ABSTRACT
In recent years, mobile health (mHealth) technologies have received increasing attention from industry and researchers. Such technologies have been the focus of both criticism and high expectations. In this paper, we analyze the integration of mHealth tools in everyday life. Insights into the actual use of such tools have empirical importance and could contribute to our theoretical understanding of mHealth technologies. Our research is based on 23 interviews with the participants of a smartphone-based mobile health intervention aimed at increasing physical activity. We followed the principles of grounded theory during data collection and our analysis is framed by the domestication approach. Our results reveal that the intervention design can result in the participants feeling ill-represented by the reductive nature of the data they generate. The results also reveal the inadequacy between biomedical standards and the social contexts of use. In addition, we describe how middle-class users perceive step-counting through the prism of a moralizing ethos of self-responsibility. Our research has practical implications for the developers and participants of mHealth interventions and theoretical implications regarding mHealth as a societal practice. We also suggest that mHealth-related public policies may fail to reach certain population groups, namely those who do not share the values that surround those technologies and their uses.
Introduction
Recent years have seen a rapid development of discourses and practices related to mobile health (mHealth) and self-tracking. In the fields of health and physical activity, these terms generally refer to the measurement of bodily functions via connected tools. Many countries (e.g., the United States,Footnote1 the United Kingdom,Footnote2 Germany,Footnote3 FranceFootnote4 and SwitzerlandFootnote5) have developed guidelines for mHealth, hoping that it will improve user health and lower health costs. The production of, and research in industryFootnote6 and laboratories on, mHealth devices and softwares have exhibited rapid growth (the number of mHealth references on PubMed increased from 1,806 in 2013 to 3,551 in 2018). This development seems to be characteristic of the ‘promise economy’ often observed in innovation (Audétat, Citation2015). A ‘healthist’ (Crawford, Citation1980; Lupton, Citation2013, Citation2017) sociocultural context often frames the marketing of these technologies (Fotopoulou & O’Riordan, Citation2017). Aside from promises and discourses, our goal in this article is to analyze the reception of an mHealth self-tracking application in users’ daily life.
Deborah Lupton analyzed the market of self-tracking applications and described its focus on self-responsibility and individualism (Lupton, Citation2014). Similarly, researchers have shown that a biopedagogy that targets ‘acceptable modes of conduct in a neoliberal health landscape’ is embedded in the most diffused self-tracking tools (Fotopoulou & O’Riordan, Citation2017, p. 13). For example, Fitbit devices are designed to mediate the implementation of micropractices such as calorie counting in the everyday life of users. They thereby promote the alignment of user behavior with dominant health norms (Fotopoulou & O’Riordan, Citation2017). Concerning practices, an early study identified three categories of individuals who use self-tracking applications for (1) the surveillance of a specific metric, (2) the routinization of a health habit and (3) the tracking of personal objectives (Pharabod et al. Citation2013). In 2019, Deborah Lupton drew on 40 interviews to show that self-trackers, although their practices are integrated into neoliberal and surveillance rationales, generate agential capacities such as awareness and self-control (Lupton, Citation2019). As noted by Tamar Sharon, self-tracking can be both enabling and constraining and is highly dependent on the specificities of the tools and the context in which they are used (Sharon, Citation2017). Our aim is to document this duality in practice: that is, in the process through which users adopt or reject (or both) mHealth interventions.
The focus of the application that we analyzed was walking as a daily physical activity. The application is described in detail by Kramer et al. (Citation2019). Other studies on apps to increase walking have demonstrated that the measurement of steps via an app has an effect on the users’ perception of walking (Harries & Rettie, Citation2016). Walking to the local post office, a previously incidental practice, can gain the added value of improving health when framed by daily tracking and digital health interventions. The same researchers suggest that measurement may result in a transformation of the daily practice of walking into a health practice (Carter et al. Citation2018). Similarly, drawing on Foucault and phenomenology, Mary Louise Adams indicated that the practice of step-counting reduces the user’s understanding of walking to a form of ‘healthism’ (Adams, Citation2018). By extending such research, we seek to analyze what occurs when an mHealth intervention on walking developed in the context of insurance and health promotion is used in everyday life.
Theoretical framework
Describing the integration of an mHealth intervention in everyday life and documenting the work performed by users requires us to acknowledge that practices are co-constructed by both the participants and the technology. Our analysis thus addresses the technical features of the technology (Akrich, Citation1997) and how they both enable and constrain uses (Oudshoorn & Pinch, Citation2008). Though we do not focus on the work of designers, we acknowledge that the technical features of the technologies are ‘the products of human decision-making, underpinned by tacit assumptions, norms and discourses already circulating in the social and cultural contexts in which they are generated, marketed and used’ (Lupton, Citation2014, p. 607).
After describing the technology, we turn to its interaction with users. We want to contribute to the understanding of the integration of mHealth interventions in daily life. The domestication approach is focused on the entrance of technologies into users’ lives (Haddon, Citation2011; Silverstone et al. Citation1992). It offers an analytical framework that emphasizes the symbolic work that users must perform to either adopt, reshape or reject the meanings inscribed in technologies and the practical work needed to incorporate them in everyday routines (Sorensen, Citation2006). Domestication acknowledges not only the work performed by users but also the impact of the embedded meanings of the medium on domestication (Berker, Citation2006). Moreover, domestication draws attention to the transformations or resistances that can occur. In this framework, the domestication of technology can both enable and constrain the ‘performances of identities and negotiations of status and social position’ (Oudshoorn & Pinch, Citation2008). There is a need for a contextualized, that is, a technology and participant-specific, account of the domestication of digital health interventions. We offer such an account, suggesting that the analytical framework presented by the domestication approach, which allows us to account for the practical and symbolical work involved in the coconstruction of the practice, is adapted for this task. It must be noted that our users domesticated the technology in the context of a scientific protocol (see methodology). Therefore, most of them felt responsible for finishing the protocol, even if they did not particularly enjoy the technology. It certainly prevented some disengagements from the technology which would have happened outside of the research context, for example in the case of a failed appropriation.
Domestication is analytically divided into four phases, namely, appropriation, objectivation, incorporation and conversion (Haddon, Citation2007, Citation2011; Hirsch & Silverstone, Citation1992). Appropriation describes the negotiations and considerations through which individuals decide to buy and adopt a technology. It has been described as the construction of a desire for the technology and can take the shape of a ‘desire for difference and social meaning’ (Hynes & Rommes, Citation2005, p. 128). In the process of objectification, the technology is given space both materially and symbolically in the individuals’ moral economy. Incorporation focuses on temporality and the ways in which users fit the technology into their everyday routines. Finally, conversion occurs when individuals recast the meanings that they have created with the technology to themselves or other people and thus participate in the public definition of the technology.
Our goal in this article is to analyze how users incorporate a mHealth application in everyday life. Using the conceptual framework of domestication, we describe how the interaction between users and the application, which involves both resistances and agreements, results in a specific health tracking practice. Our results indicate that the specificities of a mHealth intervention and the social values of its participants have a significant impact on the type of practice that emerges from their interaction. If the literature has often emphasized the technical features of the technologies, we argue that the social values and the social position of users should be more systematically addressed. Furthermore, emphasis should be put on how these are reshaped in the process of domestication.
Methodology
The ALLY application analyzed in this paper was developed by an interdisciplinary team of researchers whose expertise lies in the fields of behavioral medicine, health psychology and computer science. The ALLY application was developed in a research project that was jointly funded by a large health insurer. It was evaluated in a six-week optimization trial, e.g., an experimental study to select the intervention components that qualify for implementation in the final version of the application (Kramer et al., Citation2019). The first and last authors of the present article, who are both sociologists, were not involved in the development of the application. They designed and directed the interviews in collaboration with the other two authors, who are part of the team that developed the application.
The invitation to participate in the study was sent to 30,000 German-speaking insurance customers who were enrolled in complementary (that is, in addition to compulsory basic health insurance) insurance plans. A total of 274 customers agreed to participate. At the end of the study, all participants completed an online questionnaire in which they were asked whether they would participate in an interview. Of the 170 participants who completed the follow-up survey, 83 agreed to participate in interviews, of which 31 reaffirmed willingness after email and 23 were interviewed to achieve data saturation (Corbin & Strauss, Citation1990). The sample consisted of 10 women and 13 men aged between 38 and 64. The participants, both in the digital health intervention and in the interviews, were highly educated and financially well-off compared to the entire Swiss population.
The interviews were conducted by the sociologists in the four months following the end of the six-week digital health intervention and covered six main themes: practical software use; use of data; engagement in tracking; motivations; body; and sociality. The collected data were coded with QSR International’s Nvivo 11 software. An open coding phase, which was conducted sentence-by-sentence, led to the identification of 59 codes. Collaborative axial coding and a focus on user-system interaction as a research question led to the emergence of three relevant themes (Corbin & Strauss, Citation1990).
Results
The first section presents the characteristics of the mHealth intervention. It is followed by three sections that describe what occurred when it was domesticated in everyday life. Second and third sections show how being faithfully represented by the data was a crucial matter for our interviewees and how everyday social rhythms resulted in a renegotiation of daily objectives in the context of the interviews. The last section describes how the participants used their numbers as a means to distinguish between ‘active’ and ‘lazy’ individuals.
What is ALLY? Characteristics of the mHealth intervention
ALLY is the name of a digital coach, which is also known as a conversational agent or healthcare chatbot. It was made available via a smartphone application and had the goal of helping individuals increase their level of physical activity. The objective of the developers is ‘to design behavior-oriented, scalable and self-improving digital health interventions that are more effective and cost-efficient than existing interventions’(Center for digital health interventions, Citation2019). ‘ALLY’ stands for Assistant to lift your level of activity. Specifically, ALLY assigns a personalized daily step objective to participants and uses the notion of a digital coach and a chat-based interface (like in WhatsApp) to deliver the intervention, for example, by brief words of encouragement and other messages to push the participant to attain his/her objective (see ).
Figure 1. The Ally app: daily overview (left), weekly overview (center) and chat interactions with the chatbot (right)
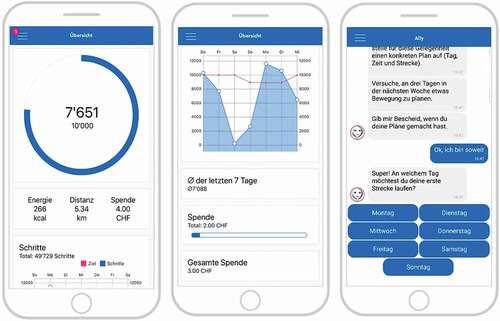
ALLY has characteristics in common with those identified in previous scholarship on mHealth. The first characteristic is a reductionist approach to health and its quantification (Lupton, Citation2014). In the functioning of ALLY, physical activity is reduced to the sole measurement of steps as a metric unit. A second characteristic is the ‘bracketing’ of the social environment and contexts of use (Maturo & Setiffi, Citation2016). ALLY does not consider context (such as the weather, professional life, family, etc.) during the intervention. ALLY sometimes pushed users to reflect on the planning of their daily lives but never took this planning into account to determine daily objectives. Finally, others have noted that a ‘neoliberal ideology that implicitly stigmatizes people who are not capable of meeting the standard definition of “healthy”’ is often embedded in self-tracking applications (Maturo & Setiffi, Citation2016, p. 439). In the ALLY intervention, people who reach their objective received an encouraging message and possibly a financial or charitable reward depending on the participant’s random group allocation (see Kramer et al., Citation2019). The participants who were unable to reach their standardized daily step objective were not rewarded but were encouraged by the chatbot to ameliorate their behavior in the future. The following three sections will elaborate users’ reception of an intervention in which a reductionist approach of physical activity, a ‘bracketing’ of the social context and an emphasis on self-responsibility are embedded.
The reduction of physical activity to steps. A brake on appropriation?
ALLY is a profoundly normative mHealth intervention. Its goal is to compel individuals to persist in a standardized behavior: taking a specific number of steps a day as a proxy to the recommendations for physical activity made by various leading health organizations. Even though they completed questionnaires during the protocol, were invited to give written feedback and had access to a FAQ section that described the rationale of the study, users felt that they could not dispute their daily objectives. They felt unable to negotiate with ALLY. This issue was a consistently appearing topic in the participants’ interviews.
ALLY promised me that I would get a Swiss franc every time I reach 10,000 steps. On some days, ALLY counted wrong! And I always had to confirm. For example, ALLY said, ‘you did 8,000 steps today, ok?’ The only response available was: ‘ok!’ I could not say: ‘no, it is wrong’! So, I made records [the interviewee displays a piece of paper with two columns of numbers]. Look at the numbers. You can keep it; it is only to help. You can see the data of the digital tracker, and you can see that ALLY sometimes counted wrong. And when ALLY makes mistakes, I have to go out and walk for an hour again; the day is not over for me then. (70-year-old man, retired finance counsellor)
According to the participant, the application did not count properly. Of course, we can argue that the participant’s reference (another application) was mistaken. However, the primary problem is that the individual could not negotiate with ALLY: ‘I could not say, “It is wrong”’. This problem was a substantial source of frustration for the participants. This frustration also occurred when the participants wanted the application to consider forms of activity other than steps:
I was skiing all day. In the end, ALLY counts 2,000 steps. So, I say to myself, ‘I did sporty behavior; I did a lot, and in the end, I have 2,000 steps’. So, it did not count and … or when I go swimming. It does not count. Or when I bike, it counts of course, but not steps, another kind of movement. Yes, another kind of movement, and you do not count that the same way. That was really the limitation, I think. Because it only counts steps. Yes, I find it bad. Movement is not always the same; sport is not always the same. Well, some have a bracelet or an armband that measures the pulse or other things. Myself, if I go jogging, I do not take my Smartphone with me; there is a limit between what I measure and what I do. (47-year-old man, business executive)
In this statement, the participant switches from step-counting to physical activity in general, which is a switch that the application was not designed to accommodate (it only counts steps). This problem probably arises from the ALLY dialogues, which tend to use physical activity as a synonym for steps:
ALLY: ‘Physical activity can reduce stress and positively influences well-being!’
ALLY: ‘When you move, you feel better’
(Extracts from ALLY’s statements)
Interestingly, except for one participant, the imprecision or limitation of the measures were not perceived as an argument against the logic of the intervention. One could think that this discrepancy between the measure and actual behavior would be used to undermine the rationale of the ALLY system. However, most participants pointed out the limitations as a way to call for a better measure, which is a behavior also identified in long-term uses (Fritz et al. Citation2014). They were seeking a better measurement, namely, one that would provide a more accurate image of their activities. Basically, they agree to be measured as long as they feel accurately represented by the data, which shows a strong acceptance of the overall self-responsibilizing rationale:
It should at least be representative … I do not care if the insurance sees it. But if someone really wants to see what is happening, then they should know how many beers I drink, for example. If we want to adapt insurance premiums in relation to movement, then all other activities should be integrated, shouldn’t they? (47-year-old man, market analyst)
In these accounts, we witness a mixture of two phases of domestication, specifically, appropriation and conversion. Appropriation focuses on the negotiations and considerations that lead to the acquisition of technologies, whereas conversion focuses on how they are mobilized as part of identities and the presentation of oneself to other people (Haddon, Citation2011). In the process of appropriation, our participants resisted the reductive representation of their physical activity. The main reason for this resistance is that this representation, according to them, did not fit their actual behavior. The appropriation of the technology was not fully successful because the conversion, the presentation of oneself to other people (and reflexively to oneself), did not fully fit users’ expectations. Nevertheless, this did not lead to disengagement. Appropriation was more difficult, but we cannot say that it was unsuccessful. Most users either stuck to the standard use even though they were frustrated or used another device to measure other physical activities. ALLY was thus integrated in users’ everyday lives. The two prototypical everyday uses observed were ‘surveillance’, in which people check if they comply with the norm, and ‘routinization’, in which people try to use ALLY as a trigger to change what they identify as an inactive lifestyle (Pharabod et al., Citation2013). This second type of use successfully prompted small changes such as not taking the elevator, doing ‘active breaks’ at work or avoiding public transports on small distances, at least for the duration of the protocol and up to the interviews (maximum four months after the end of the protocol).
The ‘bracketing’ of everyday life as a limit to objectivation
The participants experienced the objective as an element of everyday life. However, the metric was developed in relation to physiological and medical standards (Tudor-Locke et al. Citation2008). These standards are applied independently of what is typically termed the ‘social’ part of life. Whether it rains or whether it is the weekend or mid-week does not alter the physiological standard that underlies step-counting. However, once the recommendation enters the domestication process, the focus changes from physiology to the individuals as social beings.
When domesticating the step objective as part of everyday life, the participants understood movement (e.g., steps) as a quantity that could be viewed in terms of a balance sheet, as if more movement here could compensate for a lack of movement there. Their idea was that at the end of the week, the sheet should be balanced:
I wish I had a global objective for the week. Because sometimes I could not reach 10,000 on a particular day, but then on Saturday, I would go for a long walk, and so, I did a lot of steps. So … I thought it was a bit boring to have a daily objective. (64-year-old man, retired insurance counsellor)
For this interviewee, a weekly objective would solve the problem that it is occasionally difficult to reach a daily step goal. The reasons evoked in the interviews for not reaching a daily step goal were taking care of children, work-related meetings, having another physical activity scheduled such as swimming or skiing and cold weather or rain. In the domestication process, the incorporation phase denotes the necessity for the technology to find a place in the temporal routines of everyday life (Hynes & Rommes, Citation2005). Here, the temporal standard embedded in ALLY was confronted with users’ social rhythms. This resulted in difficult incorporation. Some users offered a potential solution based on their idea that weekdays and weekends are different temporal spaces. They considered the weekend as a period of freedom to move more or move less and the weekdays as a period for controlled activity and discipline:
Yeah, well there was this weekend day when I made only 8,000 steps, but I did not do more to reach the objective because I thought during the week I already did enough, yes. (41-year-old woman, nurse)
It is as if the responsibility for physical activity was applicable only on working days and as if weekends were days off from the step-counting discipline:
I think that here the problem is everyday life; do we move enough? On weekends, either it is laziness and we do nothing, or we go for a walk and so we naturally have an enormous step count. But that is not everyday life; everyday life is Monday to Friday! (56-year-old man, senior manager)
This tendency to reinterpret the objective as a weekly objective prevailed for our interviewees. It is not unproblematic because physiological processes (at least when mediated by biomedical sciences) do not rely on the same temporality as the users’ daily lives (Pantzar et al. Citation2017). This reinterpretation interestingly results in the subject expressing a need that differs from the ‘needs’ (mediated by science and technological design) expressed by their physiological constituents.
Conversion and the morality of steps
As we have seen, it was important for the users that the step-counting data faithfully represented their activity. However, this representation of the self should be understood as part of a larger picture. It is a representation that fits into a system of mutualized health. That is, in our users’ perspective, everyone must practice physical activity because it acts on ‘health’ and because all citizens pay for a mutualized health system. Thus, for our users, physical activity is understood as part of an individual’s duty. This idea of measurement as a social responsibility has been identified in public discourses (Lupton, Citation2012) and, as stated before, is embedded in ALLY. In our interviews, physical activity as a citizen responsibility was first expressed in the words of the users who think that they do ‘enough’. Thus, it was framed as ‘others should do more’:
I have to specify that movement is very important for me. I think that it would be better if more people did some because … yes, it is a good thing to move and to practice active … health promotion. (70-year-old man, retired finance counsellor)
Again, the participants are reasonable regarding the intervention’s objectives. The scientists who developed ALLY expressed the same idea: ‘A great proportion of the world’s disease burden is caused by behaviors, such as diet behavior, smoking or physical inactivity’ (Kramer et al., Citation2019).
I think that ALLY can mostly help people who do not have this consciousness and who are maybe lazy. So that they might say: well, I did 7,000 steps; I will try to go out for a little walk so that ALLY is happy (laugh). I think that it would be a good thing. (41-year-old woman, nurse)
This ‘active’ interviewee refers to inactive participants as ‘lazy’. This term appeared with surprising frequency in the interviews, and ‘laziness’ emerged as one of the largest coding categories. Physical activity was understood in opposition to laziness by the participants. This opposition between physical activity and laziness was mostly dominant in the self-perceived ‘inactive’ interviewees and framed their understanding of themselves and the step objective. The necessity for people to take care of themselves both individually and as a part of a mutualized health system, notably through step-counting, was a preeminent idea for the interviewees:
Because our health system is sick … If we can create that kind of application that can be used on a day-to-day basis … If it allows people to see how much they move, what they ingest, healthy, unhealthy. It is a question of equilibrium; not many things are only healthy or unhealthy? If it helps people and considering that the vast majority of people are in poor health condition … I think, if it makes them healthier, I think it is a good thing. That is also why I took part. (42-year-old woman, business consultant)
In the participants’ accounts, the step objective is reinterpreted in moral terms. The number of steps is transformed into a way to measure laziness and, by extension, good citizenship. As stated before, the moral implications were already embedded in ALLY, both in the objective-reward logic and in some of the chatbot dialogues. However, they were never expressed via morally laden terms such as ‘laziness’ or ‘unhealthy’. These results indicate that this part of the appropriation phase was successful. Appropriation refers to the transformation of the technology into something that is desirable for the individual (Hynes & Rommes, Citation2005). Here, all users passed the appropriation phase, which started when they received the invitation to participate in the intervention. They were able to match their vision of health and responsibility to ALLY’s vision. It is not surprising that none of our interviewees were opposed to this vision because the interviewees who were opposed probably did not engage with the protocol and were unable to imagine ALLY as an ‘object of desire’.
Conversion is a phase of domestication in which the users make the personal meaning they created public. In the context of the interview, that is, under the attention of the interviewer, users converted the objectives into the moral language of ‘active-lazy’. It is difficult here to disentangle the role of ALLY in the process. It seems very likely that users already had this moral vision of physical activity before they used ALLY. It also seems very likely that the similarity between their vision and ALLY’s rationale was a big part of why they engaged in the protocol. But did ALLY play a transformative role? Encountering the ‘healthist’ quotes of ALLY and a quantified proxy for physical activity on a daily basis is likely to reinforce users’ ideas and taint them with reductionism and quantification. This process is noticeable in some of our cases:
I watch and ‘hop’ I did 5,000, it is already an indicator: I have been lazy. If I see 10,000, well I know I have done better. The threshold for me is 8,000, over is an active day, under is a lazy day. (31 years old, medical engineer)
In this example, the moral understanding of physical activity – which certainly existed prior to the intervention – expressed by the interviewee has been transformed by the use of ALLY. The moral understanding has been re-formulated in the terms of ‘steps as a daily objective’. A re-formulation which denotes the influence of ALLY. The formulation of the moral understanding would probably be different if a technology with other specificities had been used (for example if ALLY had a focus on intensity or on subjective pleasure and not on numbers of steps). In this case, the conversion, that is the way people recast the meaning of the technology in their moral terms seems to have been ‘mediated’ by the particularities of ALLY as a technical system. ALLY-like apps are technological entities that ‘transform, translate, distort, and modify the meaning or the elements they are supposed to carry’ (Latour, Citation2007, p. 39).
Discussion
Digital health interventions are sometimes described as invisible or silent manipulators in the sense that they preselect or choose for the individual (Cheney-Lippold, Citation2011). Our empirical study led to a nuanced view of this assertion. We identified three characteristics embedded in the application, namely, a reductionist approach of physical activity, a ‘bracketing’ of social context and a self-responsibilizing ideology. Regarding the first two characteristics, our participants tended to force ALLY out of its planned trajectory. ALLY’s incapacity to adapt to the needs of our participants led them to conclude that the application exhibited a ‘lack of nuance or contextual understanding’ (Willson, Citation2017). Once applied to people’s lives, the code behind ALLY was limited by its own functioning, which ‘reduces people to the properties that are relevant to a given step of the algorithm’ (Totaro & Ninno, Citation2016). In our circumstances, these ‘steps’ were, ironically, the reduction of physical activity to steps and the exclusion of social context. Even though the appropriation was eventually successful, the negotiations that we observed offer a counterpoint to the idea that users trust technologies more than themselves and highlights the work and circumstances needed for data to ‘become unquestioned, normalized and invisible’ (Willson, Citation2017, p. 12).
Nevertheless, the neoliberal ethos embedded in ALLY fitted with users’ expectations. One group of our interviewees considered that they were ‘active and responsible individuals’ because they easily reached their objectives. The other group considered themselves to be ‘lazy’ and viewed step-counting as part of their effort to become active and reach the normative objective. These results are consistent with the idea that health as a social practice can be a way to affirm a specific ethos and strengthen social distinctions. The idea that a responsible individual should be physically active to maintain his or her good health was dominant in our sample. The technical specificity of ALLY and the assignment of a daily step objective linked to a reward and supported by a chatbot were thus consistent with users’ ethos. The mHealth intervention fosters a quantifiable and actionable materialization of this ethos, which objectifies it and – in certain cases – is likely to transform or reinforce it. It is important to underline the importance of the step-counting measurement apparatus itself. It uses a specific mode (reduction and quantification) of these distinction and surveillance processes and crudely brings them to the individuals’ attention.
The context of use also plays a role in the domestication process. It is actively interpreted and recast by users. In our case, the context involved an insurance company that currently offers a step-counting program (different from ALLY). This program financially rewards customers when they reach their daily step objective.Footnote7 For now, such selective pricingFootnote8 is legally restricted to supplementary insurance plans in Switzerland. As we have shown, applications like ALLY are likely to normalize such practices.
It is important to note that not all sociocultural groups were represented in this study. The domestication of the mHealth intervention that we documented reflects the values of a specific social group (our sample) and promotes their particular definition of ‘health’. The group comprised highly educated and financially well-off individuals. We acknowledge that devices such as ALLY can incite certain users to conform to ‘healthist’ forms of citizenship and thus increase their physical activity. However, these devices may create barriers for people who do not share the same values. The domestication of ALLY and the engagement in the intervention is correlated with an ethos that may be connected to a certain social position. This exemplifies the idea that the way that people domesticate technologies is influenced – among many other things – by socioeconomic factors (Hynes & Rommes, Citation2005). As noted by scholars, the diffusion of practices similar to ALLY could lead to the progressive exclusion and marginalization of citizens who have not interiorized these values (Halford & Savage, Citation2010). Health policies should not be blind to this potential for an opposing social reception of self-tracking tools. For certain sociocultural groups, which may paradoxically be the purported main target of health promotion, self-tracking could contradict the aims of a public policy that supports physical activity as a way to prevent disease and promote health.
Our research triggers another question: should recommendations and mHealth interventions consider users’ social rhythms? Should the next version of ALLY suspend counting on weekends? Should it adopt a weekly count? Should it set lower objectives on rainy days? Our results suggest that the integration of the ‘social rhythms’ (Pantzar et al., Citation2017) in physical activity guidelines and by extension in the technologies that mediate them may facilitate their incorporation in everyday life.
Conclusion
In this article, we documented the emergence of a self-tracking practice, co-constructed by users and a technology. Our discussion might suggest that participants and technology are fixed entities. Nevertheless, the application is likely to evolve due to participant feedback, and users are likely to be transformed by the use of the application. What we observed is thus a moment in the dynamic co-construction of a self-tracking practice. The users, their values, their social position and the technical features of the mHealth intervention thus preexist and constrain the domestication process as much as they are transformed and reworked by it (Halford & Savage, Citation2010). It should be noted that our work and this article are also likely to contribute to the shared construction of the mHealth intervention practice (notably through the feedback that it created for designers and the discussions that it triggered with users).
Based on our analysis of an mHealth intervention through user discourse, we offer the following conclusions. Although scientists recognize that numerical recommendations, such as ‘10,000 steps’, should be ‘assistive rather than prescriptive’ (Tudor-Locke et al., Citation2008), such recommendations are often understood in a prescriptive manner. The domestication of a mHealth intervention is tightly linked to the specific design of the technology and to the social values of its users. In the ALLY case, there was a strong alignment between the technical features of the technology and the users’ social values which led to an overall acceptance of the technology. In this context, we discovered how users expressed the normativity of measurements through their own moral vocabulary. This suggests that populations who do not share those values are likely to fail the early stages of appropriation, that is, be unable to construct the intervention as an ‘object of desire’. In a public health context, this means that the intervention will probably not affect those individuals, although specific research on non-users would be needed to document this process. We also documented instances in which the domestication process was slowed, notably when users encountered the embedded reductive nature of physical activity or the ‘bracketing’ of the social context.
Our findings indicate that additional qualitative empirical research on mHealth is required. The domestication process seems to be dependent on the sociocultural profile of the user and on software and hardware specificity. Only a detailed description of users and technologies can lead to an understanding of the domestication process. We understand that our position might be considered to encourage or participate in the neoliberal paradigm discussed in the introduction. Our claim is that in a space often defined by opposites, i.e., enthusiasts and critics (Del Rio Carral et al. Citation2016), it is important to have middle-ground empirical research that may facilitate fruitful communication among social scientists, engineers and public-health policy makers (Neff et al. Citation2017). We also hope that such research can lead to the production of applications that take a different approach to self-tracking than the current mainstream in the market.
Disclosure statement
Bastien Presset (principal investigator) and Fabien Ohl are researchers at the Institute for Sport Sciences of the University of Lausanne (ISSUL). Their studies are funded by the canton de Vaud (public funds). Jan-Niklas Kramer and Tobias Kowatsch are affiliated with the Center for Digital Health Interventions (CDHI, www.c4dhi.org), a joint initiative of the Department of Management, Technology and Economics at ETH Zurich and the Institute of Technology Management at the University of St.Gallen, which is funded in part by the Swiss health insurer CSS. The CSS insurance supported recruitment but had no role in the other aspects of the study design, data analysis and interpretation or in reviewing and approving the manuscript for publication. Tobias Kowatsch is also the co-founder of Pathmate Technologies, a university spin-off company that has used the open source MobileCoach platform, which was also used to build the ALLY smartphone app. However, Pathmate Technologies is not involved in the ALLY intervention. No other conflicts of interests are declared.
Additional information
Funding
Notes
1. https://www.fda.gov/downloads/MedicalDevices/DigitalHealth/UCM568735.pdf (accessed 14.08.18).
2. https://www.gov.uk/government/publications/medical-devices-software-applications-apps (accessed 28.06.18).
3. https://www.iges.com/clients/health/forschungsergebnisse/2016/health-apps-ii/index_eng.html (accessed 28.06.18).
5. whttps://ww.e-health-suisse.ch/fr/mise-en-oeuvre-communautes/activites-ehealth/mhealth.html (accessed 28.06.18).
6. https://www.grandviewresearch.com/industry-analysis/mhealth-app-market (accesssed14.08.18).
7. Customers can earn 0.20 CHF/day if they reach 7,500 steps or 0,40CHF/day if they reach 10,000 steps.
8. The insurance perspective is that the program only offers bonus and that the premiums remain the same. In that perspective ‘financial rewards’ may be more accurate than ‘selective pricing’. On the other end, interviewees perceived the program as ‘selective pricing’ and if one considers the overall financial balance an ‘active’ customer has, indeed, paid a lower premium (the usual premium minus the financial rewards).
References
- Adams, M. L. (2018). Step-counting in the “health-society”: Phenomenological reflections on walking in the era of the Fitbit. Social Theory & Health, 17(1), 109–124.
- Akrich, M. (1997). The description of technical objects. In W. E. Bijker & J. Law (Eds.), Shaping technologies/building society. Studies in sociotechnical change (pp. 205–224). Cambridge, MA: The MIT Press.
- Audétat, M. (Ed.). (2015). Sciences et technologies émergentes: Pourquoi tant de promesses? Paris: Hermann.
- Berker, T. (Ed.). (2006). Domestication of media and technology. Maidenhead: Open University Press.
- Carter, S., Green, J., & Speed, E. (2018). Digital technologies and the biomedicalisation of everyday activities: The case of walking and cycling. Sociology Compass, 12(4), e12572.
- Center for digital health intervention. (2019). Homepage. Retrieved from https://www.c4dhi.org/
- Cheney-Lippold, J. (2011). A new algorithmic identity: Soft biopolitics and the modulation of control. Theory, Culture & Society, 28(6), 164‑181.
- Corbin, J. M., & Strauss, A. (1990). Grounded theory research: Procedures, canons, and evaluative criteria. Qualitative Sociology, 13(1), 3‑21.
- Crawford, R. (1980). Healthism and the medicalization of everyday life. International Journal of Health Services, 10(3), 365–388.
- Del Rio Carral, M., Roux, P., Bruchez, C., & Santiago-Delefosse, M. (2016). Beyond the debate on promises and risks in digital health: Analysing the psychological function of wearable devices. International Journal of Psychological Studies, 8(4), 26–37.
- Fotopoulou, A., & O’Riordan, K. (2017). Training to self-care: Fitness tracking, biopedagogy and the healthy consumer. Health Sociology Review, 26(1), 54‑68.
- Fritz, T., Huang, E. M., Murphy, G. C., & Zimmermann, T. (2014). Persuasive technology in the real world: A study of long-term use of activity sensing devices for fitness. Proceedings of the 32nd Annual ACM Conference on Human Factors in Computing Systems - CHI ’14 (pp. 487–496), Toronto, Canada.
- Haddon, L. (2007). Roger Silverstone’s legacies: Domestication. New Media & Society, 9(1), 25–32.
- Haddon, L. (2011). Domestication analysis, objects of study, and the centrality of technologies in everyday life. Canadian Journal of Communication, 36(2), 311–323.
- Halford, S., & Savage, M. (2010). Reconceptualizing digital social inequality. Information, Communication & Society, 13(7), 937‑955.
- Harries, T., & Rettie, R. (2016). Walking as a social practice: Dispersed walking and the organisation of everyday practices. Sociology of Health & Illness, 38(6), 874–883.
- Hirsch, E., & Silverstone, R. (1992). Consuming technologies: Media and information in domestic spaces. London: Routledge.
- Hynes, D., & Rommes, E. (2005). “Fitting the internet into our lives”: What IT courses have to do with it. In T. Berker, M. Hartmann, Y. Punie, & K. Ward (Eds.), Domestication of media and technology (pp. 125–144). Maidenhead: Open University Press.
- Kramer, J.-N., Künzler, F., Mishra, V., Presset, B., Kotz, D., Smith, S., … Kowatsch, T. (2019). Investigating intervention components and exploring states of receptivity for a smartphone app to promote physical activity: Protocol of a microrandomized trial. JMIR Research Protocols, 8, 1.
- Latour, B. (2007). Reassembling the social: An introduction to actor-network-theory. Oxford: Oxford Univ. Press.
- Lupton, D. (2012). M-health and health promotion: The digital cyborg and surveillance society. Social Theory & Health, 10(3), 229–244.
- Lupton, D. (2013). Quantifying the body: Monitoring and measuring health in the age of mHealth technologies. Critical Public Health, 23(4), 393–403.
- Lupton, D. (2014). Apps as artefacts: Towards a critical perspective on mobile health and medical apps. Societies, 4(4), 606–622.
- Lupton, D. (2017). Self-tracking, health and medicine. Health Sociology Review, 26(1), 1–5.
- Lupton, D. (2019). ‘It’s made me a lot more aware’: A new materialist analysis of health self-tracking. Media International Australia, 171(1), 66–79.
- Maturo, A., & Setiffi, F. (2016). The gamification of risk: How health apps foster self-confidence and why this is not enough. Health, Risk & Society, 17(7–8), 477–494.
- Neff, G., Tanweer, A., Fiore-Gartland, B., & Osburn, L. (2017). Critique and contribute: A practice-based framework for improving critical data studies and data science. Big Data, 5(2), 85–97.
- Oudshoorn, N., & Pinch, T. (2008). User-technology relationships: Some recent developments. In E. J. Hackett, O. Amsterdamska, M. Lynch, & J. Wajcman (Eds.), The handbook of science and technology studies (3rd ed., pp. 541–565). London: MIT Press.
- Pantzar, M., Ruckenstein, M., & Mustonen, V. (2017). Social rhythms of the heart. Health Sociology Review, 26(1), 22‑37.
- Pharabod, A.-S., Nikolski, V., & Granjon, F. (2013). La mise en chiffre de soi: Une approche compréhensive des mesures personnelles [Measuring oneself: A comprehensive approach of personal measures]. Réseaux, 177(1), 97–129.
- Sharon, T. (2017). Self-tracking for health and the quantified self: Re-articulating autonomy, solidarity, and authenticity in an age of personalized healthcare. Philosophy & Technology, 30(1), 93–121.
- Silverstone, R., Hirsch, E., & Morley, D. (1992). Information and communication technologies and the moral economy of the household. In E. Hirsch & R. Silverstone (Eds.), Consuming technologies: Media and information in domestic spaces (pp. 13–28). London: Routledge.
- Sorensen, K., . H. (2006). Domestication: The enactment of technology. In T. Berker, M. Hartmann, Y. Punie, & K. Ward (Eds.), Domestication of media and technology (pp. 40–57). Maidenhead: Open University Press.
- Totaro, P., & Ninno, D. (2016). Algorithms and the practical world. Theory, Culture & Society, 33(1), 139‑152.
- Tudor-Locke, C., Hatano, Y., Pangrazi, R. P., & Kang, M. (2008). Revisiting ‘How many steps are enough?’ Medicine & Science in Sports & Exercise, 40(7 Suppl), 537–543.
- Willson, M. (2017). Algorithms (and the) everyday. Information, Communication & Society, 20(1), 137–150.
