Abstract
Purpose: There is limited information about the diagnosis and treatment of hidradenitis suppurativa (HS) in the Kingdom of Saudi Arabia (KSA). This Delphi consensus study was conducted to develop recommendations for the management of HS in the KSA.Methods: The expert panel including 12 dermatologists with extensive experience treating HS patients provided nine consensus statements and recommendations on diagnosis and assessment, management, comorbidities and multidisciplinary approach, and education. The experts also developed clinical questions pertaining to the management of HS and rolled out as a survey to 119 dermatologists practising in the KSA.Results: The topics covered included: referring physicians’ awareness of HS; referral criteria for HS; definition of moderate-to-severe HS; treatment goals; definition of treatment success; treatment and biologic initiation; comorbidities and multidisciplinary approach; patient education and awareness of HS. Full consensus (100%) from the expert dermatologists was received on all the topics except referring physicians’ awareness of HS, definition of treatment success, and treatment and biologic initiation. The survey results resonated with the expert opinion.Conclusion: As HS is a chronic disease with negative impact on quality-of-life, timely diagnosis and treatment, early identification of comorbid conditions and a multidisciplinary care approach are crucial for effective management of HS.
Introduction
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic, recurrent debilitating skin disease that mainly affects areas rich in apocrine glands, such as the axillae, groin, and anogenital region (Citation1, Citation2). It is characterized by painful, inflammatory lesions ranging from nodules and painful abscesses to severe forms such as scarring and fistulas (Citation1, Citation3). Data on the prevalence of HS are scarce. Moreover, it is difficult to get accurate estimates on the number of people living with HS, mainly because of misdiagnosis, underdiagnosis, or delayed diagnosis (Citation4). A systematic review and meta-analysis of 16 studies from the Asia-Pacific region, the US, Europe, and South America reported an overall prevalence of HS of 0.4% (Citation5).
HS imposes a substantial burden on patients by negatively impacting their quality of life (QoL) and psychological well-being, which may lead to depression and anxiety (Citation2, Citation6, Citation7). The literature suggests that increased disease severity results in poor QoL outcomes – this emphasizes the importance of appropriate assessment tools for measuring disease severity and QoL (Citation6). Different tools or scoring systems are available to classify patients with HS based on their severity, a few of which include the Hurley staging system, the HS Clinical Response (HiSCR) score, the Sartorius score and the modified Sartorius score, the Physician Global Assessment (PGA), the Hidradenitis Suppurativa Severity Index (HSSI) and Severity Assessment of Hidradenitis Suppurativa (SAHS) score (Citation8–13). The Dermatology Life Quality Index (DLQI) is the most commonly used outcome measure to assess QoL, and the Visual Analogue Scale (VAS) is used to measure pain (Citation8).
Treatment of HS should aim to manage disease symptoms (minimize pain and drainage), treat existing lesions, decrease recurrence, and prevent disease progression and the need for surgery (Citation2, Citation14–17). Smoking and weight gain are linked with increased HS severity. Thus, in addition to pharmacotherapy, lifestyle interventions such as smoking cessation and weight loss should be encouraged for effective management of the condition (Citation18). The various treatment options for HS include topical and systemic medications, biologics, and surgical interventions (Citation2, Citation17, Citation18). Topical therapies are recommended for mild cases, whereas systemic therapies, particularly antibiotics, are preferred for moderate-to-severe disease (Citation2, Citation17, Citation18). Many guidelines recommend treatment with biologics for patients with moderate-to-severe HS who do not respond to systemic antibiotics (Citation17, Citation18). Surgery is mostly recommended for patients with HS who have widespread lesions, for those with recurrent abscesses and for advanced cases with irreversible damage such as fistulas and scars (Citation1, Citation2, Citation17–19). Also, as HS is associated with various comorbidities such as cardiovascular diseases, diabetes mellitus, metabolic syndrome, autoimmune conditions (especially inflammatory bowel disease and inflammatory arthropathies), polycystic ovary syndrome, depression, and anxiety, a multidisciplinary approach with the involvement of dermatologists, surgeons, gynecologists, psychiatrists, and other specialists, as needed, should be employed for the management of HS (Citation17, Citation18, Citation20).
In Riyadh, Saudi Arabia, the prevalence of HS is estimated at 1.29% (Citation3). This study reported a higher prevalence of HS in males compared with females (Citation3), in contrast to data from other studies reporting an increased prevalence in females (Citation21, Citation22) – this may be attributed to sample bias. Data on the diagnosis and treatment of HS in the Kingdom of Saudi Arabia (KSA) are limited, and hence there is a need to raise awareness about the disease. A Delphi consensus was conducted to develop a set of recommendations for the diagnosis and management of HS in the KSA.
Methods
A three-round Delphi consensus study was conducted, in which an expert panel of 12 dermatologists with extensive experience treating patients with HS considered scientific evidence and expert opinions to develop useful guidance for the diagnosis and management of HS in the KSA. Of the 12 dermatologists 09 are HS specialized practicing in the KSA. During Round 1, the expert panel agreed on the consensus scope, drafted the consensus statements, and reviewed the survey instrument and questionnaire. During Round 2, the experts voted on consensus statements and provided their final comments. In addition, a survey comprising 17 questions on the management of HS was distributed to a wide range of dermatologists practising in the KSA to understand their perceptions and actual practice and identify similarities and gaps between dermatologists’ insights and experts’ opinions. These questions addressed the following:
Referring physician awareness of HS
Referral criteria for HS
Definition of moderate-to-severe HS
Treatment goals
Definition of treatment success
Treatment and biologic initiation
Comorbidities and multidisciplinary approach
Patient education and awareness of HS
A consensus of agreement was considered achieved if at least 70% of dermatologists agreed on a particular statement. If at least 80% of the dermatologists agreed, it was considered a strong agreement.
The study was approved by Institutional Review Board (IRB).
Results
The expert panel arrived at nine consensus statements and recommendations that were categorized into four groups: diagnosis and assessment; management; comorbidities and multidisciplinary approach; and education (). A total of 119 dermatologists from the KSA responded to the survey. The participants had an average experience of about 12 years. About three-fourths of the dermatologists (73%) practiced in private hospitals or clinics and treated an average of about ten patients with HS per month.
Table 1. Nine consensus statements and recommendations generated during the expert discussion, and the level of agreement from the experts.
Diagnosis and assessment
Statement 1 – Referring physician awareness of HS: Patients with HS experience a significant delay from disease onset to diagnosis. This is often due to low awareness among non-dermatology clinicians, leading to misdiagnosis and delayed referrals.
About 92% of the experts (n = 11) strongly agreed with this statement. The survey indicated that the dermatologists were involved in the direct diagnosis of HS in about 66% of patients; about 14% of patients who were undiagnosed were referred to a dermatologist by another physician. There is an average delay of about eight years between the onset of HS symptoms and the diagnosis of HS. Considering the challenges affecting the diagnosis of HS, about 77% of the dermatologists found it challenging (rating 4) or very challenging (rating 5) to diagnose HS due to a lack of knowledge about the disease among the population, whereas 57% of the dermatologists found it challenging/very challenging due to a lack of knowledge about the disease among non-dermatologists or due to cultural barriers (e.g., women are hesitant to discuss and/or refuse examination of sensitive areas) ().
Figure 1. Challenges affecting time to diagnosis and management of hidradenitis suppurativa*.
*More than one response are possible.

Statement 2 – Referral criteria: Referral criteria should be followed in the presence of a typical history and clinical findings: patients suffering from recurrent abscesses, drainage, or nodules should be referred directly to a dermatologist (2 or more recurrences in 6 months).
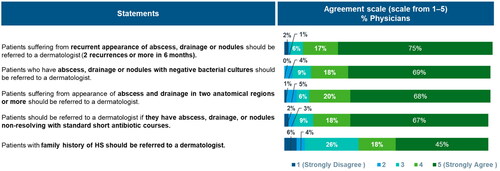
There was complete agreement among the expert panel about the criteria for referral to dermatologists. The survey results resonated with the experts’ opinions − 75% of the dermatologists strongly agreed (rating 5) and 17% of the dermatologists agreed (rating 4) that patients suffering from recurrent abscesses, drainage, or nodules should be referred by a non-dermatologist to a dermatologist (2 or more recurrences in 6 months). About 87% of the dermatologists opined (69% strongly agreed; 18% agreed) that patients who have abscesses, drainage, or nodules with negative bacterial culturesFootnote1 should be referred to a dermatologist, and about 88% opined (68% strongly agreed; 20% agreed) that patients with abscesses and drainage in two or more anatomical regions should be referred to a dermatologist ().
Figure 2. Criteria for referral of patients with hidradenitis suppurativa to dermatologists*.
*More than one response are possible.
Statement 3 – Definition of moderate-to-severe HS: Hurley staging is a widely used grading system for assessing HS disease severity. It can be used as a standard tool to characterize the extent of disease in patients with HS, where mild HS is defined as Hurley Stage 1, moderate HS as Hurley Stage 2, and severe HS as Hurley Stage 3.
All the experts on the panel strongly agreed that Hurley staging is widely used for assessing HS disease severity. The survey indicated that about 65% of the dermatologists followed Hurley staging as the most common assessment tool for classifying patients with HS. Other assessment tools or scoring and severity indexes used by dermatologists in the KSA include HSSI (28%) and HiSCR (24%) (). According to the surveyed dermatologists, about 35%, 40%, and 25% of patients with HS in the KSA were classified as Hurley Stages I, II, and III, respectively.
Table 2. Commonly used assessment tools assessment tools’/’scoring and severity indexes’, do you follow to assess or classify your HS patients.
Management
Statement 4 – Treatment goals: Overall treatment goals should include the following:
Relieving skin pain
Improving patients’ QoL
Improving physical signs (≥50% improvement in inflammatory lesion counts [nodules and abscesses])
Controlling disease progression (no increase in new abscesses or draining fistulas compared with baseline)
Improvement in PGA
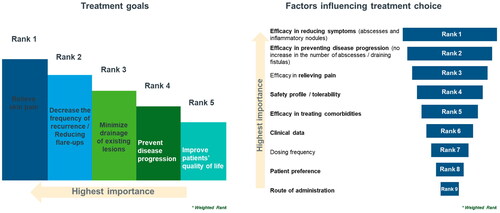
There was a clear consensus among the panel that the overall treatment goals should include the outcomes mentioned in the above statement. During the survey, the dermatologists were asked to rank the importance of the following treatment goals on a scale of 1 (not at all important) to 5 (extremely important): relieving skin pain; minimize drainage of existing lesions; decreasing the frequency of recurrence; preventing disease progression and improving patients’ QoL. Based on the rating, relieving skin pain was the most important goal, followed by decreasing the frequency of recurrences or reducing flare-ups. Similarly, regarding the factors influencing treatment choice, efficacy in reducing symptoms (abscesses and inflammatory nodules) was considered the most important attribute, and efficacy in preventing disease progression (no increase in the number of abscesses/draining fistulas) was the second most important attribute ().
Statement 5 – Definition of treatment success: Near Complete response should be defined as ≥50% improvement in inflammatory lesion counts (nodules and abscesses) and no increase in new abscesses or draining fistulas compared with baseline, as well as an improvement in the DLQI <5.
There was strong agreement among the panel (92%) about the definition of complete response. However, according to the survey, about 91% of the dermatologists felt treatment response should be defined as ≥50% improvement in inflammatory lesion counts (nodules and abscesses) and no increase in new abscesses or draining fistulas compared with baseline, and only 6% of the dermatologists defined treatment response as improvement in DLQI <5. The other 3% defined treatment response as pain VAS 0 or 1.
Statement 6 – Treatment and biologic initiation: Biologics should be used for moderate-to-severe HS after the failure of systemic antibiotics for 12 weeks to reduce disease severity and improve patients’ QoL.
Of the 12 dermatologists on the expert panel, 10 (83%) strongly agreed that patients with moderate-to-severe HS who failed treatment with systemic antibiotics for 12 weeks should be given biologics. According to the survey, topical treatment, systemic antibiotics, and lifestyle modifications were the most received interventions in patients with mild HS, as well as in patients with moderate-to-severe HS. About 42% of patients with mild HS receive topical treatment, 37% receive systemic antibiotics, and 35% follow lifestyle modifications. About 43% of patients with moderate-to-severe HS receive systemic antibiotics, whereas 34% of patients receive lifestyle modifications and topical treatments respectively. The proportion of patients receiving an approved biologic, adalimumab/biosimilar differed based on disease severity. Only 6% of patients with mild HS receive adalimumab/biosimilar, whereas about 19% of patients with moderate-to-severe HS receive adalimumab/biosimilar.
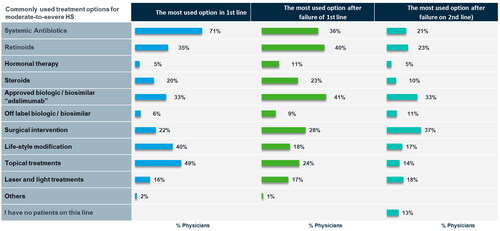
The most commonly used treatment options for moderate-to-severe HS varied depending on whether the patients were treatment naïve or had received any previous therapies (). For treatment-naïve patients, about 71% of the dermatologists preferred treatment with systemic antibiotics and 49% preferred topical treatments. About 33%, 41%, and 33% of the dermatologists preferred adalimumab/biosimilar in treatment-naïve patients, patients who failed first-line therapy, and those who failed second-line therapy, respectively. Surgical intervention was considered by 37% of the dermatologists in patients who failed second-line therapy.
Comorbidities and a multidisciplinary approach
Statement 7 – Comorbidities and multidisciplinary approach: HS is associated with multiple comorbidities such as metabolic syndrome, sexual dysfunction, axial spondyloarthritis, inflammatory bowel disease, depression, polycystic ovary syndrome, and anxiety. Appropriate screening should be implemented for early identification of comorbidities; this also should be considered while designing treatment strategies and assessing treatment outcomes.
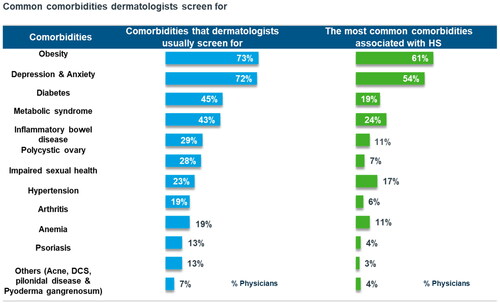
All the experts strongly agreed with the consensus statement on comorbidity screening. The survey results demonstrated that obesity and depression/anxiety were the most common comorbidities that the dermatologists usually screen for (as per 73% and 72% of the dermatologists, respectively) and also the most common comorbidities associated with HS (as per 61% and 54% of the dermatologists, respectively). Diabetes and metabolic syndrome were other comorbidities that dermatologists usually screened for and that were usually associated with HS ().
Figure 5. Common comorbidities dermatologists screen for and most common comorbidities associated with hidradenitis suppurativa.
Statement 8 – Comorbidities and multidisciplinary approach: Effective interventions are needed to address the challenges of collaborating with/referring patients with HS to experienced surgeons in the area.
There was full consensus among the panel with the above statement. Three challenges affecting the quality of surgical care offered to patients with HS were identified for the survey, and the dermatologists were asked to rank each of these challenges on a scale of 1 (not at all challenging) to 5 (extremely challenging). Lack of experienced surgeons in the area was considered the most challenging, followed by experienced surgeons not interested in managing patients with HS; about 68% and 64% of the dermatologists, respectively, ranked them as 3 or above. Difficulty in referring patients with HS to surgeons was considered the least challenging, with 57% of the dermatologists ranking it as 3 or above.
Education
Statement 9: Patient education and awareness of HS: There is a gap in patient education and awareness of HS; therefore, more time should be allocated to providing education to patients with HS and their circle of care to improve patient understanding and treatment adherence.
All the physicians on the expert panel strongly agreed that more time should be allocated for educating patients about the disease to improve patient understanding and treatment adherence. However, according to the survey, about three-fourths of the dermatologists (76%) believed that the time allocated for patients with HS was enough, whereas about one-fourth (24%) of the dermatologists felt more time should be allocated. Moreover, 38% of the dermatologists working in public hospitals believed the time allocated for patients with HS was not enough, while only 20% of those working in private hospitals believed the same.
Discussion
This Delphi study was conducted to generate consensus statements to highlight the unmet needs for HS, identify referral criteria and treatment goals in KSA. Nine consensus statements were formulated and agreed upon by the dermatologists.
One of the important aspects highlighted during the consensus meeting was the substantial delay between disease onset and diagnosis (Citation3). The Canadian Dermatology Association and the Swiss Practice recommendations emphasize the importance of early diagnosis and effective treatment of HS to reduce the disease burden on both patients and caregivers (Citation15, Citation17). Despite guidelines outlining the importance of early diagnosis, the survey results reported that there is an average delay of about eight years between symptom onset and diagnosis. This is also supported by the literature, which demonstrates a mean diagnostic delay of 7.2 ± 8.7 years for HS compared to 1.6 ± 4.8 years for psoriasis (Citation23). The average delay in consulting a physician was found to be 2.5 ± 5.0 years for patients with HS, compared with 1.0 ± 4.3 years for patients with psoriasis (Citation23). The results of the Global Survey of Impact and Healthcare Needs (VOICE) Project showed a mean diagnostic delay of 10.2 ± 8.9 years (Citation24). Moreover, patients with HS usually visit more physicians before being formally diagnosed, compared with patients with other dermatological conditions such as psoriasis (Citation24). The results from the VOICE project showed that 63.7% (n = 827) of patients visited a physician ≥5 times before receiving a confirmed HS diagnosis (Citation24). Thus, delayed diagnosis was identified as a global feature of HS compared with other conditions, and a few reasons for the same could be patient delay in visiting a physician, or the physician consulted not making the right diagnosis, or both (Citation23).
Early referral of patients with HS to dermatologists could improve outcomes; however, there is only limited evidence on the referral criteria, even from the guidelines, that should be followed by non-dermatologists. The British Association of Dermatologists guidelines recommend referral to dermatology secondary care in the context of inadequate response to initial management or if HS is severe (Hurley Stage III) at initial presentation (Citation16, Citation25). A cross-sectional survey of UK general practitioners reported the factors influencing referral decisions from primary to secondary care, including: (i) the severity of disease; (ii) previous treatment by a speciality (which would impact re-referral to that speciality); (iii) HS affecting a specific body site; (iv) availability of agreed-upon local patient pathways for patients with HS; and (v) the presence of a local physician with special interest in treating patients with HS (Citation26). Overall, there is a need for developing criteria to guide non-dermatologists to refer patients with HS to dermatologists on time (Citation24, Citation27). In line with this unmet need, there was strong agreement among the panel as well as the surveyed dermatologists that proper referral criteria should be followed for early diagnosis. The criteria must emphasize that patients with recurrent abscesses, drainage, or nodules be referred by a non-dermatologist to a dermatologist (2 or more recurrences in 6 months). The interviewed dermatologists also strongly agreed (67%) that patients should be referred to a dermatologist directly if they have non-resolving skin lesions, despite receiving standard, short antibiotic courses.
The Hurley staging system is universally recommended across most guidelines as a tool for classifying the severity of HS (Citation2, Citation16, Citation17). All the experts strongly agreed with this recommendation. About two-thirds of the surveyed dermatologists also indicated that they followed Hurley staging to determine HS severity. In addition to Hurley staging, the European S1 guidelines and the Swiss practice recommendations discuss the Sartorius score as an alternative grading system for HS (Citation2, Citation15). Some of the other assessment tools or scoring and severity indexes used by the dermatologists included HSSI, HiSCR, DLQI patient reported outcomes, SAHS score and HS-PGA.
Different treatment goals for HS have been described in different guidelines. For instance, the North American clinical management guidelines suggest that the goal should be to minimize scarring, progression, and the need for surgery (Citation28). The British Association of Dermatologists guidelines list QoL, seriousness of adverse effects, pain, disease-specific physician score, physician’s global assessment (PGA), and adverse event nuisance as goals for medical interventions, among which the first three outcomes are critical for patient decision-making. Similarly, QoL, recurrence rates, overall satisfaction, functional (arm abduction), complication rates, cosmetic, the duration of hospitalization, and total patient downtime are the goals for surgical intervention, with the first five outcomes being considered critical for patient decision-making (Citation16). During the consensus meeting, the experts strongly agreed that relieving pain; improving patients’ QoL, PGA, and physical signs; and controlling disease progression should be the treatment goals. The survey also revealed that the dermatologists consider relieving skin pain the most important goal, followed by decreasing the frequency of recurrences or reducing flare-ups. The most important factors influencing treatment choices among the dermatologists included efficacy in reducing symptoms, preventing disease progression, and relieving pain.
The literature does not provide any clear agreed-upon definitions for treatment success in HS yet; however, most guidelines list common tools for outcome measures. Most guidelines or consensus documents, including the HS ALLIANCE recommendations, North American clinical management guidelines, Canadian consensus, European HS Foundation, and Brazilian guidelines, recommend HiSCR (≥50% reduction in inflammatory lesion counts and no increase in abscesses or draining fistulas compared with baseline) for assessment of HS treatment response (Citation28–32). The HS ALLIANCE recommendations, European S1 guidelines, and North American clinical management guidelines also recommend the inclusion of pain VAS and DLQI as treatment outcome measures, as they provide valuable insights about treatment response (Citation2, Citation28, Citation32). Despite the increasing importance of pain and QoL as treatment outcome measures, 91% of the surveyed dermatologists defined treatment response based on HiSCR, whereas only 6% and 3% considered an improvement in DLQI <5 and pain VAS 0 or 1 as treatment response, respectively.
Guidelines recommend treatment with biologics in patients with moderate-to-severe HS who have not responded to conventional therapy (Citation2, Citation17, Citation28, Citation32). The North American clinical management guidelines recommend treatment with adalimumab and infliximab for patients with moderate-to-severe HS; however, dose-ranging studies with infliximab are necessary to determine the optimal dose (Citation28). The European S1 guidelines highlight that biologics (adalimumab and infliximab) are effective in patients with moderate-to-severe HS and improve QoL (Citation2). The Canadian guidelines recommend adalimumab as first-line therapy, infliximab as second-line therapy, and ustekinumab and anakinra as third-line therapy in patients with moderate-to-severe HS (Citation17). Other biologics that have shown efficacy in moderate-to-severe HS include secukinumab, brodalumab, and bimekizumab (Citation17). Secukinumab has received approval from the European Commission for the treatment of moderate-to-severe HS following inadequate response to conventional systemic HS therapy (Citation33). In line with the evidence from all the above guidelines and recommendations, the expert panel agreed that biologics should be used in moderate-to-severe HS following treatment failure with systemic antibiotics for 12 weeks. The survey revealed that systemic antibiotics (43% of patients) were the most commonly received treatment in patients with moderate-to-severe HS; of note, 19% of patients received adalimumab/biosimilar. About 33% of the dermatologists considered adalimumab/biosimilar as the preferred first-line treatment option for moderate-to-severe HS; 41% of the dermatologists considered it after the failure of first-line treatment, and 33% after the failure of second-line treatment.
In patients with severe HS or those with recurring lesions or those with irreversible damage such as fistulas and scars, surgery is the preferred option to decrease morbidity (Citation2, Citation29, Citation34). Patients were also positive overall about the surgical management of HS (Citation34). However, according to the survey, dermatologists face certain challenges related to collaborating with surgeons, of which lack of experienced surgeons in the area was the greatest challenge, followed by experienced surgeons not interested in managing patients with HS and difficulty in referring patients with HS to surgeons. The literature also suggests that patients with HS have reduced access to surgery due to various reasons, such as a lack of surgeons experienced in treating HS and limited number of providers and patients traveling to a different area for surgery (Citation35, Citation36). To overcome this, effective interventions are needed to address the challenges of collaborating with or referring patients with HS to experienced surgeons in the area. Furthermore, educating dermatologist about minor surgical procedures for HS such as deroofing and excision, and providing appropriate training are essential for improving the care of HS patients – this is also important for improved patient outcomes and QoL. HS is associated with several comorbidities, and appropriate screening methods should be implemented for the early identification of concomitant and secondary diseases (Citation16–18). As per the survey, obesity, followed by depression and anxiety, are the most common comorbidities dermatologists usually screen for and also the most commonly observed comorbidities in practice. Moreover, there is a gap in patient education and awareness about HS. Based on the results of a recently published qualitative interview study involving patients with HS and physicians experienced in treating patients with HS, low disease awareness was ranked as one of the most frequently reported unmet needs by patients with HS, in addition to treatment-related issues (Citation37). In light of this, guidelines highlight the importance of close communication between patients and dermatologists, as well as between dermatologists and other healthcare providers specializing in mental health, pain management, and surgery, with an emphasis on a multidisciplinary approach for the treatment of HS. This involves patient education, regular communication between physicians, and the assessment of comorbid conditions. To accomplish this, it is important to establish clarity on the responsibilities of each of the specialists involved in multidisciplinary care, and effective strategies should be devised for patients, so that they can visit the relevant healthcare professional at the right time (Citation29). Also, more time should be allocated by the physician to provide education to patients with HS and their caregivers, to improve patient understanding and treatment outcomes.
Conclusions
HS is a complex disease with a profound impact on QoL and requires early diagnosis and appropriate treatment initiation for effective management. It is important to raise awareness about the disease among physicians as well as patients to avoid the delay from symptom onset to diagnosis. Also, to facilitate the timely diagnosis of HS and improve patient outcomes, proper referral criteria should be framed. There should be standard assessment tools to assess disease severity and measure treatment success. Treatment goals should encompass improvements in clinical outcomes as well as QoL. Biologics should be considered for treating patients with moderate-to-severe HS who are not responding to first-line conventional systemic treatments, in line with the recommendations from guidelines. Emphasis must also be laid on the early identification of comorbid conditions to facilitate referrals and establish a multidisciplinary care team for HS.
Authors’ contributions
ME conceptualized the project and provided supervision. ME assessed the methodology jointly with the rest of the authors. All authors drafted the Adelphi research question and made substantive revision and critically read, revised, and approved the final manuscript.
Acknowledgments
The authors thank Novartis Saudi for funding medical writing/editorial support in accordance with latest Good Publication Practices guidelines.
Disclosure statement
Yousef Binamer has participated in the advisory boards or speakers’ bureau for AbbVie, Sanofi, Novartis, Janssen, Kyowa Kirin, Eli Lilly, Amgen, Therakos, NewBridge, LEO, and in the research or clinical trials for BioGen and AbbVie. He also received speaker or consulting fees for AbbVie, Sanofi, Novartis, Janssen, Kyowa Kirin, NewBridge. Falk G. Bechara has received honoraria for participation in advisory boards, in clinical trials, and/or as a speaker for AbbVie Inc., AbbVie Deutschland GmbH & Co. KG, Boehringer Ingelheim Pharma GmbH & Co. KG, Incyte Corporation, Moonlake Immunotherapeutics, Novartis Pharma GmbH, Celltrion, Mölnlycke, UCB Pharma, and Janssen-Cilag GmbH. Maysa T. Eshmawi, Hajer Almudaiheem, Mohamed Fatani, Mohamed Alajlan, Ruaa Alharithy, Hind Alotaibi, Hind Almohanna, Adel Santli, Abdulaziz Madani, Nadya Alfaraidy, and Ahmed Aljedai have nothing to disclose.
Additional information
Funding
Notes
1 it should be noted that a positive bacterial culture is possible and common in patients with HS. This does not exclude the diagnosis of HS.
References
- Rathod U, Prasad PN, Patel BM, et al. Hidradenitis suppurativa: a literature review comparing current therapeutic modalities. Cureus. 2023;15(8):1. doi:10.7759/cureus.43695.
- Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619–9. doi:10.1111/jdv.12966.
- Alsadhan H, Alfawzan AI, Yaqoub A, et al. Hidradenitis suppurativa: estimated prevalence, clinical features, and risk factors in Riyadh, Saudi Arabia. Cureus. 2022;14(3):e23029. doi:10.7759/cureus.23029.
- Miller IM, McAndrew RJ, Hamzavi I. Prevalence, risk factors, and comorbidities of hidradenitis suppurativa. Dermatol Clin. 2016;34(1):7–16. doi:10.1016/j.det.2015.08.002.
- Phan K, Charlton O, Smith SD. Global prevalence of hidradenitis suppurativa and geographical variation—systematic review and meta-analysis. Biomed Dermatol. 2020;4(1):2. doi:10.1186/s41702-019-0052-0.
- Ooi XT, Choi E, Han H, et al. The psychosocial burden of hidradenitis suppurativa in Singapore. JAAD Int. 2023;10:89–94. doi:10.1016/j.jdin.2022.10.010.
- Scholl L, Schneider-Burrus S, Fritz B, et al. The impact of surgical interventions on the psychosocial well-being of patients with hidradenitis suppurativa. J Dtsch Dermatol Ges. 2023;21(2):131–139. doi:10.1111/ddg.14934.
- Maghfour J, Sivesind TE, Dellavalle RP, et al. Trends in hidradenitis suppurativa disease severity and quality of life outcome measures: scoping review. JMIR Dermatol. 2021;4(2):e27869. doi:10.2196/27869.
- Horváth B, Janse I, Blok J, et al. Hurley staging refined: a proposal by the Dutch hidradenitis suppurativa expert group. Acta Derm Venerol. 2017;97(3):412–413. doi:10.2340/00015555-2513.
- Sartorius K, Emtestam L, Jemec GB, et al. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol. 2009;161(4):831–839. doi:10.1111/j.1365-2133.2009.09198.x.
- Sartorius K, Lapins J, Emtestam L, et al. Suggestions for uniform outcome variables when reporting treatment effects in hidradenitis suppurativa. Br J Dermatol. 2003;149(1):211–213. doi:10.1046/j.1365-2133.2003.05390.x.
- Marzano AV, Chiricozzi A, Giovanardi G, et al. Creation of a severity index for hidradenitis suppurativa that includes a validated quality-of-life measure: the HIDRAscore. J Eur Acad Dermatol Venereol. 2020;34(8):1815–1821. doi:10.1111/jdv.16328.
- Hessam S, Scholl L, Sand M, et al. Distinguishing mild, moderate, and severe hidradenitis suppurativa-reply. JAMA Dermatol. 2018;154(8):972. doi:10.1001/jamadermatol.2018.1600.
- Nesbitt E, Clements S, Driscoll M. A concise clinician’s guide to therapy for hidradenitis suppurativa. Int J Womens Dermatol. 2020;6(2):80–84. doi:10.1016/j.ijwd.2019.11.004.
- Hunger RE, Laffitte E, Läuchli S, et al. Swiss practice recommendations for the management of hidradenitis suppurativa/acne inversa. Dermatology. 2017;233(2-3):113–119. doi:10.1159/000477459.
- Ingram JR, Collier F, Brown D, et al. British association of dermatologists guidelines for the management of hidradenitis suppurativa (acne inversa) 2018. Br J Dermatol. 2019;180(5):1009–1017. doi:10.1111/bjd.17537.
- Johnston LA, Alhusayen R, Bourcier M, et al. Practical guidelines for managing patients with hidradenitis suppurativa: an update. J Cutan Med Surg. 2022;26(2_suppl):2S–24S. doi:10.1177/12034754221116115.
- Hendricks AJ, Hsiao JL, Lowes MA, et al. A comparison of international management guidelines for hidradenitis suppurativa. Dermatology. 2021;237(1):81–96. doi:10.1159/000503605.
- Bechara FG, Podda M, Prens EP, et al. Efficacy and safety of adalimumab in conjunction with surgery in moderate to severe hidradenitis suppurativa: the SHARPS randomized clinical trial. JAMA Surg. 2021;156(11):1001–1009. doi:10.1001/jamasurg.2021.3655.
- Abu Rached N, Gambichler T, Ocker L, et al. Screening for diabetes mellitus in patients with hidradenitis suppurativa-a monocentric study in Germany. Int J Mol Sci. 2023;24(7):6596. doi:10.3390/ijms24076596.
- Schrader AM, Deckers IE, van der Zee HH, et al. Hidradenitis suppurativa: a retrospective study of 846 dutch patients to identify factors associated with disease severity. J Am Acad Dermatol. 2014;71(3):460–467. doi:10.1016/j.jaad.2014.04.001.
- Richette P, Molto A, Viguier M, et al. Hidradenitis suppurativa associated with spondyloarthritis – results from a multicenter national prospective study. J Rheumatol. 2014;41(3):490–494. doi:10.3899/jrheum.130977.
- Saunte DM, Boer J, Stratigos A, et al. Diagnostic delay in hidradenitis suppurativa is a global problem. Br J Dermatol. 2015;173(6):1546–1549. doi:10.1111/bjd.14038.
- Garg A, Neuren E, Cha D, et al. Evaluating patients’ unmet needs in hidradenitis suppurativa: results from the global survey of impact and healthcare needs (VOICE) project. J Am Acad Dermatol. 2020;82(2):366–376. doi:10.1016/j.jaad.2019.06.1301.
- Hidradenitis Suppurativa: early Recognition Improves Prognosis - Medscape - 30. August 2019.
- Collier F, Howes R, Rodrigues J, et al. Primary care management of hidradenitis suppurativa: a cross-sectional survey of UK GPs. BJGP Open. 2021;5(5):BJGPO.2021.0051. doi:10.3399/BJGPO.2021.0051.
- Management of hidradenitis suppurativa: an Australasian consensus statement. Available at: https://dermnetnz.org/topics/hidradenitis-suppurativa-guidelines. Last updated: August 2018.
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian hidradenitis suppurativa foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81(1):76–90. doi:10.1016/j.jaad.2019.02.067.
- Alavi A, Lynde C, Alhusayen R, et al. Approach to the management of patients with hidradenitis suppurativa: a consensus document. J Cutan Med Surg. 2017;21(6):513–524. doi:10.1177/1203475417716117.
- Gulliver W, Zouboulis CC, Prens E, et al. Evidence-based approach to the treatment of hidradenitis suppurativa/acne inversa, based on the european guidelines for hidradenitis suppurativa. Rev Endocr Metab Disord. 2016;17(3):343–351. doi:10.1007/s11154-016-9328-5.
- Kimball AB, Jemec GBE, Yang M, et al. Assessing the validity, responsiveness and meaningfulness of the hidradenitis suppurativa clinical response (HiSCR) as the clinical endpoint for hidradenitis suppurativa treatment. Br J Dermatol. 2014;171(6):1434–1442. doi:10.1111/bjd.13270.
- Zouboulis CC, Bechara FG, Dickinson-Blok JL, et al. Hidradenitis suppurativa/acne inversa: a practical framework for treatment optimization - systematic review and recommendations from the HS ALLIANCE working group. J Eur Acad Dermatol Venereol. 2019;33(1):19–31. doi:10.1111/jdv.15233.
- Novartis Europharm Limited. Cosentyx® (secukinumab): Summary of Product Characteristics. Available at: https://www.ema.europa.eu/en/documents/product-information/cosentyx-epar-product-information_en.pdf. Accessed on October 05, 2023.
- Kohorst JJ, Baum CL, Otley CC, et al. Patient satisfaction and quality of life following surgery for hidradenitis suppurativa. Dermatol Surg. 2017;43(1):125–133. doi:10.1097/DSS.0000000000000942.
- Finstad A, Lee A, George R, et al. Exploring access to surgical interventions for hidradenitis suppurativa: retrospective population-based analysis. JMIR Dermatol. 2021;4(2):e31047. doi:10.2196/31047.
- Shukla N, Paul M, Halley M, et al. Identifying barriers to care and research in hidradenitis suppurativa: findings from a patient engagement event. Br J Dermatol. 2020;182(6):1490–1492. doi:10.1111/bjd.18818.
- Willems D, Hiligsmann M, van der Zee HH, et al. Identifying unmet care needs and important treatment attributes in the management of hidradenitis suppurativa: a qualitative interview study. Patient. 2022;15(2):207–218. doi:10.1007/s40271-021-00539-7.