?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Purpose: Early detection of breast cancer-related lymphedema through simple self-monitoring techniques may lead to early treatment and improved outcomes. Methods: Prospective study of circumference measurements at four time points before, during, and after adjuvant chemotherapy with docetaxel, doxorubicin, and cyclophosphamide. Volume was calculated using the 10-cm interval circumference measurement method (reference test) and percentage difference between arms, for volume and circumference, was determined. First, the most valid single measurement location was determined by calculating Pearson’s correlation coefficient relative to the reference test. Second, to evaluate the responsiveness to change over four time points, outcomes of the selected single measurement and the reference test were analyzed by repeated-measures ANOVA. Third, area under the curve (AUC) was used to determine the optimal sensitivity and specificity of the selected single measurement site (index test). Relationship between lymphedema (yes/no) and heaviness and swelling (yes/no) was analyzed using phi-coefficient. Results: The measurement point 30 cm proximal to the styloid process showed the highest correlation with percentage difference in total arm volume (r = 0.80) and detected increased percentage difference between arms after treatment. Analyses showed high accuracy (AUC = 0.94; 95% CI 0.90–0.99) and good sensitivity (0.85) and specificity (0.85) using a cutoff score of 4% circumference difference between arms at this location. A moderate correlation between feelings of heaviness and swelling to lymphedema was observed (rφ = 0.64). Conclusions: Circumference difference between arms of 4% measured at 30 cm proximal to the styloid process can be used as a surveillance site for further monitoring of patients at risk for lymphedema and may contribute to early diagnosis. Feelings of heaviness or swelling have moderate relationship with lymphedema, which needs to be confirmed in clinical practice.
Introduction
Lymphedema in the arm is a chronic disease with swelling and impairments in function, resulting in limitations in activities in daily life (Hidding et al., Citation2014; Pinto et al., Citation2013; Viehoff et al., Citation2015). Detecting possible development of lymphedema in patients with breast cancer at risk is important, as early detection of adverse effects of breast cancer treatment and consequently early intervention can improve health outcomes and cost-effectiveness of care (Schmitz, DiSipio, Gordon, and Hayes, Citation2015; Stout et al., Citation2011). Internationally, a volume difference between arms of ≥10% is considered as a cutoff point to diagnose lymphedema (Moffat, Doherty, and Morgan, Citation2006). Furthermore, earlier research showed that heaviness and swelling as reported by the patient are highly correlated with the diagnosis of lymphedema based on volume measurements (Armer et al., Citation2008; Czerniec et al., Citation2010). Water volumetry via water displacement in a water tank and tape measurement using multiple measurement points are both reliable and feasible instruments to monitor swelling (Hidding et al., Citation2016), but these measurements are burdensome for the patient and the health-care provider in terms of the time spent on the measurements. In general, differences between affected and unaffected arms are described in absolute or in percentage difference in circumference (in centimeters) or volume (in milliliters). As absolute values in centimeters or milliliters are less valid and depend on body composition (Ancukiewicz et al., Citation2011), percentage volume difference between arms is considered the gold standard (Hidding et al., Citation2016). However, centimeter difference is easier to interpret for the patient than percentage difference.
To support patients and clinicians in monitoring development of lymphedema in patients at risk for arm lymphedema, ideally the patient her/himself would be instructed to measure swelling and monitor the development of lymphedema in a simple way. Therefore, measuring circumference with a tape measure at a single measurement site would be preferred. We hypothesized that it should be possible to identify patients at risk of lymphedema who need to consult a health-care provider for further diagnosis by detecting a clinically relevant difference in circumference between arms using tape measurements at an appointed location, combined with feelings of heaviness and swelling.
It is unknown which measurement locations are most closely associated with percentage difference in total arm volume and whether the psychometric properties, particularly those related to validity of a single measurement site, are sensitive and specific enough to be used as a monitoring instrument. Therefore, this study focuses on the following research question: Is it possible to detect lymphedema in the arm using bilateral arm circumference measurement at a single site on each arm? The following hypotheses are formulated: (1) A valid single measurement location can be identified when compared to the reference test; (2) Percentage difference in total arm volume (calculated from circumference measurements) as well as the difference in circumference at the most valid single measurement can detect changes over time; (3) For the most valid single measurement, a clear cutoff point can be identified for detecting lymphedema, with good sensitivity and specificity; and (4) Lymphedema is related to feelings of heaviness and swelling.
Methods
Participants
Patients with tumor stage I–III and scheduled for six-cycle adjuvant cytotoxic treatment with docetaxel, doxorubicin, and cyclophosphamide (TAC) at the University Medical Center were invited by a specialized nurse (WB) to participate in this prospective study. Patients were included between August 2011 and January 2015. Surgery, as well as radiotherapy if indicated, was completed, at the start of the TAC treatment. Exclusion criteria were recurrence or second cancer and insufficient understanding of Dutch language for filling out the questionnaire.
Patients were measured at four time points: before the start of cycle 1 (T0), cycle 2 (T1), and cycle 4 (T2) and one month after completion of the 6th cycle (T3). All participants signed informed consent before the first measurement. Formal ethical approval was waived by the Medical Ethical Committee of the University Medical Center and registered under number 2011/234.
Measurements
Circumference measurements were performed with a tape measure using the 10-cm interval circumference measurement method, starting at the ulnar styloid process. Both arms were measured. Total limb volume was calculated from circumference measurements, using the conical formula, and differences between arms were calculated as percentage difference (Hidding et al., Citation2016). Total limb volume measurement was the reference test used for assessment of validity. An arm volume difference of ≥10% was considered as lymphedema. For all used measurement sites, differences between both arms were calculated in percentage as well as in absolute difference in centimeters (affected limb − unaffected limb). Tape measurement is a reliable measurement instrument, with excellent intra- and inter-test–retest reliability (intraclass correlatie coëfficiënt (ICC) 0.99 and 0.98, respectively) and good convergent validity (0.80–1.00) compared with water volumetry (the gold standard) when a standardized protocol is used and both measurements are calculated to percentage difference (Hidding et al., Citation2016). Measurements were performed by three physiotherapists (CB, RD, and JH), experienced in measuring circumferences. Investigators were blinded for results of prior measurements. The measurement protocol was described in detail to reduce measurement error and, if possible, patients were measured by the same therapist throughout the whole study. During measurement, the patient was sitting, with the hand supported on a pillow. Position of the shoulder was in 90° anteflexion with the elbow extended.
Scores of heaviness and swelling were derived from the Lymph-ICF questionnaire (Devoogdt et al., Citation2011). The Lymph-ICF is a quality of life questionnaire developed for patients with lymphedema, with 29 items over five domains: physical function, mental function, household activities, mobility activities, and social activities. Measurement properties of the Lymph-ICF have been studied before and showed a fair to excellent reliability for all scales (r = 0.65–0.93) (Devoogdt et al., Citation2011). Each item can be scored between 0 and 100 on a horizontal line of 100 mm. A higher score means more patient complaints on that item (i.e. heaviness and swelling): scores under 25 indicate minor complaints and scores from 25 reveal marked problems (Devoogdt et al., Citation2011).
Statistical analysis
Descriptive analyses were used to describe patient characteristics and treatment characteristics. For statistical analysis, SPSS version 23 was used. To determine the most valid single measurement site, correlation between the reference test (total arm volume) and the difference in circumference measurement (percentage and absolute difference) was determined using Pearson’s correlation coefficients. Correlations between measurements were interpreted as follows: r > 0.75 is excellent; r > 0.40–0.75 is fair to good. ICCs were interpreted as follows: r > 0.90 is high; r > 0.80 is good (Fleiss, Levin, and Paik, Citation2003). We assumed r > 0.75 is sufficient to indicate a single measurement site valid when compared to percentage difference of total volume (Fleiss, Levin, and Paik, Citation2003).
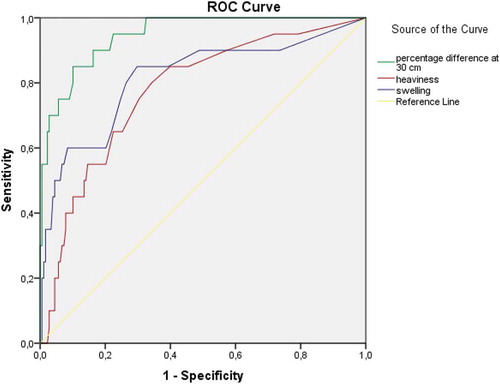
To determine responsiveness to changes between time points T0–T3 in percentage difference in total volume and in outcome of the most valid single measurement, repeated-measures ANOVA was used. To determine the optimal cutoff point of the most valid single measurement, sensitivity and specificity were estimated and a receiver-operating characteristic (ROC) curve was constructed, comparing the most valid single measurement, heaviness, and swelling with the reference test (percentage volume difference ≥10% yes or no). An area under the curve (AUC) over 0.80 was considered as representing high accuracy and over 0.90 as excellent accuracy. In a second step, the optimal cutoff point was compared to the smallest detectable change at all time points.
To determine the strength of the relationship between lymphedema and feelings of heaviness and swelling as a clinical decision tool for development of lymphedema, percentage difference in total arm volume and feelings of heaviness and swelling were dichotomized. Lymphedema was defined as ≥10% volume difference between both arms using the 10-cm interval circumference measurement method and swelling and heaviness as a score ≥25 on the Lymph-ICF questionnaire. For analysis, a phi-coefficient was calculated. A p-value of <0.05 (two-sided) was considered statistically significant. Sensitivity and specificity >0.80 were considered clinically relevant.
Results
A total of 74 patients scheduled for adjuvant TAC were invited to participate in the study. Fifty-one patients consented to participate, of which 48 completed all measurements. Two patients switched treatment to FEC (5-fluorouracil, epirubicine, and cyclofosfamide) after the third and fourth cycles. One patient was treated without docetaxel in the fourth cycle of TAC and stopped after this cycle. Mean age of the included patients was 51.3 years (range 30–68; standard deviation 8.5). Patient and tumor characteristics of these patients are summarized in . All data provided by the patients were analyzed. In total, 199 measurements were analyzed.
Table 1. Patient, tumor, and treatment characteristics at baseline.
Associations between percentage difference in total arm volume and single measurement sites are summarized in and visualized in . When differences between both arms were calculated to percentage difference, r is ranged between 0.28 for the 0-cm measurement location and 0.80 for the 30-cm measurement location. When differences were calculated as centimeter difference, r is ranged between −0.04 for the 10-cm measurement location and 0.71 for both the 20 and 40-cm measurement locations. The 30-cm measurement location, with differences between both arms calculated in percentage difference, was indicated as the most valid measurement point.
Table 2. Associations between percentage difference and centimeter difference of all measurement points and total arm measurement.
Figure 1. Scatterplot of percentage difference of total arm volume and percentage difference at the 30-cm measurement site.
A significant increase in percentage difference in total arm volume was observed at T3 compared to T0, as well as in percentage difference at the 30-cm measurement location at T3 compared to T1 (p < 0.05). At T0–T2, mean percentage difference of the circumference measurements ranged from 1.3% to 1.7%, increasing to 3.0% at T3. Before a significant increase was observed, the smallest detectable change ranged between 0.73% and 0.78% ().
Table 3. Circumference measurements with tape measured with 10-cm distance intervals and circumference measurements of the 30-cm location, calculated as percentage difference between affected and unaffected upper extremity, at baseline before chemotherapy (T0), during chemotherapy before the second (T1) and fourth cycles (T2), and one month after completion of chemotherapy (T3).
Analysis showed high accuracy with an AUC of 0.94 (95% CI 0.90–0.99; p < 0.001) for the single measurement at 30 cm (). The preferred cutoff point as indication for lymphedema appeared to be 4% difference, with a sensitivity and specificity of 0.85 (). A statistically significant relationship was observed between lymphedema and heaviness and swelling (rφ = 0.64, p < 0.001).
Table 4. Area under the curve (AUC) for percentage difference of a single measurement location at 30 cm proximal of the styloid process and feelings of heaviness and swelling compared to total volume, calculated with 10-cm intervals.
Discussion
A good association was observed between measurements at 30 cm proximal to the styloid process and percentage difference of total volume when differences in centimeters between arms were calculated in percentage difference, with high accuracy and good sensitivity and specificity. Measurements over time showed the single measurement site being responsive to change. The relationship between swelling and heaviness with lymphedema was moderate.
The first hypothesis that a valid single measurement site can be indicated comparing single measurements with the reference test is accepted. A good association between the reference test and percentage difference between arms at the 30-cm measurement location was observed. In contrast, using absolute difference in centimeters, fair associations were observed with percentage difference in total arm volume. The second hypothesis that percentage difference of total volume as well as percentage difference of the most valid single circumference measurement can detect changes over time changes was also accepted. It can be stated as well that percentage difference of total volume as of a single measurement is sensitive to change over time. The third hypothesis that for the most valid single measurement a clear cutoff point can be identified for development of lymphedema, with good sensitivity and specificity, was accepted as well. Using a cutoff point of 4% at the 30-cm site, sensitivity and specificity in relation to percentage difference of total arm volume are good. The fourth hypothesis that lymphedema is related to feelings of heaviness and swelling is accepted. However, as only a moderate association was observed, and only a part of the patients with lymphedema reported heaviness and swelling, This finding, a cut-off score of 4.0% difference between arms, has to be investigated,
The single measurement point at 30 cm proximal to the styloid process, calculated in percentage difference, appears to be a good control point for surveillance of patients at risk for lymphedema. In this study population, the cutoff score of the single measurement for further diagnosis of possible development of lymphedema was beyond the smallest detectable change. A cutoff score of 4.0% difference in circumference between affected and unaffected arm can be indicated as a decision tool for the patient to consult a health-care provider for further analysis in relation to development of lymphedema. This finding, a cut-off score of 4.0% difference between arms, has to be investigated, following patients at risk for developing lymphedema measuring by themselves over a longer time period. Even more, in a population of patients with lymphedema, outcomes may be different. Although a single measurement saves time, attention has to be given to the following aspects. Measurements in this research were performed by experienced therapists. For a patient, measuring by her/himself, it is more difficult to find the same location at every measurement time and in both upper extremities. Measurements have to be performed at a fixed daytime point, preferably early in the morning, as arm volume can change during daytime and can change as a result of activities during the day. Even more, during warm weather, volume can increase as well. Therefore, the patient needs to be instructed carefully. To facilitate measurements by the patient her/himself and for accurate measurements, preferably a tape measure with a locking mechanism should be used.
Dominance may play a role in volume differences between arms. One study showed no effect on volume difference in relation to surgery on dominant or nondominant side (Smoot et al., Citation2014). In our study, surgery on the dominant side showed no effect on percentage volume differences as well (data not shown); therefore, control for dominance seems not necessary. As earlier studies reported volume differences between arms, with the dominant arm being 2.2–3.0% larger (Adriaenssens et al., Citation2013; Dylke et al., Citation2012; Gebruers, Truijen, Engelborghs, and De Deyn, Citation2007; Smoot et al., Citation2014), too small cutoff points (less than 3%) may overestimate signs of development of lymphedema. These findings are in line with the smallest detectable change as described above.
Both our study and the study by Smoot et al. (Citation2014) confirmed the 30-cm location as the measurement site with the highest accuracy. In contrast to our study, a cutoff point of 200 ml was used for diagnosis of lymphedema and ≥2 cm circumference difference between both arms as cutoff point for a single measurement site (Smoot et al., Citation2014). The AUC in our study is higher than in the study of Smoot et al. (Citation2014) where patients with and without lymphedema were included and measured only once. In their study, a high specificity was chosen (0.94; 95% CI 0.86–0.98), resulting in a far lower sensitivity (0.36; 95% CI 0.25–0.48) than our ROC curve showed. This can be explained by findings of our study, indicating that percentage difference between arms is more sensitive than centimeter difference. Furthermore, including patients with lymphedema as well as without lymphedema may play a role in difference in outcomes between the studies, which has to be confirmed in future studies.
In relation to self-measurements by the patient, reliability of tape measurement was reported in earlier studies, both using 10-cm interval measurements (Foroughi et al., Citation2011; Mori, Lustman, and Katz-Leurer, Citation2014). One study reported a high intrarater reliability of tape measurements by the patient (ICCintra > 0.97) (Mori, Lustman, and Katz-Leurer, Citation2014). Another study compared self-measurement by the patient with tape measurement by a therapist and reported inter-rater reliability of dominant and nondominant arm, with good to high reliability at the 30-cm location (ICCinter 0.88 and 0.91, respectively) (Foroughi et al., Citation2011). These findings indicate that self-measurement using a tape measure is quite probably a reliable method for self-monitoring of swelling by the patient.
For the patient as well as the clinician, a tool that registers outcomes of measurements over time would be helpful. In a simple way, the outcomes can be registered using a spreadsheet. Nowadays, most people use their mobile phone for many purposes. As the 30-cm location is associated with percentage difference of total volume at all measurement time points, a mobile application can be developed for self-management. Ideally, this app should contain the formula for calculating percentage difference between affected and non-affected arm, to indicate if the difference between both arms can be indicated as possible development of lymphedema. Especially in patients with chronic diseases, self-efficacy is important in relation to quality of life, as well as in time spent with health-care providers and may save costs. Self-monitoring by the patient, together with careful explanation of risk profile and signs of lymphedema by health-care providers and easy access to a health-care provider in case of uncertainties, makes patients stakeholder of their own health problems. If applicable, this clinical decision tool will help patients to control possible onset of lymphedema.
Conclusion
In patients with breast cancer at risk for developing lymphedema in the arm, percentage difference of circumference measurement at a single measurement site at 30 cm proximal of the styloid process is associated with percentage difference of total arm volume. A difference of 4% between both arms has high accuracy and good sensitivity and specificity in relation to total arm volume. Future research has to confirm usefulness and validity in clinical practice.
Declaration of interest
The authors report no declarations of interest.
References
- Adriaenssens N, Buyl R, Lievens P, Fontaine C, Lamote J 2013 Comparative study between mobile infrared optoelectronic volumetry with a Perometer and two commonly used methods for the evaluation of arm volume in patients with breast cancer related lymphedema of the arm. Lymphology 46: 132–143.
- Ancukiewicz M, Russell TA, Otoole J, Specht M, Singer M, Kelada A, Murphy CD, Pogachar J, Gioioso V, Patel M, et al 2011 Standardized method for quantification of developing lymphedema in patients treated for breast cancer. International Journal of Radiation Oncology, Biology, Physics 79: 1436–1443.
- Armer JM, Henggeler MH, Brooks CW, Zagar EA, Homan S, Stewart BR 2008 The health deviation of post-breast cancer lymphedema: symptom assessment and impact on self-care agency. Self-Care, Dependend-Care and Nursing 16: 14–21.
- Czerniec SA, Ward LC, Refshauge KM, Beith J, Lee MJ, York S, Kilbreath SL 2010 Assessment of breast cancer-related arm lymphedema-comparison of physical measurement methods and self-report. Cancer Investigation 28: 54–62.
- Devoogdt N, Van Kampen M, Geraerts I, Coremans T, Christiaens MR 2011 Lymphoedema functioning, disability and health questionnaire (Lymph-ICF): reliability and validity. Physical Therapy 91: 944–957.
- Dylke ES, Yee J, Ward LC, Foroughi N, Kilbreath SL 2012 Normative volume difference between the dominant and nondominant upper limbs in healthy older women. Lymphatic Research and Biology 10: 182–188.
- Fleiss JL, Levin B, Paik MC 2003 Analysis of correlated binary data. In: Statistical Methods for Rates and Proportions, Hoboken, USA, John Wiley & Sons, Inc.
- Foroughi N, Dylke ES, Paterson RD, Sparrow KA, Fan J, Warwick EB, Kilbreath SL 2011 Inter-rater reliability of arm circumference measurement. Lymphatic Research and Biology 9: 101–107.
- Gebruers N, Truijen S, Engelborghs S, De Deyn PP 2007 Volumetric evaluation of upper extremities in 250 healthy persons. Clinical Physiology and Functional Imaging 27: 17–22.
- Hidding JT, Beurskens CH, van der Wees PJ, van Laarhoven HW, Nijhuis-van der Sanden MW 2014 Treatment related impairments in arm and shoulder in patients with breast cancer: a systematic review. PLoS ONE 9: 17.
- Hidding JT, Viehoff PB, Beurskens CH, van Laarhoven HW, Nijhuis-van der Sanden MW, van der Wees PJ 2016 Measurement properties of instruments for measuring of lymphedema: a systematic review. Physical Therapy 96: 1965–1981.
- Moffat C, Doherty D, Morgan P 2006 Best practice for the management of lymphoedema. Accessed 20-12-2017. http://www.lympho.org/portfolio/best-practice-for-the-management-of-lymphoedema/
- Mori T, Lustman A, Katz-Leurer M 2014 Self-measurement of upper extremity volume in women post-breast cancer: reliability and validity study. Physiotherapy Theory and Practice 31: 283–287.
- Pinto M, Gimigliano F, Tatangelo F, Megna M, Izzo F, Gimigliano R, Iolascon G 2013 Upper limb function and quality of life in breast cancer related lymphedema: a cross-sectional study. European Journal of Physical and Rehabilitation Medicine 49: 665–673.
- Schmitz KH, DiSipio T, Gordon LG, Hayes SC 2015 Adverse breast cancer treatment effects: the economic case for making rehabilitative programs standard of care. Supportive Care in Cancer 23: 1807–1817.
- Smoot B, Paul SM, Aouizerat BE, Elboim C, Levine JD, Abrams G, Hamolsky D, Neuhaus J, Schmidt B, West C, et al 2014 Side of cancer does not influence limb volumes in women prior to breast cancer surgery. Lymphatic Research and Biology 12: 189–193.
- Stout NL, Pfalzer LA, Levy E, McGarvey C, Springer B, Gerber LH, Soballe P 2011 Segmental limb volume change as a predictor of the onset of lymphedema in women with early breast cancer. Physical Medicine and Rehabilitation 3: 1098–1105.
- Viehoff PB, Heerkens YF, van Ravensberg CD, Hidding J, Damstra RJ, Ten Napel H, Neumann HA 2015 Development of consensus International Classification of Functioning, Disability and Health (ICF) core sets for lymphedema. Lymphology 48: 38–50.