ABSTRACT
Postural instability in Parkinson’s disease (PD) is associated with several downstream consequences that ultimately lead to a greater risk of falling. Among the prominent downstream consequences is fear of falling (FOF), which is both common and problematic in PD. It can lead to a vicious cycle of FOF avoidance behavior that results in more sedentary behavior, physical deconditioning, and weakening of already impaired balance systems. This, in turn, may make the person with PD more susceptible to a future fall even with benign daily tasks. While FOF activity avoidance can be adaptive (appropriate), it can also be maladaptive (inappropriate or exaggerated). When this adaptive and maladaptive FOF avoidance behavior is contextualized to gait/balance performance, it provides a theoretical framework that can be used by clinicians to match patterns of behavior to a concordant treatment approach. In the theoretical framework proposed in this perspective, four different patterns related to FOF avoidance behavior and gait/balance performance are suggested: appropriate avoiders, appropriate non-avoiders, inappropriate avoiders, and inappropriate non-avoiders. For each of the four FOF avoidance behavior patterns, this paper also provides suggested treatment focuses, approaches and recommendations.
Background
Over the years, several guidelines and theoretical frameworks in Parkinson’s disease (PD) have been developed to help physical therapists to organize treatment goals and strategies, and to consolidate current evidence to the progressive nature of the disease. Most of the guidelines and some process frameworks have taken a comprehensive and general approach to physical therapy and exercise across disease severity (Keus et al., Citation2014; Rafferty, Nettnin, Goldman, and MacDonald, Citation2021). However, some frameworks have taken a more narrow, theoretical approach based on treatment strategies like task-specific training (Morris, Citation2000); or PD-specific signs and symptoms such as: freezing of gait (Delgado-Alvarado et al., Citation2020; Ginis, Nackaerts, Nieuwboer, and Heremans, Citation2018); and gait and balance impairment (Conradsson et al., Citation2012; Mille et al., Citation2012; Morris, Citation2006). While these guidelines and theoretical frameworks have helped clinicians in their clinical-decision making, there have been no theoretical treatment frameworks addressing fear of falling (FOF) and FOF avoidance behavior in PD. To our knowledge, the theoretical framework presented in this paper is the first to address this common and problematic consequence of postural instability in PD. Moreover, it is our proposition that the framework proposed in this perspective will promote future research studies and complement clinical-decision making and, ultimately, result in improved treatment outcomes.
Falling and Parkinson’s disease
Postural instability, which is a cardinal sign in PD, is a causative factor for falls and a prominent contributor to premature morbidity and mortality in PD (Macleod, Taylor, and Counsell, Citation2014; Pinter et al., Citation2015). Postural instability is also mostly non-responsive to PD medication (Baer et al., Citation2018; Crouse, Phillips, Jahanshahi, and Moustafa, Citation2016; Curtze et al., Citation2015) and worsens as the disease progresses. In a systematic review by Allen, Schwarzel, and Canning (Citation2013) 35% to 90% of people with PD report at least one fall per year with recurrent falls accounting for 39%. A relatively recent study on the natural history of falls in PD found that 79.7% fell at least once over a 54-month period (Lord et al., Citation2017). The sequelae of events after a fall include decreased function and quality of life, an increased risk of hospital/nursing home admission, increased likelihood of injury and long-term disability, and increased mortality (Hely et al., Citation1999; Pickering et al., Citation2007; Soh et al., Citation2013; Temlett and Thompson, Citation2006). Collectively, these findings highlight the importance of developing treatment strategies to address the root causes and contributing factors.
While age-related fall risk factors are common among all groups, there are many fall risk factors that are unique in the PD population, including axial rigidity, dyskinesias, festination, and functional neurosurgery (i.e. deep brain stimulation) (Fasano et al., Citation2017). Researchers have also shown that slow gait speed/mobility, a cardinal manifestation of PD, is associated with falling (Almeida et al., Citation2021; Canning, Paul, and Nieuwboer, Citation2014; Fasano et al., Citation2017; Lord et al., Citation2016). Additionally, fall history (Almeida et al., Citation2021; Canning, Paul, and Nieuwboer, Citation2014; Paul et al., Citation2014a); freezing of gait (Almeida et al., Citation2021; Canning, Paul, and Nieuwboer, Citation2014; Paul et al., Citation2014a, Citation2014b); and dyskinesias (Paul et al., Citation2014b) have been associated with future falls. In addition to those, researchers have reported that the following were also related to recurrent falling in PD: increased PD severity and duration; increased motor impairment; increased levodopa usage; cognitive impairment; reduced physical activity; impaired mobility; and FOF (Allen, Schwarzel, and Canning, Citation2013). While there are many factors associated with falls in PD, FOF may be one of the most debilitating because it is associated with significant negative downstream consequences.
Fear of falling
Fear of falling is a related but different construct from balance confidence and balance self-efficacy, but some consider FOF as an umbrella term. It is common in the elderly and develops in about one-third of individuals who have experienced a fall (Vellas et al., Citation1997). As falling is common in PD, people with PD also have high FOF prevalence rates with estimates ranging from 37% to 59% (Bloem et al., Citation2001; Dennison et al., Citation2007; Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Matinolli et al., Citation2009; Nilsson, Drake, and Hagell, Citation2010; Nilsson et al., Citation2010). FOF also appears to increase as PD progresses with one recent prospective study reporting an increased prevalence of FOF from 40% to 55% over three years’ time (Lindh-Rengifo et al., Citation2019). In addition, the severity of FOF also increases over time in people with PD (Gazibara et al., Citation2019; Lindh-Rengifo et al., Citation2019). Several studies have shown that a history of falls is not significantly associated with FOF in people with PD (Jonasson et al., Citation2015; Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Lindh-Rengifo et al., Citation2019; Mak, Pang, and Mok, Citation2012; Nilsson, Hariz, Iwarsson, and Hagell, Citation2012). However, one study by Gazibara et al. (Citation2019) suggested that the number of falls seems to be of importance for future FOF in PD.
Whatever the cause, FOF may serve a useful purpose in that it may heighten self-awareness about adaptive strategies to prevent a future fall. However, in some cases, FOF may be maladaptive in that it may stimulate a vicious cycle of deconditioning thereby making the person more susceptible to a future fall (Landers et al., Citation2021). In support of this, researchers have demonstrated that FOF in PD is independently associated with a higher risk of sustaining a future fall (Lindholm, Hagell, Hansson, and Nilsson, Citation2015; Mak and Pang, Citation2009); however, it is not clear if FOF is directly or indirectly linked to fall risk.
Because FOF is the self-perception that one is more susceptible to a fall, it is logical that the person may have accurately perceived a weakened balance system. On the other hand, it is also possible that cognitive processes may have influenced one’s ability to accurately perceive or interpret the current state of one’s balance capability and this can result in a mismatch between actual balance performance and an appropriate FOF self-perception. Two cross-sectional PD studies showed that cognitive functioning had an effect on FOF (Chomiak et al., Citation2018; Gazibara et al., Citation2013), and Chomiak et al. (Citation2018) demonstrated that this persisted even after adjusting for motor impairments. However, other studies have shown no effect of cognition on FOF in PD (Jonasson et al., Citation2015; Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Lindh-Rengifo et al., Citation2019).
Because FOF is a self-perception, it is logical that people with PD who have FOF also may have more profound psychological co-morbidities, including depression, anxiety, and catastrophization (Landers et al., Citation2017). For instance, depression in PD has been shown to be more associated with FOF than balance performance and the use of mobility devices (Franzen, Conradsson, Hagstromer, and Nilsson, Citation2016). In addition, researchers have reported that anxiety was associated with fall-related activity avoidance in people with PD (Rahman, Griffin, Quinn, and Jahanshahi, Citation2011). Taken together, these studies suggest that FOF is a complex self-perception that may involve other cognitive and affective processes.
Physical processes, like gait and balance problems, likely play the largest role in the development of FOF. Several studies have shown that perceived walking difficulties were the strongest contributing factor to FOF in people with PD (Jonasson et al., Citation2015; Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Lindh-Rengifo et al., Citation2019; Nilsson, Hariz, Iwarsson, and Hagell, Citation2012). In addition to walking difficulties, researchers have shown that that: fatigue (Jonasson et al., Citation2015; Lindholm, Hagell, Hansson, and Nilsson, Citation2014); balance performance (Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Lindh-Rengifo et al., Citation2019); motor symptoms (Jonasson et al., Citation2015); age (Jonasson et al., Citation2015); and the need for help in daily activities (Lindholm, Hagell, Hansson, and Nilsson, Citation2014; Lindh-Rengifo et al., Citation2019; Nilsson, Hariz, Iwarsson, and Hagell, Citation2012) were most associated with FOF (Lindholm, Hagell, Hansson, and Nilsson, Citation2014). While the aforementioned studies suggest that FOF is associated with motor and non-motor PD symptoms, the relationship with cognitive dimensions (e.g. balance problems during dual tasking) (Lindh-Rengifo et al., Citation2019) highlights a complex interaction that parallels a similar interaction between physical and cognitive factors in falls and postural instability in PD (Allen, Schwarzel, and Canning, Citation2013; Crouse, Phillips, Jahanshahi, and Moustafa, Citation2016). Importantly, FOF has been reported to be a barrier to engaging in exercise (Ellis et al., Citation2013) which is one of the few evidence-based approaches along with physical therapy that has been shown to improve: cognitive function (Dauwan et al., Citation2021); affective function (Adamson, Ensari, and Motl, Citation2015; Dauwan et al., Citation2021; Jayakody, Gunadasa, and Hosker, Citation2014; Wu, Lee, and Huang, Citation2017); physical function (i.e. gait/balance) (Klamroth, Steib, Devan, and Pfeifer, Citation2016; Uhrbrand, Stenager, Pedersen, and Dalgas, Citation2015); and falls in older adults (Sherrington et al., Citation2019) and people with PD (Shen, Wong-Yu, and Mak, Citation2016).
Fear of falling avoidance behavior
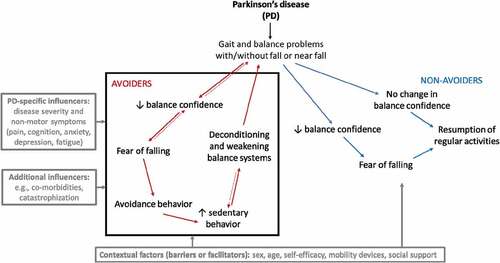
Some people with PD who experience a fall or near fall do not develop FOF (Howland et al., Citation1993), which usually results in a return to regular routines. Thus, they maintain their regular activities that help preserve their strength, endurance, and balance. Some may develop FOF but do not alter their normal routines or activities. Collectively, those that resume normal activities are referred to as non-avoiders (). However, in other cases, FOF can result in a change of behavior wherein one may avoid activities that put them at risk for a fall. This response pattern may be either adaptive or maladaptive. An appropriate adaptive response is one in which the person avoids appropriately risky balance activities. Naturally, this would decrease the risk and incidence of a future fall because the person is avoiding the activity that is perceived to expose them to a higher risk. Thus, their exposure to “risky” balance tasks would be less than a non-avoider and, subsequently, they would fall less. In support of this notion was a PD study that reported no differences in fall history between avoiders and non-avoiders despite poorer balance, gait, and motor performance in the avoiders (Landers et al., Citation2017). This suggests that avoidance behavior can have a positive effect on fall history. Moreover, people with PD and no fall history still report FOF avoidance behavior even in early disease stages (Hoehn and Yahr stages I–II) (Kader, Iwarsson, Odin, and Nilsson, Citation2016). While falls are not a prerequisite for developing avoidance behavior, others have shown that PD fallers spend more time in sedentary behavior and less time standing than PD non-fallers (Hiorth et al., Citation2016).
Figure 1. A conceptual model of the vicious cycle of fear of falling avoidance behavior (black box).
Avoidance behavior due to FOF is common in PD with studies reporting that 44.1% (Bloem et al., Citation2001) and up to 70% having avoided activities due to it (Brozova, Stochl, Roth, and Ruzicka, Citation2009; Kader, Iwarsson, Odin, and Nilsson, Citation2016). These data warrant investigation into related and predictive factors associated with it. A recent longitudinal study identified several predictive factors of FOF avoidance behavior in people with PD, including FOF, pain, unsteadiness while turning, and perceived walking difficulties (Nilsson, Jonasson, and Zijlstra, Citation2020). They also reported that both the prevalence (i.e. 34% vs 50%) and the severity of activity avoidance increased in people with PD after three years. As FOF is linked to avoidance behavior, these predictive variables support the notion that avoidance behavior is related to a self-perception of poor gait and balance.
Vicious cycle of fear of falling avoidance behavior
FOF can also trigger exaggerated or disproportionate avoidance behavior which may be more likely associated with affective processes, including anxiety and catastrophization (i.e. imagining the worst-case scenario), both of which figure prominently in contemporary understanding of fear. While activity avoidance can be adaptive (i.e. appropriate) it can also be maladaptive (i.e. inappropriate or disproportionate). In either case, the most important reason for the necessity of this theoretical framework and for developing treatment strategies, is that avoidance behavior can stimulate a vicious cycle, which may put one at an even greater risk for a future fall because of deconditioning and weakening of balance systems () (Brozova, Stochl, Roth, and Ruzicka, Citation2009; Dennison et al., Citation2007; Landers et al., Citation2021; Matinolli et al., Citation2009).
The typical sequelae of FOF is avoidance behavior that causes more sedentary behavior which, in turn, causes further functional decline because of inactivity and deconditioning. Thus, a vicious cycle begins with deconditioning and weakness making one more susceptible to a future fall with progressively more benign balance tasks, which, in turn, broadens FOF, increases the scope of the avoidance behavior, and causes more profound deconditioning (). Evidence for the validity of this vicious cycle of FOF avoidance behavior in PD using path analysis has recently been reported in the literature and it suggests that FOF and avoidance behavior can eventually make postural instabilty in PD worse (Landers et al., Citation2021). This vicious cycle is further complicated by PD-specific influencers (), like disease severity and non-motor symptoms (e.g. pain, cognition, anxiety, depression, and fatigue). For instance, PD fatigue is a strong contributor to decreased physical activity and exercise in PD (Garber and Friedman, Citation2003). Other influencers (e.g. co-morbities and catastrophization) may also logically influence some of the components of the vicous cycle. Lastly, contextual factors (e.g. sex, age, self-efficacy, mobility aids, and social support) can act as either barriers or facilitators to both avoiders and non-avoiders in their response to gait and balance impairment ().
Ultimately, this vicious cycle may increase the rate of disability and, subsequently, may decrease quality of life. People who avoid behavior from FOF may also begin to socially isolate themselves, which has been shown to negatively impact behavioral symptoms like sleep disturbances, depression, and fatigue (Choi, Irwin, and Cho, Citation2015). These behavioral symptoms, in turn, can theoretically also further contribute to more sedentary behavior. In addition to an increase in deconditioning and disability related to FOF avoidance behavior, sedentary behavior may cause secondary problems, diseases, or health conditions (Booth, Roberts, and Laye, Citation2012; Kohl et al., Citation2012). One additional problematic secondary problem of sedentary behavior and also a complication of PD itself is bone weakness (i.e. osteopenia and osteoporosis) (van Den Bos et al., Citation2013) which could potentiate the consequences of a fall.
Evidence demonstrating that avoidance behavior is associated with many negative downstream consequences is beginning to emerge in the PD literature and this highlights the need for a theoretical framework that can give guidance on how to mitigate avoidance behavior in the context of falls and gait/balance function. People with PD who report high FOF avoidance behaviors despite no difference in PD severity have more PD symptoms, more balance dysfunction (i.e. poorer performance and balance confidence), and poorer functional mobility than those who report low FOF avoidance behavior (Landers et al., Citation2017). Importantly, it has been shown that decreased physical activity from FOF increases susceptibility to a future fall and elevates the rate of disability, reduces quality of life, and hastens mortality in older adults and those with PD (Deshpande et al., Citation2008; Howland et al., Citation1993; Nilsson, Drake, and Hagell, Citation2010).
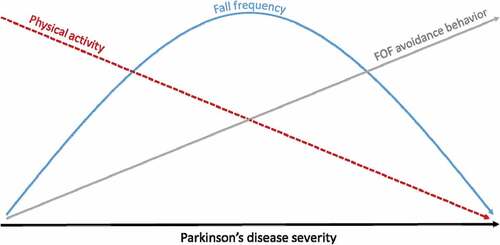
FOF activity avoidance may cause physical weakening and deconditioning which accelerates the decay of already weakened balance systems in PD (Blaszczyk, Orawiec, Duda-Klodowska, and Opala, Citation2007; Bloem et al., Citation2001) and further increases the risk for falls. Despite the self-imposed decreased exposure to challenging balance tasks, high FOF avoidance behavior is more predictive of a fall within the next year (Landers, Oscar, Sasaoka, and Vaughn, Citation2016). This supports the notion that avoidance behavior taxes already weakened balance systems and puts one at more risk for a future fall (see avoiders, ). Interestingly, in that study, FOF avoidance behavior was more predictive of a future fall than having had a previous fall (Landers, Oscar, Sasaoka, and Vaughn, Citation2016). Thus, using fall history as a predictor of future falls may not be appropriate because those with FOF avoidance behavior may have recalibrated their balance exposure. Thus, it is possible that someone with really poor balance performance may not fall because they have avoided all activities that would put them at risk. In , the impact of PD progression on falls, physical activity, and FOF avoidance behavior is illustrated. In essence, as falls accumulate there is a concomitant decrease in physical activity and an increase in FOF avoidance behavior. Eventually, the faller avoids so many challenging balance tasks that fall frequency begins to decrease as well and hence the inverted U curve that has been described elsewhere (Mactier et al., Citation2015). This inverted U curve also suggests that fall history alone does not provide a complete picture of actual fall risk. For this reason, fall history should be contextualized with physical activity or avoidance behavior in the form of a ratio (e.g. fall-to-step count ratio, fall-to-metabolic equivalent ratio, and fall-to-sedentary/avoidance behavior) as has been described by Del Din et al. (Citation2020).
Figure 2. Theoretical relationship between falls, physical activity, and FOF avoidance behavior over time in PD. Adapted from Mactier et al. (Citation2015) .
Theoretical framework for a treatment approach
Some degree of FOF avoidance behavior is theoretically protective and beneficial, especially for those who have poor gait and balance. By avoiding risky activities, falls can be prevented and this may be beneficial in the short term. However, eventually, the consequences of avoidance may hasten deconditioning and further functional decline. Thus, the more avoidance, the faster the progression into deconditioning and disability. Therefore, activity avoidance should be addressed in rehabilitation treatment plans because of the potential for negative downstream consequences. Specifically, it is important to determine if the activity avoidance is adaptive or maladaptive as that will help provide guidance for clinical reasoning. This can be done by measuring gait/balance performance and FOF avoidance behavior concurrently to see if the avoidance behavior is proportional to the current level of gait/balance function.
Because of the potential for “appropriate” adaptive and “inappropriate” maladaptive avoidance behavior response patterns, it is important to contextualize them. Here, a new theoretical framework using a concurrent measurement of gait/balance performance and avoidance behavior is proposed. These measurements are plotted onto a graph to determine the response pattern (). These patterns will help inform clinicians on how to contextualize the avoidance behavior and gait/balance function and prioritize treatment to best address the important root causes of the avoidance behavior. This framework proposes different treatment approaches and recommendations for each of the four patterns to help guide the clinician to the best treatment plan (.
Figure 3. Theoretical gait/balance and FOF avoidance behavior patterns. Maladaptive responses are found in light blue and light green, whereas appropriate responses are found in dark green and dark blue.
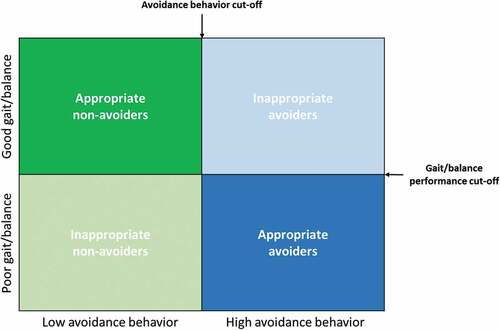
Table 1. Theoretical priorities for suggested physical therapy treatment strategies based on pattern of gait/balance performance and fear of falling (FOF) avoidance behavior for people with PD.
There are two patterns that represent appropriate adaptive responses: 1) appropriate non-avoiders; and 2) appropriate avoiders. Appropriate non-avoiders are those who have relatively normal or good gait/balance and exhibit little or no avoidance behavior. This is an appropriate response for someone who has experienced a fall or near fall despite good balance. In , these people are classified as “non-avoiders” who have not developed a FOF. Appropriate avoiders have poor gait/balance and are exhibiting avoidance behavior that is consistent with their gait/balance capability. In other words, those in this pattern are appropriately avoiding activity because they recognize their gait/balance limitations. However, by avoiding activity, they may be less engaged in physical activity which is important for maintenance of strength, conditioning, and gait/balance function. People in this pattern, even if their avoidance is appropriate, should be encouraged to increase their physical activity and exercise under safe conditions.
This theoretical framework also proposes two additional patterns that represent mismatches or maladaptive responses: 1) inappropriate non-avoiders; and 2) inappropriate avoiders. Inappropriate non-avoiders are those with poor gait/balance and do not exhibit FOF avoidance behavior. While people in this pattern would fall under non-avoiders in , they may be considered cavalier, unconcerned, or dismissive because they have not yet made adaptive responses to their poor balance. Theoretically, they would be at a high risk for falling because of poor gait/balance function and no FOF avoidance of risky gait/balance activities. Inappropriate avoiders have normal or good gait/balance but are exhibiting FOF avoidance behavior. People in this pattern are at risk for the vicious cycle of FOF described in . Theoretically, they may have more psychological overlay and, subsequently, the clinical treatment approach may need some focus on anxiety-attenuating treatment approaches.
Evidence for the construct validity of the theoretical framework
The evidence for the construct validity of the model comes from three sources: 1) evidence from the literature that supports the main components of the model; 2) face validity of the model; and 3) data from a previously published cross-sectional study. The main components of the proposed framework have significant evidence to support the validity of those constructs. Specifically, there is considerable evidence in support of many different gait and balance measurements and clinical cut points in people with PD, other neurological diseases, and older adults. Likewise, there is considerable evidence in support of the validity of the FOF avoidance behavior model in PD and this was detailed earlier in this paper. The novel part of this theoretical framework is putting these two, well-established constructs into a framework that may help the clinician to contextualize the patient’s presentation and improve clinical reasoning. Additionally, because of the evidence supporting these two components, it supports the face validity of the framework. That is the framework appears to measure what it purports to measure. Ultimately the face validity of this theoretical framework will be assessed by those that consider using it. Importantly, establishing validity is an iterative process.
To support the construct validity of the model, a real-world example of the gait/balance impairment and FOF avoidance behavior patterns applied to individuals with PD has been provided (). In sixty-three participants with PD from a previously published study (Landers et al., Citation2017) have been plotted into the framework with fallers noted in red with the Berg Balance Scale (BBS) as the representation of gait/balance function and the Fear of Falling Avoidance Behavior Questionnaire (FFABQ) as the FOF avoidance behavior component. While the BBS was used as the measure of gait/balance function in this example, other measures of gait/balance function or mobility (e.g. Timed Up and Go Test and gait velocity) with suitable cutoff scores would also work. In support of the face and construct validity of the framework, most of the participants in are in the “appropriate” response quadrants, which is to be expected. Additionally, there are fewer found in the “inappropriate” quadrants which supports the notion that only a small proportion of people will have a mismatched response pattern. Interestingly and not surprisingly, fallers and non-fallers are also found in each of the four patterns, which supports our hypothesis that fall history in isolation gives an incomplete picture of one’s status and only offers value when other factors, like FOF avoidance behavior and gait/balance function, are considered at the same time (). It also supports the notion that fall history is non-linear as has been proposed in this paper ().
Figure 4. Scatterplot of FOF avoidance behavior (FFABQ) and balance performance (BBS) and categorization based on BBS (43.5) (Landers et al., Citation2008) and FFABQ (20) (Landers et al., Citation2011) cutoffs.
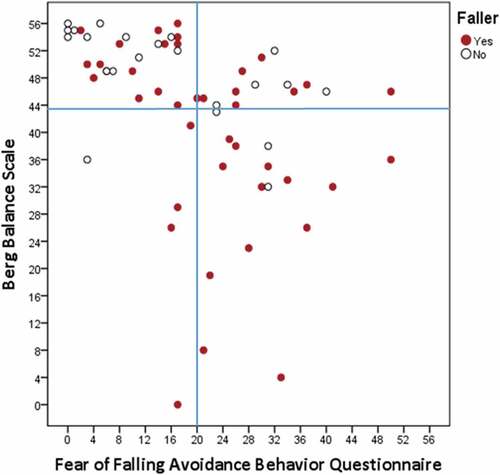
Using the same data (Landers et al., Citation2017) participants with PD were plotted into one of the four quadrants (appropriate avoider n = 16, appropriate non-avoider n = 28, inappropriate avoider n = 14, inappropriate non-avoider n = 5), These four groups were then compared using a Kruskall-Wallis test (non-parametric analyses used because only 5 in inappropriate non-avoider quadrant) across 6 different variables: 1) Zung Anxiety Scale (ZAS) (Zung, Citation1971); 2) Catastrophizing about Falls Scale (CAFS) (Van Haastregt and Vlaeyen, Citation2002); 3) Consequences of Falling Questionnaire (COFQ) (Yardley and Smith, Citation2002); 4) Impact of Events Scale – Revised (IES-R) (Weiss, Citation2004); 5) time stepping; and 6) steps taken per day using an ActivPAL activity monitor (PAL Technologies LDT, Glasgow, United Kingdom). Post hoc analyses were compared using Mann-Whitney analyses with a Bonferroni corrected alpha for 6 post hoc tests (α = 0.008). Results for the analysis of the differences among the four quadrants are the following (): ZAS (p = .009); CAFS (p = .001); COFS (p < .001); IES-R (p = .122); time stepping (p < .001); and steps taken (p < .001). From a construct validity perspective, there would be an expectation that those in the low avoidance behavior quadrants (appropriate non-avoiders and inappropriate non-avoiders) would have higher daily step counts and spend more time stepping per day and, collectively, this was found to be the case. Appropriate non-avoiders and inappropriate non-avoiders spent more time stepping and took more steps than the appropriate avoiders (ps < 0.003). There were no statistically significant differences with inappropriate avoiders for either non-avoider group. These data support the notion that avoiders are less active than non-avoiders.
Figure 5. A bar graph of the four different patterns across 6 different variables with means and standard error: A) Zung Anxiety Scale (ZAS) and Catastrophizing About Falls Questionnaire (CAFS); B) Consequences About Falls Scale (CAFS), Impact of Events Scale – Revised (IES-R), activity monitor recorded average daily time stepping (time stepping); and C) activity monitor recorded average steps taken per day (steps taken).
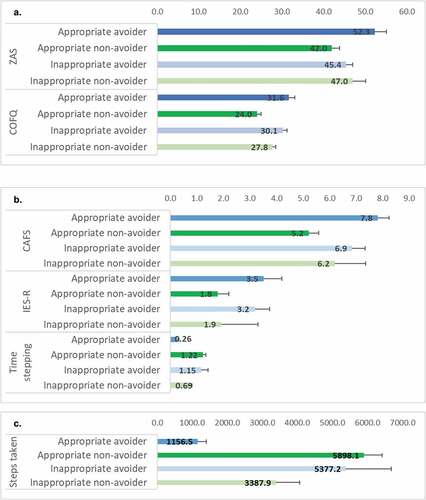
Additionally, from a construct validity perspective, there would be an expectation that those in the high avoidance categories with more FOF would have higher scores on anxiety-related measures and, collectively, the results bear that out. Appropriate avoiders had higher ZAS, COFQ, and CAFS scores than appropriate non-avoiders (ps < 0.002). Inappropriate avoiders had higher COFQ and CAFS scores than appropriate non-avoiders (ps < 0.003). There were no other statistically significant post hoc pairwise comparisons. These data suggest that those in the two avoider quadrants report more general anxiety and more fall anxiety. Taken together, these data provide some preliminary evidence for the construct validity of the four quadrants in this theoretical framework. However, more research in this area is warranted.
Treatment approach based on gait/balance and avoidance behavior patterns
The aforementioned theoretical framework outlines treatment strategies that take into account the complexity of gait/balance impairment contextualized with FOF avoidance behavior. This framework organizes a person’s presentation into 4 different gait/balance and avoidance behavior patterns with an accompanying treatment approach for each. From a face validity perspective, it is important that these 4 different treatment approaches logically match the pattern and, while there may be some overlap or reclassification based on changing status, the general idea is that these different approaches are general clinical guidelines that are specific to the person’s current presentation and should be used to assist clinical decision-making. Using data collected from an initial evaluation, a clinician can place the patient into a quadrant or pattern and then use that as a guide to build a treatment plan. Below, a suggested treatment approach for each of the patterns () is detailed. In addition to pattern-specific treatment focuses, general exercise guidelines for all of the patterns are included. This framework should not replace clinical reasoning but serve as a guideline especially in cases where a person’s status is on the border and not clearly in one pattern/quadrant.
Appropriate non-avoiders
People in this pattern have good gait/balance and do not exhibit high FOF avoidance behavior. In , they would be classified as non-avoiders. Because of this, these individuals may not need to initiate an extensive, one-on-one, formalized physical therapy treatment plan. Instead, the main priority for people in this pattern is a preventative plan with education, guidance and support for maintaining physical conditioning and balance. Home and community/group exercise programs are appropriate for people in this pattern. As there is an inevitable decay in gait and balance as PD progresses, people with PD should be encouraged to return to their physical therapist at regular intervals (every 6 to 12 months) to get a reevaluation and determine the following next steps: 1) Continue with a general home/community exercise program if still appropriate; 2) Fine tune the exercise program based on current gait and balance impairment; and 3) Begin a formalized exercise program if the gait and balance impairments have decayed sufficiently that they now need supervised attention or if their condition progresses to one of the other patterns.
Appropriate avoiders
People in this pattern have an avoidance behavior response that matches their level of balance function. Thus, they have poor gait/balance and are appropriately avoiding activities that put them at risk for a fall. Since PD medications do little to improve gait and balance in PD (Baer et al., Citation2018; Crouse, Phillips, Jahanshahi, and Moustafa, Citation2016; Curtze et al., Citation2015) the treatment plan should include a physical therapist-supervised, gait/balance training program that is supported by evidence to improve balance (Klamroth, Steib, Devan, and Pfeifer, Citation2016) and physical activity levels (Conradsson et al., Citation2015) and to reduce FOF and fall rates in PD (Sparrow et al., Citation2016). Because people in this pattern have poor balance, safety is a primary focus. Therefore, supervision is imperative and expertise is needed to facilitate gait/balance training progression. A safety harness or gait belt to prevent a fall may be needed in some instances.
An additional important treatment priority in this pattern is doing strength training and weight bearing exercises that are sufficient to improve bone health. Since people in this pattern are avoiding activity, it is possible, from a theoretical perspective, that their bone health may be less than ideal due to a lack of participation in physical activity. Additionally, as falling is one of the two main causes that hastens mortality in PD, it is important to prevent the consequences of a fall (e.g. bone fractures) in those who are at high risk for falling. Mobility aids or assistive devices (e.g. rolling walker or rollator) to decrease the risk should also be recommended for people in this pattern if it is appropriate. Moreover, there should be encouragement to use the mobility aid or assistive device to facilitate more participation in physical activity. That is, these devices should be used to help enable the person to increase their physical activity without increasing their fall risk. Lastly, as improvements in balance and gait are realized, there should be a concomitant increase in physical activity (i.e. decreased avoidance behavior). If avoidance behavior due to FOF persists despite improved gait and balance, a therapist-led, social cognitive theory (Bandura, Citation2004; Ellis and Motl, Citation2013) and/or cognitive behavioral therapy (CBT) strategy (Dobkin et al., Citation2019; Herning, Cook, and Schneider, Citation2005; Kraepelien et al., Citation2020; Reynolds et al., Citation2020) may be needed to increase self-efficacy and physical activity levels and to decrease cognitive and affective factors associated with the avoidance behavior.
Inappropriate non-avoiders
People in this pattern have poor gait/balance but do not exhibit concomitant FOF avoidance behavior. People in this pattern may be unaware of their current balance state, may deny their balance impairment, may refuse or be reluctant to use an assistive device, and/or may be cavalier in their approach to their condition. Because of the discrepancy between poor gait/balance function and lack of FOF avoidance behavior, it is possible that cognitive impairment may be playing a role. Whatever the cause, people in this pattern are at high risk for falling because of their exposure to potentially risky activities and their poor gait/balance. The physical therapy treatment priority is education about their current fall risk, fall consequences, behaviors to avoid, and the possible need for a mobility aid. It is important to include the family in the education as their support can help facilitate an appropriate behavioral change. Another important treatment priority is participation in a structured exercise and balance program to address the impaired gait and balance.
Inappropriate avoiders
People in this pattern have good gait and balance but have disproportinately high FOF avoidance behavior. Subsequently, the treatment emphasis for this pattern should be attenuating the FOF avoidance behavior. In addition to a physical therapist-supervised exercise and balance training program to improve their balance self-confidence and efficacy, a CBT strategy may be an important interventional consideration since fear and anxiety about falling can potentiate the aforementioned vicious cycle. In older adults with FOF avoidance behavior, CBT has been shown to be effective in reducing activity avoidance and improving social function (Lawrence et al., Citation1998). Additionally, researchers found that a group exercise program with CBT designed to reduce FOF and avoidance behavior (A Matter of Balance) reduced FOF and avoidance behavior (Sartor-Glittenberg et al., Citation2018).
Another important tool in decreasing FOF is exercise. In a systematic review on FOF and exercise in older people, researchers concluded that exercise is effective at reducing falls in community-dwelling older people and FOF to a small or moderate degree (Kumar et al., Citation2016). A recent meta-analysis that adressed the effects of interventions on FOF in community dwelling older people suggest that holistic exercise, tai chi, or delivery of the intervention in a community setting were significantly more effective than interventions without these characteristics (Kruisbrink et al., Citation2021). Interventions that were delivered at home or with written materials were significantly less effective at reducing FOF.
Based on the evidence of these approaches, utilizing both physical and psychological interventions for FOF avoidance behaviors is warranted. Additionally, consultation from a clinical psychologist may also be warranted if the anxiety is beyond the scope of the therapist. Researchers add that activity avoidance is also associated with social support (Howland et al., Citation1998). Specifically, those with social support were least likely to report activity avoidance. They suggest that friends, relatives, and health care providers play a critical role in providing encouragement to help address the FOF and avoidance behavior.
Summary
In the theoretical framework proposed in this paper, four different patterns related to FOF avoidance behavior and gait/balance performance have been described: appropriate avoiders, appropriate non-avoiders, inappropriate avoiders, and inappropriate non-avoiders. For each of the four different patterns, special considerations and recommended treatment focuses have been made. This theoretical framework may help the clinician to understand and contextualize the complexity of FOF avoidance behavior and gait/balance impairment in PD. While the main components of this theoretical framework are supported by the literature, the framework itself and the treatment recommendations are based on face validity and preliminary data. However, establishing validity is an iterative process and, subsequently, more research is still needed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Adamson BC, Ensari I, Motl RW 2015 Effect of exercise on depressive symptoms in adults with neurologic disorders: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation 96(7): 1329–1338. 10.1016/j.apmr.2015.01.005.
- Allen NE, Schwarzel AK, Canning CG 2013 Recurrent falls in Parkinson’s disease: A systematic review. Parkinson’s Disease 2013: 906274. 10.1155/2013/906274.
- Almeida L, Piemonte M, Cavalcanti H, Canning C, Paul S 2021 A self-reported clinical tool predicts falls in people with Parkinson’s disease. Movement Disorders Clinical Practice 8(3): 427–434. 10.1002/mdc3.13170.
- Armstrong C 2019 Physical activity: Updated recommendations from HHS. American Family Physician 100(1): 58–59.
- Baer M, Klemetson B, Scott D, Murtishaw AS, Navalta JW, Kinney J, Landers MR 2018 Effects of fatigue on balance in individuals with Parkinson disease: Influence of medication and brain-derived neurotrophic factor genotype. Journal of Neurologic Physical Therapy 42(2): 61–71. 10.1097/NPT.0000000000000213.
- Bandura A 2004 Health promotion by social cognitive means. Health Education and Behavior 31(2): 143–164. 10.1177/1090198104263660.
- Behaviour Research Networ S Sedentary Behaviour Research Network 2012 Letter to the editor: Standardized use of the terms “sedentary” and “sedentary behaviours.” Applied Physiology, Nutrition, and Metabolism 37(3): 540–542. 10.1139/h2012-024.
- Benka Wallen M, Franzen E, Nero H, Hagstromer M 2015 Levels and patterns of physical activity and sedentary behavior in elderly people with mild to moderate Parkinson disease. Physical Therapy 95(8): 1135–1141. 10.2522/ptj.20140374.
- Blaszczyk JW, Orawiec R, Duda-Klodowska D, Opala G 2007 Assessment of postural instability in patients with Parkinson’s disease. Experimental Brain Research 183(1): 107–114. 10.1007/s00221-007-1024-y.
- Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH 2001 Prospective assessment of falls in Parkinson’s disease. Journal of Neurology 248(11): 950–958. 10.1007/s004150170047.
- Booth FW, Roberts CK, Laye MJ 2012 Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology 2: 1143–1211.
- Brozova H, Stochl J, Roth J, Ruzicka E 2009 Fear of falling has greater influence than other aspects of gait disorders on quality of life in patients with Parkinson’s disease. Neuro Endocrinology Letters 30(4): 453–457.
- Canning CG, Paul SS, Nieuwboer A 2014 Prevention of falls in Parkinson’s disease: A review of fall risk factors and the role of physical interventions. Neurodegenerative Disease Management 4(3): 203–221. 10.2217/nmt.14.22.
- Choi H, Irwin M, Cho H 2015 Impact of social isolation on behavioral health in elderly: Systematic review. World Journal of Psychiatry 5(4): 432–438. 10.5498/wjp.v5.i4.432.
- Chomiak T, Watts A, Burt J, Camicioli R, Tan SN, McKeown MJ, Hu B 2018 Differentiating cognitive or motor dimensions associated with the perception of fall-related self-efficacy in Parkinson’s disease. NPJ Parkinson’s Disease 4(1): 26. 10.1038/s41531-018-0059-z.
- Conradsson D, Lofgren N, Nero H, Hagstromer M, Stahle A, Lokk J, Franzen E 2015 The effects of highly challenging balance training in elderly with Parkinson’s disease: A randomized controlled trial. Neurorehabilitation and Neural Repair 29(9): 827–836. 10.1177/1545968314567150.
- Conradsson D, Lofgren N, Stahle A, Hagstromer M, Franzen E 2012 A novel conceptual framework for balance training in Parkinson’s disease - Study protocol for a randomised controlled trial. BMC Neurology 12(1): 111. 10.1186/1471-2377-12-111.
- Crouse JJ, Phillips JR, Jahanshahi M, Moustafa AA 2016 Postural instability and falls in Parkinson’s disease. Reviews in the Neurosciences 27(5): 549–555. 10.1515/revneuro-2016-0002.
- Curtze C, Nutt JG, Carlson-Kuhta P, Mancini M, Horak F 2015 Levodopa is a double-edged sword for balance and gait in people with Parkinson’s disease. Movement Disorders 30(10): 1361–1370. 10.1002/mds.26269.
- Dauwan M, Begemann M, Slot M, Lee E, Scheltens P, Sommer IE 2021 Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: A trans-diagnostic systematic review and meta-analysis of randomized controlled trials. Journal of Neurology 268(4): 1222–1246. 10.1007/s00415-019-09493-9.
- Del Din S, Galna B, Lord S, Nieuwboer A, Bekkers EM, Pelosin E, Avanzino L, Bloem BR, Olde Rikkert MG, Nieuwhof F, et al. 2020 Falls risk in relation to activity exposure in high-risk older adults. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences 75(6): 1198–1205. 10.1093/gerona/glaa007.
- Delgado-Alvarado M, Marano M, Santurtun A, Urtiaga-Gallano A, Tordesillas-Gutierrez D, Infante J 2020 Nonpharmacological, nonsurgical treatments for freezing of gait in Parkinson’s disease: A systematic review. Movement Disorders 35(2): 204–214. 10.1002/mds.27913.
- Dennison AC, Noorigian J, Robinson K, Fisman DN, Cianci HJ, Moberg P, Bunting-Perry L, Martine R, Duda J, Stern MB 2007 Falling in Parkinson disease: Identifying and prioritizing risk factors in recurrent fallers. American Journal of Physical Medicine & Rehabilitation 86(8): 621–632. 10.1097/PHM.0b013e311611583.
- Deshpande N, Metter EJ, Lauretani F, Bandinelli S, Guralnik J, Ferrucci L 2008 Activity restriction induced by fear of falling and objective and subjective measures of physical function: A prospective cohort study. Journal of the American Geriatrics Society 56(4): 615–620. 10.1111/j.1532-5415.2007.01639.x.
- Dobkin RD, Mann SL, Interian A, Gara MA, Menza M 2019 Cognitive behavioral therapy improves diverse profiles of depressive symptoms in Parkinson’s disease. International Journal of Geriatric Psychiatry 34(5): 722–729. 10.1002/gps.5077.
- Ellis T, Boudreau J, DeAngelis T, Brown L, Cavanaugh J, Earhart G, Ford MP, Foreman KB, Dibble LE 2013 Barriers to exercise in people with Parkinson disease. Physical Therapy 93(5): 628–636. 10.2522/ptj.20120279.
- Ellis T, Motl RW 2013 Physical activity behavior change in persons with neurologic disorders: Overview and examples from Parkinson disease and multiple sclerosis. Journal of Neurologic Physical Therapy 37(2): 85–90. 10.1097/NPT.0b013e31829157c0.
- Elsawy B, Higgins KE 2010 Physical activity guidelines for older adults. American Family Physician 81: 55–59.
- Fasano A, Canning CG, Hausdorff JM, Lord S, Rochester L 2017 Falls in Parkinson’s disease: A complex and evolving picture. Movement Disorders 32(11): 1524–1536. 10.1002/mds.27195.
- Flynn A, Allen NE, Dennis S, Canning CG, Preston E 2019 Home-based prescribed exercise improves balance-related activities in people with Parkinson’s disease and has benefits similar to centre-based exercise: A systematic review. Journal of Physiotherapy 65(4): 189–199. 10.1016/j.jphys.2019.08.003.
- Franzen E, Conradsson D, Hagstromer M, Nilsson MH 2016 Depressive symptoms associated with concerns about falling in Parkinson’s disease. Brain and Behavior 6(10): e00524. 10.1002/brb3.524.
- Fuzeki E, Banzer W 2018 Physical activity recommendations for health and beyond in currently inactive populations. International Journal of Environmental Research and Public Health 15(5): 1042. 10.3390/ijerph15051042.
- Garber CE, Friedman JH 2003 Effects of fatigue on physical activity and function in patients with Parkinson’s disease. Neurology 60(7): 1119–1124. 10.1212/01.WNL.0000055868.06222.AB.
- Gazibara T, Stankovic I, Tomic A, Svetel M, Tepavcevic D, Kostic VS, Pekmezovic T 2013 Validation and cross-cultural adaptation of the Falls Efficacy Scale in patients with Parkinson’s disease in Serbia. Geriatrics & Gerontology International 13(4): 936–941. 10.1111/ggi.12034.
- Gazibara T, Tepavcevic DK, Svetel M, Tomic A, Stankovic I, Kostic VS, Pekmezovic T 2019 Change in fear of falling in Parkinson’s disease: A two-year prospective cohort study. International Psychogeriatrics 31(1): 13–20. 10.1017/S1041610217002514.
- Ginis P, Nackaerts E, Nieuwboer A, Heremans E 2018 Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-the-art and novel perspectives. Annals of Physical and Rehabilitation Medicine 61(6): 407–413. 10.1016/j.rehab.2017.08.002.
- Hely MA, Morris JG, Traficante R, Reid WG, O’Sullivan DJ, Williamson PM 1999 The sydney multicentre study of Parkinson’s disease: Progression and mortality at 10 years. Journal of Neurology, Neurosurgery, and Psychiatry 67(3): 300–307. 10.1136/jnnp.67.3.300.
- Herning MM, Cook JH, Schneider JK 2005 Cognitive behavioral therapy to promote exercise behavior in older adults: Implications for physical therapists. Journal of Geriatric Physical Therapy 28(2): 34–38. 10.1519/00139143-200508000-00001.
- Heyn P, Hirsch M, York M, Backus D 2016 Physical activity recommendations for the aging brain: A clinician-patient guide. Archives of Physical Medicine and Rehabilitation 97(6): 1045–1047. 10.1016/j.apmr.2016.02.003.
- Hiorth YH, Larsen JP, Lode K, Tysnes OB, Godfrey A, Lord S, Rochester L, Pedersen KF 2016 Impact of falls on physical activity in people with Parkinson’s disease. Journal of Parkinson’s Disease 6(1): 175–182. 10.3233/JPD-150640.
- Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A 1998 Covariates of fear of falling and associated activity curtailment. Gerontologist 38(5): 549–555. 10.1093/geront/38.5.549.
- Howland J, Peterson EW, Levin WC, Fried L, Pordon D, Bak S 1993 Fear of falling among the community-dwelling elderly. Journal of Aging and Health 5(2): 229–243. 10.1177/089826439300500205.
- Jayakody K, Gunadasa S, Hosker C 2014 Exercise for anxiety disorders: Systematic review. British Journal of Sports Medicine 48(3): 187–196. 10.1136/bjsports-2012-091287.
- Jonasson SB, Ullen S, Iwarsson S, Lexell J, Nilsson MH 2015 Concerns about falling in Parkinson’s disease: Associations with disabilities and personal and environmental factors. Journal of Parkinson’s Disease 5(2): 341–349. 10.3233/JPD-140524.
- Kader M, Iwarsson S, Odin P, Nilsson MH 2016 Fall-related activity avoidance in relation to a history of falls or near falls, fear of falling and disease severity in people with Parkinson’s disease. BMC Neurology 16(1): 84. 10.1186/s12883-016-0612-5.
- Keus S, Munneke M, Graziano M, Paltamaa J, Pelosin E, Domingos J, Bruhlmann S, Ramaswamy B, Prins J, and Struiksma C, et al 2014 European Physiotherapy Guideline for Parkinson’s Disease: Development and Implementation. Netherlands: KNG/ParkinsonNet. Accessed January 24, 2022. https://www.parkinsonnet.nl/app/uploads/sites/3/2019/11/eu_guideline_parkinson_guideline_for_pt_s1.pdf
- Klamroth S, Steib S, Devan S, Pfeifer K 2016 Effects of exercise therapy on postural instability in Parkinson disease: A meta-analysis. Journal of Neurologic Physical Therapy 40(1): 3–14. 10.1097/NPT.0000000000000117.
- Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, Kahlmeier S 2012 Lancet physical activity series working group 2012 The pandemic of physical inactivity: Global action for public health. Lancet 380(9838): 294–305. 10.1016/S0140-6736(12)60898-8.
- Kraepelien M, Schibbye R, Mansson K, Sundstrom C, Riggare S, Andersson G, Lindefors N, Svenningsson P, Kaldo V 2020 Individually tailored internet-based cognitive-behavioral therapy for daily functioning in patients with Parkinson’s disease: A randomized controlled trial. Journal of Parkinson’s Disease 10(2): 653–664. 10.3233/JPD-191894.
- Kruisbrink M, Delbaere K, Kempen G, Crutzen R, Ambergen T, Cheung KL, Kendrick D, Iliffe S, Zijlstra GA 2021 Intervention characteristics associated with a reduction in fear of falling among community-dwelling older people: A systematic review and meta-analysis of randomized controlled trials. Gerontologist 61(6): e269–e282. 10.1093/geront/gnaa021.
- Kumar A, Delbaere K, Zijlstra GA, Carpenter H, Iliffe S, Masud T, Skelton D, Morris R, Kendrick D 2016 Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age and Ageing 45(3): 345–352. 10.1093/ageing/afw036.
- LaHue SC, Comella CL, Tanner CM 2016 The best medicine? The influence of physical activity and inactivity on Parkinson’s disease. Movement Disorders 31(10): 1444–1454. 10.1002/mds.26728.
- Landers MR 2020 Evidence that exercise is neuroprotective in Parkinson’s disease, Association of Chartered Physiotherapists in Neurology, United Kingdom: Synapse, 16–19.
- Landers MR, Backlund A, Davenport J, Fortune J, Schuerman S, Altenburger P 2008 Postural instability in idiopathic Parkinson’s disease: Discriminating fallers from nonfallers based on standardized clinical measures. Journal of Neurologic Physical Therapy 32(2): 56–61. 10.1097/NPT.0b013e3181761330.
- Landers MR, Durand C, Powell DS, Dibble LE, Young DL 2011 Development of a scale to assess avoidance behavior due to a fear of falling: The fear of falling avoidance behavior questionnaire. Physical Therapy 91(8): 1253–1265. 10.2522/ptj.20100304.
- Landers MR, Jacobson KM, Matsunami NE, McCarl HE, Regis MT, Longhurst JK 2021 A vicious cycle of fear of falling avoidance behavior in Parkinson’s disease: A path analysis. Clinical Parkinsonism and Related Disorders 4: 100089. 10.1016/j.prdoa.2021.100089.
- Landers MR, Lopker M, Newman M, Gourlie R, Sorensen S, Vong R 2017 A cross-sectional analysis of the characteristics of individuals with Parkinson disease who avoid activities and participation due to fear of falling. Journal of Neurologic Physical Therapy 41(1): 31–42. 10.1097/NPT.0000000000000162.
- Landers MR, Oscar S, Sasaoka J, Vaughn K 2016 Balance confidence and fear of falling avoidance behavior are most predictive of falling in older adults: Prospective analysis. Physical Therapy 96(4): 433–442. 10.2522/ptj.20150184.
- Lawrence RH, Tennstedt SL, Kasten LE, Shih J, Howland J, Jette AM 1998 Intensity and correlates of fear of falling and hurting oneself in the next year: Baseline findings from a Roybal Center fear of falling intervention. Journal of Aging and Health 10(3): 267–286. 10.1177/089826439801000301.
- Lindholm B, Hagell P, Hansson O, Nilsson MH 2014 Factors associated with fear of falling in people with Parkinson’s disease. BMC Neurology 14(1): 19. 10.1186/1471-2377-14-19.
- Lindholm B, Hagell P, Hansson O, Nilsson MH 2015 Prediction of falls and/or near falls in people with mild Parkinson’s disease. PloS One 10(1): e0117018. 10.1371/journal.pone.0117018.
- Lindh-Rengifo M, Jonasson SB, Mattsson N, Ullen S, Nilsson MH 2019 Predictive factors of concerns about falling in people with Parkinson’s disease: A 3-year longitudinal study. Parkinson’s Disease 2019: 4747320. 10.1155/2019/4747320.
- Lord S, Galna B, Yarnall AJ, Coleman S, Burn D, Rochester L 2016 Predicting first fall in newly diagnosed Parkinson’s disease: Insights from a fall-naïve cohort. Movement Disorders 31(12): 1829–1836. 10.1002/mds.26742.
- Lord S, Galna B, Yarnall AJ, Morris R, Coleman S, Burn D, Rochester L 2017 Natural history of falls in an incident cohort of Parkinson’s disease: Early evolution, risk and protective features. Journal of Neurology 264(11): 2268–2276. 10.1007/s00415-017-8620-y.
- Macleod AD, Taylor KS, Counsell CE 2014 Mortality in Parkinson’s disease: A systematic review and meta-analysis. Movement Disorders 29(13): 1615–1622. 10.1002/mds.25898.
- Mactier K, Lord S, Godfrey A, Burn D, Rochester L 2015 The relationship between real world ambulatory activity and falls in incident Parkinson’s disease: Influence of classification scheme. Parkinsonism & Related Disorders 21(3): 236–242. 10.1016/j.parkreldis.2014.12.014.
- Mak MK, Pang MY 2009 Balance confidence and functional mobility are independently associated with falls in people with Parkinson’s disease. Journal of Neurology 256(5): 742–749. 10.1007/s00415-009-5007-8.
- Mak MK, Pang MY, Mok V 2012 Gait difficulty, postural instability, and muscle weakness are associated with fear of falling in people with Parkinson’s disease. Parkinsons Disease 2012: 901721.
- Mansoubi M, Pearson N, Clemes SA, Biddle SJ, Bodicoat DH, Tolfrey K, Edwardson CL, Yates T 2015 Energy expenditure during common sitting and standing tasks: Examining the 1.5 MET definition of sedentary behaviour. BMC Public Health 15(1): 516. 10.1186/s12889-015-1851-x.
- Matinolli M, Korpelainen JT, Korpelainen R, Sotaniemi KA, Matinolli VM, Myllyla VV 2009 Mobility and balance in Parkinson’s disease: A population-based study. European Journal of Neurology 16(1): 105–111. 10.1111/j.1468-1331.2008.02358.x.
- Mille ML, Creath RA, Prettyman MG, Johnson Hilliard M, Martinez KM, Mackinnon CD, Rogers MW 2012 Posture and locomotion coupling: A target for rehabilitation interventions in persons with Parkinson’s disease. Parkinson’s Disease 2012: 754186. 10.1155/2012/754186.
- Morris ME 2000 Movement disorders in people with Parkinson disease: A model for physical therapy. Physical Therapy 80(6): 578–597. 10.1093/ptj/80.6.578.
- Morris ME 2006 Locomotor training in people with Parkinson disease. Physical Therapy 86(10): 1426–1435. 10.2522/ptj.20050277.
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C 2007 Physical activity and public health in older adults: Recommendation from the American college of sports medicine and the American heart association. Medicine and Science in Sports and Exercise 39(8): 1435–1445. 10.1249/mss.0b013e3180616aa2.
- Nilsson MH, Drake AM, Hagell P 2010 Assessment of fall-related self-efficacy and activity avoidance in people with Parkinson’s disease. BMC Geriatrics 10(1): 78. 10.1186/1471-2318-10-78.
- Nilsson MH, Hariz GM, Iwarsson S, Hagell P 2012 Walking ability is a major contributor to fear of falling in people with Parkinson’s disease: Implications for rehabilitation. Parkinson’s Disease 2012: 713236. 10.1155/2012/713236.
- Nilsson MH, Hariz GM, Wictorin K, Miller M, Forsgren L, Hagell P 2010 Development and testing of a self administered version of the freezing of gait questionnaire. BMC Neurology 10(1): 85. 10.1186/1471-2377-10-85.
- Nilsson MH, Jonasson SB, Zijlstra GA 2020 Predictive factors of fall-related activity avoidance in people with Parkinson disease: A longitudinal study with a 3-Year follow-up. Journal of Neurologic Physical Therapy 44(3): 188–194. 10.1097/NPT.0000000000000316.
- Paul SS, Allen N, Sherrington C, Heller G, Fung VS, Close J, Lord S, Canning CG 2014a Risk factors for frequent falls in people with Parkinson’s disease. Journal of Parkinson’s Disease 4(4): 699–703. 10.3233/JPD-140438.
- Paul SS, Sherrington C, Canning CG, Fung VS, Close JC, Lord SR 2014b The relative contribution of physical and cognitive fall risk factors in people with Parkinson’s disease: A large prospective cohort study. Neurorehabilitation and Neural Repair 28(3): 282–290. 10.1177/1545968313508470.
- Pickering RM, Grimbergen YA, Rigney U, Ashburn A, Mazibrada G, Wood B, Gray P, Kerr G, Bloem BR 2007 A meta-analysis of six prospective studies of falling in Parkinson’s disease. Movement Disorders 22(13): 1892–1900. 10.1002/mds.21598.
- Pinter B, Diem-Zangerl A, Wenning GK, Scherfler C, Oberaigner W, Seppi K, Poewe W 2015 Mortality in Parkinson’s disease: A 38-year follow-up study. Movement Disorders 30(2): 266–269. 10.1002/mds.26060.
- Rafferty M, Nettnin E, Goldman J, MacDonald J 2021 Frameworks for Parkinson’s disease rehab-ilitation addressing when, what, and how. Current Neurology and Neuroscience Reports 21(3): 12. 10.1007/s11910-021-01096-0.
- Rahman S, Griffin HJ, Quinn NP, Jahanshahi M 2011 On the nature of fear of falling in Parkinson’s disease. Behavioural Neurology 24(3): 219–228. 10.1155/2011/274539.
- Reynolds GO, Saint-Hilaire M, Thomas C, Barlow D, Cronin-Golomb A 2020 Cognitive-behavioral therapy for anxiety in Parkinson’s disease. Behavior Modification 44(4): 552–579. 10.1177/0145445519838828.
- Sartor-Glittenberg C, Bordenave E, Bay C, Bordenave L, Alexander JL 2018 Effect of a matter of balance programme on avoidance behaviour due to fear of falling in older adults. Psychogeriatrics 18(3): 224–230. 10.1111/psyg.12310.
- Shen X, Wong-Yu IS, Mak MK 2016 Effects of exercise on falls, balance, and gait ability in Parkinson’s Disease: A meta-analysis. Neurorehabilitation and Neural Repair 30(6): 512–527. 10.1177/1545968315613447.
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE 2019 Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 1: CD012424.
- Soh SE, McGinley JL, Watts JJ, Iansek R, Murphy AT, Menz HB, Huxham F, Morris ME 2013 Determinants of health-related quality of life in people with Parkinson’s disease: A path analysis. Quality of Life Research 22(7): 1543–1553. 10.1007/s11136-012-0289-1.
- Sparling PB, Howard BJ, Dunstan DW, Owen N 2015 Recommendations for physical activity in older adults. BMJ 350(jan20 6): h100. 10.1136/bmj.h100.
- Sparrow D, DeAngelis TR, Hendron K, Thomas CA, Saint-Hilaire M, Ellis T 2016 Highly challenging balance program reduces fall rate in Parkinson disease. Journal of Neurologic Physical Therapy 40(1): 24–30. 10.1097/NPT.0000000000000111.
- Temlett JA, Thompson PD 2006 Reasons for admission to hospital for Parkinson’s disease. Internal Medicine Journal 36(8): 524–526. 10.1111/j.1445-5994.2006.01123.x.
- Uhrbrand A, Stenager E, Pedersen MS, Dalgas U 2015 Parkinson’s disease and intensive exercise therapy: A systematic review and meta-analysis of randomized controlled trials. Journal of the Neurological Sciences 353(1–2): 9–19. 10.1016/j.jns.2015.04.004.
- van Den Bos F, Speelman AD, Samson M, Munneke M, Bloem BR, Verhaar HJ 2013 Parkinson’s disease and osteoporosis. Age and Ageing 42(2): 156–162. 10.1093/ageing/afs161.
- Van Haastregt JC, Vlaeyen JW 2002 Catastrophizing About Falls Scale (CAFS). preventing falls and morbidity impairments in elderly people living in the community. Theses: Maastricht University, Netherlands.
- Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ 1997 Fear of falling and restriction of mobility in elderly fallers. Age and Ageing 26(3): 189–193. 10.1093/ageing/26.3.189.
- Weiss DS 2004 The Impact of Events Scale - Revised (2nd ed), New York, NY: Guilford Press.
- Wu PL, Lee M, Huang TT 2017 Effectiveness of physical activity on patients with depression and Parkinson’s disease: A systematic review. PloS One 12(7): e0181515. 10.1371/journal.pone.0181515.
- Yardley L, Smith H 2002 A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 42(1): 17–23. 10.1093/geront/42.1.17.
- Zung WW 1971 A rating instrument for anxiety disorders. Psychosomatics 12(6): 371–379. 10.1016/S0033-3182(71)71479-0.
