ABSTRACT
The global rollout of antiretroviral treatment (ART) for HIV is one of the largest public health interventions ever undertaken. As the rollout expands, a growing body of research has focused on adherence to ART: how is it measured, what are the flaws of these metrics, and how may these be improved? We provide an overview of current, critical developments in adherence research among adolescents, and of how research on adherence to ART among adolescents within hyper-epidemic contexts has challenged definitions and measurements of adherence. We then explore the development of adherence metrics within an interdisciplinary study about HIV-positive adolescents: the Mzantsi Wakho study. Tracing the conceptualisation and adaptation of adherence metrics within this study, we examine how qualitative and quantitative approaches may be combined to establish more comprehensive adherence metrics. Findings highlight the challenges and the imperatives of synthesising numerous methods, data points, and temporalities. They also point to the need for researchers to establish direct and continued participation by adolescents themselves to better conceptualise and measure adherence, as well as other health behaviours.
The rollout of antiretroviral treatment (ART) has played a profound role in improving global public health, but it has also highlighted the challenges of sustaining access and adherence to treatment, including among adolescents and young adults. While global rates of AIDS-related mortality are declining among adults and children, they are increasing among adolescents (UNAIDS, Citation2016). Despite substantial investments in programmes for HIV prevention, treatment, and care, AIDS-related mortality among adolescents (aged 10–19) rose by 50% globally between 2005 and 2012 (UNAIDS, Citation2013). South Africa now has the largest ART programme in the world, with an estimated 3.7 million people having initiated ART by the end of 2016 (Republic of South Africa, Citation2017). However, adolescents are not benefitting proportionately from the ART rollout. They continue to experience higher rates virologic failure on ART, and higher rates of AIDS-related mortality, both related to non-adherence to medicines.
Studies from Southern Africa have documented lower rates of adherence to ART among adolescents compared to children and adults (Evans et al., Citation2013; Nachega et al., Citation2009) The difficulties of taking medication for chronic illnesses among adolescents have been long documented. However, the scale of the epidemic in this region – particularly among adolescents and young people – requires particular attention to long-term ART adherence. This paper elucidates the importance of understanding and measuring ART adherence, and the challenges of doing so. It maps the design and integration of interdisciplinary measurements and indicators of adherence within a study located in South Africa, named Mzantsi Wakho. This is the largest known, longitudinal, community-traced study of medicines and sexual health practices among HIV-positive adolescents.
Recent research that focuses on medicines-taking among HIV-positive adolescents emphasises the need for further studies, exploring new methodologies and combinations. But it is also imperative for research within this field to draw on older and wider literatures on adherence to medicines, including the benefits and pitfalls of various adherence metrics. Far from a distinct feature of the ART rollout, non-adherence to medical regimens is common across populations, locations, and disease type (DiMatteao, Citation2004, p. 200). The diversity of diseases, medical regimens, patient groups, and adherence indicators make it difficult to understand the specific nature of non-adherence for different medicine-users over time. A principal development in research on medicines-taking has been a shift in focus from the biomedical model of ‘compliance’ to that of ‘adherence’. This signals a conceptual expansion of medicines-taking from models of ‘perfect-use’ to broader understandings of patient ‘engagement’ with their treatment regimens (Amico & Stirratt, Citation2014, p. S56). While models of ‘perfect use’ might entail a stark classification of patient behaviour as either ‘compliant’ or ‘non-compliant’, investigating patient ‘engagement’ with medicines means understanding the unevenness and adaptations of medicines-taking over time, and exploring how different groups – such as adolescents and youth – conceive of adherence as it relates to their own, particular understandings of health, illness, and the practices of medicines-taking. Given that perfect-use is often unachievable, how do we best delineate ‘adherent’ from ‘non-adherent’?
Following from the challenges of conceptualising adherence are disputes about its means of measurement (Berg & Arnsten, Citation2006; Williams, Amico, Bova, & Womack, Citation2013). While the copious literature on adherence includes many examples of interdisciplinary research, traditional divisions between quantitative and qualitative research remain apparent, reflecting broader epistemological disputes about what constitutes methodological rigour and analytical value (Colvin, Citation2015). Indeed, there is now a substantive critical literature that seeks to interrogate how ‘evidence’ is made, weighted, and evaluated in different health contexts (Fan & Uretsky, Citation2016). Typically, qualitative studies on adherence are focused on comparably smaller groups and are concerned with the ‘subjective’ aspects of medicines-taking, including experiential and affective components. Quantitative studies have traditionally worked with larger sample sizes, using statistical techniques to demonstrate the significance and representativeness of findings, and seeking ‘objective’ means of validating patient self-report, including pharmacy pill-counts and biomarker data.
As in the broader literature on adherence to medicines, metrics for ART adherence have differed widely. They include various forms of self-report, ‘collateral rating’ (such as adherence reporting by a ‘treatment buddy’, healthcare worker or, in the case of young adolescents, caregivers), pill counts, and electronic measures. To offset the potential biases within each of these methods, studies may seek to combine multiple adherence measurements and time points. However, it is essential to recognise that even those adherence metrics that are classified as ‘objective’ – pill counts, physical tests and electronic measurements – are shown to have limitations to reliability (DiMatteao, Citation2004). Moreover, while statistical models may control for confounders to reduce or mitigate biases, the validity of adherence indicators remains much disputed (McCoy, Citation2009; Wilson et al., Citation2013).
Among the most widely used methods for quantifying ART adherence are patient self-report of different recall periods (past three days, past month, or last missed dose), pill counts (random or during routine clinic appointments), and pharmacy refill records. Each of these methods has attendant biases. Self-report is vulnerable to social desirability, cognitive, and recall bias. Pill counts – conducted largely by healthcare workers – enumerate how many pills patients have presented to be counted by healthcare workers or researchers at the end of a refill cycle, rather than how many they have taken. Pharmacy refills may be difficult to conduct, capture, and track in healthcare contexts with limited human resources, and in which pharmacists and other healthcare workers, already overburdened with the demands of clinical work, may be either unable or unwilling to keep detailed, longitudinal records of patients’ pill counts and of their compliance with prescription repeats and punctual return visits.
Attempts to improve the rigours of reporting on ART adherence heralded the introduction of magnetised pill containers within research studies (Haberer et al., Citation2010; Hersch et al., Citation2013). However, while these devices may capture the time and date at which a pill container is opened, they do not guarantee that tablets are taken.
Cognisant that behavioural metrics are flawed, studies on ART adherence have explored other metrics to ‘triangulate’ analyses, introducing an additional data point: biomarkers. The combination of adherence self-report with biomarkers has, for decades, been the ‘gold standard’ in studies on medicine compliance (Rudd, Citation1979). Through capturing biomarkers such as CD4 count and viral load measures, and computing these in association with other forms of adherence reporting, a more robust prognosis of a patient’s adherence practices theoretically emerges (Horvath et al., Citation2013). In reality, correlations between ART adherence and biomarkers may not be direct. Immunological outcomes are determined by a range of factors including, but not exclusive to, ART adherence, co-infections, and viral load at the point of treatment initiation. Among multidrug experienced children, who may already have drug resistance, CD4 count may be especially imprecise as a mode of inferring adherence through tracking immunological recovery.
There is a growing recognition of the importance of combining various methods and data points and of diversifying the evidence-base of critical public health research (Colvin, Citation2015; McLaren, Citation2017). Within the sphere of adherence research, a number of current studies seek to combine quantitative and qualitative methods, and to integrate their analytical approaches through synthesising modes of measurement. Their findings identify additional complexities in triangulating adherence practices with health outcomes (Bernays, Paparini, Seeley, & Rhodes, Citation2017; Stadler, Scorgie, van der Straten, & Saethrie, Citation2016).
Expanding contexts of ART adherence
In addition to an expanding critical literature on conceptualising, capturing, and analysing adherence, there is a growing recognition of the significance of context and location in researching the rollout of ART among adolescents. The majority of research studies on ART adherence have been conducted in the global north, among adult populations. The literature on adherence to medicines in the global south, particularly among children and adolescents, remains comparably sparse (Hudelson & Cluver, Citation2015; Mofenson & Cotton, Citation2013). Existing studies have, in large part, been health facilities-based (Evans et al., Citation2013). Yet, locating studies about medical behaviours within health facilities, particularly those that benefit from additional support and resourcing due to their ‘hosting’ of research studies, introduces powerful biases. Patients often behave differently within hospitals and clinics, where they are being monitored by healthcare workers and other patients, compared with how they behave outside them. Clinic research sites may also benefit from training, support, and monitoring, for both healthcare workers and for patients, resulting in a higher quality of care and improved health outcomes.
Public access to ART within hyper-endemic and resource-constrained settings has allowed for a more sustained focus on the practicable and experiential challenges of adolescent ART adherence within an array of settings (Merten et al., Citation2010; Sahay, Reddy, & Dhayarkar, Citation2011). A number of recent studies on adherence have sought to confront challenges of representativeness through locating research within multiple sites, providing potential for comparison across different locations and adolescent populations (Bernays et al., Citation2017; Kim et al., Citation2017; Nabukeera-Barungi et al., Citation2015). As an adjunct to research focusing on the clinical efficacy of ART, studies on ART adherence have included components on the socio-behavioural factors of adherence. They have each combined various forms of ART adherence, including ‘objective’ and ‘subjective’ measures, delving into definitional and conceptual challenges, and mapping discrepancies between ‘reported’ and ‘actual’ adherence.
Whether conducted through blood tests, nurse administered pill counts, self-report or electronic monitoring systems; each adherence measure is limited in its ability to offer an accurate picture of medicines-taking. Yet, it is imperative that we gain a greater understanding of the adherence practices of adolescents, in order both to monitor their immunological responses and to track the efficacy of their treatment regimens, as well as to identify if they are struggling to adhere, and to ensure that they are given the care and support that they need to take the medicines that are essential to their survival. Adding to the complexities of combining different adherence measures in order to establish a more comprehensive understanding of how individual patients use their medicines, there are additional challenges relating to the cost and feasibility of collecting comprehensive data on adherence. As Lorway (Citation2017) has shown in his study of the material artefacts – including the reams of paperwork – required to comply with the standardised reporting requirements of global health initiatives, the ever-growing demand for documents monitoring the health of patients and evaluating the workings of healthcare provision is often a source of frustration and alienation for healthcare workers themselves.
While researchers grapple with these methodological conundrums, and with the practicable difficulties of producing robust data about patients’ compliance in collaboration with healthcare workers, the demand grows for empirical, accessible, and timely information to inform HIV policy, programming and care for HIV-positive adolescents. Calls for ‘holistic’ or ‘comprehensive’ programmes to promote better health outcomes among adolescents recognise the imperatives of socio-economic, relational, and structural factors (World Health Organization, Citation2014). Alongside the greater rhetorical focus on the social dimensions of health, there is a growing commitment to including representatives of ‘target populations’ – the intended recipients of healthcare interventions – in the design and implementation of these programmes (Hodes et al., Citation2018a; Hodes et al., Citation2018b). To date, design and implementation of programming to improve adherence has rarely included the direct involvement of medicines-users. Participatory research provides an opportunity for the meaningful co-design of adherence interventions, which hold the possibility of strengthening users’ engagement with programming. Long-term participation of medicines-users in the development of adherence interventions can also help researchers move beyond short-term, instrumental models of participation towards those that account for the ever-changing workings of medicines in relation to the physical and social experiences, and the contextual realities, of their users (Montgomery & Pool, Citation2017).
The Mzantsi Wakho study – a multi-method cohort study of adherence among adolescents
In response to calls for more ‘holistic’ formulations of adherence, that reach beyond the clinical context to include social-environmental dynamics, and that include the insights of HIV-positive adolescents and their conceptualisations of medicines-taking, the Mzantsi Wakho ‘Your South Africa’ study was established in 2013. This is a cohort of 1060 HIV-positive adolescents and 467 ‘community controls’, which has had 94% retention over 3 years (2015–2018) (Figure S1). It aims to identify how we can improve healthcare access and retention in care for HIV-positive adolescents. In a relatively poorly resourced urban and rural health district of South Africa’s Eastern Cape, all 52 government clinics providing ART were sampled, and paper files reviewed to identify all adolescents who had ever initiated treatment. These adolescents were traced to 180 communities, to reach both those retained in healthcare, and those who had disengaged from care or were ‘lost to follow up’. Of 1176 eligible adolescents, 90.1% were included, 4.1% refused participation (either adolescent or caregiver), 0.9% had very severe cognitive delay, 3.7% were untraceable, and 1.2% no longer lived in the area. Data collected over three years comprised (1) detailed annual interviews in participants’ language of choice by local fieldworkers trained in working with vulnerable adolescents; (2) patient file records; and (3) information about services and resources in the clinics in which adolescents received care.
Preceding, and throughout, the quantitative study, researchers also conducted in-depth, qualitative research with 66 adolescents, their families, and their health providers. Research methods included semi-structured interviews, focus groups, and participatory workshops, as well as observations in clinics, homes, leisure spaces, and support groups.
The research project was initiated in 2013. Eight months of ethnographic research preceded the design and piloting of the baseline quantitative survey. In this first phase, 23 adolescents were enrolled in the study through local healthcare and social service providers. Rather than engaging with adults, such as caregivers or healthcare workers, as ‘proxy informants’ for adolescents, the study approached adolescents as direct, principal participants.
A study such as this poses serious ethical considerations: its primary participants were often below the legal age of consent, living with a stigmatised illness, and socio-economically vulnerable. Enabling voluntary, safe and meaningful participation demanded careful collaboration with adolescents and their families, regular renewals of consent, and fastidious training of the fieldwork team. Our responses to the ethical dilemmas that arose in this research are described further in the ‘Findings’ section. Ethics approval for this study was provided by Research Ethics Committees at the Universities of Oxford (SSD/CUREC2/12-21) and Cape Town (CSSR 2013/4), Eastern Cape Departments of Health and Basic Education, as well as ethical review boards of participating facilities. Written voluntary informed consent was given by all adolescents and their primary caregivers, and consent information was read aloud in cases of low literacy. There were no financial incentives, but all adolescents received a snack, participant pack containing toiletries and household items (such as soap, shoe polish, and face cloths) and a certificate. Confidentiality was maintained except in cases of risk of harm: if adolescents reported abuse, suicidality, rape, or severe illness, then referrals were made to relevant social or health services and followed up to ensure that support services were received.
In the baseline quantitative survey, adolescents were 55% female, with a mean age of 13.8 years. Forty-four per cent were maternally bereaved and 30% paternally bereaved. Around 74% were vertically infected. The study combined various methods for investigating ART adherence among adolescents, seeking their direct engagement in the design and adaptation of research tools. Its multiple components are united by three principal objectives. The first was to position young people as the primary experts on their own health behaviours. Second, we investigated health behaviours both within and beyond clinical contexts. While interviews and observations were conducted within health facilities, the bulk of both qualitative and quantitative research took place in participants’ homes and leisure spaces. Third, the study followed an iterative approach in developing, piloting, and adapting research tools; analysing data; and capturing findings (described further below). Emerging themes from qualitative research informed the structure of the quantitative questionnaire, and, as the study progressed, findings from the quantitative survey informed further qualitative data collection and analyses.
Findings
Our initial findings concerned the difficulties that adolescents faced in recalling and relating their precise adherence practices. In the first year of qualitative data collection, which took place both in villages and peri-urban townships of the Eastern Cape, researchers noted that adolescent, caregiver, and health worker reports of adolescent adherence were often partial and inconsistent. Almost all adolescent participants reported that that they were adhering diligently to their regimens. For many, taking ART inconsistently was an experience that was difficult to convey, particularly since admissions of non-adherence were often followed by reproaches or reprimands by guardians and health providers, who viewed it as their duty to oversee, coax, and at times enforce adherence. Responses to caregivers’ and healthcare workers’ discoveries of non-adherence among adolescents ranged from verbal rebukes to physical threats and punishments, and took place both in homes and in clinics (Cluver et al., Citation2018).
Hesitancy to speak about non-adherence produced murky and inconsistent accounts of adolescent pill-taking. When asked if they took their pills well, all adolescent respondents said ‘yes’. Similarly, when asked if they ever forgot to take their pills or made a decision not to take them, adolescents responded, ‘no’. However, when asked if there was ever a time they ‘wanted’ to take their pills but could not, more detailed narratives emerged. These included accounts of stock-outs in clinics, an inability to take treatment on an empty stomach, and the fear of being seen in public in possession of ART (which would disclose the adolescents’ HIV-positive status to those nearby). Participants also explained that they forgot their medicines when they were busy or traveling, or grew bored and frustrated with the routine and proscribed nature of pill-taking. By asking questions on adherence in ways that assumed the adolescent or caregivers’ ‘good intentions’, or that reassured participants that they were not be reprimanded or punished for honest accounts of non-adherence, researchers were better able to uncover the practicable realities of medicines-use, and to investigate barriers to adherence.
These qualitative findings informed the phrasing of the study’s quantitative survey. To offset gaming and social desirability bias, researchers encouraged participants to be honest about their medicines-taking practices and assured them that there would not be negative consequences if they reported missing doses. These commitments were upheld in the years of primary research that followed, with researchers aiming to maintain a neutral approach to accounts of non-adherence while upholding the ethical requirements for reporting recent or urgent cases of physical danger to local healthcare and social service providers. Within interviews, participatory research, and particularly within direct observations, discrepancies between the reports and actualities of ART adherence were revealed. At times, these discrepancies surfaced within a single interview, in which a participant’s initial reports of perfect adherence were qualified and changed, supplanted by longer-term recollections of haphazard adherence and defaulting.
Qualitative findings further underscored the importance of using participatory approaches to encourage adolescents to conceptualise and convey their experiences of living with HIV and on ART, and to combine a range of metrics to capture adherence. In order to provide a new mode of description, encouraging participants to focus on the specific difficulties of medicines-taking, a participatory exercise was piloted. In this exercise, titled ‘The Smarties Game’, participants were invited to compare the experience of ART-taking with a behaviour that was more familiar and less stigmatised, and which adolescents had confidence in relating: eating sweets. In the course of multiple in-depth interviews with each participant, conducted over Eight months, adolescents were invited to eat sweets that were similar in size and shape to the tablets commonly prescribed for colds and widely available in clinics and shops. They were asked to explain how eating sweets was similar or different from taking ART, comparing the emotional and sensory qualities of each experience.
This pilot exercise identified a number of experiential aspects of ART adherence, including the salience of palatability and pill burden. Participants spoke about the number of tablets they were taking, which ranged from two to seven a day, reflecting the diversity of ART regimens available within a single health district. In describing why they missed doses of their treatment, participants described ART adherence as arduous and awkward. Palesa (female, 18) recounted: ‘taking the pills is hard work. I get lazy to take them. They are big and they stick in my throat’ (interview, 14 February 2013). The exercise revealed the dense and variegated emotions bound up in ART adherence. Rather than a neutral exercise, the act of medicines-taking was imbued with thought and feeling, overlaid with memory, and qualified through association. The exercise invited participants to consider and to describe how different factors affected, altered, and ascribed their healthcare behaviours, and related to other social identities and systems of belief.
Conducting research on medicines-taking both within and outside healthcare facilities underscored the importance of research setting in creating a comprehensive account of adherence. Within facilities, adolescent participants strived to present as ideal patients, reporting perfect ART adherence, in keeping with the proscriptions of healthcare workers. They were polite towards elders, and patient in waiting areas. Outside facilities, in leisure spaces or homes, they spoke more freely about the difficulties they encountered in adhering to ART. They shared doubts about the efficacy of their medicines, and vented frustrations about the perceived strictness of adherence protocols. Indeed, outside clinical contexts, adolescents’ identities were composed of a myriad social roles, experiences, and aspirations – including, but not solely determined by, their HIV-status. Adherence to ART was bound up in competing health and social concerns, including desires for self-regulation and autonomy, as well as for privacy and belonging. In order to understand adolescents’ experiences of health-care, and their medicines-taking, further research was located primarily within the homes and recreational spaces of adolescent participants.
Participants’ hesitancy to disclose instances of non-adherence also posed important questions at the intersection of methodology and ethics. For example: in some cases, an adolescent’s admission of missed doses might hinge on their confidence that this information would not be disclosed to their guardians or healthcare workers. In assuring and protecting adolescent confidentiality, valuable information about non-adherence was gathered – of central importance to a research study about the real-world practices of medicines-taking among adolescents. However, since consistent non-adherence poses a serious threat to adolescents’ health and survival, retaining confidentiality risked compromising the ethical obligation to protecting participants from harm. These complex ethical quandaries were negotiated carefully on a case-by-case basis within the study. They not only compound the methodological challenges for ART adherence research, but indeed any research endeavour related to risky, stigmatised behaviours, and to the health of children and adolescents as well as other potentially marginalised or vulnerable populations.
Informing the adherence measure
These findings informed the conceptualisation of adherence within Mzantsi Wakho’s quantitative survey, which combines multiple recall strategies and timelines with the aim of constructing a robust adherence metric, and of revealing potential discrepancies between various means of self-report and biomarker data. The quantitative adherence outcome measure was developed incrementally. A literature review identified studies that had measured ART adherence among adolescents, and explored the utility of standardised measures for assessing adherence among adolescents in Southern Africa (Duong et al., Citation2015; Lowenthal et al., Citation2014). The standardised Patient Medication Adherence Questionnaire, the quantitative measure for adherence used in the Mzantsti Wakho questionnaire, was adapted in several ways to incorporate findings from both preceding qualitative research within the study, and from the secondary literature.
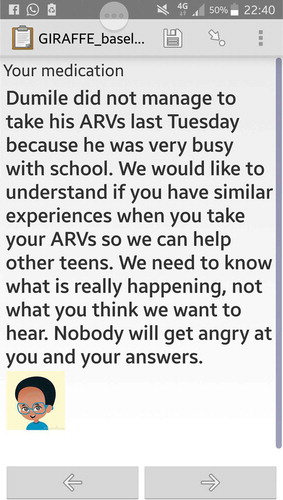
First, ART adherence was measured across several timelines, aiming to minimise recall bias and to document patterns of non-adherence unique to adolescents: correct number of doses at the right time in the past week, last missed dose, and number of missed doses in the previous weekend and past month. Second, items investigating missed clinic appointments, ART stock-outs, and who attended the scheduled clinic appointment (adolescent, caregiver, or both) provided insights into the dynamics of adolescent ART-taking beyond the actions of the individual patient. Third, vignettes were added at the start of a cluster of questions about adherence, assuring participants that researchers were aware of the difficulties bound up in ART adherence. Based on qualitative findings that participants would be more likely to disclosure non-adherence if approached in a non-judgmental way, these vignettes aimed to encourage honest accounts, providing examples of a range of treatment-taking practices with which participants could potentially identify. Images of these vignettes, as they appeared on the tablets in the quantitative questionnaire, are provided in (see also Figures S2 and S3). Fourth, in the second round of quantitative data collection (2016–2017), audio and mobile-assisted self-interviewing was used to capture responses of highly stigmatised behaviours, including non-adherence to ART. The quantitative questionnaire was conducted using low-cost digital tablets with audio tracks designed for populations with limited literacy.
Figure 1. Vignette introducing a section within the quantitative survey on factors affecting non-adherence.
The first version of the quantitative questionnaire was completed in late 2013. Over the course of six weeks, the Mzantsi Wakho research team – made up of interdisciplinary researchers – analysed its verbal and visual content. Based on the insights and recommendations from this collaboration, the content of the quantitative adherence measure was adapted further to ensure it was accessible and understandable to both researchers collecting primary data and to research participants. In February 2014, the quantitative adherence measures were piloted with 25 HIV-positive adolescents who lived in rural, peri-urban, and urban locations of the study site. Adolescents suggested modifications to the wording and content of the questions. For example, the standardised measure of ‘missed doses over the past three days’ was worded as the ‘correct number of doses each day: yesterday, day before, and two days ago’. Thus, the questionnaire reworded the negative valuation of ‘missing’ doses to the positive recognition of ‘correct’ number of doses taken. Participants also suggested preceding a question about missed doses over the weekend with a more neutral question about their weekend activities. These revisions were incorporated into the content of the questionnaire.
Gathering clinical data on ART adherence
Between 2013 and 2015, the Mzantsi Wakho study captured and analysed baseline qualitative and quantitative data on adherence among adolescents, based largely on participant-self-report and observations conducted in antiretroviral, family planning, and trauma units at public healthcare facilities. In 2015, a dedicated team of researchers within the broader investigator team was established to capture biomarker data from adolescents’ patient folders, housed at public clinics that provided their care. Emerging findings presented new challenges in integrating adherence self-report and biomarkers, as well as information about pill-counts captured within patient files. As of December 2017, 88.4% of the patient files for the 1060 Mzantsi Wakho participants had been located. Of these, 92.1% had any viral load data recorded, but less than half had a viral load measure collected in the past two years (Haghighat, Cluver, Bungane, & Toska, Citation2017). A community healthcare worker, whose primary role was to support HIV-positive patients enrolled in the ART programme at a Day Hospital in the research area, summed up the challenges faced by the facility’s data capturers: ‘They don’t have time to go through the whole backlog of patient folders. There’s some chaos in the data’ (personal communication, Day Hospital 2, 30 August 2015). Data capturers at the same facilities had different impressions about the reasons for incomplete and chaotically stored patient records. The facility’s principal data capturer explained: ‘The nurses don’t fill in the registers properly, because they say they are busy … Then you will have lots of gaps in your data’. The challenges of maintaining accurate patient records, and the temptations of fabricating data to meet formal measures of quality control, were evident at many facilities.
Patient records were often incomplete and outdated. In many instances, diagnostic reports such as CD4 counts were included in patient folders, while their results were not copied into forms that documented a patient’s history of HIV-testing and ART initiation (known as the ‘ART stationary’). At other times, laboratory reports were stored in boxes in data capturers’ offices, awaiting copying, sorting, and - at least foreseeably - inclusion in patient folders. The ART paediatric stationary was intended to serve as a comprehensive dossier of a patient’s HIV treatment. In assessing a patient’s adherence, healthcare workers were required to fill in a section of the paediatric ART stationery (released in 2015). On dosing, the section provided four options as boxes to be ticked: ‘takes all doses; frequently misses a dose; occasionally misses a dose; not taking medicines’.
In the course of South Africa’s public rollout of ART, the content and the categories captured by patient forms have been painstakingly debated and reworked. The different versions of the ART stationary circulating within facilities reveal repeated attempts to improve the data quality. However, as noted during extensive observations within healthcare facilities, filling in the form was often an automatic exercise. Healthcare workers frequently completed forms based on recall of adolescent patients, or in conversation with adult caregivers (‘proxy patients’) who had travelled to the healthcare facility to fetch medicines on the adolescent patient’s behalf. At times, forms were completed by data capturers with no knowledge of the patient, and no formal experience of clinical consultation. While these practices were observed within a particular health district, they highlight the biases and inaccuracies of adherence metrics as recorded in patient folders within public health facilities. Much of the empirical evidence about the initiation and retention of ART patients in South Africa is based on data from these folders.
In response to the limited availability of current biomarker data for participants, quantitative analyses validated self-reported adherence measures against viral suppression rates among adolescents for whom recent biomarker data were available. Results indicated a strong association between these two measures, even when tested in multivariate regressions, controlling for a wide range of socio-demographic and clinic-related factors (odds ratio [OR] = 2.32, confidence interval [CI] 1.41–3.84, p = 0,001) (Cluver et al., Citation2016). As an additional validation check, self-reported non-adherence was validated against symptomatic tuberculosis, with similar associations (OR = 1.54, CI 1.07–2.22, p = 0.02). Emerging analysis from the first wave of the Mzantsi Wakho study demonstrated the predictive validity of combining self-report with biologic outcomes in assessing the health impacts of ART adherence. However, gaps in the availability of biological markers reveal the real-world difficulties in capturing and analysing clinical records as a source of information on health behaviours. These records highlighted the hazards of empirical analysis based on the adherence metrics captured in patient reports: including pill counts and pharmacy refills.
Discussion
This paper provides a synthesis of some of the key methodological, conceptual, and practical challenges that arise in studying ART adherence among adolescents, while offering insights into how a large, mixed methods, longitudinal study sought to adapt and integrate research approaches to elicit more comprehensive accounts of adolescents’ experiences of medicines-taking. With a focus on the methodological complexities of measuring adherence, this paper describes how adherence metrics are amenable to various biases, and how their capture and analysis rely on forms of selection and extrapolation. But while the paper acknowledges the flaws inherent in various adherence measures – the peskiness of metrics – it also explores how interdisciplinary methods may be used to diversify studies of health behaviours. It describes how conducting research in ‘extra-clinical’ settings may broaden understandings of adherence across multiple times and settings, expanding patient-recall from a single snapshot, to a more detailed portrait, including patterns of use. It documents how accounts of ART adherence, provided by patients within facilities, and captured by healthcare workers in clinic documents, have differed from of what patients relate about adherence to medicines within their homes.
Biomedical programmes that aim to improve health-seeking behaviours often focus on a single dimension of healthcare, targeting healthcare facilities, disease groups, or individual patients. Evidence on the global, public ART rollout increasingly recognises the necessity of a multidimensional approach to research and programming, and to the combination of research strategies to elicit more inclusive accounts of health behaviours beyond models of ‘perfect use’. As emerging findings from the Mzantsi Wakho study have shown, qualitative techniques may be incorporated within the design and analysis of quantitative and biometric data to build a more comprehensive picture of adolescent adherence. Experimental, qualitative methods, including participatory research, may be used to provide reflexive, participant-centred perspectives on adherence to ART.
ART adherence research has grown substantially in the last five decades, branching out from its clinical and pharmacological bases. The expansion of research settings is mirrored in the growth and diversification of study cohorts – from studies on adherence among ‘patients’, to more expansive and sustained engagements with the social and experiential dimensions of adherence among diverse populations. As the ART rollout ages, and as the challenges of retaining patients in life-long, chronic care become more apparent, there is a need for improved understandings of adherence. This includes a recognition of both the flaws and the benefits inherent in different metrics, and for novel attempts at their triangulation across diverse research disciplines and settings.
This paper has outlined the challenges of researching adherence, as well as the gains to be made with a participatory, mixed-methods and multi-setting approach. Given that adherence is a long-term, dynamic and often uneven practice, with medicines taken at different hours of the day, across multiple settings, and at different stages of a persons’ life, it is essential that research moves beyond short-term, clinically-focused studies of adherence to include more expansive and integrated accounts of medicines-taking.
Figure S1
Download PDF (213.6 KB)Figure S2
Download PDF (182.8 KB)Figure S3
Download PDF (309.5 KB)Acknowledgements
Authors thank participants and their families, and acknowledge the crucial support of the Mzantsi Wakho research team: S Banzana, O Barns, P Bellem, W Booi, N Boqwana, M Boyes, N Bungane, L Button, L Campeau, A Carlqvist, M Casale, C Carty, KE Chademana, M Coqui, J Doubt, M Dukata, Y Dunkley, C Dyer, A Egan, N Ella, J Ellis, V Evans Gutiérrez, N Galela, C Gilmer, L Gittings, N Gwebecimele, R Haghighat, E He, A Heusel, N Hlwele, S Hoeksma, N Homani, M Isaacsohn, V Jali, Z Jantjies, J Jochim, R Jopling, C Kama, B Kamile, C Kelly, B Kinana, P Kom, V Luke, O Madikane, B Madondo, S Mahleza, K Makabane, B Makwenkwe, T Mampangashe, Z Marikeni, D Mark, X Matebese, A Mayekiso, A Mbiko, A Mboyiya, S Mbula, N Mdi, F Meinck, D Mhlauli, B Mkati, S Medley, N Mendu, F Menziwa, P Mngese, S Mngese, P Mjo, S Mona, M Moshabela, T Moyikwa, S Mpimpilashe, M Mpumlwana, S Mqalo, Z Mqhashane, S Mwellie, N Myeketsi, P Myoyo, H Natukunda, T Ncapai, M Neel, U Ngesi, S Ngozi, P Nobatye, N Nurova, A Nyamweda, M Orkin, M Pancoast, M Pantelic, L Parmley, L Pilard, T Ramncwana, A Robb, J Rosenfeld, B Saliwe, J Sandelson, I Savage, D Sephula, N Shah, A Sharma, L Sherr, N Sibanda, L Sidloyi, M Simandla, U Simandla, N Simaya, I Skracic, R Smith, N Sontsonga, J Steinert, X Swelindawo, B Taleni, M Thabeng, S Tshaka, T Tsiba, J Van der Wal, T Walker, S Walters, P Wardle, and C Wittesaele. We are grateful to Judith Green, Ariene Kayette Malanog and two anonymous reviewers for their excellent guidance on improving the content of this paper. We thank the students and staff of the Centre for Social Science Research at the University of Cape Town for their comments on this research, provided in a seminar convened in January 2018. In particular, we thank Nicoli Nattrass for her insights and critical advice.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Amico, K. R., & Stirratt, M. J. (2014). Adherence to preexposure prophylaxis: Current, emerging, and anticipated bases of evidence. Clinical Infectious Diseases, 59(1), S55–S60.
- Berg, K., & Arnsten, J. (2006). Practical and conceptual challenges in measuring antiretroviral adherence. Journal of Acquired Immune Deficiency Syndromes, 43(1), S79–S87.
- Bernays, S., Paparini, S., Seeley, J., & Rhodes, T. (2017). “Not taking it will just be like a sin”: Young people living with HIV and the stigmatization of less-than-perfect adherence to antiretroviral therapy. Medical Anthropology, 5, 1–15.
- Cluver, L., Meinck, F., Toska, E., Orkin, F. M., Hodes, R., & Sherr, L. (2018). Multi-type violence exposures and adolescent antiretroviral non-adherence in South Africa. AIDS, 32(8), 975–983.
- Cluver, L. D., Toska, E., Orkin, F. M., Meinck, F., Hodes, R., Yakubovich, A. R., & Sherr, L. (2016). Achieving equity in HIV-treatment outcomes: Can social protection improve adolescent ART-adherence in South Africa? AIDS Care, 28(2), 73–82.
- Colvin, C. (2015). Anthropologies in and of evidence making in global health research and policy. Medical Anthropology, 34(2), 99–105.
- DiMatteao, M. R. (2004). Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care, 42(3), 200–209.
- Duong, M., Piroth, L., Grappin, M., Forte, F., Peytavin, G., Buisson, M., et al. (2015). Evaluation of the patient medication adherence questionnaire as a tool for self-reported adherence assessment in HIV-infected patients on antiretroviral regimens. HIV Clinical Trials, 2(2), 128–135.
- Evans, D., Menezes, C., Mahomed, K., Macdonald, P., Untiedt, S., Levin, L., … Maskew, M. (2013). Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Research and Human Retroviruses, 29(6), 892–900.
- Fan, E., & Uretsky, E. (2016). In search of results: Anthropological interrogations of evidence-based global health. Critical Public Health, 27(2), 157–162.
- Haberer, J., Kahane, J., Kigozi, I., Emenyonu, N., Hunt, P., Martin, J., & Bangsberg, D. (2010). Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behaviour, 14(6), 1340–1346.
- Haghighat, R., Cluver, L., Bungane, N., & Toska, E. (June, 2017). HIV treatment cascade among ART-initiated adolescents in South Africa. Poster presented at the Southern African AIDS Conference, Durban, South Africa.
- Hersch, R., Cook, R., Billings, D., Kaplan, S., Murray, D., Safren, S., … Spencer, J. (2013). Test of a web-based program to improve adherence to HIV medications. AIDS Behaviour, 17(9), S1–26.
- Hodes, R., Doubt, J., Toska, E., Vale, B., Zungu, M., & Cluver, L. (2018a). The stuff that dreams are made of: HIV-positive adolescents’ aspirations for development. JIAS, 21(S1), E25057.
- Hodes, R., Vale, B., Toska, E., Cluver, L., Dowse, R., & Ashorn, M. (2018b). Yummy or crummy? The multisensory components of medicines-taking among HIV-positive youth. Global Public Health, ISSN: 1744-1692 ISSN: 1744-1692 (Print) 1744-1706 (Online). doi:https://doi.org/10.1080/17441692.2018.1504103
- Horvath, K., Oakes, M., Simon, B. R., Danilenko, R., Vezina, H., Amico, K. R., … Simoni, J. (2013). Feasibility, acceptability and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. AIDS Behaviour, 17(6), 2031–2044.
- Hudelson, C., & Cluver, L. (2015). Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: A systematic review. AIDS Care, 27(7), 805–816.
- Kim, M., Mazenga, A., Yu, X., Ahmed, S., Paul, M., Kazembe, P., & Abrams, E. (2017). High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: Barriers and associated factors. JIAS, 20, 21437.
- Lorway, R. (2017). Making global health knowledge: Documents, standards, and evidentiary sovereignty in HIV interventions in South India. Critical Public Health, 27(2), 177–192.
- Lowenthal, E. D., Bakeera-Kitaka, S., Marukutira, T., Chapman, J., Goldrath, K., & Ferrand, R. A. (2014). Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: A review of emerging challenges. The Lancet Infectious Diseases, 14(7), 627–639.
- McCoy, L. (2009). Time, self and the medication day: A closer look at the everyday work of ‘adherence. Sociology of Health and Illness, 31(1), 128–146.
- McLaren, L. (2017). A space for critical quantitative public health research? Critical Public Health, 27(4), 391–393.
- Merten, S., Kenter, E., McKenzie, O., Musheke, M., Ntalasha, H., & Martin-Hilber, A. (2010). Patient-reported barriers and drivers of adherence to antiretrovirals in sub-Saharan Africa: A meta-ethnography. Tropical Medicine and International Health, 15(1), 16–35.
- Mofenson, L. M., & Cotton, M. F. (2013). The challenges of success: Adolescents with perinatal HIV infection. JIAS, 16(18650), 15–17.
- Montgomery, C., & Pool, R. (2017). From ‘trial community’ to ‘experimental publics’: How clinical research shapes public participation. Critical Public Health, 27(1), 50–62.
- Nabukeera-Barungi, N., Elyanu, P., Asire, B., Katureebe, C., Lukabwe, I., Namusoke, E., … Tumwesigye, N. (2015). Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infectious Diseases, 15(520). doi:10.1186/s12879-015-1265-5
- Nachega, J. B., Hislop, M., Nguyen, H., Dowdy, D. W., Chaisson, R. E., Regensberg, L., Martens, G. (2009). Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in Southern Africa. JAIDS, 51(1), 65–71.
- Republic of South Africa. (2017). Let our actions count: South Africa’s National strategic plan for HIV, TB and STIs 2017-2022. Pretoria, South Africa.
- Rudd, P. (1979). In search of a gold standard for compliance measurement. Archives of Internal Medicine, 139(6), 627–628.
- Sahay, K., Reddy, S., & Dhayarkar, S. (2011). Optimizing adherence to antiretroviral therapy. Indian Journal of Medical Research, 134(6), 835–849.
- Stadler, J., Scorgie, F., van der Straten, A., & Saethrie, E. (2016). Adherence and the lie in a HIV prevention clinical trial. Medical Anthropology, 35(6), 503–516.
- UNAIDS. (2013). Global report: UNAIDS report on the global AIDS epidemic 2013. Retrieved from http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf
- UNAIDS. (2016). Global AIDS Update. Retrieved from http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf
- Williams, A., Amico, K., Bova, C., & Womack, J. (2013). A proposal for quality standards in measuring medication adherence in research. AIDS Behaviour, 17(1), 284–297.
- Wilson, I., Bangsberg, D., Shen, J., Simoni, J., Reynolds, N., Goggin, K., … Liu, H. (2013). Heterogeneity among studies in rates of decline of antiretroviral therapy adherence over time: Results form the multisite adherence collaboration on HIV 14 study. JAIDS, 64, 448–454.
- World Health Organization. (2014). Adolescence: A second chance in the second decade. Geneva: WHO.
