ABSTRACT
Purpose
This study examined the effects of physical activity prescription (PAP) in patients after gastric bypass surgery. Patients’ physical activity (PA) levels and outcomes were followed over their first postoperative year.
Methods
Patients slated for bariatric surgery were randomized to a control group (n = 64) (basic information about postoperative PA) or an intervention group (n = 57) (also received physical therapist-prescribed PAP). Outcome measures were self-reported PA/exercise and sedentary time; and weight, waist circumference, blood pressure, and blood lipids; recorded pre-operatively and at 2, 6, and 12 months postoperatively. Follow-ups were conducted by nurses/dieticians. Trial registration: “Research and Development in Sweden” number 107371.
Results
There were no differences between the groups except for higher level of PA (579 vs. 182 minutes/week) six months after surgery (p = .046) and a larger decrease in cholesterol (−24 vs. −8%) after a year (p = .017) in the intervention group. Patients in both groups lost considerable weight, had reduced waist circumference, and increased PA (p < .001).
Conclusion
Although marked differences between groups were not observed over one year, the intervention group increased its PA 6-months postoperatively, but not at other time points. Whether long-term outcomes of PAP use are more robust with physical therapist participation across follow-ups warrants study.
Introduction
In recent decades, the obesity pandemic has become a global health priority (World Health Organization, Citation2013). Complications increase commensurate with increasing body mass, particularly with increasing abdominal fat (Virji and Murr, Citation2006; World Health Organization, Citation2013). Complications include type 2 diabetes, hypertension, myocardial infarction, gallstones, sleep apnea, and musculoskeletal complaints (World Health Organization, Citation2013). In addition, mortality rates are higher in individuals who are overweight or are obese. The World Health Organization reports over 2.8 million premature deaths annually from obesity-related causes; the fifth most common cause of premature death globally (World Health Organization, Citation2013).
For patients who are morbidly obese, bariatric surgery such as laparoscopic Roux-en-Y gastric bypass (LRYGB) has been reported to result in greater weight loss than non-surgical interventions (Sjöstrom, Citation2008; Sjöström et al., Citation2007). Physical activity (PA) and exercise are essential to maintain a healthy weight, and facilitate weight loss and weight stability (Jakicic, Marcus, Lang, and Janney, Citation2008; Wing and Phelan, Citation2005). In addition, PA and exercise can prevent or help manage the multisystem consequences of obesity as well as maintain general health and wellbeing. Physical inactivity, on the other hand, contributes both directly and indirectly to the total burden of disease, in addition, human suffering. Physical inactivity contributes to considerable socioeconomic burden due to related illnesses, injuries, and disability including limitation in activities of daily living and employment, and premature death (Peterson, Backlund, and Diderichsen, Citation1998).
Physical activity has been defined by Caspersen, Powell, and Christenson (Citation1985) as “any bodily movement, produced by skeletal muscles that result in energy expenditure” and exercise as “planned, structured, repetitive and purposeful movement to improve or maintain one or more components of physical fitness”. The health effects of PA are well known (World Health Organization, Citation2010). Even small increases in PA impact morbidity and mortality. For example, individuals who are active for as little as 15 minutes/day may reduce risk of all-cause mortality by 14% and increase life expectancy by 3 years compared with inactive individuals (Wen et al., Citation2011). Each additional 15 minutes of PA a day beyond the minimum of 15 minutes may further reduce all-cause mortality by 4% and all-cancer mortality by 1%. The benefits are observed across age groups, in both sexes, and in those at risk of cardiovascular disease. Light-intensity PA for 4 hours/week has also been reported to be associated with a 38% reduction in all-cause mortality compared with being sedentary (Holme and Anderssen, Citation2015). Further, for each added hour of PA per week, there is a significant increase in survival. There is no formal definition of the minimal important difference in level of PA to achieve its benefits, but it has been suggested that an increase of 15 minutes/day (105 minutes/week) is likely clinically relevant (Holme and Anderssen, Citation2015).
People who are obese report that weight is a hindrance to being physically active (Wiklund, Olsén, and Willén, Citation2011). It limits the ability to be active. For instance, people who have knee osteoarthritis as well as are obese or have large waist circumferences have been reported to have reduced gait speeds and less ability to walk compared to individuals with healthy weights and small to medium waist circumferences (Gill et al., Citation2017).
Bariatric surgery with commensurate weight loss has been reported to improve patients’ self-reported physical function including less back and knee pain, increased walking speed, and improved ability to climb stairs and navigate obstacles (Gill et al., Citation2016; King et al., Citation2016; Morrow et al., Citation2020; Vincent et al., Citation2012). Patients’ physical activity before and after surgery has been investigated in several trials. In 2016, one review reported on 26 articles evaluating changes in PA after bariatric surgery (Herring et al., Citation2016). The investigators reported a shift toward more active time but with less intensity, within the first 6 months postoperatively. This was demonstrated by a reduction in intensity of PA and an increase in step count. In a trial of 2458 participants, 76.5% who completed baseline and follow-up assessments improved their physical function beyond a clinically meaningful difference (King et al., Citation2016). Patients who have undergone laparoscopic surgery reported being more active than those undergoing open procedures in both the short (i.e. 2 weeks) and long-term (i.e. 3 months) (Evans et al., Citation2004). Other studies such as one by Berglind et al. (Citation2015) have not reported differences between pre – and post-surgery differences in PA or sedentary behavior. With respect to the perspectives of patients, investigators have reported that although being physically active and exercising is easier for patients after bypass surgery, modifying exercise and identifying the optimal parameters of exercise remain challenging for them (Wiklund, Olsén, and Willén, Citation2011).
Physical activity on prescription (PAP) is a strategy recommended for use by licensed health care practitioners in Sweden for promoting both PA and exercise within this population (Swedish National Board of Health and Welfare (Socialstyrelsen), Citation2018). This strategy has been shown to increase PA and exercise in the population as a whole, thereby enhancing cardiovascular and metabolic health, and health-related quality of life (Kallings et al., Citation2009; Leijon et al., Citation2009; Lundqvist et al., Citation2017; Olsson et al., Citation2015; Rodjer, Jonsdottir, and Borjesson, Citation2016). In one systematic review, a high level of evidence supported use of the PAP for increasing PA in inactive adult patients (Onerup et al., Citation2018). The PAP embodies patient-centered care and includes three core individualized elements: dialogue, recommendation of PA with a written prescription, and follow-up (Kallings, Citation2008). Despite its being actively promoted by the Swedish National Board of Health and Welfare (Socialstyrelsen) (Citation2018), PAP is underused by licensed health professionals in the country due to lack of knowledge, and lack of supportive management and supporting structures for its routine implementation (Borjesson, Citation2012; Gustavsson et al., Citation2018). Not only are studies needed to increase its use clinically, but they are also needed to evaluate the effectiveness of PAP for various subgroups of patients who are in urgent need of increasing their activity (Arsenijevic and Groot, Citation2017). Those having undergone bariatric surgery constitute one such subgroup. Therefore, the purpose of this study was to examine the long-term effects of PAP on levels of PA, exercise, and weight loss in addition to several other health-related variables in patients after LRYGB.
Methods
Participants and Experimental Design
Over 30 months, patients slated for LRYGB surgery at Sahlgrenska University Hospital were invited to participate in a randomized controlled trial after having had access to both written and verbal information about the study and its requirements. Exclusion criteria were not being fluent in Swedish or having concurrent cardiovascular, orthopedic, respiratory, rheumatologic, or neurologic conditions or injury that would limit participants’ capacity to be physically active at a moderate-intensity level for at least 150 minutes/week. The study protocol was approved by the Regional Ethics Committee for the region of Västra Götaland, Sweden (Registration number: 925–12). The trial was registered in “FoU in Sweden” (Research and Development in Sweden). Registration number: 107371.
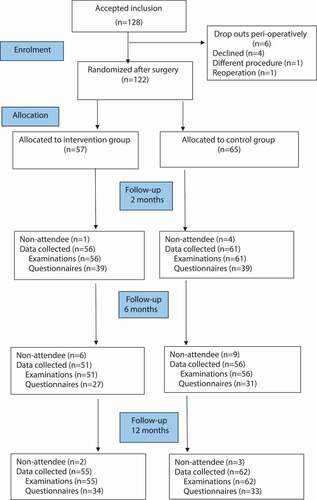
A consecutive series of 128 patients provided written consent and were included based on the inclusion and exclusion criteria. Seven patients withdrew during the postoperative hospital stay () resulting in 122 patients who were randomized to one of two groups (ratio 1:1), the control group or intervention group, prior to hospital discharge. Randomization was performed using opaque sealed envelopes; the content of which was prepared after an electronic random table generated by a person independent of the study.
The characteristics of the 122 patients appear in . The patients in the control and intervention groups were comparable at inclusion to the study with one exception, height. The control group had a higher proportion of men (28% vs. 14%), thus was taller on average compared with the experimental group (p = .012).
Table 1. Characteristics of the patients with obesity who underwent gastric bypass surgery.
Intervention
The patients in the control group (n = 64) received care that is standard in Sweden. Administered by physical therapists, this included general written and verbal information about the importance of PA and exercise and how to return to an optimal level after surgery. In addition to general information administered to the control group, patients in the intervention group (n = 57) received a PAP that was individually prescribed by the physical therapist based on patients’ general multisystem assessment and their baseline PA, exercise, and preferences. Based on each patient’s goals, the dose of PA in the written instruction included type of exercise, frequency, intensity, and duration (Garber et al., Citation2011; World Health Organization, Citation2010). Patients were to start with low-intensity aerobic exercise such as walking during the first three weeks post-operatively. Thereafter, the exercise dose parameters were progressed with the goal of reaching at least 150 minutes of moderately intense PA and exercise per week and maintaining it throughout the first year after surgery. Motivational interviewing strategies were used with goal setting and establishing the initial PAP, to encourage and enable patients to succeed in adhering to the program for one year, the duration of the study.
After hospital discharge, patients were followed at 2, 6 and 12 months by nurses or dieticians at the surgical out-patient clinic which is established practice after bariatric surgery. At each follow-up, patients in the control group received additional general advice about the importance of PA and the patients in the intervention group received the same advice, but also reinforcement and modifications or progressions of the PAP.
Preoperatively and at the three designated follow-ups, patients received the same two questions regarding PA (subjective primary outcome) and exercise based on the established recommendations of the Swedish National Board of Health and Welfare (Socialstyrelsen) (Citation2018): 1) How much time do you spend being physically active in a typical week, such as walking, cycling, or gardening; and 2) How much time do you spend exercising in a typical week that makes you become breathless, such as running, group exercises or ball sports?
So the investigators could calculate metabolic equivalents (METs), patients also completed the International Physical Activity Questionnaire (IPAQ) (Craig et al., Citation2003; Ekelund et al., Citation2006). The IPAQ assesses the amount (i.e. duration in minutes and frequency in days) of three categories of activity during the last 7 days with three individual scores: 1) low-intensity activities such as walking at a comfortable pace; 2) moderate-intensity activities (above comfortable pace); and 3) vigorous-intensity activities (much above a comfortable pace). In addition, they recorded how much time participants were sedentary each day. A total weekly MET level was calculated according to guidelines by multiplying the reported minutes per week in each category by 3.3 for low-intensity activity, 4.0 for moderate-intensity activity, and 8.0 for vigorous-intensity activity (International Physical Activity Questionnaire, Citation2005). The scores from these three categories were consolidated into a total MET-minutes/week score.
Patients’ weights (objective primary outcome), heights, and waist circumferences were measured, and body mass index (BMI) was calculated pre-operatively. These measures were recorded at baseline and at each of the three successive follow-up time points by a person who was blinded to each patient’s group allocation. In addition, blood pressure, blood lipids (high – and low-density lipoproteins), cholesterol, and triglycerides, before and one year after surgery, were recorded.
Statistical Analysis
Two power analyses were performed with power of 0.87 and alpha of 0.05. For the subjective primary outcome (i.e. estimated number of minutes of PA per week) the analysis was based on a statistically significant difference between the two groups of 50 minutes (150 vs. 100 [SD 50]), giving a sample size of 20 participants per group. For the objective primary outcome, weight, the analysis was based on the hypothesis of a statistically significant difference of 4 kg (100 vs 104 kg [SD 6]) at the end of the first postoperative year, giving a sample size of 43 people per group. To detect differences in the secondary outcomes and account for dropouts, we aimed to include at least 50 per group who would be followed up one year postoperatively. The results were analyzed with a mixed repeated measurements covariance pattern compound symmetry model based on change from baseline with baseline values as covariates; and t-test for continuous variables, and Chi-square and Fisher’s exact test for dichotomous variables.
Results
Preoperatively, 82 of 122 patients reported engaging in moderately intense exercise and the remaining 40 were more vigorously active. Levels of PA, exercise and sedentary time assessed with the two key questions and the IPAQ are presented in . Postoperatively, the two groups were comparable except for the intervention group which reported being more physically active at 6-month follow-up compared with the control group (p = .046). There were no differences (p > .05) between the two groups across the four data collection points (data not shown) in the proportion of patients who reached at least 150 minutes of moderate-intensity PA per week.
Table 2. Level of physical activity and exercise in the participants before, and 2, 6 and 12 months postoperatively.
Compared with preoperative baseline measures, patients in both groups increased their PA levels two months after surgery and this was sustained at 6 months postoperatively in the intervention group. With respect to exercise, the level was low during the first postoperative year in both groups but greater across follow-ups for the intervention group (p < .05) compared to only at 2 months in the control group (p = .024). The intervention group also expended more METs minutes across the three follow-ups (p < .05) which was not observed in the control group. Although both groups tended to increase sedentary time after 2 months, this was only significantly so for the intervention group (p = .001). However, both groups sat less at one-year follow-up (p < .001).
Twenty-two patients in the intervention group and 20 in the control group completed the two physical activity-related questionnaires across the four data collection points (i.e. preoperatively, and postoperatively at 2, 6 and 12 months). Their PA and sedentary time per day are presented in and. There appeared to be tendencies in the intervention group toward more activity and less sedentary time 2 and 6 months postoperatively but these tendencies were not apparent at one year.
Figure 2. A and b. Duration of physical activity and sedentary behavior during the first year after bariatric surgery (Median, 95% confidence intervals).
Weight, BMI, and waist circumference in the intervention group and control group before surgery and 2, 6 and 12 months after surgery are presented in . There were overall differences between the two groups and across time points for all three variables (ANOVA p < .001). Post-hoc analysis showed no difference between groups for any of the data collection time points, but differences were observed within groups between time-points (p < .001). There was a difference between groups with respect to cholesterol levels during the first postoperative year (p = .017), but not for other blood tests or blood pressure ().
Table 3. Weight, body mass index, and waist circumference over the first year after bariatric surgery in the intervention and control groups.
Table 4. Systolic and diastolic blood pressures, high-density lipoprotein, low-density lipoprotein, cholesterol, and triglycerides, and % change before and 1 year after bariatric surgery.
Discussion
Bariatric surgery appears to be the only intervention that results in long-term weight loss in patients with morbid obesity (Sjöstrom, Citation2008; Sjöström et al., Citation2007). Although an increasing number of individuals undergo various types of bariatric surgery each year worldwide, it is not the solution for all patients and certainly less desirable than other noninvasive interventions (e.g. various types of prescribed lifestyle interventions). Generally, PA and exercise have a weight reduction effect (Donnelly et al., Citation2009), however the evidence for such interventions in individuals who are obese is sparse (Wu, Gao, Chen, and van Dam, Citation2009) despite the likelihood that it has a role in weight stabilization (Jakicic, Marcus, Lang, and Janney, Citation2008; Wing and Phelan, Citation2005). Other advantages include reduced obesity-related complications. Individuals who are obese but also fit have been reported to have lower risk of all-cause and cardiovascular disease mortality than those who are not fit (McAuley and Blair, Citation2011; McAuley et al., Citation2010).
This study’s aim was to evaluate the long-term effects of PAP in patients slated for bariatric surgery on their levels of PA, exercise, and weight loss in addition to several health-related variables. We identified no differences between the intervention and control groups, but a higher level of PA in the intervention group six months postoperatively and a larger reduction in cholesterol levels after one year. There were tendencies toward a more active lifestyle after two and six months in the sub-group of patients in the intervention group that completed the questionnaires across all four time points compared with the same sub-group in the control group (–). However, these tendencies were not observed at one-year follow-up. The results are therefore contradictory.
Exercise counseling including use of a pedometer has earlier been compared with the use of a pedometer alone or standard care (Creel et al., Citation2016). The counseling included: psychosocial assessment (e.g. social support and perceived benefits/barriers); sequence of education topics (e.g. goal setting and maintaining motivation); and counseling strategies (e.g. motivational interviewing and barrier review). The addition of exercise counseling increased PA from the perioperative period to 6½ months after surgery. However, the group that used pedometers without professional feedback was not observed to be more active than those receiving standard care. The counseling in the trial was more extensive both in scope and time than in the current study even if there are similarities such as the use of motivational interviewing and goal setting. Pre-surgical physical conditioning training in addition to individual lifestyle counseling has also been evaluated (Baillot et al., Citation2016, Citation2018). Both strength and endurance training before surgery were reported to improve physical fitness and social interaction and reduce self-consciousness and embarrassment (Baillot et al., Citation2016). Positive effects of the additional intervention were also observed one-year post-surgery with respect to level of PA and weight loss (Baillot et al., Citation2018).
Two other studies from our research group have explored patients’ experiences of PA before and after bariatric surgery. Preoperatively, individuals experienced their weight as the main obstacle to PA and exercise, and they planned to increase their activity and exercise levels as they lost weight after surgery (Wiklund, Olsén, and Willén, Citation2011). One year postoperatively, they met some goals but also challenges remained related to being physically active (Wiklund, Olsén, Olbers, and Willén, Citation2014). Hindrances were described. Not only were their physical bodies considered obstacles, but also their motivation to exercise was low. Nonetheless, the patients expressed increased understanding of the benefits of PA and exercise. In the current study, patients in both groups were more physically active postoperatively which may be a result of weight loss (i.e. being less heavy and more mobile). The results showed an increase in PA exceeding 150 minutes/week in both groups which is more than the 105 minutes/week which has been proposed as being clinically relevant (Holme and Anderssen, Citation2015). In addition, use of the PAP improved PA more measured six months postoperatively, compared with the control group which only received general information.
The PAPs were administered by physical therapists to patients in the intervention group after their surgeries and before discharge from hospital. It was tailored to suit the patients´ contexts and preferences with respect to the type of PA and individualized regarding intensity, duration and frequency. Modification of the PAP coupled with reinforcement of general information at the three follow-up time points however were conducted by nurses and dieticians at the surgical out-patient clinic. Physical therapists are applied clinical exercise physiologists who maximize people’s capacity to develop, maintain and restore movement and functional capacity across the life cycle (World Confederation for Physical Therapy, Citation2020). In the present study, the patients did not have access to physical therapists throughout the postoperative year. Further studies are needed to establish whether the outcomes of use of the PAP would have been substantially superior if physical therapists conducted the follow-ups along the care continuum.
The PAP was originally designed to be readily implemented in clinical practice. There are several alternatives regarding types of PA and exercise to prescribe; one type does not fit all. That people overestimate their PA and exercise levels have been well established; this is also true for patients with obesity (Lee, Macfarlane, Lam, and Stewart, Citation2011). In addition, patients who are obese can be challenged to identify an appropriate PA level, thus need qualified guidance and support (Wiklund, Olsén, Olbers, and Willén, Citation2014; Wiklund, Olsén, and Willén, Citation2011). Individualized advice therefore is critical to increase adherence and to minimize side effects of the training such as musculoskeletal strains and injuries.
There is growing evidence supporting the essential role of PA and exercise after bariatric surgery. However, questions remain for this cohort regarding how to prescribe exercise and monitor PA, and how and when physical conditioning, muscle strength, fat and fat-free mass, and bone mineral density should be assessed (Hansen et al., Citation2020). In the present trial, PA and exercise were assessed in two ways: two simple questions and completing the IPAQ. The questions in the IPAQ cover a range of physical activities and exercises which enabled the research team to calculate METs. The patients reported having some challenges responding to the questions. The three intensity levels, low/moderate/high, must be answered with respect to both duration (in minutes) and number of sessions per week. Difficulties in completing the IPAQ have been reported previously (Wiklund, Olsén, Olbers, and Cider, Citation2014). In one systematic review (Lee, Macfarlane, Lam, and Stewart, Citation2011) regarding the validity of the IPAQ, the investigators reported that the IPAQ overestimated activity levels when compared with an objective measure, by an average of 84% and that the correlation between the score on the IPAQ and objective measure of PA was generally lower than the acceptable standard. These findings were confirmed by investigators in another study in which the IPAQ scores for activity measures reflected substantial over-reporting of PA and under-reporting of sedentary behavior, compared to objective, accelerometer-derived measures (Celis-Morales et al., Citation2012).
There are several strengths of our study. All patients underwent surgery at the same clinic and received the same clinical care before, during and after surgery. They were also followed according to established guidelines.
There are also potential limitations. Although we evaluated the intervention effects using objective clinical and laboratory measurements performed at the hospital during follow-up visits, subjective assessment tools were used for PA and exercise. These two related questionnaires were not returned as consistently as expected. Therefore, we had limited results for the outcome measures that depended on responses in the questionnaires. Less than half of the participants in both groups completed the PA questionnaire across the four time points. In addition, because patients did not respond to the IPAQ as completely as expected, the volume of data was further reduced. Both issues may contribute to bias and lowered confidence in the validity of the results. However, only a minimal number of participants failed to complete the follow-up sessions at the clinic yielding a low drop-out rate to the follow-ups collected at the hospital (). As several statistical analyses were carried out and no adjustment was made to correct for multiple comparisons, there is a risk that the effects have been misinterpreted. We performed two power analyses to estimate the sample size, a difference of 50 minutes in PA per week or 4 kg in body weight. However, such calculations can be arbitrary running the risk of over – or under-estimation. Another limitation is that the patients were not followed postoperatively by a physical therapist who has exercise physiology knowledge and with practice and experience working with patients who are obese. In addition, because we intended to evaluate the impact of PAP only, adherence was not monitored or tracked. Doing so could have identified another variable influencing the study’s findings. Thus, whether and to what degree patients followed instructions cannot be confirmed.
In conclusion, written and verbal instructions about PA and exercise along with a PAP administered to patients by physical therapists at discharge after bariatric surgery and followed up three times over the first postoperative year by nurses or dieticians appear to increase PA. However, although PAP may be a useful tool in the postoperative management of patients after bariatric surgery, its impact may be sub-optimal without having physical therapists participate in patients’ long-term rehabilitation. Physical therapists warrant being included in the postoperative team in the care of patients after bariatric surgery over the long term to maximize their return to their activities of daily living and return to work. Finally, objective rather than subjective measures of PA and exercise are warranted to optimize the validity of the exercise data. Further studies are needed to confirm these hypotheses, thereby maximizing the utility of the PAP in patients after bariatric surgery and perhaps other patient cohorts.
Disclosure of Interest
The authors declare no conflicts of interest.
Acknowledgments
This work was supported by the Research and Development Council for Gothenburg and Southern Bohuslän under grant VGFOUGSB-258521
References
- Arsenijevic J, Groot W 2017 Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open 7: e012156.
- Baillot A, Mampuya WM, Dionne IJ, Comeau E, Méziat-Burdin A, Langlois MF 2016 Impacts of supervised exercise training in addition to interdisciplinary lifestyle management in subjects awaiting bariatric surgery: A randomized controlled study. Obesity Surgery 26: 2602–2610.
- Baillot A, Vallée CA, Mampuya WM, Dionne IJ, Comeau E, Méziat-Burdin A, Langlois MF 2018 Effects of a pre-surgery supervised exercise training 1 year after bariatric surgery: A randomized controlled study. Obesity Surgery 28: 955–962.
- Berglind D, Willmer M, Eriksson U, Thorell A, Sundbom M, Uddén J, Raoof M, Hedberg J, Tynelius P, Näslund E, et al. 2015 Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obesity Surgery 25: 119–125.
- Borjesson M 2012 Health care services can boost physical activity on prescription - More people need prescriptions. Lakartidningen. 109: 2340.
- Caspersen CJ, Powell KE, Christenson GM 1985 Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports. 100: 126–131.
- Celis-Morales CA, Perez-Bravo F, Ibanez L, Salas C, Bailey ME, Gill JM 2012 Objective vs. self-reported physical activity and sedentary time: Effects of measurement method on relationships with risk biomarkers. PLoS One 7: e36345.
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF et al. 2003 International Physical Activity Questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 35: 1381–1395.
- Creel DB, Schuh LM, Reed CA, Gomez AR, Hurst LA, Stote J, Cacucci BM 2016 A randomized trial comparing two interventions to increase physical activity among patients undergoing bariatric surgery. Obesity 24: 1660–1668.
- Donnelly J, Blair S, Jakicic J, Manore M, Rankin J, Smith B 2009 American College of Sports Medicine Position Stand. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Medicine and Science in Sports and Exercise. 41: 459–471
- Ekelund U, Sepp H, Brage S, Becker W, Jakes R, Hennings M, Wareham NJ 2006 Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutrition 9: 258–265.
- Evans RK, Bond DS, Demaria EJ, Wolfe LG, Meador JG, Kellum JM 2004 Initiation and progression of physical activity after laparoscopic and open gastric bypass surgery. Surgical Innovation 11: 235–239.
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP 2011 American College of Sports Medicine 2011 American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Medicine and Science in Sports and Exercise.43: 1334–1359.
- Gill SV, Hicks G, Zhang Y, Niu J, Apovian CM, White DK 2017 The association of waist circumference with community walking ability in knee osteoarthritis: The osteoarthritis initiative. Osteoarthritis and Cartilage 25: 60–66.
- Gill SV, Walsh MK, Pratt JA, Toosizadeh N, Najafi B, Travison TG 2016 Changes in spatio-temporal gait patterns during flat ground walking and obstacle crossing one year after bariatric surgery. Surgery for Obesity and Related Diseases 12: 1080–1085.
- Gustavsson C, Nordqvist M, Broms K, Jerden L, Kallings LV, Wallin L 2018 What is required to facilitate implementation of Swedish physical activity on prescription? - Interview study with primary healthcare staff and management. BMC Health Services Research 18: 196.
- Hansen D, Decroix L, Devos Y, Nocca D, Cornelissen V, Dillemans B, Lannoo M 2020 Towards optimized care after bariatric surgery by physical activity and exercise intervention: A review. Obesity Surgery 30: 1118–1125.
- Herring LY, Stevinson C, Davies MJ, Biddle SJ, Sutton C, Bowrey D, Carter P 2016 Changes in physical activity behaviour and physical function after bariatric surgery: A systematic review and meta-analysis. Obesity Reviews 17: 250–261.
- Holme I, Anderssen SA 2015 Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. British Journal of Sports Medicine 49: 743–748.
- International Physical Activity Questionnaire 2005 Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). www.ipaq.ki.se/scoring.pdf.
- Jakicic JM, Marcus BH, Lang W, Janney C 2008 Effect of exercise on 24-month weight loss maintenance in overweight women. Archives of Internal Medicine 168: 1550–1559.
- Kallings LV 2008 Physical Activity on Prescription: Studies on Physical Activity Level, Adherence and Cardiovascular Risk Factors. Doctoral Dissertation, Karolinska Institute, Stockholm.
- Kallings LV, Sierra Johnson J, Fisher RM, Faire U, Ståhle A, Hemmingsson E, Hellénius M 2009 Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: Results from a randomized controlled trial. European Journal of Cardiovascular Prevention and Rehabilitation 16: 80–84.
- King WC, Chen JY, Belle SH, Courcoulas AP, Dakin GF, Elder KA, Flum DR, Hinojosa MW, Mitchell JE, Pories WJ et al. 2016 Change in pain and physical function following bariatric surgery for severe obesity. JAMA. 315: 1362–1367.
- Lee PH, Macfarlane DJ, Lam TH, Stewart SM 2011 Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. International Journal of Behavioral Nutrition and Physical Activity 8: 115.
- Leijon ME, Bendtsen P, Nilsen P, Festin K, Stahle A 2009 Does a physical activity referral scheme improve the physical activity among routine primary health care patients? Scandinavian Journal of Medicine & Science in Sports 19: 627–636.
- Lundqvist S, Borjesson M, Larsson ME, Hagberg L, Cider A 2017 Physical Activity on Prescription (PAP), in patients with metabolic risk factors. A 6-month follow-up study in primary health care. PLoS One 12: e0175190.
- McAuley PA, Blair SN 2011 Obesity paradoxes. Journal of Sports Science 29: 773–782.
- McAuley PA, Kokkinos PF, Oliveira RB, Emerson BT, Myers JN 2010 Obesity paradox and cardiorespiratory fitness in 12,417 male veterans aged 40 to 70 years. Mayo Clinic Proceedings 85: 115–121.
- Morrow E, Chang JW, Biber J, Miller M, McGarrity L, Glasgow R, Volckmann E, Ibele A 2020 Prospective collection of PROMIS physical function measure demonstrates significant improvement after bariatric surgery. Obesity Surgery 30: 1898–1903.
- Olsson SJ, Börjesson M, Ekblom-Bak E, Hemmingsson E, Hellénius ML, Kallings LV 2015 Effects of the Swedish physical activity on prescription model on health-related quality of life in overweight older adults: A randomised controlled trial. BMC Public Health 15: 687.
- Onerup A, Arvidsson D, Blomqvist A, Daxberg EL, Jivegard L, Jonsdottir IH, Lundqvist S, Mellén A, Persson J, Sjögren P et al. 2018 Physical activity on prescription in accordance with the Swedish model increases physical activity: A systematic review. British Journal of Sports Medicine. 53: 383–388.
- Peterson S, Backlund I, Diderichsen F 1998 Sjukdomsbördan i Sverige - en Svensk DALY-Kalkyl [The burden of disease in Swedem- A Swedish DALY-Calculation]. Stockholm: Folkhälsomyndigheten (The Public Health Agency of Sweden)
- Rodjer L, Jonsdottir IH, Borjesson M 2016 Physical activity on prescription (PAP): Self-reported physical activity and quality of life in a Swedish primary care population, 2-year follow-up. Scandinavian Journal of Primary Health Care 34: 443–452.
- Sjöstrom L 2008 Bariatric surgery and reduction in morbidity and mortality: Experiences from the SOS study. International Journal of Obesity. 32: S93–97.
- Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, Lystig T, Sullivan M, Bouchard C, Carlsson B et al. 2007 Effects of bariatric surgery on mortality in Swedish obese subjects. New England Journal of Medicine. 357: 741–752.
- Swedish National Board of Health and Welfare (Socialstyrelsen) 2018 Nationella Riktlinjer för Prevention och Behandling vid Ohälsosamma Levnadsvanor: Stöd för Styrning och Ledning [National Guidelines for Prevention and Treatment for Unhealthy Lifestyle]. Stockholm.
- Vincent HK, Ben-David K, Conrad BP, Lamb KM, Seay AN, Vincent KR 2012 Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surgery of Obesity and Related Diseases 8: 346–354.
- Virji A, Murr MM 2006 Caring for patients after bariatric surgery. American Family Physician. 73: 1403–1408.
- Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, Chan HT, Tsao CK, Tsai SP, Wu X 2011 Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 378: 1244–1253.
- Wiklund M, Olsén MF, Olbers T, Cider Å 2014 Physical fitness and physical activity in Swedish women before and one year after roux-en-Y gastric bypass surgery. Open Obesity Journal 6: 38–43.
- Wiklund M, Olsén MF, Olbers T, Willén C 2014 Experiences of physical activity one year after bariatric surgery. Open Obesity Journal 6: 25–30.
- Wiklund M, Olsén MF, Willén C 2011 Physical activity as viewed by adults with severe obesity, awaiting gastric by-pass surgery. Physiotherapy Research International 16: 179–186.
- Wing RR, Phelan S 2005 Long-term weight loss maintenance. American Journal of Clinical Nutrition 82: 222S–225S.
- World Confederation for Physical Therapy 2020 Policy Statement: Description of Physical Therapy. https://world.physio/policy/ps-descriptionPT.
- World Health Organization 2010 Global Recommendations on Physical Activity for Health. www.who.int/dietphysicalactivity/publications/9789241599979/en/.
- World Health Organization 2013 Fact sheet N° 311: Obesity and Overweight. www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- Wu T, Gao X, Chen M, van Dam RM 2009 Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: A meta-analysis. Obesity Reviews 10: 313–323.