibitor (OR 5.5; 95% CI 2.2, >100) but not the IL-23 inhibitor class (OR 1.3; (5% CI 0.6, 3.2) (). For all individual biologics, a similar unadjusted response rate for PASI 100 was observed in patients with a disease duration of ≤2 and >2 years (). Among these, IXE’s unadjusted response rate (42.1%) was numerically the highest compared to all other individual biologics (SEC 27.3%, GUS 31.6%, and RIS 33.3%) with a disease duration ≤2 years. The adjusted odds ratio were found to be comparable between IXE and all individual biologics at disease duration of ≤2 years with a statistical significance being observed at >2 years disease duration. Similar results were observed for the on-label population (Figure S1).
Figure 1. Actual response rates and adjusted odds ratios of PASI 100, for IXE vs. other drugs, anti-IL-17A vs other drug classes, and anti-IL-17A vs other biologics at week 12 among patients with psoriasis stratified by ≤2 years and >2 years disease duration. Disease duration of ≤2 years is depicted by top/square lines, and >2 years disease duration is depicted by bottom/circle lines. Results are statistically significant if 1 is not covered by the 95% CI. Unadjusted CIs were calculated using the normal approximation.
CI: confidence interval; IL: interleukin; IXE: ixekizumab; NRI: nonresponder imputation; PASI: Psoriasis Area and Severity Index; TNF: tumor necrosis factor. *denotes that lower CI is greater than 1.
Discussion
In this post hoc analysis using data from the real-world PSoHO study, at week 12, similar unadjusted numerical PASI 100 response rates were observed in patients with a shorter (≤2 years) and longer (>2 years) disease duration. However, when interpreting these results, prior treatment with a biologic must be considered, as a population naïve to therapy will demonstrate higher response rates compared to a population of biologic experienced patients (Citation14,Citation15). Indeed, in this analysis, shorter (≤2 years) compared to longer (>2 years) disease duration had a lower percentage of patients previously treated with a biologic, across both cohorts, for all drug classes except TNF inhibitors, and all individual biologics. Additionally, disease severity must be considered too. If two populations have comparable disease severity at baseline but differ in duration of disease, it can be assumed that the population with a shorter disease duration will necessarily experience superior durability of response compared to that with longer disease duration. Overall, our results adjusting for these factors in the comparative analysis suggest that, in general, irrespective of cohort, class, or biologic studied, patients treated with biologics may benefit from treatment regardless of disease duration. However, it is worth noting that secukinumab-treated patients with a shorter disease duration have reported to remain relapse-free after withdrawal for longer periods of time than patients who initiated treatment later (Citation16). Furthermore, it is hypothesized in rheumatology diseases that there is a ‘window of opportunity’ whereby aggressive treatment in the early phase of the disease may lead to longer drug-free remission (Citation17). Therefore, although patients treated with biologics may benefit from treatment regardless of disease duration, increased benefits of early disease intervention may become more apparent after longer follow-up periods.
In accordance with the results for the overall cohort (Citation1), the anti-IL-17A cohort showed the highest unadjusted response rates for both disease duration populations compared to other biologics. Similarly, anti-IL-17A cohort presented the highest unadjusted response rates for both disease duration populations compared to IL-23 inhibitors and TNF inhibitors, with a significantly higher adjusted OR being observed compared to the TNF inhibitors in patients with a disease duration ≤2 years. TNF inhibitors displayed the highest difference in unadjusted response rate (6.8%) between the two disease durations studied, with a more favorable outcome being observed for the longer (>2 years) disease duration.
For individual biologics, the difference in response rates between the disease duration ≤2 years and >2 years was highest for guselkumab (9.1%) and ranged from −2.8% to 4.3% for the other biologics studied. Guselkumab’s higher PASI 100 response rates in patients with a short disease duration has also recently been reported by another study, showing that a significantly higher proportion of guselkumab-treated patients with a short disease duration of ≤2 years achieved a PASI 100 response at week 20 and 28 compared to patients with a disease duration >2 years (Citation10). Interestingly, complete clearance rates of guselkumab in PSoHO at week 12 are still numerically lower than the response rates for IXE and RIS, indicating the faster onset of action and short-term effectiveness of these drugs. More specifically, irrespective of disease duration, patients treated with IXE showed numerically higher response rates relative to other individual biologics. The PSoHO results presented here should be interpreted in the context of the study design and its recently published primary data (1).
Limitations in this study include the relatively low patient population, particularly for the ≤2 years disease duration subgroup, (19/138 patients received prior treatment with a biologic). For this disease duration subgroup, cohorts with low response rates resulted in less precision of the odds ratio estimates. For these cases, sensitivity analyses were performed. Statistical analyses and strategies were prespecified in the protocol, and pairwise comparisons of individual treatment effectiveness were only completed relative to IXE. Furthermore, at baseline, differences were observed among cohorts with anti-IL-17A cohort displaying a lower rate of prior biologic treatments (8.3%) compared to other biologics (18.0%) and a higher rate of PsA and nail PsO (21.7% vs 7.7% and 36.7% vs 26.0%, respectively). Furthermore, this study investigates treatment outcomes at week 12, longer term follow-up studies could provide further evidence if early disease interventions result in increased patient benefits. However, a strength of this study is the use of the machine learning FMA statistical methodology as it mitigates some typical limitations of observational trials, including confounding that can result in selection and other forms of bias.
Taken together, our results do not clearly indicate that treating patients early (i.e. within the first 2 years of establishing the diagnosis) is critical in achieving optimal patient outcomes. Overall, it was found that patients treated with IXE showed numerically higher response rates relative to other individual biologics irrespective of disease duration. Long-term follow-up data are necessary to understand if treating patients with biologics early has any significant benefit.
Supplemental Material
Download MS Word (133.2 KB)Acknowledgments
Medical writing assistance was provided by Caroline Murphy, PhD, of Eli Lilly and Company.
Disclosure statement
The following authors have served as an investigator, scientific officer, speaker, advisor, received research grants, participated in steering committees and/or received honoraria: AP: AbbVie, Almirall Hermal GmbH, Amgen, Biogen Idec, BMS, BioNTech, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Galderma, GlaxoSmithKline, Hexal, Janssen, LEO Pharma, MC2 Therapeutics, Medac, Merck (MSD), Merck Serono, Mitsubishi Tanabe Pharma Corporation, Novartis, Pascoe, Pfizer, Regeneron, Roche, Sandoz Biopharmaceuticals, Sanofi Aventis/Genzyme, Schering Plough, Tigercat Pharma, UCB and Eva Pharma; KE: AbbVie, Almirall, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly and Company, Galderma, Incyte, Janssen, LEO Pharma, Novartis, Pfizer, Sanofi, and UCB; AC: AbbVie, Almirall, Biogen, Eli Lilly and Company, LEO Pharma, Janssen, Novartis, Pfizer, Sanofi Aventis/Genzyme, and UCB; J-TM: AbbVie, Almirall, Amgen, B.M.S., Celgene, Eli Lilly and Company, Incyte, LEO Pharma, Janssen-Cilag, MSD, Novartis, Pfizer, Pierre Fabre, Roche, Sanofi, and UCB; KAP: AbbVie, Acelyrin, Akros Pharma Inc., Amgen, Anacor Pharmaceuticals, Aralez Pharmaceuticals, Arcutis Biotherapeutics, Avillion, Bausch Health/Valeant, Boehringer Ingelheim, Bristol-Myers Squibb, Can-Fite BioPharma, Celgene, Celltrion, Coherus BioSciences, CorEvitas, Dermavant Sciences, Dermira, DICE Therapeutics, Dow Pharma, Eli Lilly and Company, Evelo Biosciences, Forbion, Galderma, Gilead Sciences, GlaxoSmithKline, Incyte, Janssen, Kyowa Hakko Kirin, LEO Pharma, Meiji Seika Pharma, Merck (MSD), Mitsubishi Tanabe Pharma Corporation, Novartis, Pfizer, Regeneron, Reistone, Roche, Sanofi-Aventis/Genzyme, Sandoz, Sun Pharma, Takeda, UCB, vTv Therapeutics and Xencor; AG, CS, AL, and KF: are employees and stockholders of Eli Lilly and Company; and CM: is a contractor of HaaPACS GmbH and provides statistical services for Eli Lilly, and is a stockholder of Eli Lilly.
Additional information
Funding
References
- Pinter A, Puig L, Schäkel K, et al. Comparative effectiveness of biologics in clinical practice: week 12 primary outcomes from an international observational psoriasis study of health outcomes (PSoHO). J Eur Acad Dermatol Venereol. 2022;36(11):1–5. doi: 10.1111/jdv.18376.
- Reich K, Augustin M, Thaçi D, et al. A 24-week multicentre, randomized, open-label, parallel-group study comparing the efficacy and safety of ixekizumab vs. fumaric acid esters and methotrexate in patients with moderate-to-severe plaque psoriasis naive to systemic treatment. Br J Dermatol. 2020;182(4):869–879. doi: 10.1111/bjd.18384.
- Salame N, Ehsani-Chimeh N, Armstrong AW. Comparison of physical and mental functioning among moderate-to-severe psoriasis patients on biologic versus oral therapy. Arch Dermatol Res. 2019;311(6):453–460. doi: 10.1007/s00403-019-01918-9.
- van den Reek JMPA, Seyger MMB, van Lümig PPM, et al. The journey of adult psoriasis patients towards biologics: past and present-results from the BioCAPTURE registry. J Eur Acad Dermatol Venereol. 2018;32(4):615–623. doi: 10.1111/jdv.14684.
- Seneschal J, Lacour J-P, Bewley A, et al. A multinational, prospective, observational study to estimate complete skin clearance in patients with moderate-to-severe plaque PSOriasis treated with BIOlogics in a REAL world setting (PSO-BIO-REAL). J Eur Acad Dermatol Venereol. 2020;34(11):2566–2573. doi: 10.1111/jdv.16568.
- Scala E, Megna M, Amerio P, et al. Patients’ demographic and socioeconomic characteristics influence the therapeutic decision-making process in psoriasis. PLoS One. 2020;15(8):e0237267. doi: 10.1371/journal.pone.0237267.
- Maurelli M, Gisondi P, Girolomoni G. Tailored biological treatment for patients with moderate-to-severe psoriasis. Expert Rev Clin Immunol. 2023;19(1):37–43. doi: 10.1080/1744666X.2023.2141226.
- Anandarajah A. Imaging in psoriatic arthritis. Clin Rev Allergy Immunol. 2013;44(2):157–165. doi: 10.1007/s12016-012-8304-4.
- Gladman DD, Thavaneswaran A, Chandran V, et al. Do patients with psoriatic arthritis who present early fare better than those presenting later in the disease? Ann Rheum Dis. 2011;70(12):2152–2154. doi: 10.1136/ard.2011.150938.
- Schäkel K, Reich K, Asadullah K, et al. Early disease intervention with guselkumab in psoriasis leads to a higher rate of stable complete skin clearance (‘clinical super response’): week 28 results from the ongoing phase IIIb randomized, double-blind, parallel-group, GUIDE study. J Eur Acad Dermatol Venereol. 2023;37(10):2016–2027. doi: 10.1111/jdv.19236.
- Lynde C, Riedl E, Maul J-T, et al. Comparative effectiveness of biologics across subgroups of patients with moderate-to-Severe plaque psoriasis: results at week 12 from the PSoHO study in a Real-World setting. Adv Ther. 2023;40(3):869–886. doi: 10.1007/s12325-022-02379-9.
- Zagar A, Kadziola Z, Lipkovich I, et al. Evaluating bias control strategies in observational studies using frequentist model averaging. J Biopharm Stat. 2022;32(2):247–276. doi: 10.1080/10543406.2021.1998095.
- Hjort NL, Claeskens G. Frequentist model average estimators. J Am Stat Assoc. 2003;98(464):879–899. doi: 10.1198/016214503000000828.
- van Lümig PPM, van de Kerkhof PCM, Boezeman JBM, et al. Adalimumab therapy for psoriasis in real-world practice: efficacy, safety and results in biologic-naïve vs. non-naïve patients. J Eur Acad Dermatol Venereol. 2013;27(5):593–600. doi: 10.1111/j.1468-3083.2012.04496.x.
- Torres T, Puig L, Vender R, et al. Drug survival of IL-12/23, IL-17 and IL-23 inhibitors for psoriasis treatment: a retrospective multi-country, multicentric cohort study. Am J Clin Dermatol. 2021;22(4):567–579. doi: 10.1007/s40257-021-00598-4.
- Lebwohl M, Iversen L, Eidsmo L, et al. Investigation of plaque psoriasis relapse after secukinumab withdrawal in patients from two phase III studies. Clin Exp Dermatol. 2023. doi: 10.1093/ced/llad329.
- Nagy G, van Vollenhoven RF. Sustained biologic-free and drug-free remission in rheumatoid arthritis, where are we now? Arthritis Res Ther. 2015;17(1):181. doi: 10.1186/s13075-015-0707-1.
