ABSTRACT
Background
Digital tools are becoming more and more common in healthcare. Their potential to improve treatment, monitoring, and coaching in physiotherapy has been recognized. Yet studies report that the adoption of digital health tools in ambulatory physiotherapy is rather low and that their potential is underexploited.
Objective
This paper aims to investigate how digital health tools in general, and the mobile health tool physitrackTM (hereafter the app) more particularly, are used in outpatient physiotherapy clinics and also to identify what facilitates or hinders the app’s use.
Methods
The paper is part of a larger study and adopts an ethnographic approach. It is based on observational and interview data collected at two outpatient clinics.
Results
We reveal how physiotherapists and patients use the app in physiotherapy and identify 16 interdependent factors, on the macro-, meso-, and micro-level, that either facilitate or hinder its use.
Conclusions
We argue that a single factor’s facilitating or hindering impact cannot be grasped in isolation but needs to be investigated as one piece of a dynamic interplay. Further qualitative research is required, especially to shed more light on the app’s compatibility with physiotherapy practice and use in therapist-patient interactions.
Introduction
In this paper, when talking about digital health tools, or eHealth tools for short, we refer to electronic technologies used in healthcare to remotely collect, provide, and/or analyze patient data and other medical information, using techniques that are not yet perceived as standard (Matusiewicz and Thielscher, Citation2017). Based on this general definition, the subcategory of mobile health (hereafter mHealth) includes tools for medical and therapeutic practices, as well as measures of private or public health, that are gathered and distributed via wireless devices (e.g. smartphones, tablets, patient monitoring devices, and personal digital assistants (PDAs)) (eHealth Suisse, Citation2017; Endl, Jäschke, Thiel, and Wickinghoff, Citation2015).
Over the past couple decades, the use of eHealth tools in healthcare has become ubiquitous and increasingly important. Studies have highlighted their potential to improve: therapeutic interventions and outcomes (Corbetta, Imeri, and Gatti, Citation2015); self-management (Vorrink, Kort, Troosters, and Lammers, Citation2016); access to remote consultations (Hinman, Nelligan, Bennell, and Delany, Citation2017); and coaching (Morris et al., Citation2019). Despite the growth of this field, studies and reports point out that the adoption of eHealth tools in clinical practice is rather low and that their potential remains underexploited in healthcare in general (Albrecht et al., Citation2017; Angerer et al., Citation2017; Chan and Kaufman, Citation2011; Endl, Jäschke, Thiel, and Wickinghoff, Citation2015; Gagnon, Ngangue, Payne-Gagnon, and Desmartis, Citation2016) and in physiotherapy more particularly (Postolache, Oliveira, and Postolache, Citation2017). Moreover, in Switzerland investigations into eHealth tools in physiotherapy are scarce and limited to small-scale studies (e.g. employee surveys or case studies) (Medbase, Citation2019a).
This contribution is part of a larger study that investigates the use of the mHealth tool physitrackTM (hereafter the app) and other eHealth tools used in ambulatory physiotherapy, adopting a workplace study approach (vom Lehn, Citation2019). It is undertaken in partnership with Medbase, which owns over 50 medical and physiotherapy outpatient clinics in Switzerland. Medbase provides physiotherapists and their patients with the app, which makes it possible to create and distribute home exercise programs, monitor patients’ progress and offer chat/video-based remote coaching and educational material.
In this article, we discuss the findings of our ethnographic fieldwork (Pollner and Emerson, Citation2001). The main aims of our ethnographic investigation were to reveal how the app and other eHealth tools are used in ambulatory physiotherapy practice and to identify what facilitates or hinders the app’s use and/or the full exploitation of its potential. From January to June 2020, we conducted non-participative observations of physiotherapists’ everyday work, carried out ad-hoc informal interviews with participating physiotherapists and patients and collected other ethnographic data at two Medbase outpatient clinics. Our analysis shows that physiotherapists and their patients barely use the app, much less fully exploit its distinct functions in daily physiotherapy practice. Furthermore, it identifies 16 factors on three distinct levels: 1) macro; 2) meso; and 3) micro that facilitate or hinder the use of the app and reveals their inextricable interdependence.
In a background section, we begin by discussing studies on eHealth tools in healthcare and physiotherapy. We then outline the adopted ethnographic research approach. In the findings section, we discuss our analysis of the app’s use/non-use in physiotherapy. Finally, in the conclusion, we bring together the themes and observations of the analysis and discuss its implications for further research on the use of mHealth tools in physiotherapy.
Background: Digital Technology in Healthcare
Digital technology is gaining ground in healthcare. Numerous studies report on its potential to improve healthcare practices in inpatient and outpatient care settings. It has been suggested that digital technology has facilitated communication between healthcare professionals (HCPs) and patients (Cai et al., Citation2017; Hilliard et al., Citation2014; Hinman, Nelligan, Bennell, and Delany, Citation2017), and made information exchanges between HCPs easier (Gagnon, Ngangue, Payne-Gagnon, and Desmartis, Citation2016). Digital technology has also increased patient self-efficacy (Blixt, Solbraekke, and Bjorbaekmo, Citation2021; Danbjorg et al., Citation2018; Hilliard et al., Citation2014); enhanced goal setting (Revenas et al., Citation2015); allowed for more personalized exercise plans for patients (Button et al., Citation2018; Hinman, Nelligan, Bennell, and Delany, Citation2017); improved adherence to home exercise programs (Danbjorg et al., Citation2018; Lambert et al., Citation2017) and physical activity (Revenas et al., Citation2015); and provided outcomes in rehabilitation care that are comparable or better than care without the incorporation of such technology (e.g. in terms of pain, functionality or quality of life) (Bennell et al., Citation2017; Corbetta, Imeri, and Gatti, Citation2015; Huber et al., Citation2017; Lambert et al., Citation2017; Lawford, Delany, Bennell, and Hinman, Citation2018; Nicholl et al., Citation2017), which may result in a reduced need for surgery (Danbjorg et al., Citation2018; Smittenaar et al., Citation2017).
Moreover, studies have highlighted users’ mostly positive perceptions of eHealth tools, for example their ease of use (O’Malley et al., Citation2014; Vorrink, Kort, Troosters, and Lammers, Citation2016) contribution to fostering self-management (Spasic et al., Citation2015; Vorrink, Kort, Troosters, and Lammers, Citation2016), and the option of monitoring one’s own progress (Cai et al., Citation2017; O’Malley et al., Citation2014). Similar positive patient experiences have also been reported with respect to physiotherapy practice (Button et al., Citation2018; Hinman, Nelligan, Bennell, and Delany, Citation2017; Lawford, Delany, Bennell, and Hinman, Citation2018; Medbase, Citation2019b).
Current adoption of eHealth tools among physiotherapists
Yet studies have pointed out that the adoption of eHealth tools among physiotherapists remains low (Blumenthal, Wilkinson, and Chignell, Citation2018; Button et al., Citation2018; Postolache, Oliveira, and Postolache, Citation2017). Interestingly, physiotherapists’ level of education (Wentink et al., Citation2019), age, gender, work setting, or professional experience (Blumenthal, Wilkinson, and Chignell, Citation2018) do not seem to have any influence on adoption rate.
In the Swiss context, research on the use and incorporation of eHealth tools in physiotherapy practice is rare. We identified a master thesis investigating the use of eHealth information by patients and its impact on physiotherapists’ perceptions of clinical practice (Schäublin, Citation2018); a report by the Swiss Physiotherapy Association with field experiences of therapists on various eHealth tools and electronic technologies (Physioswiss, Citation2017); and staff surveys on the use of physitrackTM by Medbase (Citation2019a). A recently conducted study on physiotherapists’ use and perceptions of remote physiotherapy during the first COVID-19 lockdown in Switzerland stated that during the lockdown, the percentage of physiotherapists treating patients remotely increased by 40% (Rausch et al., Citation2021). However, nearly 70% of the surveyed physiotherapists were not convinced that remote physiotherapy could be used as an additional treatment approach after COVID-19 restrictions ended, and 43.8% had no interest at all in continuing remote therapy.
Outside of Switzerland, most of the studies discussed above have focused on the process of implementing specific digital health tools (Dunphy, Hamilton, Spasic, and Button, Citation2017), providing interesting insight into what facilitates or poses an obstacle to its implementation in physiotherapy practice, the question to which we will turn now.
Barriers to eHealth implementation in physiotherapy
Qualitative interviews and mixed-method studies have revealed a hindering impact of physiotherapists’ perceptions and attitudes regarding the use of eHealth tools and their approach to implementing them in their day-to-day practice. Therapists criticize the lack of reimbursement for digitally mediated treatments (Hinman, Nelligan, Bennell, and Delany, Citation2017; Postolache, Oliveira, and Postolache, Citation2017; Wentink et al.,); uncertainties about laws and regulations on data privacy (Schäublin, Citation2018); a lack of clear evidence for eHealth tools having a positive impact in terms of treatment quality, efficiency and lower treatment costs (Endl, Jäschke, Thiel, and Wickinghoff, Citation2015); and a lack of quality certifications for eHealth tools (Schäublin, Citation2018; Wentink et al., Citation2019). Further barriers include technical issues (e.g. insufficient technical resources) (Postolache, Oliveira, and Postolache, Citation2017); cost of implementation and maintenance (Postolache, Oliveira, and Postolache, Citation2017; Schäublin, Citation2018); unclear implementation policy (Postolache, Oliveira, and Postolache, Citation2017); lack of familiarity with implemented eHealth tools (Button et al., Citation2018); insufficient continuous training for physiotherapists on eHealth tools (Medbase, Citation2019a; Medbase, Citation2019b; Wentink et al., Citation2019); and impractical eHealth tool design, (e.g. when important functions are missing) (Medbase, Citation2019a; Medbase, Citation2019b; Postolache, Oliveira, and Postolache, Citation2017).
Physiotherapists are furthermore concerned about treatment quality, for example, since their ability to correct a patient’s exercise performance would be limited in remote consultations (Hinman, Nelligan, Bennell, and Delany, Citation2017) and also about the high administrative burden (Button et al., Citation2018) and the time they would need to devote to the digital health tools compared to the therapy time (Dunphy, Hamilton, Spasic, and Button, Citation2017; Medbase, Citation2019a; Medbase, Citation2019b), and some worry that the application of eHealth tools might give a false impression regarding physiotherapists’ core competences (Blixt, Solbraekke, and Bjorbaekmo, Citation2021).
Finally, it is argued that a lack of digital health literacy among professionals and patients (Postolache, Oliveira, and Postolache, Citation2017) and therapists’ low confidence in using eHealth tools can make their adoption difficult (Button et al., Citation2018). Digital health literacy, or eHealth literacy for short, is the ability of end-users (i.e. patients and professionals alike) to find, understand, and transfer digitally mediated healthcare information into their work and/or everyday life in order to improve patient health (Norman and Skinner, Citation2006). The term also refers to the skills and knowledge an individual needs to successfully interact with eHealth tools (Chan and Kaufman, Citation2011).
Facilitators to the implementation of eHealth tools in physiotherapy
In contrast to the hindering elements discussed above, physiotherapists remark that an eHealth tool can help them become more efficient in their daily work (Schäublin, Citation2018) and function as a digital assistant during physiotherapy interventions (Blixt, Solbraekke, and Bjorbaekmo, Citation2021). Perceived good eHealth literacy in patients (Button et al., Citation2018); enough time to improve one’s own proficiency in using and tinkering with digital health tools (Blixt, Solbraekke, and Bjorbaekmo, Citation2021); availability of peer support (Wentink et al., Citation2019); and a tool’s perceived usefulness (e.g. in terms of value for daily practice) (Blumenthal, Wilkinson, and Chignell, Citation2018; Button et al., Citation2018) are further facilitators for the adoption of digital health tools.
Finally, and on a slightly different note, studies have highlighted therapists’ feeling that using eHealth tools alters their professional practices and their organization in a profound way (Blixt, Solbraekke, and Bjorbaekmo, Citation2021; Schoeb and Hiller, Citation2018). This transformation of current working practices implies not only new forms of interventions and communication between patients and therapists (Button et al., Citation2018; Hinman, Nelligan, Bennell, and Delany, Citation2017), but also requires them to rethink their roles, learn new ways of doing things, and acquire new competences (Vestergaard, Citation2021).
In summary, the studies discussed above reveal a number of elements that explain why the adoption and use of eHealth tools in physiotherapy progresses slowly and remains rather low, and some of them also argue that the implementation of eHealth tools in healthcare/physiotherapy raises important questions regarding their impact on physiotherapy practice, healthcare provider-patient interaction, and with respect to what is involved concerning the end-user’s competences, mutual expectations, etc. Most of the studies are based on data obtained through structured or semi-structured interviews and surveys. They rely on professionals’ and patients’ accounts of their experiences with and perceptions and representations of digital tools in healthcare/ physiotherapy and/or on information regarding participants’ age, gender, educational background, etc. We argue that for a better understanding of what eHealth tools’ implementation involves for physiotherapy practice and users, and how hindering/facilitating factors interact with each other, more in-depth qualitative research is required. In the following section, we first outline the adopted ethnographic research approach and then present and discuss our empirical findings.
Methods and Materials
This contribution is part of a larger study that investigates the use of the app in ambulatory physiotherapy, adopting a workplace study approach (vom Lehn, Citation2019). The workplace approach has emerged in the context of technological developments, whose initial aim to support collaborative activities and social interaction in workplaces has not been fully achieved in practice (Luff, Hindmarsh, and Heath, Citation2000). Workplace studies investigate the situated organization of collaborative professional practices and the ways participants mobilize and coordinate the handling of technology, tools, and other artifacts for their accomplishment (Luff, Hindmarsh, and Heath, Citation2000). Unpacking the situated organization of practices, these studies show that for the functioning of the collaboration in general and for the efficient use of technology in particular, participants’ “minute action is critical” (vom Lehn, Citation2019). Our study investigates use of the app as part of situated working practices and interactions between the physiotherapist and patient and seeks to understand “lived ordering” (i.e. “how participants in […] concrete circumstances […] concertedly organize, recognize, use and achieve whatever they regard or define as sensible, rational, intelligible or orderly”) (Pollner and Emerson, Citation2001). To do so, we first conducted ethnographic fieldwork. On the basis of our ethnography, we then video-recorded physiotherapy consultations in which the app was introduced and/or used, and interviewed the filmed physiotherapists (N = 4) and patients (N = 8) on their subjective stance and experiences with the app. Three authors were involved in this fieldwork: Sara Keel: SKE; Anja Schmid: ASC; Fabienne Keller: FKE.
This contribution focuses on the findings of our ethnographic fieldwork. Its main aims were to provide for a better understanding of how eHealth tools and the app are used in physiotherapy practice, and to reveal factors that facilitate or hinder the use of the app and/or the full exploitation of its potential. Our study partner, Medbase, helped us make contact with outpatient physiotherapy clinics. At the beginning of 2020, two sites in German-speaking Switzerland (hereafter site A and site B) agreed to participate. Once the requirement for approval had been waived by the respective Cantonal Ethics Committees, we conducted the ethnographic fieldwork from the end of January to June 2020. We obtained informed written consent from all participating physiotherapists and patients. In accordance with the terms set forth on our consent form, we anonymized all names and have used abbreviations to refer to the participants: physiotherapist 1: PHY1; patient 1: PAT1.
Different levels of engagement from the researcher in the field are recommended for various distinct approaches (Cruz and Higginbottom, Citation2013; Pink and Morgan, Citation2013; vom Lehn, Citation2019). Depending on their chosen engagement level, researchers might aim to “go native” (Pollner and Emerson, Citation2001), become a “competent member” (Pollner and Emerson, Citation2001) of the studied community (see the notion of unique adequacy introduced by Garfinkel (Citation1967)), or just spend short periods in the field to get a general grasp of the studied setting and/or to conduct theory-driven, “structured observations” (Mulhall, Citation2003). Not wanting to impede the physiotherapy practice in any way (Pink and Morgan, Citation2013), while at the same time seeking to investigate participants’ situated use/non-use of the app from an emic perspective, meaning from a users’ perspective, we opted for a non-participative, “bottom-up” ethnographic approach (Pollner and Emerson, Citation2001).
We followed the physiotherapists in their daily work to observe how their use, or rather non-use, of the app was handled, understood, talked about and oriented to by participants during physiotherapy consultations, team meetings, physiotherapists’ administrative work, and an introductory session to the app held for a new team member of site B. Drawing on a list of questions that we wanted to address with participants of the study and also on our exploratory observations, we conducted informal ad-hoc interviews with physiotherapists during their breaks and/or administrative time. These interviews allowed us to elicit the physiotherapists’ explanations and understandings of our observations (Mulhall, Citation2003) and to gain further insight regarding their use and non-use, experiences, understandings, and perceptions of digital health tools in general and of the app more particularly. While seeking informed consent from patients, we further collected information on 50 participating patients (i.e. age, gender, use, and attitude toward digital tools) and received some occasional accounts of their take on the app more specifically. Finally, we obtained procedural and other relevant internal documents (vom Lehn, Citation2019) and tried out the app ourselves using both the patient’s and the therapist’s interfaces to further deepen our understanding of the app from a user’s perspective.
Due to COVID-19 restrictions, during which face-to-face physiotherapy consultations were limited to emergency patients, our fieldwork, and data collection were interrupted for three months, from mid-March to late May 2020 ().
Table 1. Data collection and number of participants during ethnographic fieldwork.
Throughout our fieldwork, we took handwritten notes while observing or conducting informal interviews with physiotherapists and patients, made drawings and took photos of observed interactions and their settings. The aim was to focus on both “action and dialogue” and to provide “descriptions that portray the physical environment, people, actions and smells which make up a setting,” and “transcription […] of something that was said” (Mulhall, Citation2003). This material was revised and digitalized by the respective author as soon after the conducted fieldwork as possible.
Altogether, we compiled 116 pages of chronologically organized data in the form of typed descriptions of actions, photos or scanned drawings of observed interactions and their settings and line-by-line renderings of informal interviews with physiotherapists and patients, conversations among physiotherapists and/or between physiotherapists and patients, and last but not least, the researcher’s reflections on the ways the researcher considered distinct fieldwork experiences and collected material, as constituting another piece to the question of how eHealth tools and the app’s use or non-use in physiotherapy practice is handled, understood, talked about and oriented to by physiotherapists and/or patients.
During our fieldwork and the period of time it was on hold, our discussions of each researcher’s revised material, the procedural documents we collected, and our own testing of the app allowed us on the one hand to specify the use or non-use of the app and its distinct functions with respect to situated physiotherapy practices, such as distributing a home exercise program to the patient or requiring the patient to accomplish an assessment test. On the other hand, our aim was to come to a shared understanding of how each observation (i.e. description of situated actions/practices, transcription of dialogue or procedural document) allows a better appreciation of the factors that contribute to the use/non-use of the app at the different sites. Our thorough and repeated discussion of the observations revealed their complex and multilayered nature. Discussing the material at hand was key to disentangle different physiotherapy practices, to distinguish them as facilitating (+) or hindering (-) the use of the app, and as belonging to distinct overarching factors that can be attributed to one of three levels: 1) macro- (i.e. healthcare system); 2) meso- (i.e. institutions) or 3) micro-level (i.e. individuals/interactions). For some observations, both facilitating and hindering effects were made concurrently relevant: for instance, in one of the observed sites, the team organized a one-hour introduction to the app for a new colleague. On the one hand, we observed how the introduction provided physiotherapists with a training opportunity that encouraged and enabled them to use the app. On the other hand, during this introduction, physiotherapists reported on difficulties with the app that hindered its use.
The differentiation of physiotherapy practices, their identification as hindering or facilitating the use of the app, their attribution to distinct factors, and their mapping onto the macro-, meso- or micro-level, allowed us to formulate primary findings that then iteratively informed and incorporated further field observations and discussions. All in all, the bottom-up approach that we adopted meant that our analysis had to begin before and to continue during fieldwork (Mulhall, Citation2003). For example, we drew on the literature (see the background section) and our first-hand experience with the app to prepare a list of questions for informal interviews with participants before the fieldwork. During the fieldwork, our analysis of collected materials helped us to formulate new questions or specify others. The analytic process required not only a continuous back and forth between the analysis of fieldwork material and the collection of further data in order to deepen our analysis, but also between the findings obtained in this way and our discussions of the literature (see the background section). This way of conducting our analysis was time-consuming and challenging. However, instead of presupposing specific ways that the app is used and/or potential hindering/facilitating factors prior to our fieldwork and then using the fieldwork mainly to validate them (Mulhall, Citation2003), we reached shared understanding with respect to the findings presented below by repeatedly analyzing and discussing the material and findings we obtained throughout our fieldwork or identified in the literature.
Findings
Our ethnographic fieldwork at two outpatient physiotherapy clinics (sites A and B) revealed how Medbase physiotherapists use the app in their daily work and pointed to 16 distinct factors having an impact on the adoption and use of the app as well as its potential for physiotherapy interventions. In the following section, we will first outline our main observations of the ways the app was used at sites A and B, then present an overview of identified facilitators and barriers and finally discuss related factors in more detail.
Investigating the use of the app in physiotherapy practice
Throughout ethnographic fieldwork, we came to understand that the app provided to Medbase physiotherapists and patients has a number of resources and distinct functions, most notably: 1) it offers approximately 4,500 therapeutic exercise videos, which include spoken and written instructions on how to do the exercise. These videos are a base that the physiotherapists can use to compile and distribute home exercise programs to their patients; 2) while physiotherapists can define the frequency and number of repetitions, and introduce an individualized specification for each exercise in a patient’s program, patients can set reminders, confirm that they performed the exercise(s) and subsequently assess the pain level involved with a specific exercise and/or send a personalized comment about an exercise to the physiotherapist; 3) once patients confirm their completion of the exercise via the app, it generates statistics and/or graphs showing how often they did their home exercise program and how much pain they had during it. The app thus allows physiotherapists and patients to monitor frequency of use, pain levels for a specific exercise and patients’ progress; 4) physiotherapists can send online assessment questionnaires to the patient, who can then respond via the app; 5) physiotherapists can send online educational material to the patient via the app; and 6) physiotherapists and patients can securely communicate over chat and participate in remote video coaching.
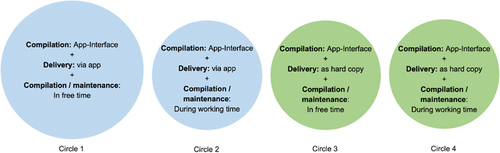
As already identified by internal surveys (Medbase, Citation2019a; Medbase, Citation2019b; Medbase, Citation2019c) our ethnographic observations confirmed that physiotherapists’ use of the app remains low overall; only a small proportion of Medbase physiotherapists use the app on a regular basis and suggest it to their patients. Those who do regularly use the app do so to compile exercise programs and distribute them to their patients, as shown in .
We observed that most physiotherapists compile exercise programs for patients outside their paid working time, as indicated in circles 1 and 3 in . Only a minority manages to compile the program during the session with the patient and/or during their working hours. We will come back to this issue later. Moreover, a large number of physiotherapists compile exercise programs with the app but then give them to the patients in hard copy (circles 3 and 4). In such a case, the physiotherapist uses the app for physiotherapy practice but the patient does not. Practices such as incorporating the app into interactions during a consultation, explaining it to the patient, using it as a resource for at-home exercise and remote communication are not found in these cases. Moreover, as below shows, therapists using the app did not exploit all of its different functions.
Table 2. Physiotherapists’ use of different functions of the app.
While several physiotherapists used the app to create home exercise programs, distributing them to patients either via the app or in paper form and, in the former case, communicating with them using the chat function, practically none of them used the other functions or mentioned having used them during our fieldwork. Instead, physiotherapists used alternative digital (health) tools (i.e. e-mail, anatomy-app, video-call tool, and phone), or non-digital resources (i.e. paper questionnaires for assessments).
The app’s low adoption rate and the limited deployment of its distinct resources and functions, and thus its potential for physiotherapy can be better understood from our ethnographic fieldwork, which sheds new light on the factors that facilitate or hinder adoption and use of the app in practice.
Factors hindering or facilitating adoption and use of the app
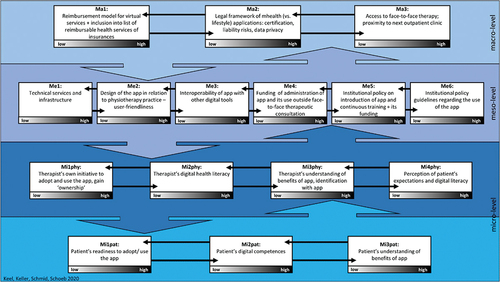
Overall, we identified 16 factors that impact adoption and use of the app. As shown in below, these factors can be differentiated into three levels: 1) the Swiss healthcare system level (macro-level; Ma1-3); 2) the institutional level (meso-level; Me1-6); and 3) the individual and interactional physiotherapist-patient level (micro-level; Miphy1-4; Mipat1-3).
The low-high bar at the bottom of each factor refers to the fact that in practice, the observed configuration of an individual factor might either hinder (low) or facilitate (high) adoption and use of the app. However, the impact of a single factor cannot be grasped per se but needs to be looked at as one piece of a dynamic interplay. The factors influence each other horizontally. See the horizontal arrows between distinct factors inside a given level in . They also influence each other vertically (i.e. factors of different levels: general (macro-level); more site-specific (meso-level); or interactive/individual (micro-level) factors have reciprocal impacts). See the vertical up-and-down arrows between the distinct levels in .
In the following sections we discuss the three levels and the identified factors in more detail. We provide selected quotes and observations taken from our fieldwork notes (excerpts 1–43) to illustrate our summary discussion of each factor and to point to a large number of practical organizational issues involved in daily work using the app. The excerpts are indicated with the respective date of fieldwork, abbreviation of researcher’s name, and page number of type-written revised fieldnotes. The original excerpts are in German or Swiss-German. For reasons of space, this article presents only the English translations.
Macro-Level – Healthcare System Level
The influencing factors identified on the macro-level (Ma1-3) concern the Swiss healthcare sector, referring to national regulations and definitions with respect to the use of mHealth tools in healthcare generally and in ambulatory physiotherapy more particularly. The three identified factors concern national reimbursement models for virtual services in physiotherapy (Ma1), legal frameworks on certification, liability risks, and data protection connected to mHealth tools versus lifestyle applications (Ma2), and last but not least, availability of and access to face-to-face physiotherapy consultations and other services (Ma3). As we will see in what follows, in Switzerland, these three issues are organized in a way that hinders rather than facilitates the use of mHealth solutions in ambulatory physiotherapy.
Ma1: reimbursement model for virtual services and inclusion in insurance providers’ list of reimbursable health services
The first factor on the macro-level refers to the lack of national tariff regulations with respect to reimbursement models that include virtual healthcare services and mHealth solutions. As several physiotherapists pointed out, Swiss regulations (Article of Law SR 832.102.5, art. 2a.) on the obligation for the therapist and patient to be physically co-present during physiotherapy services and the absence of financial incentives (Endl, Jäschke, Thiel, and Wickinghoff, Citation2015) can discourage physiotherapists from using the app.
Excerpt 1:
PHY5: That’s all great, but it [using the app] just takes time. Also sending the PDF by e-mail or by postal mail, again, something extra. And we can’t charge for it. Now [after COVID-19 restrictions] it works because we don’t have full schedules yet. But later. I don’t know … I just find it really difficult that we can’t bill for it. Did you hear from Physioswiss [Swiss physiotherapy association]? They had negotiations with the health insurance companies regarding the tariff for video-consultations and were only able to negotiate an MTT (Medical Training Therapy) tariff. That never covers an individual treatment. (200609_FKE, p.6)
Physiotherapists also mention the loss of earnings associated with increased virtual consultations and mHealth solutions in the outpatient sector. According to them, it should be reimbursable for healthcare providers if it is not to act as a major barrier to using the app. To facilitate the use of mHealth tools in physiotherapy, incentives for their targeted use oriented to the patient experience therefore need to be introduced.
Ma2: legal framework of mHealth (vs. lifestyle) applications: certification, liability risks, and data privacy
The second factor on the macro-level addresses the necessity of adopting a national legal framework that makes it possible to distinguish mHealth tools from lifestyle (fitness) applications, to set the terms and conditions for certification of the former, and to clarify liability risks and data privacy issues. With respect to these matters, our observations indicate that certain physiotherapists and patients assess the app’s trustworthiness as rather low. From the patients’ perspective, regulations with regard to data security connected with the app might not be fully transparent and/or comprehensible.
Excerpt 2:
PAT25 feels that for him as a patient, the first question and concern about a digital tool, such as the app, would be about data security: where does my data go? Who owns the tool? Apart from the data protection issue, the advantages of digital tools are “obvious.” (200306_ASC, p.11)
From the physiotherapists’ perspective too, it is unclear how privacy can be guaranteed when using the app or at what point it could be violated.
Excerpt 3:
PHY1/PHY3 mention that they use patients’ private cell phones during the sessions, in order to film the patient, for example, when he does a therapeutic exercise. Patients thus have access to the video when they do the exercise at home and can watch it repeatedly, while having the instructions of the physiotherapist at the same time. PHY3 finds this type of video much more useful than the exercise videos provided by the app, and appreciates the fact that it is completely safe in terms of confidentiality/data protection. As it is the patient’s cell phone, the patient has control over it. He can delete it whenever he wants. (200211_SKE, p.2, 6)
Excerpt 4:
PHY6 mentions that he usually does not send the access code for the app but gives it to the patient verbally during the session, because of privacy issues … (200128_introduction app_ASC, p.2)
Altogether, our observations suggest that facilitating the use of mHealth tools in ambulatory physiotherapy on the macro-level requires increasing their trustworthiness for patients and physiotherapists. Endl, Jäschke, Thiel, and Wickinghoff (Citation2015) argue that achieving this goal involves on the one hand making a clear-cut distinction between mHealth solutions, whose purpose is to initiate or monitor medical therapies, diagnoses, or implement screening/prevention measures, and lifestyle applications, which are intended merely for wellness/fitness purposes. On the other hand, they state that it also requires the existence of a legal framework that sets forth the terms with respect to certification of mHealth tools, uniform standards, distribution via trusted platforms and data privacy, as well as transparency about data security and legal certainty regarding liability risks.
Ma3: access to face-to-face therapy; proximity to next outpatient clinic
The third factor on the macro-level concerns the easy accessibility of face-to-face physiotherapy consultations in Switzerland. At both sites, we observed that face-to-face consultations and opportunities to do exercises under a therapist’s supervision and with other patients play an important social and motivating role.
Excerpt 5:
PHY4: For a moderate additional amount, Medbase patients can come to our training room 3 times a week. They have their individual exercise program that we generate with the app and usually print out for the patient. There is always a physiotherapist available to explain, supervise, help, etc., if needed. Many come regularly to have motivation to exercise and/or for social reasons … (200211_SKE, p.9)
Furthermore, physiotherapists mentioned that if the context did not require it, patients were not interested in using the app as a means for remote consultation and coaching. This became evident when we resumed our ethnographic fieldwork after the COVID-19 restrictions (March-May 2020) ended.
Excerpt 6:
FKE: Do you still use video calls, chat, etc. [on the app]?
PHY9: No, it’s flattening out. People also prefer to come to therapy with physical contact. (200609_FKE, p.2).
Excerpt 7:
PHY5: Often the phone was enough [during COVID-19 restrictions]. But now people prefer to come directly to therapy again anyway. (200609_FKE, p.6).
As illustrated in the above quotations, neither the app nor its functionality for remote consultation/coaching meet patients’ preferences for social connection, motivation, and physical contact. The proximity and/or easy accessibility of face-to-face outpatient physiotherapy consultations and services thus hinder rather than facilitate adoption of the app and exploitation of its full potential.
Factors on the macro-level: facilitators or barriers
In the context of the Swiss healthcare system, an absence of incentives with respect to reimbursement models for virtual services in physiotherapy (Ma1), an absence of legal frameworks regarding data security, certification of mHealth tools and liability risks (Ma2), and patients’ proximity and easy access to face-to-face physiotherapy services hinder the deployment of the app for remote physiotherapy practices (Ma3). These factors converge and reinforce each other, forming a significant barrier to the regular use of mHealth solutions in general and the use of the app in physiotherapy more particularly.
Meso-Level in Detail – Institutional Level
The influencing factors identified on the meso-level (Me1-6) concern the institutional aspects of the observed outpatient physiotherapy clinics. Note that in our case, the institutional level is twofold. On the one hand, Medbase provides the app, funds access to it and the necessary infrastructure, such as WLAN service and the devices necessary to run it (e.g. iPad, laptops, and desktop computer), and designates a person from the management team to handle contacts with the developer of the app, be responsible for technical support, and continue the app’s development in terms of design and interoperability with other tools (see Me1-3). Altogether, these meso-level investments are important prerequisites and thus key facilitators for the adoption and use of the app in ambulatory physiotherapy, despite the fact that in practice and from physiotherapists’ point of view, these factors also present some hindering elements.
On the other hand, each Medbase site is responsible for and has, within the institutional boundaries, room for maneuver to adapt meso-level factors Me4-6 to its specific context. These factors describe several responsibilities: regulations concerning funding of the administration and use of the app outside of face-to-face therapeutic interventions (e.g. to create an exercise program for a patient via the app) (Me4); organizing the introduction of the app to newcomers, ongoing training, and decisions on the funding of training (Me5); and developing institutional policy guidelines regarding use of the app (Me6). Our ethnographic observations at sites A and B revealed that the ways in which these three factors (Me4-6) are managed and organized differ considerably from site to site, having a facilitating impact on the app’s use at one site (B) but a hindering impact at the other one (A). Moreover, our observations suggest that the management and organization of these three factors seem to be contingent on a site’s team composition (see for example Me5 and Me6 below) and salary model (fixed salary at site A, versus salary based on turnover at site B). For reasons of space, we cannot discuss this last point any further here.
Me1: technical services and infrastructure
The first factor on the meso-level has to do with the supply of technical devices and infrastructure that enable the use of digital health tools in general and the app in particular. More specifically, our observations revealed that digital devices must be easily accessible and it must be possible to use them during daily therapy for the app to be used.
Excerpt 8:
PHY2: Generally, I have not used the app much lately. It is quicker to take a piece of paper [to sketch a home exercise program]; often the WIFI reception is not good. (200211_SKE, p.5)
Furthermore, since the therapist monitors the app via an online platform, patients can download their program there as well, and various functions of the app are web-based, a strong and stable internet connection is key for the app to be used.
Excerpt 9:
FKE: Some physiotherapists told me that during the COVID-19 restrictions you didn’t use the app for the video treatments. You used EmergencyEye. Why?
PHY5: Let me think. The problem was, I think, that our internet network was not strong enough. And with this EmergencyEye you only see the patient, but he doesn’t see us. Therefore, you need less data and a less strong WLAN connection. And I also think that with the app, we would have had to pay even more fees for this extra video telephony function. (200609_FKE, p.7)
The app, as well as the operating systems and software used to manage it, also need regular updates and coordination between updates.
Excerpt 10:
During the introduction to the app:
PHY6: Ah and by the way, it matters which browser you use. I always have problems with Internet Explorer, it doesn’t update the program. Chrome is better, with Safari I don’t know. (200128_introduction app_ASC, p.3)
As the illustrations above show, the availability and unobstructed functioning of digital devices and technical infrastructure required for the app to be used efficiently are considered prerequisites for its integration into everyday practice and thus facilitate its use.
Me2: design of the app in relation to physiotherapy practice – user-friendliness
The second factor on the meso-level concerns the app’s design, interface, and user-friendliness. Our observations regarding physiotherapists’ handling of the app when compiling exercise programs, for example, suggest that its design and interface also play a role in impeding its usage. Physiotherapists stated that the app should have content that is well organized and easy to find, with intuitive naming systems or filter functions, and also compatible with current physiotherapy practices and approaches.
Excerpt 11:
While looking for a specific exercise to add to an exercise program:
PHY9: You know, sometimes you don’t see the nuances of the exercises. Then I have to click on them and watch the video. Then they always sit there for the first few seconds and don’t do anything …
PHY9: And when I enter the keywords strength, musculoskeletal, shoulder, elbow and cervical spine into the filter, a ballet plié appears! And the whole thing is not organized at all, there is no system in it. (B_200128_introduction app_ASC, p.1)
About one month later:
PHY9: Other problem: there are exercises for which no standard names exist, no “official names”. Official names for strength building (fitness) are mostly no problem, easy to find. But if you are looking for exercises that don’t have an official name, then it’s difficult […] to find because there are so many exercises. (200303_SKE, p.9)
Moreover, the type, coverage, quality, and visual presentation of the content that is provided and captured by the app should correspond to physiotherapists’ expectations.
Excerpt 12:
PHY9: The outfits of the people in the app’s exercise videos are inadequate. We do work with patients, not in a fitness studio. (200303_SKE, p.8)
Additionally, the functions that the app provides, for example to individualize a home exercise program, ought to be congruent with professionals’ and patients’ expectations, for example with respect to patient-centered physiotherapy.
Excerpt 13:
ASC: What do you do if, for example, a patient is only allowed to use an exercise with one weight?
PHY4: You can put that in the “comment” option.ASC: Do you use this option?PHY4: Yes! You can also do exercises yourself. Wait a minute … ((shows ASC an exercise video that a colleague of hers recorded.))ASC: But you can’t print them out?PHY4: No.ASC: Have you already uploaded videos yourself?PHY4: No.(200306_ASC, p.13)
Finally, the app and its interface should be user-friendly on any device.
Excerpt 14:
PHY4 states that she uses the app regularly. She would compile exercise programs after the consultation [with the patient]. She finds its interface on the iPad to be not very user-friendly, so she would use the desktop computer in the common room for that. (200211_ ASC, p.12 f.)
Overall, our ethnographic fieldwork showed that to facilitate the use of the app, its design and interface need to be user-friendly and in line with physiotherapists’ and patients’ expectations and everyday practice. This allows physiotherapists to deploy the app’s various possibilities, functions and contents more easily and efficiently. Efficiency is key in the Swiss context, in which physiotherapists’ work with the app outside of face-to-face consultations with the patient is not reimbursed (see Ma1 and Me4).
Me3: interoperability of the app with other digital tools
The third factor on the meso-level involves interoperability between distinct devices, tools/software, and the app. At the examined sites, physiotherapists use different digital devices and health tools, including various software designed to meet legally binding documentation requirements and to accomplish and/or support various organizational and daily administrative tasks. Our observations suggest that two interdependent aspects of interoperability are particularly critical for adoption of the app. First, there is the question of whether the app could benefit from the exchange of data and information introduced in other devices, tools/software, or vice-versa.
Excerpt 15:
PHY9: I don’t really need the assessment questionnaires [on the app], because you only get the score and not the patient’s answers to the questions. I don’t think that it is adequate in relation to the documentation requirement. We actually have to keep the assessment questionnaires for 10 years. Having a general score is not enough. (200303_SKE_ p. 9)
Second, interoperability also depends on the possibility of transferring data introduced in and/or compiled using the app directly to other devices and tools/software and vice-versa.
Excerpt 16:
Follow-up sessions with patients are introduced in the digital planning tool on the desktop computer. It’s located in the common room and is not connected to the app, which runs on an iPad … (200211_SKE, p.1, 5)
Excerpt 17:
PHY8/PHY9/PHY10: Point out that printing out an exercise program that one compiled using the app is very inconvenient as you first have to save it to the desktop and only then, you can print it. (200128_introduction app_FKE, p.1)
At the observed sites, interoperability between the app and other commonly used digital devices, tools, and software was perceived as limited by the physiotherapists. To compensate for the limited interoperability, the physiotherapist needed to invest additional time and effort, which was a further obstacle to the app’s use and integration into processes, physiotherapy practices, and tasks.
Me4: regulations concerning funding for the app’s administration and its use outside of face-to-face therapeutic consultations
The fourth factor on the meso-level concerns institutional regulations and salary models that take into account funding for using the app outside of face-to-face consultations. For example, physiotherapists recurrently mentioned working with the app before or after their session with a patient in order to prepare, compile or update a patient’s exercise program.
Excerpt 18:
PHY1/PHY4: Physios have 1/2 hour of (paid) admin time in the morning and in the afternoon. During this time, they have to do many administrative and organizational tasks: contacting the doctor; billing; closing cases; documentation; cleaning equipment; compiling programs with the app for MTT (Medical Training Therapy), … Physios who want to work with the app are more or less forced to spend time outside of the sessions with the patient to compile individualized exercise programs, etc. (200211_SKE, p.5)
Excerpt 19:
PHY6: In the end, we had much more time [during COVID-19 restrictions] for everything that we would not have otherwise and would not be paid for. We didn’t earn anything while compiling programs [via the app] for the MTT visitors and the patients. It was simply about maintaining the client base. (200609_FKE, p.1)
Furthermore, whenever physiotherapists did conduct interventions, consultations, and supervision via the app’s remote functions (e.g. chat, phone or video conference) this also required them to work outside of face-to-face consultations and/or paid administrative working time.
Excerpt 20:
PHY8: For me, the decisive factor [for using the app more during COVID-19 restrictions], was that I had a lot of [consultation-free, but paid] time …. That was great.
PHY9: But you know, if we extrapolate how many hours it took us [for example to compile exercise programs, etc. during this time], no employer would pay that (in normal times). (200609_FKE, p.4)
These observations suggest that institutional funding regulations and salary models, which compensate for an absence of financial incentives on the macro-level (Ma1 above) at least partially, promote physiotherapists’ increased use of the app and in turn their appropriation of new remote therapeutic practices. They relieve the physiotherapists’ burden of working during unpaid free time if they want to include the app in their service.
Me5: institutional policy on the app’s introduction and continuous training as well as funding for training
The fifth factor on the meso-level involves site-specific institutional guidelines and strategies regarding staff’s acquisition of digital health literacy in general, or with respect to the app’s specific affordances more particularly. Observing the institutional processes at the sites, we identified the various efforts to facilitate the use of the app. For instance, new team members were systematically introduced to the app’s functions and how it can be successfully used in physiotherapeutic practice.
Excerpt 21:
PHY6 conducts a one-hour introduction to working with the app for new staff (PHY9). PHY7, PHY8 and PHY10 attend the introduction as a refresher. (200128_introduction app_ASC, p.1)
Furthermore, a key user in the team, who has teaching abilities and practical expertise with the app, was capable of providing necessary ad hoc training to less competent colleagues.
Excerpt 22:
PHY6 has no specific training to work with the app. He just works with it regularly and became the “expert” in the team. (…) PHY6 has compiled a manual where it is explained step by step how to do what and where. (200128_introduction app_ASC, p.1)
Moreover, one physiotherapy site decided to make regular ad-hoc or planned opportunities for continuous training available to all staff members. They looked in particular at specific details related to handling the app in physiotherapy practice.
Excerpt 23:
During a team meeting
PHY5: For me the question is whether you need 1–2 hours to deal with the app, to reacquaint yourselves with it again?
PHY?: Yes, 1–2 hours is certainly useful.
PHY5: Then I’ll plan 1–2 hours for April so that you have time to familiarize yourselves with the tool … (200303_SKE, p.11)
Finally, introductory courses and/or these continuous training opportunities were provided during physiotherapists’ working hours and were therefore funded by the institution.
Excerpt 24:
PHY10: If you expect them as physios to delve into the app, to use it, they should be given time to do so. There is no time in our current work schedules for such familiarization. (200128_introduction app_ASC, p.3)
All in all, we observed that offering introductions, as well as opportunities for continuous and ad-hoc training during paid working hours, allowed physiotherapists to get accustomed to the app, learn its functions and use the app more readily. Facilitating the acquisition of indispensable digital health literacy encourages and enables the employees to use the app in daily physiotherapy practice and thus increases its adoption rate.
Me6: institutional policy guidelines regarding the app’s use
The sixth factor on the meso-level has to do with site-specific guidelines and best practices regarding the app’s use. We noted that the teams may establish and share explicit instructions or goals regarding how often to use the app and related best practices.
Excerpt 25:
At Site B: PHY6: the team’s target is for all PHYs to put together at least 5 exercise programs by June. (200128_introduction app_ASC, p.1)
In contrast to site B, at site A there were no common goals:
Excerpt 26:
PHY1: Some physios never use it and have also forgotten their password, for example. […] I think we have reached the point where some use the app regularly and others never do. […] Theoretically, everyone knows that the app exists. Now it’s up to the individual to use it or not, right? (200211_ ASC, p.8)
Moreover, depending on the site, different standard uses are agreed upon for the app’s various functions (e.g. chat, video, and compilation of exercise programs) and/or for specific patient groups in order to achieve their respective treatment goals (e.g. increased muscle strength).
Excerpt 27:
For the Medbase MTT (Medical Training Therapy) group, the app is used systematically so that the various participants in the group have an individualized exercise program at their disposal, which they should then also work through regularly at home. (200211_SKE, p.3)
Finally, there were also site-specific regulations regarding data privacy and data protection (see Ma2 above). Our observations suggest that the existence of institutional guidelines and best practices make it easier for physiotherapists to work regularly with the app, increasing the likelihood that it will become part of their routine practices. Meanwhile, absence of such guidelines and best practices promotes a usage of the app that is informed by a team’s composition and their practices.
Factors on the meso-level: facilitators or barriers
Overall, our observations reveal that in the Swiss context, facilitating the app’s adoption in physiotherapy on the meso-level involves compensating for a quasi-absence of incentives for the adoption of mHealth solutions on the macro-level (see the macro-level in detail above). The meso-level must invest considerably in order to provide technical support and meet infrastructure affordances that correspond to the app’s adoption by physiotherapists and patients in consultations (Me1); finance and contribute to the continuous development of the app’s design and interface to bring it into line with current physiotherapy practices (Me2); meet rapidly changing interoperability requirements between the app and other digital (health) tools and devices (Me3); establish regulations and at least partial funding of the app’s administration and its use outside of face-to-face consultation (Me4); fund, organize, and design an introduction to the app for new team members and continuous education related to the app for all physiotherapists, while taking into account physiotherapists’ and site-specific heterogeneous needs (Me5); and provide experience-based guidelines and best practices for its use (Me6).
Micro-Level in Detail – Individual and Interactional Physiotherapist-Patient Level
The factors that facilitate or hinder the app’s use on the individual and thus micro-level concern physiotherapists’ and patients’ eHealth and digital literacy, attitudes, and stances toward the app (Mi1-3phy and Mi1-3pat), and therapists’ assumptions regarding patients’ literacy (Mi4phy). For reasons of clarity, we will discuss the factors concerning the physiotherapists (Mi1-4phy) and patients (Mi1-3pat) separately. However, as will become evident through the illustrations (excerpts 28–43 below), in practice, factors concerning physiotherapists (Mi1-4phy) and patients (Mi1-3pat) are inextricably interdependent. The ways in which the app’s use is eventually hindered or facilitated in practice can only be fully understood with this interdependency in mind.
Mi1phy: therapist’s own initiative to adopt and use the app, gain ownership of it
The first factor on the micro-level involves physiotherapists’ own initiative to adopt and integrate the app into their practices and to suggest it to patients. We noted that to integrate it into their practice, physiotherapists must invest paid and non-paid time to get to know and work with the app in the first place.
Excerpt 28:
FKE: Was the introduction training on the app enough for you to adopt and use it?
PHY6: No, not at all. Afterward I did a lot of self-study at home and tried it out. I wrote a program for myself, for my wife. Just close people, to practice, to be able to make mistakes. (200609_FKE, p.1)
Furthermore, the physiotherapists’ initiative also includes their decision to suggest the app to patients, or not.
Excerpt 29:
PHY7 tells FKE that in the last consultation, she gave PAT32 some exercises in the form of paper notes, but today, she wants to ask him if he would like to have it digitally. She thought she would just try and bring herself to do it. (200311_FKE, p.7)
Finally, physiotherapists may or may not accept and adapt to the design and functioning of the app, embrace new strategies for handling it, and gain knowledge confidently for therapy interventions.
Excerpt 30:
PHY7: Now [after the COVID-19 restrictions ended], I am just much more confident in creating exercise programs and it takes less time. And it’s also cool to see when the patients have done the exercises. At the beginning I had no idea that such a statistic would emerge with all these bars, I did it so little. And suddenly you can look it up and see: Ah, they’re doing the exercises, the bar goes up. That’s great. (200609_FKE, p.5)
Overall, physiotherapists’ own initiative, as specified above, is key for facilitating adoption and use of the app: we observed that it allows them to enter an upward spiral of increased use, development of eHealth literacy, practices, and confidence in the app’s possibilities for supporting therapy.
Mi2phy: therapist’s eHealth literacy
The second factor on the micro-level concerns the ways physiotherapists mobilize and display their eHealth literacy and competences in handling the app. We observed that facilitating adoption and use of the app requires physiotherapists to have solid experience and know-how with digital tools in daily life and more specifically with the app in physiotherapy practice.
Excerpt 31:
PHY2 does not use the app frequently, openly telling PAT20 that she hasn’t worked with it very often (“I’m a bit old school”). Yet, when she introduces it to PAT20, she explains its functions and its use clearly and confidently without displaying markers of hesitation. (200306_ ASC, p. 3)
Also, physiotherapists with an interest in digital tools and the willingness to build their own digital health literacy are more likely to use the app.
Excerpt 32:
During the introduction to the app, PHY7 and PHY10 are overwhelmed by the amount of information provided by the app:
PHY6: In the information, there is a lot that makes sense and a lot that doesn’t, so it’s best to have a look at it first. (200128_introduction app_ASC, p.3)
Confidence in one’s own digital health literacy and an ability to enable patients to use it too is a further facilitator for usage of the app.
Excerpt 33:
PHY9: Do you have your cell phone with you?
PAT35: My cell phone? It’s in the dressing room. Why?!
PHY9: Can you get it to download the app for the exercises?
PAT35 ((rolls his eyes slightly)): I don’t really want to download anything ((makes his way to the changing room to get the cell phone and comes back)).
PHY9: You know, it has really good stuff. For example, you can fill out an assessment questionnaire electronically. We can both still learn something at our age.
Later while having some trouble using the app:
PAT35: I thought the program was good?!
PHY9: Yes, but I also said that I am still learning. But just, you do it in this V position. Because it looks like a V. I’ll write it down for you in the comment box, ok? (200311_FKE, p.12–13)
As our illustrations above show, for physiotherapists, having eHealth literacy is not enough to adopt and use the app in practice. Moreover, they have to mobilize and display their literacy confidently to make up for certain limitations of the app, and more importantly, to motivate and enable patients, who might be reluctant to use it and/or lack the necessary digital competence (see Mi2pat below) to do so.
Mi3phy: therapist’s understanding of the app’s benefits, identification with app
The third factor on the micro-level concerns a physiotherapist’s stance toward the app in general, and its usefulness for therapeutic intervention and its consistency with physiotherapists’ understanding of professional identity and practices more particularly. We noticed that the physiotherapists who were more inclined to use the app considered it to enhance physiotherapy practice and promote patients’ involvement in improving their health.
Excerpt 34:
PHY10: What I like about the app is that everything is compact and in the same place. I don’t have a paper note here and another one there and no overview [about which information is filed where]. (200128_introduction app_ASC, p.4)
Excerpt 35:
Before PAT14 enters the consultation room, PHY12 explains that PAT14 tore their cruciate ligament and that physiotherapy is mainly about building muscles/strength. He remarks that the app is especially convenient for this therapeutic goal. (200303_SKE, p.1)
Furthermore, perceiving the app as a helpful substitution for existing (i.e. analogue) alternatives and understanding it as a valuable and powerful tool for supporting patients’ home exercise programs, beyond face-to-face consultations, facilitated its use.
Excerpt 36:
PHY1: I think with the app the patients actually do the home exercise more accurately because they have the videos. Before the app, we worked with sketches and they are not always so clear. (200211_ ASC, p. 9)
Finally, physiotherapists were more willing to work with the app if they saw it as promulgating a correct and adequate image of physiotherapy, one with which they can identify.
Our observations show that a physiotherapist’s understanding of the app’s benefits varies across different types of situations and activities, favoring its use in some situations or activities, but not in others. This factor Mi3phy thus has manifold implications for adoption and use of the app. Moreover, different physiotherapists might have conflicting understandings of the app’s benefits and adequacy with professional identity and practices. This raises important questions regarding the organization and level of participation of the app’s design development (see Me2 above). Finally, our observations also stress the interdependency between physiotherapists’ understanding of the app’s benefits and their perception of patients’ expectations.
Mi4phy: therapist’s perception of patient’s expectations and digital literacy
The fourth micro-level factor has to do with whether a physiotherapist considers the app beneficial for a specific patient. We observed that physiotherapists were more inclined to suggest the app to some patients but not to others. This might be related to a patient’s affiliation to a certain patient group and/or a specific type of treatment (see excerpt 35 in Mi3phy). Another aspect was physiotherapists’ appraisal of the patient’s assumed high level of digital literacy and affinity for digital tools, which was mainly linked to the patient’s age. While young people were considered to be interested in and used to digital tools, elderly people were perceived as having a more problematic attitude toward them.
Excerpt 37:
PHY3 asserts that generally, young people are getting along quite well with the app, there would be the opportunity to use it. For elderly people, there are often difficulties, for example, they register more than once and then can’t figure it out. The problems that come up for them while using the app have to be solved in the following therapy session. This takes a lot of time. (200211_SKE, p.2f.)
Physiotherapists also more often suggested the app to patients when they perceived that the app would be compatible with their perception of both physiotherapy and their own role in physiotherapy practice.
These different perceived patient characteristics were interwoven with each other, influencing physiotherapists’ decision to suggest the app or not. Age and digital literacy were made dependent on each other especially often.
Factors on the micro-level – physiotherapist: facilitators and barriers
Overall, our observations concerning the micro-level factors suggest that physiotherapists’ own initiative (Mi1phy), eHealth literacy (Mi2phy), their understanding of the app’s benefits (Mi3phy), and their perception of patients’ expectations and digital literacy (Mi4phy) are not the only key factors for facilitating physiotherapists’ adoption and use of the app. Since patients barely ever begin using the app on their own, physiotherapists’ initiative and display thereof are also decisive for its use. They thus fulfill an important gatekeeping role. The last section, on the micro-level factors concerning patients, will therefore be succinct.
Mi1pat: patient’s readiness to adopt/use the app
The first factor on the micro-level concerning the patient involves their openness to using the app as a digitalized extension of their treatment. We observed a relationship between patients’ readiness to use the app and several stances. First, if patients had a positive view of digitalization and were generally willing to use digital tools, they were also more inclined to use the app.
Excerpt 38:
PAT20 shows a vivid interest in the app, and is very positive about using it, when PHY2 suggests it to her. She tells ASC that she has a general interest in digital tools. She is the eldest of three sisters (between 60–70 years of age), but among them, she is the one who uses digital tools most often. As an example, she talks about an app used for traveling with public transport that would be most useful to her. (200306_ ASC , p.2)
In contrast:
Excerpt 39:
PHY7: asks if PAT32 is interested in using the app.
PAT32: declines the suggestion. He struggles with the over-digitalization of society and does not want to have an app. (200311_FKE, p.7)
Furthermore, patients were more willing to use the app if they trusted the app’s data protection and safety measures, or if these details were of neglectable relevance to them. Similarly, patients who perceived digital tools and the app in particular to be consistent with their personal goals and identity showed a great openness to using the app.
Our ethnographic fieldwork shows that the initiative to use the app came from the therapists. Patients did not know about its existence. However, patients’ positive stances to digital technology led them to accept and embrace the app, once their therapist suggested using it.
Mi2pat: patient’s digital competence
The second factor on the level of the individual patient concerns her or his digital competences in everyday life. We noted that in the first place, use of the app was enabled and facilitated by patients’ access to a digital device for personal use that is suited to the app’s user interface.
Excerpt 40:
PAT8 has a cell phone for making calls, but no smartphone. She mentions that she does not send text messages either, although this would technically be possible with her cell phone, because text messages are too small for her to read. (200211_ASC, p.10)
The use of the app was also facilitated when patients had solid digital literacy and experience with mobile applications, and, related to that frequently used digital tools in different daily activities and for different reasons,for professional or leisure time purposes and health-related or other uses.
Excerpt 41:
PAT24 says he uses many apps, especially for drawing, which is his hobby. An app for physiotherapy seems to be an exciting idea for him, especially if you can look up how an exercise has to be done. (200306_ASC, p.9)
We noticed that patients who had access to the necessary digital devices and considered themselves to be experienced in using digital tools often also display more ease, confidence, and motivation to use the app, which in turn makes it easier for the therapist to suggest and introduce the app to them.
Mi3pat: patient’s understanding of the app’s benefits
The third factor on the level of the individual patient concerns his or her understanding of the app as helpful for therapy or not. We noticed that an understanding of the app’s benefits was based for instance on patients’ appreciation of a specific function of the app as particularly motivating or helpful.
Excerpt 42:
PAT20 asks if the app has a daily reminder feature. PHY2 and ASC affirm that it does. PHY2 notices PAT20ʹs interest and thinks out loud that the app would indeed be a good option for PAT20: with the app, she could exercise even without regular physiotherapy consultations. (200306_ ASC, p.3)
Patients were also more open to the app if they considered its functions to be a valuable and more promising substitution for existing (analogue) alternatives.
See in contrast:
Excerpt 43:
PAT9: I do not use the app; I am able to remember the exercises myself. (200211_ ASC, p.12)
Finally, patients considered the app to be beneficial if they perceived its role for therapy and home exercise to be adequately defined and in line with their preferences and expectations (e.g. patients who did not feel comfortable exercising without supervision did not consider the app beneficial).
In our observations, the patients who responded very positively to the suggestion to use the app often saw a particular benefit for their treatment in it. If the app meets a particular need of a patient, he or she is more likely to agree to use it. The app then becomes a welcoming enrichment to physiotherapy.
Factors on the micro-level – patient: facilitators and barriers
In our ethnographic fieldwork, we spoke with physiotherapy patients, both users and non-users of the app. As stated earlier, the characteristics listed in factors Mi1-3pat did not lead to patients initiating the use of the app. However, when their therapist suggested that they use it, this made them more likely to agree. In the consultations in which therapists suggested working with the app, patients’ stances to digital tools and digitalization ranged from vivid interest to critical. In one case (see Mi1pat, excerpt 39), the patient refused to work with the app. Yet this seemed to be rather an exceptional case, for the physiotherapists reported that most patients agreed to use it once it was suggested to them. This may be linked to factor Mi4phy and the physiotherapists’ choice to suggest the app only to some patients.
Discussion
In line with other studies (Hennemann, Beutel, and Zwerenz, Citation2017), our ethnographic investigation in two outpatient clinics shows that the adoption of the app in physiotherapy remains low overall and that its potential is underexploited. Moreover, it goes beyond this assertion and puts things into perspective. Our findings regarding factors that facilitate or hinder mHealth tools’ adoption (Konttila et al., Citation2019) reveal that the impact of a single factor cannot be understood in isolation but needs to be looked at as one piece of a dynamic interplay.
Whether a factor functions as a facilitator or a barrier depends on its individual valence: a therapist’s high initiative (Mi1phy) and adaptation of his or her physiotherapy practice (Vestergaard, Citation2021), which is required to adopt, use, and introduce the app to the patient, functions as a crucial facilitator to the patient’s use of the app per se. However, the physiotherapist’s and the patient’s use of the app are contingent upon the interdependent workings of the other factors on a macro-, meso-, and micro-level. The impact of a single factor thus needs to be understood within a network of: 1) horizontal; and 2) vertical influences.
For example, on the horizontal level, a therapist’s high initiative (Mi1phy) to adopt the app and introduce it to the patient engenders on the one hand his or her regular or even systematic use of the app in therapy. This contributes to his or her acquisition and development of digital health literacy (Mi2phy) and his or her competence to enable others to use it in turn (Bird et al., Citation2020). On the other hand, high digital health literacy (Mi2phy) facilitates a physiotherapist’s adoption of the app and increases his or her initiative to introduce it to patients.
On the vertical level, effective reimbursement models (Ma1) for mHealth solutions in physiotherapy on the macro-level on the one hand facilitate the implementation of transparent funding regulations on the institutional level (Me4 and Me5) and act as an incentive for therapist’s own initiative to adopt the app (Mi1phy). On the other hand, large institutions’ initiative to define a reimbursement policy for the use of digital tools in physiotherapy (Me4 and Me5) may exert pressure on national physiotherapy federations to seek a solution on the Swiss healthcare system level.
Moreover, our study shows that in Switzerland an absence of incentives for adopting and using mHealth solutions, in our case the app, on the macro-level and an open policy on the meso-level involves a high degree of freedom and responsibility on the micro-level (i.e. decisions about when, how, and for what purposes to adopt and use the app in therapy depend on individuals in the interactional physiotherapist–patient realm). If a physiotherapist sees a benefit in using the app (Mi3phy), is competent to do so (Mi2phy), perceives patients to be in a position to use it (Mi4phy) and takes the initiative to adopt, use, and suggest it to the patient (Mi1phy), this might eventually lead to the patient’s adoption of the app, if he or she perceives a benefit in using it (Mi3pat), is ready to engage with it (Mi1pat) and has the necessary digital literacy to do so (Mi2pat).
How these interdependencies between the factors on the micro-, meso- and macro-level interact and eventually impact the use and adoption of the app in physiotherapy requires further research. During and after the COVID-19 restrictions, we observed an increase in the use of the app. We suggest that adaptations to the particular context on the macro-level (Ma1 and Ma3) and meso-level (Me4-6) and physiotherapists’ own initiative (Mi1phy) proved particularly relevant for this increase (Keel, Keller, Schmid, and Schoeb, Citation2020). However, we also suggest that how the temporary increase during and shortly after the COVID-19 restrictions plays out over the long term is something in need of further research.
Lastly in line with studies conducted by Procter et al. (Citation2016) and Randall, Rouncefield, and Tolmie (Citation2020) we argue that further ethnographic research on end-users’ situated practices involving digital technology is required. Showing the ways eHealth tools and the app are used, handled, and oriented to by end-users in naturally occurring, situated physiotherapy practices and interactions does not increase only our understanding of healthcare professionals’ and patients’ use and adoption, or in our case low adoption, of the app and of factors hindering/facilitating the adoption. Quite the contrary, it also sheds new light on everyday circumstances, including practical, social, and technical contingencies, such as time constraints, reimbursement issues, or worries about data security or infrastructure, that end-users face in their situated physiotherapy practices. We thus suggest that further development and implementation of eHealth tools in healthcare/physiotherapy need to adopt more participative forms of research that involve end-users of eHealth tools and/or take their working and everyday life experiences into account.
Acknowledgments
This work was supported by the ‘Commission Scientifique du Domaine Santé’ of the University of Applied Sciences and Arts Western Switzerland (HES-SO), under Grant number: 95846/S-RAD19-04. We thank Medbase for the stimulating collaboration. And we are most grateful to all the participating physiotherapists for allowing us to access and follow their daily work and for taking precious time to answer all our questions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Albrecht UV, Afshar K, Illiger K, Becker S, Hartz T, Breil B, Wichelhaus D, von JU 2017 Expectancy, usage and acceptance by general practitioners and patients: Exploratory results from a study in the German outpatient sector. Digital Health 3: 1–22. 10.1177/2055207617695135
- Angerer A, Schmidt R, Moll C, Strunk L, and Brügger U 2017 Digital Health - Die Zukunft des Schweizer Gesundheitswesens. https://digitalcollection.zhaw.ch/bitstream/11475/1458/1/Digital%20Health%20Report_DC_2017_11_08.pdf. Accessed 27 April 2020
- Bennell KL, Nelligan R, Dobson F, Rini C, Keefe F, Kasza J, French S, Bryant C, Dalwood A, Abbott JH 2017 Effectiveness of an internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain: A randomized trial. Annals of Internal Medicine 1667: 453–462. 10.7326/M16-1714
- Bird ML, Elmer S, Osborne RH, Flittner A, O’Brien J 2020 Training physiotherapists to be responsive to their clients’ health literacy needs. Physiotherapy Theory and Practice Online ahead of print: 1–9. 10.1080/09593985.2020.1850956
- Blixt L, Solbraekke KN, Bjorbaekmo WS 2021 Physiotherapists’ experiences of adopting an eTool in clinical practice: A post-phenomenological investigation. Physiotherapy Theory and Practice 379: 1005–1017. 10.1080/09593985.2019.1681042
- Blumenthal J, Wilkinson A, Chignell M 2018 Physiotherapists’ and physiotherapy students’ perspectives on the use of mobile or wearable technology in their practice. Physiotherapy Canada 70: 251–261. 10.3138/ptc.2016-100.e
- Button K, Nicholas K, Busse M, Collins M, Spasic I 2018 Integrating self-management support for knee injuries into routine clinical practice: TRAK intervention design and delivery. Musculoskeletal Science and Practice 33: 53–60. 10.1016/j.msksp.2017.11.002
- Cai RA, Beste D, Chaplin H, Varakliotis S, Suffield L, Josephs F, Sen D, Wedderburn LR, Ioannou Y, Hailes S, et al. 2017 Developing and evaluating JIApp: Acceptability and usability of a smartphone app system to improve self-management in young people with juvenile idiopathic arthritis. JMIR Mhealth and Uhealth 58: e121. 10.2196/mhealth.7229
- Chan CV, Kaufman DR 2011 A framework for characterizing eHealth literacy demands and barriers. Journal of Medical Internet Research 134: e94. 10.2196/jmir.1750
- Corbetta D, Imeri F, Gatti R 2015 Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: A systematic review. Journal of Physiotherapy 613: 117–124. 10.1016/j.jphys.2015.05.017
- Cruz EV, Higginbottom G 2013 The use of focused ethnography in nursing research. Nurse Researcher 20: 36–43. 10.7748/nr2013.03.20.4.36.e305
- Danbjorg DB, Villadsen A, Gill E, Rothmann MJ, Clemensen J 2018 Usage of an Exercise app in the care for people with osteoarthritis: User-driven exploratory study. JMIR Mhealth and Uhealth 61: e11. 10.2196/mhealth.7734
- Dunphy E, Hamilton FL, Spasic I, Button K 2017 Acceptability of a digital health intervention alongside physiotherapy to support patients following anterior cruciate ligament re-construction. BMC Musculoskeletal Disorders 181: 471. 10.1186/s12891-017-1846-0
- eHealth Suisse 2017 Mobile Health (mHealth) Empfehlungen - Ausgangslage und erste Schritte [Mobile Health (mHealth). Recommendations: Starting Point and First Steps]. https://www.e-health-suisse.ch/fileadmin/user_upload/Dokumente/2017/D/170316_mHealth_Empfehlungen_I_d.pdf Accessed 15 April 2020
- Endl R, Jäschke T, Thiel C, and Wickinghoff DV 2015 mHealth im Kontext des elektronischen Patientendossiers - Eine Studie im Auftrag von eHealth Suisse [mHealth in the Context of the Electronic Patient Record - A Study Commissioned by eHealth Switzerland]. https://www.e-health-suisse.ch/fileadmin/user_upload/Dokumente/2015/D/150309_Bericht_FHSG_mHealth_D.pdf Accessed 16 March 2020.
- Gagnon MP, Ngangue P, Payne-Gagnon J, Desmartis M 2016 m-Health adoption by healthcare professionals: A systematic review. Journal of the American Medical Informatics Association 231: 212–220. 10.1093/jamia/ocv052
- Garfinkel H 1967 Studies in Ethnomethodology. Cambridge: Polity Press
- Hennemann S, Beutel ME, Zwerenz R 2017 Ready for eHealth? Health professionals’ acceptance and adoption of eHealth interventions in inpatient routine care. Journal of Health Communication 223: 274–284. 10.1080/10810730.2017.1284286
- Hilliard ME, Hahn A, Ridge AK, Eakin MN, Riekert KA 2014 User preferences and design recommendations for an mHealth app to promote cystic fibrosis self-management. JMIR Mhealth and Uhealth 24: e44. 10.2196/mhealth.3599
- Hinman RS, Nelligan RK, Bennell KL, Delany C 2017 “Sounds a bit crazy, but it was almost more personal” A qualitative study of patient and clinician experiences of physical therapist-prescribed exercise for knee osteoarthritis via Skype. Arthritis Care and Research 6912: 1834–1844. 10.1002/acr.23218
- Huber S, Priebe JA, Baumann KM, Plidschun A, Schiessl C, Tolle TR 2017 Treatment of low back pain with a digital multidisciplinary pain treatment app: Short-term results. JMIR Rehabilitation and Assistive Technologies 42: e11. 10.2196/rehab.9032
- Keel S, Keller F, Schmid A, Schoeb V 2020. The use of digital tools within physiotherapy: COVID-19 impact on facilitators and barriers. Paper presented at: International Conference on Communication in Healthcare; Online Conference.
- Konttila J, Siira H, Kyngas H, Lahtinen M, Elo S, Kaariainen M, Kaakinen P, Oikarinen A, Yamakawa M, Fukui S, et al. 2019 Healthcare professionals’ competence in digitalisation: A systematic review. Journal of Clinical Nursing 285–6: 745–761. 10.1111/jocn.14710
- Lambert TE, Harvey LA, Avdalis C, Chen LW, Jeyalingam S, Pratt CA, Tatum HJ, Bowden JL, Lucas BR 2017 An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: A randomised trial. Journal of Physiotherapy 633: 161–167. 10.1016/j.jphys.2017.05.015
- Lawford BJ, Delany C, Bennell KL, Hinman RS 2018 “I was really sceptical … but it worked really well”: A qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis Cartilage 26: 741–750.
- Luff P, Hindmarsh J, Heath C 2000 In: Luff P, Hindmarsh J, Heath C Eds Introduction, Workplace studies recovering work practice and informing system design, 1–26. Cambridge: Cambridge University Press
- Matusiewicz D, and Thielscher C 2017 In: Matusiewicz D, Pittelklau C, and Elmer A Eds Electronic health (E-Health) und mobile health (mHealth) – ein Definitionsversuch [an attempt at definition], Die digitale Transformation im Gesundheitswesen [the digital transformation in healthcare], 3–7. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft.
- Medbase 2019a Auswertung Umfrage Herbst 2018: Physitrack/physio.coach.
- Medbase 2019b PROM Umfrage - Feedback zur Nutzung von Fragebogen.
- Medbase 2019c Physitrack and Medbase physio.coach - Internal Information on Functionalities of PhysitrackTM and physio.coach Applications.
- Morris J, Jones M, Thompson N, Wallace T, DeRuyter F 2019 Clinician perspectives on mRehab interventions and technologies for people with disabilities in the United States: A national survey. International Journal of Environmental Research and Public Health 1621: 4220. 10.3390/ijerph16214220
- Mulhall A 2003 In the field: notes on observation in qualitative research. Journal of Advanced Nursing 413: 306–313. 10.1046/j.1365-2648.2003.02514.x
- Nicholl B, Sandal L, Stochkendahl MJ, McCallum M, Suresh N, Vasseljen O, Hartvigsen J, Mork P, Kjaer P, Sogaard K, et al. 2017 Digital support interventions for the self-management of low back pain: A systematic review. Journal of Medical Internet Research 195: e179. 10.2196/jmir.7290
- Norman CD, Skinner HA 2006 e-Health literacy: essential skills for consumer health in a networked world. Journal of Medical Internet Research 82: e9. 10.2196/jmir.8.2.e9
- O’Malley G, Dowdall G, Burls A, Perry IJ, Curran N 2014 Exploring the usability of a mobile app for adolescent obesity management. JMIR Mhealth and Uhealth 22: e29. 10.2196/mhealth.3262
- Physioswiss 2017 Digitale Welt, le monde digital, il mondo digitale [digital world]. Physioactive 05.
- Pink S, Morgan J 2013 Short-term ethnography: Intense routes to knowing. Symbolic Interaction 363: 351–361. 10.1002/symb.66
- Pollner M, Emerson R 2001 In: Atkinson P, Coffey A, Delamont S, Lofland J, Lofland L Eds Ethnomethodology and ethnography, Handbook of Ethnography, 118–135. Los Angeles: Sage Publications
- Postolache GB, Oliveira R, Postolache O 2017 Contextual design of ICT for physiotherapy: toward knowledge and innovation ecosystem. EAI Endorsed Transactions on Creative Technologies 413: e3. 10.4108/eai.8-11-2017.153334
- Procter R, Wherton J, Greenhalgh T, Sugarhood P, Rouncefield M, Hinder S 2016 Telecare call centre work and ageing in place. Computer Supported Cooperative Work 251: 79–105. 10.1007/s10606-015-9242-5
- Randall D, Rouncefield M, Tolmie P 2020 Ethnography, CSCW and ethnomethodology. Computer Supported Cooperative Work 30: 189–214. 10.1007/s10606-020-09388-8
- Rausch AK, Baur H, Reicherzer L, Wirz M, Keller F, Opsommer E, Schoeb V, Vercelli S, Barbero M 2021 Physiotherapists’ use and perceptions of digital remote physiotherapy during COVID-19 lockdown in Switzerland: an online cross-sectional survey. Archives of Physiotherapy 111: 18. 10.1186/s40945-021-00112-3
- Revenas A, Opava CH, Martin C, Demmelmaier I, Keller C, Asenlof P 2015 Development of a web-based and mobile app to support physical activity in individuals with rheumatoid arthritis: Results from the second step of a co-design process. JMIR Research Protocols 41: e22. 10.2196/resprot.3795
- Schäublin J 2018 Wie beurteilen Schweizer Physiotherapeuten und Physiotherapeutinnen die Physiotherapie 2.0 und den Patient 3.0 in der Praxis [how do Swiss physiotherapists assess patients in practice]. Master thesis. Bern University of Applied Sciences.
- Schoeb V, Hiller A 2018 The impact of documentation on communication during patient-physiotherapist interactions: A qualitative observational study. Physiotherapy Theory and Practice 3411: 861–871. 10.1080/09593985.2018.1429036
- Smittenaar P, Erhart-Hledik JC, Kinsella R, Hunter S, Mecklenburg G, Perez D 2017 Translating comprehensive conservative care for chronic knee pain into a digital care pathway: 12-week and 6-month outcomes for the hinge health program. JMIR Rehabilitation and Assistive Technologies 41: e4. 10.2196/rehab.7258
- Spasic I, Button K, Divoli A, Gupta S, Pataky T, Pizzocaro D, Preece A, van Deursen R, Wilson C 2015 TRAK app suite: A web-based intervention for delivering standard care for the rehabilitation of knee conditions. JMIR Research Protocoles 44: e122. 10.2196/resprot.4091
- Vestergaard K 2021 Changes in professionalism through the practice of telemedicine: conceptualizing a situated sense filter. Professions and Professionalism 11: e3857.
- vom Lehn D 2019 Phenomenology-based ethnography for management studies and organizational analysis. British Journal of Management 30: 188–202.
- Vorrink SN, Kort HS, Troosters T, and Lammers JW 2016 A mobile phone app to stimulate daily physical activity in patients with chronic obstructive pulmonary disease: development, feasibility, and pilot studies. JMIR Mhealth and Uhealth 41: e11. 10.2196/mhealth.4741
- Wentink MM, Siemonsma PC, van Bodegom-vos L, de Kloet AJ, Verhoef J, Vlieland T, and Meesters JJ 2019 Teachers’ and students’ perceptions on barriers and facilitators for eHealth education in the curriculum of functional exercise and physical therapy: A focus groups study. BMC Medical Education 191: 343.