ABSTRACT
Background
Systematic reviews have reported benefits of preoperative inspiratory muscle training in adults undergoing cardiac surgery, however there have been inconsistencies with the devices used. Threshold devices generate a constant inspiratory load independent of respiratory rate.
Objective
To assess the effect of preoperative inspiratory muscle training using threshold devices in adults undergoing cardiac surgery.
Methods
A literature search was conducted across five electronic databases. Seven randomized controlled trials met the inclusion criteria and were critically appraised. The primary outcome was length of hospital stay. Secondary outcomes included postoperative pulmonary complications, quality of life and mortality.
Results
Seven eligible randomized controlled trials were identified with a total of 642 participants. One study was a post hoc analysis of one of the included studies. Three out of five studies reported a decrease in length of postoperative hospital stay (p < 0.05). A significant reduction in postoperative pulmonary complications was reported by three studies (p < 0.05). There were concerns with bias across all papers.
Conclusions
Preoperative threshold inspiratory muscle training has potential to reduce postoperative length of hospital stay and pulmonary complications after cardiac surgery. The evidence on quality of life and mortality is inconclusive. The overall evidence for these conclusions may be influenced by bias.
Introduction
Cardiac surgery is associated with major postoperative complications which impact on long-term survival (Seese et al., Citation2020). Pulmonary complications are a leading cause of morbidity and mortality after cardiac surgery with reported incidences ranging from 2% all the way to 95% (Wynne, Citation2004) depending on the definition used, the type of cardiac surgery and the study population (Naveed et al., Citation2017).
The pathogenesis of pulmonary complications following cardiac surgery is complex and multifactorial. Suggested mechanisms for pulmonary dysfunction include direct disruption of chest wall mechanics from surgical incisions, damage to the phrenic nerve, and indirect impairment of lung function secondary to a systemic inflammatory response induced by surgery (Badenes, Lozano, and Belda, Citation2015). Subsequent implications on gas exchange and functional and vital capacities may account for pulmonary infections, through alterations in V/Q ratios, and atelectasis (Siafakas, Mitrouska, Bouros, and Georgopoulos, Citation1999). In addition to the effects of surgery, patients undergoing cardiac surgery may be more susceptible to the development of postoperative pulmonary complications due to the presence of coexisting pulmonary disease, and cardiac disease affecting lung function (Weissman, Citation2004). Such complications prolong postoperative hospital stay, are associated with increased hospital costs (Sabaté, Mazo, and Canet, Citation2014) and the potential for further complications (Hauck and Zhao, Citation2011).
A recent study by D’Arx et al. (Citation2020) reported that one quarter of patients awaiting elective cardiac surgery had inspiratory muscle weakness. Thus, there may be an important role for preoperative interventions which function to increase the function of inspiratory muscles before cardiac surgery. Inspiratory muscle training aims to improve the function of the muscles used in inspiration, primarily the diaphragm, external intercostal muscles and parts of the internal intercostal muscles (McConnell, Citation2013). Threshold inspiratory muscle training uses pressure-threshold devices which require individuals to generate a sufficiently high inspiratory pressure to overcome a negative pressure load using a one-way spring-loaded valve (McConnell, Citation2013). As a form of resistance training, threshold training functions to increase respiratory muscle strength by imposing a load on the muscles, increasing tension (McConnell, Citation2013). A unique feature of threshold devices is the load is independent of the respiratory rate, generating a linear pressure load which can be increased incrementally during training (Menzes et al., Citation2018; Paiva et al., Citation2015). Although there is no definitive consensus about which devices are most effective for inspiratory muscle training, this feature may account for its popularity of use in studies. Improvements in respiratory muscle strength using this type of device have been demonstrated across a range of patient populations, including those with chronic kidney disease, chronic obstructive pulmonary disease, heart failure and in patients undergoing bariatric surgery (Beaumont, Forget, Couturaud, and Reychler, Citation2018; Casali et al., Citation2011; de Medeiros et al., Citation2017; Lin et al., Citation2012).
In the context of cardiac surgery, inspiratory muscle training in the preoperative period is gaining interest for its reported benefits over standard care in improving postoperative outcomes, especially concerning postoperative pulmonary complications and length of postoperative hospital stay (Ge et al., Citation2018; Gomes Neto, Martinez, Reis, and Carvalho, Citation2017; Karanfil and Møller, Citation2018; Katsura et al., Citation2015; Kendall et al., Citation2018; Mans, Reeve, and Elkins, Citation2015). A number of these reviews, however, also included patients undergoing abdominal surgery; others included other physiotherapy regimes, or training using non-threshold devices. To the best of the authors’ knowledge, there is no systematic review which exclusively assesses the effect of threshold inspiratory muscle training in patients undergoing cardiac surgery. Thus, conclusions about the effectiveness of threshold inspiratory muscle training in the preoperative period in adults undergoing cardiac surgery are based on systematic reviews with limited studies evaluating this research area. This review therefore aims to provide more substantive evidence for the use of preoperative threshold inspiratory training in adults undergoing cardiac surgery in order to work toward a common protocol for preoperative care in this patient group.
Methods
Review question
Does preoperative threshold inspiratory muscle training in adults undergoing cardiac surgery improve postoperative outcomes?
Identification and selection of studies
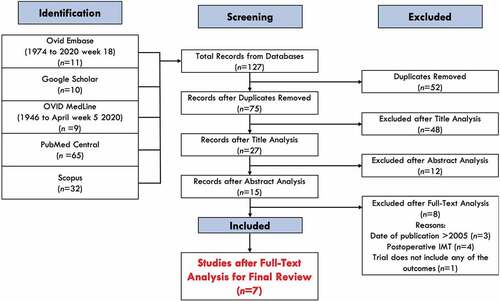
In order to be as rigorous as possible, a literature search was conducted independently by three investigators using the following five databases: Ovid EMBASE, Google Scholar, Ovid MEDLINE, PubMed Central and Scopus. The last search was carried out on 12th May 2020. Keywords used included: “cardiac surgery,” “inspiratory muscle training” and “preoperative.” Full search terms and applied limits used in each database can be found in Appendix A.
Following the removal of duplicates, the studies were screened by assessing the title, abstract, and full text against the inclusion and exclusion criteria. Each paper was independently screened by two reviewers and any discrepancies were discussed and agreed as a group. The screening process was carried out according to the Preferred Reporting Items of Systematic reviews and Meta-Analysis (PRISMA) flow diagram search protocol.
Inclusion and exclusion criteria
The PICOS framework (patient, intervention, control, outcome and study) recommended by the Cochrane Collaboration (McKenzie et al., Citation2019), was used to formulate the review question and to determine the full inclusion and exclusion criteria. Papers were selected if they included: adults undergoing cardiac surgery; preoperative inspiratory muscle training with a threshold inspiratory muscle training device; assessed postoperative pulmonary complications, postoperative hospital stay, all-cause mortality or quality of life as an outcome; and were a randomized controlled trial, in English, published in or after 2005.
Papers were excluded if they included: pediatric (<18 years) patients; non-cardiac surgery; inclusion of other non-conventional preoperative regimes, other types of inspiratory muscle training devices or no preoperative inspiratory muscle training.
Study characteristics
Population
Studies which met the inclusion criteria included adults undergoing all types of elective cardiac surgery. Data extracted about the participants were age, sex, and type of cardiac surgical procedure.
Intervention
The intervention was threshold inspiratory muscle training in the preoperative period. Data extracted about the intervention included the type of device, inspiratory load, duration of inspiratory muscle training and control intervention design.
Outcome measures
The primary outcome was the duration of postoperative hospital stay. The secondary outcomes were postoperative pulmonary complications, quality of life and all-cause mortality.
Critical appraisal
Critical appraisal of each paper was carried out independently by three investigators using the Methodology Checklist-2: Controlled Trials, developed by the Scottish Intercollegiate Guidelines Network (Citation2020). Bias was also assessed using the Cochrane Risk-of-Bias tool (RoB-2) checklist (Sterne et al., Citation2019), which assigns either a high risk, low risk, or some concerns of bias across several domains. Any discrepancies in findings were discussed and resolved as a group.
Results
Identification and selection of studies
A total of 164 articles were identified from the literature search. After applying the inclusion and exclusion criteria, seven articles were identified for inclusion using the screening protocol outlined in (Chen et al., Citation2019; Ferreira, Rodrigues, and Évora, Citation2009; Hulzebos et al., Citation2006a, Citation2006b; Savci et al., Citation2011; Sobrinho, Guirado, and Silva, Citation2014; Valkenet et al., Citation2017).
Figure 1. Flow diagram showing the literature search protocol. Adapted from the PRISMA flow diagram (Moher, Liberati, Tetzlaff, and Altman, Citation2009).
Study characteristics
Population
Of the seven studies, one (Valkenet et al., Citation2017) was a post hoc analysis of one of the other included studies (Hulzebos et al., Citation2006b), analyzing data not previously reported, from the same patient population. With this in consideration, there were 642 unique participants across the seven studies. Of the patient population, 308 participants had been allocated to an intervention group and 334 participants to a control group. The mean age of participants in each study ranged between 57 and 70 years old. The average male proportion across the groups was 50%–90.5%. Five studies specified that participants were patients undergoing exclusively coronary artery bypass graft (CABG) surgery. Chen et al. (Citation2019) studied patients undergoing either a CABG procedure or cardiac valve surgery. Ferreira, Rodrigues, and Évora (Citation2009) stated that participants were patients undergoing valvuloplasty or myocardial revascularization. The term “myocardial revascularization” was not defined. A summary of all study characteristics can be seen in .
Table 1. A summary of the study population of the seven studies reviewed.
Intervention
All studies assessed the use of preoperative threshold inspiratory muscle training in patients undergoing cardiac surgery. The same type of device for threshold inspiratory muscle training (Threshold Inspiratory Muscle Trainer) was used in all studies. A summary of all study interventions can be seen in .
Table 2. A summary of the intervention used in each study.
Inspiratory load
The baseline maximal inspiratory pressures of participants were measured prior to training in all studies. Four studies (Chen et al., Citation2019; Hulzebos et al., Citation2006a, Citation2006b; Valkenet et al., Citation2017) used an inspiratory load at 30% of the maximal inspiratory pressure, while two studies (Ferreira, Rodrigues, and Évora, Citation2009; Sobrinho, Guirado, and Silva, Citation2014) set the load at 40% and one (Savci et al., Citation2011) at 15%.
Five studies (Chen et al., Citation2019; Hulzebos et al., Citation2006a, Citation2006b; Savci et al., Citation2011; Valkenet et al., Citation2017) increased the inspiratory load incrementally. Chen et al. (Citation2019) and both studies by Hulzebos et al. (Citation2006a); Hulzebos et al. (Citation2006b) based the decision to increase the load on the rate of perceived exertion of participants, using the Borg CR-10 Scale (Borg, Citation1982). The Borg Scale is based on the intensity of exertion perceived by the individual, correlating with physiological parameters such as heart rate and blood lactate levels (Borg, Citation1982). In the two studies in which this scale was used, inspiratory load was increased when the rate of perceived exertion was less than five. It is thought that scores close to five can be used to quantify the anaerobic threshold during exercise (Zamunér et al., Citation2011).
Duration and frequency of inspiratory muscle training
Training duration varied between 5 and 15 days in the preoperative period. All studies specified that the training in the preoperative period was undertaken up until the date of surgery, except Savci et al. (Citation2011) and Hulzebos et al. (Citation2006a). These studies did not state at what point in the preoperative period the training was undertaken. The frequency of training ranged from once a day to three times a day. Two studies (Sobrinho, Guirado, and Silva, Citation2014; Valkenet et al., Citation2017) did not specify the duration of training.
Control intervention design
In all studies, the control group received standard care before cardiac surgery. This consisted of patient education prior to surgery including information about early mobilization, coughing with wound support, and in three studies, instructions for deep breathing exercises (Ferreira, Rodrigues, and Évora, Citation2009; Hulzebos et al., Citation2006a; Savci et al., Citation2011).
In the paper by Chen et al. (Citation2019), participants in both the intervention and control groups received inspiratory muscle training. However, although the control group received the same duration, repetitions, frequency and supervision of training as the intervention group, the inspiratory load was fixed at the minimum load of the device (9 cmH2O). In contrast, the intervention group used the device set at 30% of maximal inspiratory pressure.
Outcomes
Length of hospital stay
Length of stay (LoS) in all studies referred to postoperative hospital stay. LoS was measured in days except for the study by Sobrinho, Guirado, and Silva (Citation2014) which recorded the stay in minutes. Valkenet et al. (Citation2017) and Ferreira, Rodrigues, and Évora (Citation2009) did not measure LoS as an outcome.
Postoperative pulmonary complications
The incidence of postoperative pulmonary complications was investigated as a primary outcome by Chen et al. (Citation2019) and Hulzebos et al. (Citation2006b). An investigator in each of these studies graded subjects from 1 to 4 using an operational definition of postoperative pulmonary complications devised by Kroenke (Citation1992). All studies investigating postoperative pulmonary complications reported the incidence of postoperative pneumonia. Hulzebos et al. (Citation2006a) also reported the incidence of atelectasis. Sobrinho, Guirado, and Silva (Citation2014) and Valkenet et al. (Citation2017) did not report on postoperative pulmonary complications.
Quality of life
Only two studies directly reported the effect of preoperative inspiratory muscle training on postoperative quality of life (QoL). Valkenet et al. (Citation2017) investigated health-related QoL scores by secondary analysis of participants from the Hulzebos et al. (Citation2006b) study. The Medical Outcomes Study Short Form 36-Item Questionnaire (SF-36) and the Euroqol 5 Dimensions 3 Level Questionnaire (EQ-5D-3 L) were used.
The study conducted by Savci et al. (Citation2011) used the Nottingham Health Profile to report postoperative QoL in patients who received inspiratory muscle training before CABG surgery. This questionnaire measures emotional reactions, energy, physical mobility, pain, sleep and social isolation. In addition, anxiety and depression were measured using the Hospital Anxiety and Depression Scale.
Mortality
Two studies reported on all-cause deaths within the study groups, however mortality was not measured as an outcome in either study. Ferreira, Rodrigues, and Évora (Citation2009) recorded four deaths in the 30-day period after hospital discharge. Hulzebos et al. (Citation2006b) reported four deaths in the control group after surgery.
Risk of bias
All studies randomized participants to intervention or control, but two studies did not state how this was done (Ferreira, Rodrigues, and Évora, Citation2009; Valkenet et al., Citation2017). Three studies provided no detail regarding any concealment process or whether it had occurred at all (Ferreira, Rodrigues, and Évora, Citation2009; Hulzebos et al., Citation2006a; Valkenet et al., Citation2017). The study by Valkenet et al. (Citation2017) reported a secondary analysis of the Hulzebos et al. (Citation2006b) study data, however, it should be noted that the study was assessed for risk of bias as a standalone publication. Had the original paper been considered simultaneously, Valkenet et al. (Citation2017) would have achieved a low risk of bias for the first domain.
Studies that reported the effect of assignment to intervention (intention-to-treat) were assessed for risk of bias in this area using domain 2a. Those that did not use intention-to-treat analysis were assessed using domain 2b. For two studies (Ferreira, Rodrigues, and Évora, Citation2009; Sobrinho, Guirado, and Silva, Citation2014), it was difficult to ascertain which type of analysis had been performed. In these cases, the studies were assessed under both domains as a precaution. Chen et al. (Citation2019) was the only study to describe the possible blinding of participants from the intervention group, by introducing a sham therapy, however intervention providers are likely to have been unblinded in all studies. Most studies did not provide any specific information regarding important non-protocol interventions or non-adherence, whereas Hulzebos et al. (Citation2006b) stated that three patients died during the study, thus introducing bias by not taking into account patients with more severe illness or co-morbidity, contributing to a poor prognosis.
Most studies were regarded as low risk in domain 3. Sobrinho, Guirado, and Silva (Citation2014) was the only study to have a high risk of bias, due to a lack of any information regarding dropouts from the study. Results for the RoB-2 and SIGN Critical Appraisal for each study can be seen in .
Table 3. Summary of RoB-2 Bias analysis.
Table 4. Summary of SIGN critical appraisal.
Effect of inspiratory muscle training
Length of stay
In the five studies which assessed the length of postoperative hospital stay (LoS), all reported a shorter LoS in the intervention group. The average difference ranged between 0.61 and 1.99 days. However, the LoS was statistically significantly shorter in the intervention group compared to control in only three of these studies (Chen et al., Citation2019; Hulzebos et al., Citation2006b; Sobrinho, Guirado, and Silva, Citation2014). The average difference in LoS between control and intervention groups in these studies ranged between 1.06 and 1.87 days ().
Table 5. Summarizing the length of stay (LoS) as a primary outcome for six of the studies analyzed.
Postoperative pulmonary complications
Both studies which measured postoperative pulmonary complications using the criteria by Kroenke (Citation1992) and reported the incidence of postoperative pulmonary complications at Grade 2 or above found a statistically significant lower incidence in the intervention group compared to the control group (Chen et al., Citation2019; Hulzebos et al., Citation2006b). Of the studies reporting on the incidence of pneumonia, only one study (Hulzebos et al., Citation2006b) reported a statistically significant result, with a significantly reduced incidence of pneumonia in the intervention group (6.5%) compared to the control group (16.1%) (p= 0.01). Hulzebos et al. (Citation2006a) reported a lower incidence of atelectasis in the intervention group compared to the control group (p= 0.05). Overall, three studies reported significant reductions in postoperative pulmonary complications. These results are summarized in .
Table 6. Summary of postoperative pulmonary complications (PPCs) reported in the studies.
Quality of life
Valkenet et al. (Citation2017) reported that all QoL scores significantly improved (p< 0.05) at 2 weeks, and again at 3 months after surgery, regardless of whether participants had been allocated to the intervention or control group. No further improvements were noted 6 months postoperatively and there was no difference in QoL scores between intervention and control groups at any time point.
All patients who received inspiratory muscle training in the study by Savci et al. (Citation2011) showed improvement in sleep, regardless of allocation to the intervention or control groups. This improvement was statistically significantly greater (p< 0.05) in the intervention cohort compared to the control. There was no statistical difference in any of the other domains. The average of the anxiety scores in the intervention group decreased after surgery, however, the average increased in the control group. This difference between the intervention and control groups was statistically significant (p< 0.05).
Mortality
Ferreira, Rodrigues, and Évora (Citation2009) reported a 30-day all-cause mortality rate of 6.7% (one out of 15 participants) in the control group and 20% (three out of 15 participants) in the intervention group, however this was not significantly different (p> 0.05). The only other study to report all-cause mortality was Hulzebos et al. (Citation2006b). No time point at which these deaths occurred was stated. This study reported no deaths in the intervention group, but three out of 137 control participants died (2.9%). Again, this was not significant.
Discussion
Overview of results
This systematic review of seven randomized controlled trials identified that preoperative threshold inspiratory muscle training in adults undergoing cardiac surgery reduced the length of postoperative hospital stay in three out of five of the studies, and postoperative pulmonary complications in three out of five of the studies. The evidence for quality of life and mortality was inconclusive.
Our primary outcome measure was length of postoperative hospital stay, and our results suggest that preoperative threshold inspiratory muscle training has the potential to reduce postoperative length of stay in adults undergoing cardiac surgery.
Hospital stay
Our finding that preoperative threshold inspiratory muscle training significantly reduced post-operative length of stay in patients undergoing cardiac surgery in three out of five studies is in line with a systematic review conducted by Gomes Neto, Martinez, Reis, and Carvalho (Citation2017). The study reported a two day decrease in postoperative length of stay; however, this finding is based on the results from only four studies. Our review identified an average difference in postoperative length of hospital stay between control and intervention groups between 1.06 and 1.87 days. This could be assumed to be accounted for by a reduced incidence of postoperative pulmonary complications, which are known to be a significant determinant of prolonged postoperative hospital stay (Almashrafi et al., Citation2016).
The three studies which reported a significant decrease in length of postoperative hospital stay had the largest study populations of the five studies assessing this outcome. The two studies which did not report significant differences had particularly small study populations (Hulzebos et al., Citation2006a; Savci et al., Citation2011). The study by Hulzebos et al. (Citation2006a) included 26 participants, and the study by Savci et al. (Citation2011) included 43 participants. It is therefore possible that the studies were underpowered.
Influence of bias
All papers had at least “some concerns” with bias upon analysis using the Cochrane Risk-of-Bias tool (RoB-2) checklist (Sterne et al., Citation2019). The baseline characteristics of participants in the study by Sobrinho, Guirado, and Silva (Citation2014) focused on a subset of only 10 patients in each cohort, instead of the full 35 that were analyzed, and only considered age, sex and BMI. This raises concerns about the presence of unequal baseline characteristics in the two groups.
Another important consideration is that of the underlying risk of postoperative pulmonary complications in each study population. Savci et al. (Citation2011) only included patients at low risk for postoperative pulmonary complications. This may account for the findings; the study reported a zero incidence of pulmonary complications in both intervention and control groups and found no significant difference in length of postoperative hospital stay.
Hulzebos et al. (Citation2006a); Hulzebos et al. (Citation2006b), on the other hand, included only high-risk patients. The earlier study by Hulzebos et al. (Citation2006a) did not find a statistically significant difference in the duration of postoperative hospital stay between the intervention and control groups. This could be accounted for due to the small sample size. The second larger study did, however, report a lower LoS in the intervention group. Both of these papers also found statistically significantly lower incidence of postoperative pulmonary complications between groups. The authors could find no other systematic review exclusively investigating the effect of preoperative threshold inspiratory muscle training in cardiac surgical patients.
Inspiratory muscle training and respiratory muscle strength
Inspiratory muscle training can be categorized into resistance training and endurance training. Resistance training functions to increase respiratory muscle strength and is thus relevant in the context of inspiratory muscle weakness. Tension is generated in the muscle when a high-intensity load is placed on the muscle fibers for a short duration, and structural adaptations to the muscles occur (McConnell, Citation2013).
It is well established that cardiac surgery impairs pulmonary function, but there is ongoing debate in the literature as to the effects of cardiac surgery on respiratory muscle strength (Naseer, Al-Shenqiti, Ali, and Aljeraisi, Citation2019). Barros et al. (Citation2010) reported a reduction in respiratory muscle strength after cardiac surgery, however, a more recent study by Urell, Emtner, Hedenstrom, and Westerdahl (Citation2016) found no reduction of respiratory muscle strength after cardiac surgery. Pain affecting patients’ abilities to perform the tests in the postoperative period may account for reported reductions in respiratory muscle strength (Naseer, Al-Shenqiti, Ali, and Aljeraisi, Citation2019; Urell, Emtner, Hedenstrom, and Westerdahl, Citation2016). Nevertheless, a relationship between respiratory muscle strength and lung function, measured by inspiratory capacity, vital capacity and FEV1, has been demonstrated (Naseer, Al-Shenqiti, Ali, and Aljeraisi, Citation2019). This is significant as impairment of lung function is associated with atelectasis and pulmonary infections (Siafakas, Mitrouska, Bouros, and Georgopoulos, Citation1999).
Patients undergoing cardiac surgery may be susceptible to postoperative pulmonary complications due to underlying pulmonary disease or pulmonary dysfunction as a result of cardiac disease (Weissman, Citation2004). Inspiratory muscle weakness, measured by maximal inspiratory pressure (MIP), is often defined as an MIP of less than 70% of the predicted value, however this definition is not consistent across studies assessing inspiratory muscle weakness (D’Arx et al., Citation2020; Winkelmann et al., Citation2019). Research suggests that the choice of reference values in the context of equations used to predict MIP values strongly impacts on the prevalence of inspiratory muscle weakness (Rodrigues et al., Citation2017), thus comparison of predicted values must take this into account. Regarding studies included in our review, one (Hulzebos et al., Citation2006a) expressed the baseline MIP values as percentages of predicted values according to age and sex, meaning the actual MIP value was not stated, unlike in the other studies. Furthermore, there were differences in how the baseline MIP values were obtained during measurement. Thus, in this review, it is difficult to comment accurately on the prevalence of preoperative inspiratory muscle weakness, and by extension, relating this to the outcome of postoperative pulmonary complications.
Current literature highlights that the relationship between the development of postoperative pulmonary complications and inspiratory muscle strength before cardiac surgery remains unclear (D’Arx et al., Citation2020) and this raises interesting questions about to what extent improvements in respiratory muscle strength account for the reductions in postoperative pulmonary complications associated with inspiratory muscle training.
Preoperative physiotherapy regimes
Preoperative physiotherapy in the context of cardiac surgery has recognized benefits for improving postoperative outcomes, as demonstrated in studies by Nardi et al. (Citation2019) and Nardi et al. (Citation2020). These studies highlighted the potential of respiratory and motor physiotherapy protocols to improve respiratory function and reduce postoperative length of stay after cardiac surgery. A recently published best evidence analysis by Sandhu and Akowuah (Citation2019) further endorsed prehabilitation in the context of cardiac surgery. The outcomes of this analysis were that inspiratory muscle training had the most favorable evidence for reducing postoperative pulmonary complications and length of stay after cardiac surgery compared with other preoperative physiotherapy regimes. Further research is required, however, to assess the cost-effectiveness and feasibility of implementing inspiratory muscle training using threshold devices compared to other physiotherapy protocols.
Postoperative pulmonary complications
There is currently no standard definition of postoperative pulmonary complications and as such they are defined heterogeneously, encompassing a wide range of complications from surgery and anesthesia (Miskovic and Lumb, Citation2017). Postoperative pulmonary dysfunction is recognized as a common occurrence after cardiac surgery, attributed to hypoxemia, shallow breathing, ineffective cough and increased work of breathing (Wynne and Botti, Citation2004). Postoperative pain may impair the ability to cough effectively (Westerdahl, Jonsson, and Emtner, Citation2016), while the patient is predisposed to development of a cough or excessive sputum due to conditions typical of the postoperative period of extensive surgeries: posture, immobility and use of sedation or mechanical ventilation (de Sousa et al., Citation2012). The reported incidence, however, of severe pulmonary complications with clinical implications, such as pneumonia and atelectasis, is low (García-Delgado, Navarrete-Sánchez, and Colmenero, Citation2014). Thus, it is evident that comparison of the reported incidence of postoperative pulmonary complications across studies should therefore take into account the clinical significance of the complications.
Diagnosis and definition of postoperative pulmonary complications varied between the studies analyzed. Chen et al. (Citation2019) and Hulzebos et al. (Citation2006b) both used the operational definition devised by Kroenke (Citation1992) to grade postoperative pulmonary complications on a scale of 1–4, regarding any complication with two or more criteria from grade 2, or at least one from grade 3 or 4, as clinically significant. Complications were considered subclinical when there were no clinical symptoms or changes in auscultation, only abnormal radiological findings (e.g. grade 1). These criteria take into account both symptoms and clinical features of the patient, as well as radiological findings. Similarly, the earlier Hulzebos et al. study (Hulzebos et al., Citation2006a) used a set of criteria that took into account chest x-ray findings, temperature, auscultation and sputum production. In comparison, Savci et al. (Citation2011) used only radiological findings, however did regard any complications with no clinical features as “subclinical.” Ferreira, Rodrigues, and Évora (Citation2009) did not state their diagnostic criteria. The study by Chen et al. (Citation2019) and the two studies by Hulzebos et al. (Citation2006a); Hulzebos et al. (Citation2006b) found a statistically significant difference in postoperative pulmonary complications between cohorts in most of the areas assessed. Ferreira, Rodrigues, and Évora (Citation2009), conversely, did not find a statistically significant difference between their rates of pneumonia, and Savci et al. (Citation2011) recorded no incidences of pneumonia or atelectasis. Comparing these results and drawing conclusions is difficult when there are so many differences between the definitions and diagnostic criteria used.
Training regimes
Various different training regimes were used in each study, ranging from a frequency of once a day to three times a day, and a duration of five to 15 days. Chen et al. (Citation2019) and both studies by Hulzebos et al. (Citation2006a); Hulzebos et al. (Citation2006b) based the decision to increase the inspiratory load on the rate of perceived exertion of participants, using the Borg CR-10 Scale, if the rate of perceived exertion was less than five. The Borg CR-10 Scale was constructed based on exercise performed on a cycle ergometer, and not inspiratory muscle training (Borg, Citation1982). It is therefore possible that the rates of perceived exertion by participants did not correlate accurately with the scale. Furthermore, although it is thought that scores close to five can be used to quantify the anaerobic threshold during exercise, this evidence is based on exercise performed on a cycle ergometer (Zamunér et al., Citation2011). It is therefore evident that there was significant heterogeneity in the training regimes across the studies, highlighting the requirement for the optimum training regime to be determined.
Supervision of participant training
While our results show preoperative threshold inspiratory muscle training has the potential to reduce the length of postoperative hospitalization, additional contact with physiotherapists in the preoperative period is required to implement the training. In implementing the training, consideration must be taken to ensure accurate technique and patient adherence to the regime. This may therefore require several clinic appointments under supervision, either in the initial phase of training or for the duration of the training. Recognizably, there will be costs associated with clinic appointments in addition to the costs of the training equipment; this should be balanced with the limitations of home training in the context of ensuring standardization of the regime.
The degree of supervision by physiotherapists varied between studies. As can be seen from , Chen et al. (Citation2019), Savci et al. (Citation2011) and Sobrinho, Guirado, and Silva (Citation2014) noted that all training sessions were supervised. Hulzebos et al. (Citation2006a), Hulzebos et al. (Citation2006b) and Valkenet et al. (Citation2017) stated that training sessions were supervised once a week, and participants in the study by Ferreira, Rodrigues, and Évora (Citation2009) were not supervised. Work by Kendall et al. (Citation2018) showed that while no supervision of inspiratory muscle training regimes had no effect on postoperative outcomes, participants that were supervised weekly fared better in terms of postoperative length of stay, whereas those who were supervised daily experienced less postoperative pulmonary complications.
Opportunities for further study
This systematic review assessing the effect of preoperative threshold inspiratory muscle training solely in cardiac surgical patients has addressed a gap in the current literature, and has identified potential benefits of this form of preoperative training regarding postoperative outcomes. This review did not assess the effect of the intervention on inspiratory muscle strength in the context of postoperative outcomes, so a sensitivity analysis addressing this topic remains an opportunity for further study. Prospective registration with PROSPERO was not undertaken, which is a recognized limitation of this review. Additionally, the scope of this review did not cover a cost-effectiveness analysis. Future research should consider the cost effectiveness of threshold inspiratory muscle training as other physiotherapy protocols have demonstrated potential in improving postoperative outcomes (Nardi et al., Citation2019, Citation2020).
Conclusion
The results from this systematic review suggest that preoperative threshold inspiratory muscle training has potential to reduce postoperative length of hospital stay and pulmonary complications in adults following cardiac surgery. Research on the effects on quality of life and mortality is inconclusive. These findings may be influenced by bias identified across all papers. Further high-quality research is therefore required to establish the clinical significance of inspiratory muscle training; to identify the most beneficial training regime; and to determine whether the cost effectiveness is such that threshold inspiratory muscle training should be recommended to adults undergoing cardiac surgery.
Supplemental Material
Download MS Word (12.5 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Almashrafi A, Alsabti H, Mukaddirov M, Balan B, Aylin P 2016 Factors associated with prolonged length of stay following cardiac surgery in a major referral hospital in Oman: A retrospective observational study. Open 6: e010764. DOI:10.1136/bmjopen-2015-010764
- Badenes R, Lozano A, Belda F 2015 Postoperative pulmonary dysfunction and mechanical ventilation in cardiac surgery. Critical Care Research and Practice 2015: 420513. DOI:10.1155/2015/420513
- Barros G, Santos C, Granado F, Costa P, Límaco R, Gardenghi G 2010 Treinamento muscular respiratório na revascularização do miocárdio. Revista Brasileira de Cirurgia Cardiovascular 25: 483–490. DOI:10.1590/s0102-76382010000400011
- Beaumont M, Forget P, Couturaud F, Reychler G 2018 Effects of inspiratory muscle training in COPD patients: A systematic review and meta-analysis. Clinical Respiratory Journal 12: 2178–2188. DOI:10.1111/crj.12905
- Borg G 1982 Psychophysical basis of perceived exertion. Medicine and Science in Sports and Exercise 14: 377–381. DOI:10.1249/00005768-198205000-00012
- Casali C, Pereira A, Martinez J, de Souza H, Gastaldi A 2011 Effects of inspiratory muscle training on muscular and pulmonary function after bariatric surgery in obese patients. Obesity Surgery 21: 1389–1394. DOI:10.1007/s11695-010-0349-y
- Chen X, Hou L, Zhang Y, Liu X, Shao B, Yuan B, Li J, Li M, Cheng H, Teng L, et al. 2019 The effects of five days of intensive preoperative inspiratory muscle training on postoperative complications and outcome in patients having cardiac surgery: A randomized controlled trial. Clinical Rehabilitation 33: 913–922. DOI10.1177/0269215519828212
- D’Arx A, Freene N, Bowen S, Bissaker P, McKay G, Bissett B 2020 What is the prevalence of inspiratory muscle weakness in preoperative cardiac surgery patients? An observational study. Heart and Lung 49: 909–914.
- de Medeiros A, Fuzari H, Rattesa C, Brandão D, de Melo Marinho P 2017 Inspiratory muscle training improves respiratory muscle strength, functional capacity and quality of life in patients with chronic kidney disease: A systematic review. Journal of Physiotherapy 63: 76–83. DOI:10.1016/j.jphys.2017.02.016
- de Sousa V, de Oliveira Lopes M, de Araujo T, Rolim I, Do Nascimento R, Oliveira T 2012 Clinical indicators of ineffective airway clearance for patients in the cardiac postoperative period. European Journal of Cardiovascular Nursing 12: 193–200. DOI:10.1177/1474515112443931
- Ferreira P, Rodrigues A, Évora P 2009 Effects of an inspiratory muscle rehabilitation program in the postoperative period of cardiac surgery. Arquivos Brasileiros de Cardiologia 92: 275–282. DOI:10.1590/s0066-782x2009000400005
- García-Delgado M, Navarrete-Sánchez I, Colmenero M 2014 Preventing and managing peri-operative pulmonary complications following cardiac surgery. Current Opinion in Anaesthesiology 27: 146–152. DOI:10.1097/ACO.0000000000000059
- Ge X, Wang W, Hou L, Yang K, Fa X 2018 Inspiratory muscle training is associated with decreased postoperative pulmonary complications: Evidence from randomized trials. Journal of Thoracic and Cardiovascular Surgery 156: 1290–1300. DOI:10.1016/j.jtcvs.2018.02.105
- Gomes Neto M, Martinez B, Reis H, Carvalho V 2017 Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: Systematic review and meta-analysis. Clinical Rehabilitation 31: 454–464. DOI:10.1177/0269215516648754
- Hauck K, Zhao X 2011 How dangerous is a day in hospital?. Medical Care 49: 1068–1075. DOI:10.1097/MLR.0b013e31822efb09
- Hulzebos E, Helders P, Favié N, De Bie R, Brutel de La Riviere A, Van Meeteren N 2006a Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery. JAMA 296: 1851–1857. DOI:10.1001/jama.296.15.1851
- Hulzebos E, van Meeteren N, van Den Buijs B, de Bie R, de La Rivière A, Helders P 2006b Feasibility of preoperative inspiratory muscle training in patients undergoing coronary artery bypass surgery with a high risk of postoperative pulmonary complications: A randomized controlled pilot study. Clinical Rehabilitation 20: 949–959. DOI:10.1177/0269215506070691
- Karanfil E, Møller A 2018 Preoperative inspiratory muscle training prevents pulmonary complications after cardiac surgery - A systematic review. Danish Medical Journal 65: A5450.
- Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa T 2015 Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database of Systematic Reviews 10: CD010356. DOI:10.1002/14651858.CD010356.pub2
- Kendall F, Oliveira J, Peleteiro B, Pinho P, Bastos P 2018 Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: A systematic review and meta-analysis. Disability and Rehabilitation 40: 864–882. DOI:10.1080/09638288.2016.1277396
- Kroenke K 1992 Operative risk in patients with severe obstructive pulmonary disease. Archives of Internal Medicine 152: 967–971. DOI:10.1001/archinte.1992.00400170057011
- Lin S, McElfresh J, Hall B, Bloom R, Farrell K 2012 Inspiratory muscle training in patients with heart failure: A systematic review. Cardiopulmonary Physical Therapy Journal 23: 29–36. DOI:10.1097/01823246-201223030-00005
- Mans C, Reeve J, Elkins M 2015 Postoperative outcomes following preoperative inspiratory muscle training in patients undergoing cardiothoracic or upper abdominal surgery: A systematic review and meta-analysis. Clinical Rehabilitation 29: 426–438. DOI:10.1177/0269215514545350
- McConnell A 2013 Respiratory Muscle Training. Edinburgh: Churchill Livingstone.
- McKenzie J, Brennan S, Ryan R, Thomson H, Johnston R, Thomas J 2019 Chapter 3: Defining the criteria for including studies and how they will be grouped for the synthesis. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, and Welch V Eds Cochrane Handbook for Systematic Reviews of Interventions version 6.0. 13 May 2020. Cochrane. www.training.cochrane.org/handbook
- Menzes K, Nascimento L, Avelino P, Polese J, Salmela L 2018 A review on respiratory muscle training devices. Journal of Pulmonary and Respiratory Medicine 8: 1000451.
- Miskovic A, Lumb A 2017 Postoperative pulmonary complications. British Journal of Anaesthesia 118: 317–334. DOI:10.1093/bja/aex002
- Moher D, Liberati A, Tetzlaff J, Altman D 2009 Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339: b2535. DOI:10.1136/bmj.b2535
- Nardi P, Pellegrino A, Pisano C, Vacirca S, Anselmi D, Saulle S, Dandi R, Romano A, Servadio A, Gianlorenzi A, et al. 2019 The effect of preoperative respiratory physiotherapy and motor exercise in patients undergoing elective cardiac surgery: Short-term results. Polish Journal of Cardio-Thoracic Surgery 16: 81–87. DOI10.5114/kitp.2019.86360
- Nardi P, Pisano C, Altieri C, Buioni D, Pedicelli C, Saulle S, Dandi R, Romano A, Servadio A, Gianlorenzi A, et al. 2020 The benefit of a preoperative respiratory protocol and musculoskeletal exercise in patients undergoing cardiac surgery. Polish Journal of Cardio-Thoracic Surgery 17: 94–100. DOI10.5114/kitp.2020.97267
- Naseer B, Al-Shenqiti A, Ali A, Aljeraisi T 2019 Effect of cardiac surgery on respiratory muscle strength. Journal of Taibah University Medical Sciences 14: 337–342. DOI:10.1016/j.jtumed.2019.06.002
- Naveed A, Azam H, Ghulam Murtaza H, Altaf Ahmad R, Raza Baig M A 2017 Incidence and risk factors of pulmonary complications after cardiopulmonary bypass. Pakistan Journal of Medical Sciences 33: 993–996. DOI:10.12669/pjms.334.12846
- Paiva D, Assmann L, Bordin D, Gass R, Jost R, Bernardo-Filho M, França R, Cardoso D 2015 Inspiratory muscle training with threshold or incentive spirometry: Which is the most effective?. Revista Portuguesa de Pneumologia 21: 13 May2020. DOI:10.1016/j.rppnen.2014.05.005
- Rodrigues A, Da Silva M, Berton D, Cipriano G, Pitta F, O’Donnell D, Neder J 2017 Maximal inspiratory pressure. Chest 152: 32–39. DOI:10.1016/j.chest.2016.11.045
- Sabaté S, Mazo V, Canet J 2014 Predicting postoperative pulmonary complications. Current Opinion in Anaesthesiology 27: 201–209. DOI:10.1097/ACO.0000000000000045
- Sandhu M, Akowuah E 2019 Does prehabilitation improve outcomes in cardiac surgical patients?. Interactive Cardiovascular and Thoracic Surgery 29: 608–611. DOI:10.1093/icvts/ivz131
- Savci S, Degirmenci B, Saglam M, Arikan H, Inal-Ince D, Turan H, Demircin M 2011 Short-term effects of inspiratory muscle training in coronary artery bypass graft surgery: A randomized controlled trial. Scandinavian Cardiovascular Journal 45: 286–293. DOI:10.3109/14017431.2011.595820
- Scottish Intercollegiate Guidelines Network 2020 Methodology checklist 1: Systematic reviews and meta-analyses. SIGN. 14 May 2020. Edinburgh, UK. https://www.sign.ac.uk/media/1721/srchecklist.doc
- Seese L, Sultan I, Gleason T, Navid F, Wang Y, Thoma F Kilic A 2020 The impact of major postoperative complications on long-term survival after cardiac surgery. Annals of Thoracic Surgery 110: 128–135. DOI:10.1016/j.athoracsur.2019.09.100
- Siafakas N, Mitrouska I, Bouros D, Georgopoulos D 1999 Surgery and the respiratory muscles. Thorax 54: 458–465. DOI:10.1136/thx.54.5.458
- Sobrinho M, Guirado G, Silva M 2014 Preoperative therapy restores ventilatory parameters and reduces length of stay in patients undergoing myocardial revascularization. Revista Brasileira de Cirurgia Cardiovascular 29: 221–228. DOI:10.5935/1678-9741.20140021
- Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, Cates C, Cheng H, Corbett M, Eldridge S, et al. 2019 RoB 2: A revised tool for assessing risk of bias in randomized trials. BMJ 366: l4898. DOI10.1136/bmj.l4898
- Urell C, Emtner M, Hedenstrom H, Westerdahl E 2016 Respiratory muscle strength is not decreased in patients undergoing cardiac surgery. Journal of Cardiothoracic Surgery 11: 41. DOI:10.1186/s13019-016-0433-z
- Valkenet K, Trappenburg J, Hulzebos E, van Meeteren N, Backx F 2017 Effects of a pre-operative home-based inspiratory muscle training programme on perceived health-related quality of life in patients undergoing coronary artery bypass graft surgery. Physiotherapy 103: 276–282. DOI:10.1016/j.physio.2016.02.007
- Weissman C 2004 Pulmonary complications after cardiac surgery. Seminars in Cardiothoracic and Vascular Anesthesia 8: 185–211. DOI:10.1177/108925320400800303
- Westerdahl E, Jonsson M, Emtner M 2016 Pulmonary function and health-related quality of life 1-year follow up after cardiac surgery. Journal of Cardiothoracic Surgery 11: 99. DOI:10.1186/s13019-016-0491-2
- Winkelmann E, É S, Windmöller P, Fontela P, Cruz D, Battisti I 2019 Preoperative expiratory and inspiratory muscle weakness to predict postoperative outcomes in patients undergoing elective cardiac surgery. Journal of Cardiac Surgery 35: 128–134. DOI:10.1111/jocs.14355
- Wynne R 2004 Variable definitions: Implications for the prediction of pulmonary complications after adult cardiac surgery. European Journal of Cardiovascular Nursing 3: 43–52. DOI:10.1016/j.ejcnurse.2003.11.001
- Wynne R, Botti M 2004 Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: Clinical significance and implications for practice. American Journal of Critical Care 13: 384–393. DOI:10.4037/ajcc2004.13.5.384
- Zamunér A, Moreno M, Camargo T, Graetz J, Rebelo A, Tamburús N, Da Silva E 2011 Assessment of subjective perceived exertion at the anaerobic threshold with the Borg CR-10 Scale. Journal of Sports Science & Medicine 10: 130–136.
Appendix A
– Search Method
1.Database Searched: Ovid Embase 1996 to 2020 Week 18
Search Terms used:
Inspiratory muscle training
AND
Cardiac Surgery.mp. OR Heart Surgery
AND
Adult
Limits Added: Randomized Control Trials; Humans
2.Database Searched: Google Scholar
Search Terms used:
Inspiratory muscle training
AND
Cardiac Surgery
AND
Preoperative
Limits Added: Randomized Control Trials
3.Database Searched: Ovid MedLine (1946 to April Week 52,020)
Search Terms used:
Inspiratory muscle training
AND
Cardiac OR Heart
AND
Surgery
AND
Preoperative
Limits Added: Randomized Control Trials
4.Database Searched: PubMed Central
Search Terms used:
Inspiratory muscle training
AND
Cardiac
AND
Surgery
AND
Preoperative
Limits Added: Randomized Control Trials; Humans
5.Database Searched: Scopus
Search Terms used:
Inspiratory muscle training
AND
Cardiac Surgery
Limits Added: Randomized Control Trials; Humans
