ABSTRACT
Background
Hippotherapy (HPOT) is a physical therapy (PT) treatment tool using equine movement to improve mobility for children with movement impairments. Although research suggests HPOT improves body structure and function, there is limited evidence regarding its impact on activity and participation outcomes in a clinical setting. The Pediatric Evaluation of Disability Inventory Computer Adaptive Test (PEDI-CAT) may be useful in HPOT settings to highlight changes in activity and participation.
Purpose
1) Evaluate the PEDI-CAT’s sensitivity to changes in activity and participation among children receiving PT using HPOT; 2) determine feasibility of administering the PEDI-CAT in a HPOT setting; and 3) examine how PEDI-CAT scores influence clinical decision-making.
Methods
Participants (N = 34) were children who attended weekly PT using HPOT for 6 months. The PEDI-CAT was completed for all participants by a parent or caregiver at initial treatment (T1) and 6 months later (T2). A linear mixed effects model was used to evaluate changes in scores over time. Team meetings occurred monthly to discuss how PEDI-CAT scores impacted treatment.
Results
There were significant improvements across 3 PEDI-CAT domains between T1 and T2 for all children with small effect sizes and nonsignificant changes noted within two diagnostic subgroups with small-to-medium effect sizes. The PEDI-CAT was completed by all participants without interrupting treatment flow. PEDI-CAT score reports enriched therapist-client conversations increasing shared decision-making.
Conclusion
PTs who treat children using HPOT may feasibly use the PEDI-CAT to assess changes in activity level outcomes and to assist clinical decision-making.
Introduction
Strategically using horses’ movement in a rehabilitation setting can provide a critical combination of physical challenge and motivation to promote improved mobility in children with motor limitations. Hippotherapy (HPOT) refers to how physical therapy (PT), occupational therapy, and speech-language pathology professionals use the purposeful manipulation of equine (horse) movement as a therapy tool to engage sensory, neuromotor, and cognitive systems to promote functional outcomes (American Hippotherapy Association, Citation2019). Though much of HPOT treatment encourages rhythmic motor activation, there is also reason to expect it may improve children’s abilities to participate in typical daily activities (Hsieh et al., Citation2017). Activity (i.e. the execution of a task or action) and participation (i.e. involvement in a life situation) (World Health Organization, Citation2007) are key outcomes for children with functional movement impairments. Current conceptual frameworks such as: the International Classification of Functioning, Disability, and Health [ICF] (Chan et al., Citation2009; World Health Organization, Citation2007); Guide to Physical Therapy Practice (American Physical Therapy Association, Citation2014); as well as national policies (e.g. Individuals with Disabilities Education Act, Americans with Disabilities Act) encourage physical therapists to focus on improvements in activity and participation (Goldstein, Cohn, and Coster, Citation2004).
Despite calls to focus on activity and participation research investigating HPOT commonly focuses on improvements in body structure, body function, and gait characteristics (Kwon et al., Citation2015; Zadnikar and Kastrin, Citation2011). HPOT is theorized to promote balance and ambulation by utilizing the three-dimensional, reciprocal movement of horses’ gait, which imparts pelvic movements to the child. These movements stimulate active postural control throughout the head, arms, and trunk that resemble the controlled movements required during independent ambulation (Koca and Ataseven, Citation2015). During a single treatment session, clients can experience upwards of 3000 repetitive balance challenges, making HPOT a consistent and repetitive treatment tool (Thompson, Ketcham, and Hall, Citation2014). Studies have documented improvements in: adductor muscle symmetry (McGibbon, Benda, Duncan, and Silkwood-Sherer, Citation2009); gait mechanics (McGee and Reese, Citation2009); sitting balance (Kang, Jung, and Yu, Citation2012); and postural control (Champagne and Dugas, Citation2010) following HPOT interventions. A systematic review of interventions for cerebral palsy concluded HPOT was highly effective for improving balance and symmetry, but weaker results were reported for improving self-care and function (Novak et al., Citation2020). This review highlighted a need for more evidence demonstrating activity and participation improvements following HPOT.
The Pediatric Evaluation of Disability Inventory Computer Adaptive Test (PEDI-CAT) is used to measure activity and participation outcomes (Thompson, Cech, Cahill, and Krzak, Citation2018) in children age 0–20 with a variety of diagnoses. It is used to evaluate children’s performance across 4 different domains: 1) Mobility (e.g. ambulation); 2) Daily Activities (e.g. dressing); 3) Social Cognitive (e.g. interaction); and 4) Responsibility (e.g. staying safe). The breadth of the PEDI-CAT domains suggests it is viable for assessing activity and participation outcomes of clients with many diagnoses and varying needs. For instance, cerebral palsy frequently presents with motor control challenges (Sadowska, Sarecka-Hujar, and Kopyta, Citation2020) whereas individuals with autism may exhibit greater difficulties in socio-emotional domains (Maenner et al., Citation2020) both of which are assessed in different PEDI-CAT domains. Researchers have used the PEDI-CAT to assess activity and participation for children who are: typically developing (Dumas et al., Citation2012); with cerebral palsy (Shore et al., Citation2019); with autism spectrum disorder and intellectual developmental disabilities (Kao et al., Citation2012); with spinal muscular atrophy (Pasternak et al., Citation2016); and with a wide variety of diagnoses encountered in a pediatric hospital (Dumas et al., Citation2015).
Practice-based research or translational research is a critical component of improving clinical practice, as there is the potential for a gap between the structured research environment and the challenges associated with clinical settings (Westfall, Mold, and Fagnan, Citation2007). A considerable amount of HPOT research is conducted in controlled environments among homogenous populations with a specific diagnosis such as: cerebral palsy (McGee and Reese, Citation2009; McGibbon, Benda, Duncan, and Silkwood-Sherer, Citation2009); multiple sclerosis (Gencheva, Ivanova, and Stefanova, Citation2015; Menezes et al., Citation2013); and autism (Ajzenman, Standeven, and Shurtleff, Citation2013; Srinivasan, Cavagnino, and Bhat, Citation2018). However, pediatric clinical settings often serve clients who have more varied diagnoses, or even more than one diagnosis. In addition, research studies of HPOT tend to investigate shorter intervention periods between 5 and 12 weeks (Cabiddu et al., Citation2016; Homem and Oliveira, Citation2015; Kim and Lee, Citation2014; Lindroth, Sullivan, and Silkwood-Sherer, Citation2015; Lucena-Antón, Rosety-Rodríguez, and Moral-Munoz, Citation2018; Rigby et al., Citation2017); whereas clinic-based PT interventions in research settings may last up to 40 weeks (Academy of Pediatric Physical Therapy, Citation2012), and PT using HPOT commonly serves children with lifelong disabilities (Maresca et al., Citation2020; Wood and Fields, Citation2021). Therefore, it is necessary to examine changes in activity and participation outcomes with a validated assessment tool in the clinical environment and over a longer period to best reflect the effectiveness of PT treatment using HPOT and assist PT decision-making. The purpose of this study is to: 1) evaluate the PEDI-CAT’s sensitivity to changes in activity and participation among children receiving PT using HPOT; 2) evaluate the feasibility of PEDI-CAT use in a clinical environment that provides PT using HPOT; and 3) examine if PTs find PEDI-CAT scores useful when making clinical decisions. We hypothesized that the PEDI-CAT will be sensitive to changes in activity and participation outcomes across 6 months among a diverse client population receiving HPOT. It is further hypothesized that participants with cerebral palsy and autism will exhibit different amounts of change across PEDI-CAT domains. It is also hypothesized the PEDI-CAT will be feasibly incorporated into treatment, such that parents will consistently complete the PEDI-CAT during 1 treatment session without therapist assistance. Finally, PEDI-CAT scores are likely to aid clinical decision-making and stimulate collaboration between parent and clinician.
Methods
Data used in this study were collected by clinicians prior to creation of a formal study protocol, as data collection initially began as an effort by PT’s to systematically evaluate the effectiveness of their treatments. In pursuit of these aims, the clinicians began implementing the PEDI-CAT assessment with all pediatric PT clients, regardless of age or diagnosis, to assess best practices within a clinic that uses HPOT. This retrospective study was approved by Chapman University International Review Board, FWA# 00011020.
Participants
Data were collected from parents or caregivers of children (N = 34) receiving HPOT treatment at a multidisciplinary therapy center from October 2015 to April 2018. Parents or caregivers that completed the PEDI-CAT were all female and all fluent in English as their primary language. Thirty-three were mothers of participants and 1 was a fulltime caregiver who was the primary caretaker. See for a description of participants including age, gender, diagnoses, and attendance rate. Children were included in this translational application if they: 1) were between 18 months-21 years; 2) new or ongoing clients to PT using HPOT; 3) had a documented functional movement impairment; and 4) were deemed able and safe to participate in HPOT treatment by therapists. Children were excluded if they: 1) had excessive therapy absences (i.e. absent ≥ 35% of treatments); 2) had uncontrolled seizures; or 3) discontinued therapy treatment within 6 months.
Table 1. Descriptive statistics for child participants.
Measures
The PEDI-CAT was used to assess changes across four domains of activity- and participation-related outcomes. The measure has been found to have sound psychometric properties with: high test-retest reliability (Dumas et al., Citation2012); established content validity (Dumas, Fragala-Pinkham, Rosen, and Ni, Citation2021; Haley et al., Citation2012); and was responsive to change over time for children discharged from a pediatric rehabilitation hospital (Fragala-Pinkham, Dumas, Lombard, and O’Brien, Citation2016) and for children with CP (Kenyon et al., Citation2016). Scaled scores were examined in this study as they are most useful for tracking within-person change over time (Haley et al., Citation2012). Higher scores on the PEDI-CAT’s 20–80 scale are indicative of greater functional ability. Two versions of the PEDI-CAT were attempted in this study: 1) content-balanced; and 2) speedy. The content-balanced version displays approximately 30 items relevant to each domain (120 items total), whereas the speedy version displays up to 15 items relevant to each domain (< 60 items). Responses between the 2 versions tend to be highly correlated (Haley et al., Citation2012). Both the speedy and content-balanced versions of the PEDI-CAT are adaptive in that respondents see a minimum number of relevant items in each domain, but items displayed vary depending on prior responses, based on Item Response Theory modeling (Dumas, Fragala-Pinkham, Rosen, and Ni, Citation2021). The PEDI-CAT autism spectrum disorders module was not used in this study.
Feasibility data were collected by the PTs who administered the PEDI-CAT. Each PT noted: 1) if parents or caregivers completed the assessment within a single 45-min treatment session; 2) if the parent or caregiver encountered difficulties with iPad navigation; 3) if the parent or caregiver was or was not willing to participate in PEDI-CAT assessment; and 4) if the assessment interrupted PT intervention. PTs reported their feasibility data findings at monthly team meetings. In addition to feasibility evaluated by each PT, the primary investigator kept record of overall costs which included: 1) cost of the iPad; 2) PEDI-CAT application fee; and 3) cost of training time for each therapist. All these factors were indicators of PEDI-CAT feasibility.
A translational team was assembled to evaluate the clinical application of the PEDI-CAT. Team members included five PTs, 1 PT assistant, 1 administrator, 1 statistician/psychologist, and 1 translational researcher/PT. The team collaborated via formal, once-per-month team meetings with notes taken by the translational researcher/PT. The primary investigator crafted and then proposed questions to the PTs regarding their use of the PEDI-CAT, both in these meetings and via e-mail after data collection (Appendix).
Procedure
Before the study began, therapists had varying levels of experience using the PEDI-CAT from none to a great deal. An in-person training session was provided by the primary investigator for each therapist on use of the PEDI-CAT App, interpretation of scores, and navigation of the iPad. Therapists demonstrated proficiency in all areas listed above by providing a practice test to the primary investigator who assessed individual performance. On-going support was provided by the trainer throughout the data collection.
Parents or caregivers completed an initial PEDI-CAT assessment, via iPad PEDI-CAT application, for their child at initial treatment (T1). Parents or caregivers completed a second PEDI-CAT assessment following 6 months of PT treatment (T2). The same parent or caregiver who completed the assessment at T1 also completed the assessment at T2 for each child. Respondents were directed to fill out the PEDI-CAT assessment while their child participated in PT. They were encouraged to respond as accurately as possible with the child’s most recent performance of activities in mind for each question. All data used in this study were collected using the speedy version of the PEDI-CAT.
After T1 data collection, children participated in 6 months of weekly PT using HPOT. Children were not restricted from participating in other therapies and activities outside of PT. Intervention protocol was semi-structured and included a minimum of 30 minutes astride the horse. Treating therapists included five PTs and 1 PTA with a range of experience from 2 to 20 years using HPOT. Treatment was tailored to participants’ needs by selecting horses with varying movement qualities as well as individualized equipment. While astride the horse, participants engaged in developmentally challenging games and activities to work toward functional goals. Following 30 minutes on the horse, participants performed various ground- and clinic-based activities to further practice skills they worked on while astride the horse for a total treatment time of 45 minutes. This protocol could be considered usual care.
Therapists who provided PT using HPOT and who administered the PEDI-CAT were directed to discuss results of the PEDI-CAT with participants’ parent or caregiver via printed or on-screen score reports including lists of individual item responses, item maps, scaled scores, and percentile ranks within each domain. Therapists explained the meaning of scores at T1 and T2, as well as any changes in scores between T1 and T2, to each parent or caregiver. PTs reported about how discussions with parents or caregivers influenced clinical decision-making at the monthly team meetings.
Data analysis
Data were analyzed using “The R Project” statistical software version 3.5.3 (https://www.r-project.org/). A linear mixed effects model was used to assess if changes in scaled scores were significant in each functional domain (i.e. Mobility, Daily Activities, Social Cognitive, and Responsibility). Use of the linear mixed effects model allowed analysis of both fixed (i.e. time) and random (i.e. variability of initial scores) variables entered into subsequent linear equations in a stepwise manner. The first model eliminated variability due to heterogeneity of individual participants scores and was used to compare with subsequent linear models. The second model eliminated variability due to age of the participant. Subsequent predictors were added one at a time to determine if the addition of a predictor statistically improved the subsequent model. The scaled scores in each functional domain were used as dependent variables. Independent variables added to the model following the initial two models accounted for: assessment time (T1 and T2); number of treatments; the therapy status (i.e. whether they were a new, ongoing, or returning client); and the interaction of age and assessment. Cohen´s d effect sizes were calculated and adjusted for a sample size of < 50 and were used to examine the magnitude of differences (Durlak, Citation2009). A Bonferroni correction was used to control for type I error due to four significance tests with α = 0.05 divided by 4 analyses with a p-value of ≤ 0.0125 considered significant. The final linear mixed effects model utilized for this analysis was: Yij = β0+ β1*agei + β2*assessmentij + β3*treatmentsi + β4*statusi + β5*ageix assessmentij + bi + ɛij.
where Yij represents the PEDI-CAT domain standard score for ith individual for the jth assessment, with bi as the random effect for individual i; agei refers to the age at T1 for individual i, assessmentij indicates which assessment (j) being either T1 and T2 approximately 6 months later for the ith individual; treatments is the number of treatments the child had between T1 and T2, status refers to whether they were an ongoing, returning, or new client at the time of T1, and ageix assessmentij is the interaction of the child’s initial age and the assessment. The general intercept is represented by β0; and β1-5 represent the coefficients for the different variables and ɛij is the error term. Models were built with the variables using the “lmer” function in the “lme4” package (Bates, Mächler, Bolker, and Walker, Citation2015). Subsequent linear models were compared using a likelihood ratio test. See for specific models, which reached significance. We excluded Responsibility domain data for participants younger than 3 years of age (n = 11), in line with recommendations from the PEDI-CAT administration manual (Haley et al., Citation2012). Linear mixed effect models were not calculated for the subset with cerebral palsy (n = 10) or the subset with autism (n = 9) secondary to the small number of participants, therefore, mean differences and effect sizes of these differences were calculated and reported.
Table 2. Significant results of likelihood ratios for linear mixed effects models.
Feasibility measures were comprised of count data and costs by analyzing monthly team meeting notes and reviewing receipts. The count data included: 1) number of parents or caregivers who were able to complete the PEDI-CAT within one 45-min session; 2) number who encountered device issues; 3) number who were willing to participate; and 4) time therapists spent during treatment to administer the PEDI-CAT. Cost data were tallied and included: 1) cost of iPad; 2) PEDI-CAT application fee; and 3) cost of therapist training. An aggregate of these data was then calculated to represent overall cost of PEDI-CAT implementation.
Answers to open-ended questions regarding the impact of PEDI-CAT scores on clinical decision-making from team meeting notes and e-mail survey questions were coded and analyzed by one investigator. Concepts in the data were recorded as themes if they were mentioned by more than 50% of PTs. Proposed themes were then presented to the research team to engage in consensus building. Themes were only reported if there was unanimous consensus among all team members. This was done to best represent the multitude of backgrounds and experiences that are representative of a typical pediatric PT clinic.
Results
PEDI-CAT sensitivity to change
When examining the results of the linear mixed effects models, initial age and time were the only variables that improved subsequent models. χ2-values and p-values for model improvement (i.e. age and time only) are reported in . The addition of initial age improved the model for all domains except Mobility. The addition of time improved the model for all domains except Responsibility.
Small effect size improvements were observed for three domains, which demonstrated significance over time (i.e. Mobility, Social Cognitive, and Daily Activities). Mean changes, effect sizes with 95% confidence intervals are presented in . The two largest diagnostic subset groups within the sample, autism, and cerebral palsy, showed greatest improvements from T1 to T2 in different domains. The autism subgroup improved the most in the Daily Activities domain with a medium effect size, whereas the cerebral palsy subgroup improved the most in the Social Cognitive domain with a small effect size. Violin plots () reflect the distribution of the scores within each PEDI-CAT domain. These plots provide visual comparison of the changes observed within the sample and subgroups between T1 and T2. The violin plots generally shifted upward from T1 to T2, either as an entire figure or due to upward mobility of individual scores within the plot affecting the width of the plot. These figures also show that participants were unlikely to experience floor or ceiling effects, as no scores were plotted at 20 or 80 representing the end ranges of the PEDI-CAT scaled scores. There was a possible ceiling effect observed for the Autism subgroup in the mobility domain with 3 out of 9 (33%) participant scores gathered at the highest point value at T2, though this effect should be observed cautiously due to the small sample size of the subgroup.
Figure 1 a. The violin plots above depict the distribution of PEDI-CAT scaled scores for Mobility and Daily Activities domains for all participants (N = 34), cerebral palsy subset (n = 10), and autism subset (n = 9). Assessment 1 and 2 refer to T1 and T2. Solid circles represent group means, and open circles represent individuals’ scores. A wider violin corresponds to a greater density of scores.
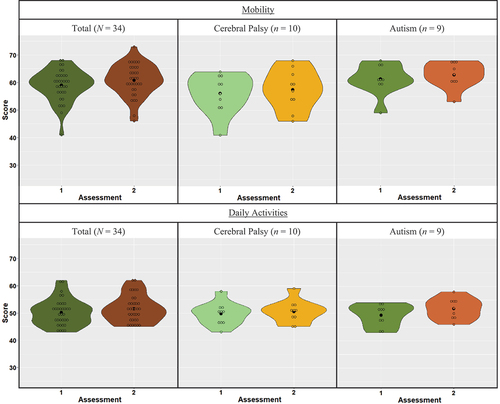
Figure 1 b. The violin plots above depict the distribution of PEDI-CAT scaled scores for the Social Cognitive domain for all participants (N = 34), cerebral palsy subset (n = 10), and autism subset (n = 9) and Responsibility domain for all participants 3 years of age or older (N = 23), cerebral palsy subset (n = 7), and autism subset (n = 6). Assessment 1 and 2 refer to T1 and T2. Solid circles represent group means, and open circles represent individuals’ scores. A wider violin corresponds to a greater density of scores.
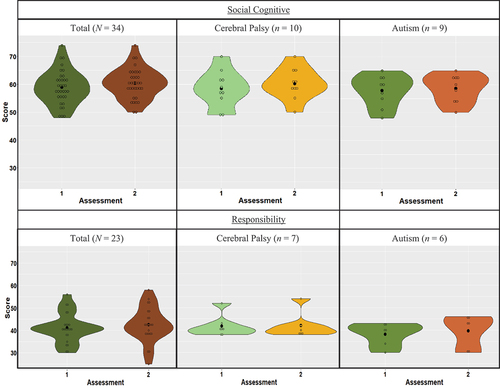
Table 3. PEDI-CAT scaled scores for time 1 and time 2.
Feasibility
Initially, parents or caregivers responded to the content-balanced version of the PEDI-CAT. The first seven parents or caregivers given the content-balanced version failed to complete the assessment during a single treatment session, resulting in incomplete data and, therefore, were not included in this study. These seven parents or caregivers then responded to the speedy version of the PEDI-CAT at their child’s next treatment session and completed the measure successfully. From that point forward, therapists administered the speedy version to ensure complete data were collected.
Analysis of feasibility data revealed that: 1) all parents and caregivers successfully completed the speedy version of the PEDI-CAT within a 45-min session at both T1 and T2; 2) there were no reports of issues with the electronic interface, indicating respondents were comfortable using the iPad; 3) all participants were willing to complete the PEDI-CAT; and 4) there was no interruption of treatment time for administration or scoring, as the PEDI-CAT program automatically scored responses upon completion and did not require any additional time or attention from PTs to complete. To purchase the software and hardware for one therapist was less than $4000. We had multiple therapists collecting data and there were changes that had to be made to technical, logistical, training, and reporting infrastructures of the therapy center’s operations to fully implement the program.
Clinical decision making
Clinicians unanimously agreed that information provided by PEDI-CAT assessments assisted with making clinical decisions and adjusting clients’ therapeutic plan of care. Several themes emerged from discussions in team meetings, including: 1) all PTs stated that reviewing the PEDI-CAT score reports with clients’ parents or caregivers enriched shared decision-making; 2) PEDI-CAT scores highlighted areas of need within specific domains, helping PTs write goals and tailor interventions to personalize their plan of care; and 3) PEDI-CAT scores provided PTs a unique parent-perspective regarding each child’s abilities that is not readily available via observational standardized assessments. One PT exemplified this saying: “The PEDI-CAT results were most useful at initial evaluation to help set goals and direct conversation with the parents regarding areas of need for PT treatment. Then when I had 2 assessments after 6 months of treatment, the PEDI-CAT scores were easy to compare across time and showed each child’s progress, as well as areas that continued to need improvement both between and within the various domains.”
Discussion
Our results support positive outcomes for all three of our aims. First, the PEDI-CAT was sensitive to improvements over 6 months among children with varied movement disorders. When we broke out and examined the two largest subset groups in our sample, autism, and cerebral palsy, we found differences in areas of improvement, which appear to fit common limitations in each diagnosis (Accardo, Citation2007; Maenner et al., Citation2020). Secondly, the PEDI-CAT was feasibly implemented with low costs and was easily completed without interrupting treatment flow. Finally, therapists found PEDI-CAT scores were useful for fostering conversation with participants’ families, leading to increased, shared decision-making.
The PEDI-CAT was found to be sensitive to changes in activity, but not participation, for pediatric clients utilizing HPOT as part of PT. The Daily Activities domain of the assessment has been found to be sensitive to changes over time in a longitudinal study of children with cerebral palsy (Burgess et al., Citation2020) and was examined for sensitivity in a setting using HPOT for children with Autism (Peters, Wood, Hepburn, and Moody, Citation2021). Burgess et al. (Citation2020) found that children with cerebral palsy demonstrated a range of estimated change in scaled score per year of 0.42 to 0.72 corresponding with our findings within the cerebral palsy subgroup who demonstrated a mean change of 0.8 over 6 months. Peters, Wood, Hepburn, and Moody (Citation2021) used the PEDI-CAT to assess changes in all 4 domains for 18 children who participated in occupational therapy using hippotherapy but did not find statistically significant improvements over time. Their data show similar small-to-medium effect size changes compared to our autism subgroup.
Our study represents one of the first attempts to evaluate the sensitivity of the PEDI-CAT to changes over time in a HPOT setting. Our results suggest the PEDI-CAT is able to detect objective changes in activity. The average changes detected for the entire sample in this study ranged between 1.3 and 1.8 points. It should be noted these changes had small effect sizes and may not exceed the minimal clinically important change value (MCID) needed to represent clinically significant change (Cook, Citation2008). More research is necessary to establish MCID for the PEDI-CAT in this setting. This sensitivity to changes in pediatric clients is important for two reasons. One, it provides objective activity and participation outcome data for a heterogeneous patient population. Two, the PEDI-CAT may be used to show progress over time for clients who participate in PT using HPOT. This information may be useful to convince insurance companies to value, recognize, and cover HPOT. Insurance coverage of PT using HPOT would have the added benefits of decreasing the financial burden of clients seeking PT using HPOT (Pham and Bitonte, Citation2016).
Improvements observed in different PEDI-CAT domains for the entire sample may be influenced by multiple factors including: bidirectional relationship of ICF levels; interrelationship between various facets of development; and the unknown impact of other activities and therapies participants may have been involved in during the study. The primary focus of PT using HPOT is to improve movement capabilities; therefore, it would be expected that the Mobility domain would increase over time for children receiving weekly PT. However, we found improvements in 3 out of 4 domains (i.e. Mobility, Daily Activities, and Social/Cognitive). These results may point to a positive cascade effect (Gonzalez, Alvarez, and Nelson, Citation2019; Iverson, Citation2010); that is as Mobility increases so does the ability to perform daily activities or social/cognitive tasks. This is in line with other research that shows improved mobility is positively correlated with higher levels of daily functional skills (Kwon et al., Citation2013) and cognitive skills (Muentener, Herrig, and Schulz, Citation2018). For example, as children improve mobility skills like independently walking with a walker rather than self-propelling a wheelchair they can then talk with peers eye to eye (Social/Cognitive), or when they gain the ability to sit upright independently they can then put on a shirt (Daily Activity).
Responsibility scores did not significantly change across time. Responsibility domain activities (e.g. keeping track of time and following a recipe) are seldomly addressed in PT and may be more closely linked to how involved the parent or caregiver is in helping the child. The Responsibility domain of the PEDI-CAT is not recommended for children younger than 3 years of age (Haley et al., Citation2012). Eleven participants were younger than 3 years at T1 and were excluded from the analysis, which may partially explain why we did not find a significant change in Responsibility scores over time for the sample. Another possible explanation may be found in the differences of abilities between diagnostic groups within our sample. While the autism subgroup participants who were older than 3 (n = 7) showed a mean change of 1.5, the CP subgroup participants who were older than 3 (n = 6) had their lowest change in this category with a mean change of only 0.3.
Two important demographic factors appeared to play a role in PEDI-CAT outcomes across the different domains. For one, with age, children gain motor and social/cognitive skills and begin to take more responsibility. This was partially true of our sample, except initial age was not correlated with the Mobility domain. This is likely because PT focuses on treating mild to severe movement impairments across all ages, which may attenuate an age-impairment relationship. Additionally, varying diagnoses pose unique developmental challenges affecting activity and participation improvements. We found that participants with cerebral palsy showed the greatest improvement in the Social Cognitive domain (Cohen’s d = 0.26), whereas participants with autism showed the greatest improvement in the Daily Activities domain (Cohen’s d = 0.58). This supports the research showing beneficial effects of HPOT for children with cerebral palsy (Novak et al., Citation2020) and autism (Srinivasan, Cavagnino, and Bhat, Citation2018); however, our data cannot explain why improvements were made in specific domains over others for these participants. This would be an interesting avenue for future research.
The PEDI-CAT was selected not only because of its ease of use in the clinical environment and reporting capabilities, but also for its cost-effectiveness and scalability as well as data collected. This assessment was especially clinically relevant because it was easily administered and incorporated within each pediatric clients’ plan of care regardless of age or diagnosis. All participants were able to complete the Speedy version of the PEDI-CAT within a single treatment session, which is in line with another study that reported all 4 domains were completed in an average time of 12 minutes (Dumas et al., Citation2012). It was noted to cost less than $4,000 for unlimited PEDI-CAT tests and 2 iPads that are also used for many relevant clinical applications such as video movement analysis, e-mail, and client education via anatomical diagrams. These costs represent a one-time setup fee for indefinite use of the PEDI-CAT assessment tool as well as the many other beneficial clinical uses of the iPads.
Individual PEDI-CAT score reports provided PTs with valuable data that informed clinical decisions. PTs were able to compare within individual reports, from initial assessment to 6 months later, to guide conversation between parent or caregiver and clinician and engage in shared, informed decision-making. If a client’s scores improved more than 2 times the standard error for a given domain, then PTs could be more certain that the outcome represented a real change in activity or participation. The PEDI-CAT score reports gave PTs and parents or caregivers a common language to discuss functional changes each child exhibited and guided the team to assess more specific areas of clients’ needs. Studies show that increasing communication between client and clinician leads to improved outcomes (Hargraves, LeBlanc, Shah, and Montori, Citation2016; Stiggelbout et al., Citation2012). PT’s in this study reported that this process often led to greater therapeutic rapport and mutual understanding.
An example of shared decision-making between PT and a participant’s parent comes from an 8-year-old girl, who was non-verbal, had behavioral challenges, and difficulty following directions. Her mother stated there was marked variability between the skills she demonstrated spontaneously at home and those she displayed upon request during treatment. The PEDI-CAT assessment allowed the therapist to capture the parent’s perspective of the child’s participation at home, as the mother was able to share about her child’s performance of activities, such as stair climbing or opening jars. Repeating the PEDI-CAT 6 months later revealed improved Mobility scaled scores from 61 to 65, as well as improved Daily Activities scaled scores from 52 to 54. The changes in Mobility scores likely represent changes beyond measurement error, as the 95% CIs of SE at Time 1 (59.20, 62.80) and Time 2 (63.58, 66.42) do not overlap. The changes in Daily Activities scores showed improvements but were slightly less likely to represent changes beyond measurement error, as only the 77% CIs of SE at Time 1 (51.05, 52.95) and Time 2 (52.99, 55.01) do not overlap. The parent and therapist discussed the improvement in scores as the therapist was not seeing her skills improve in clinical observations. The parent relayed marked improvements in her child’s abilities at home that corelated with PEDI-CAT scores representing actual functional change. The PT then tailored treatment goals to address areas of concern related to home and community performance and extended her PT plan of care.
A close examination of the HPOT process reveals why it may be particularly effective at treating not only body structure and body function impairments, but also activity limitations and participation restrictions of the ICF model (Chan et al., Citation2009). Although the activity and participation outcome improvements we observed cannot be attributed to HPOT alone, these results are in line with recent HPOT theoretical reasoning (Koca and Ataseven, Citation2015). HPOT effectively masks a high active workload, via enjoyable activities and changing environment, allowing increased repetition of motor skill practice. This repetition likely leads to solidifying motor skill acquisition (Merbah and Meulemans, Citation2011) to improve activity and participation reflected in PEDI-CAT scores. Activity and Participation skills commonly require dual-task abilities for independent completion (Huang and Mercer, Citation2001). Clients astride a walking horse frequently perform dual tasks by maintaining their balance while simultaneously reaching for objects, scanning their environment, and engaging with the therapist. This dual-task practice helps build automaticity of performance of certain tasks, as the unique challenges astride the horse may help generalize motor learning to other environments.
There are a few limitations to note about this study. Although we observed positive changes in activity following PT using HPOT, we lacked a control group and children were simultaneously involved in other therapies and activities reducing the confidence that these improvements were due solely to the use of HPOT. Participant data were collected at a single site limiting the sample size. This study did not incorporate a standardized treatment protocol–it required only that the horses’ movement be used for a minimum of 30 minutes per treatment session; however, PTs who provided HPOT were highly trained and provided similar treatments due to frequent collaboration. We chose not to include specialized PEDI-CAT modules (e.g. the PEDI-CAT with ASD scales) in the present study to specifically assess the feasibility of using a single assessment across a wide variety of diagnoses; however, it is notable that incorporating diagnosis-specific PEDI-CAT modules could produce more valid data for understanding children’s changes or improve interpretability of scaled scores by using module-specific referents. When paired with other traditional clinical methods, therapists can adjust HPOT application to address the individual needs of each child. Therefore, the application of HPOT in this study closely reflects how it is commonly implemented within clinical settings.
This study provides a foundation for future research on the incorporation of the PEDI-CAT as an assessment tool and its application in clinical settings, including those using HPOT. PTs feasibly used the PEDI-CAT to assess activity outcomes for children who received PT using HPOT with varying ages and diagnoses. It was cost-effective, easy to administer, and encouraged collaboration between clinician and caregiver to provide improved shared, clinical decision-making. Currently, our team is implementing a multi-site data collection effort to examine changes in PEDI-CAT outcomes for a larger, more geographically diverse sample. This effort will include PT, occupational therapy, and speech therapy using HPOT. This will allow more robust examination of the effectiveness of the PEDI-CAT to track changes in activity and participation outcomes among all professions that use HPOT.
Acknowledgments
We are also grateful to The Shea Center for Therapeutic Riding and the many clients and their families participated in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Academy of Pediatric Physical Therapy 2012 Intensity of service in an outpatient setting for children with chronic conditions. https://pediatricapta.org/includes/fact-sheets/pdfs/12%20Intensity%20of%20Service.pdf.
- Accardo P 2007 Capute and accardo’s neurodevelopmental disabilities in infancy and childhood. Baltimore: Brookes Publishing Company.
- Ajzenman H, Standeven J, Shurtleff T 2013 Effect of hippotherapy on motor control, adaptive behaviors, and participation in children with autism spectrum disorder: A pilot study. American Journal of Occupational Therapy 67(6): 653–663. doi:10.5014/ajot.2013.008383.
- American hippotherapy association 2019 Occupational therapy, physical therapy and speech therapy incorporating hippotherapy as a treatment tool. [accessed 2020 Mar 18]. https://aha.memberclicks.net/assets/docs/Present-Use-of-HPOT-final-proposed-revision-February-2019-2.pdf.
- American Physical Therapy Association 2014 Guide to physical therapist practice 3.0. [accessed 2022 Apirl 19]. http://guidetoptpractice.apta.org.
- Bates D, Mächler M, Bolker B, Walker S 2015 Fitting linear mixed-effects models using lme4. Journal of Statistical Software 67(1): 1–51. doi:10.18637/jss.v067.i01.
- Burgess A, Boyd RN, Chatfield MD, Ziviani J, Sakzewski L 2020 Self-care performance in children with cerebral palsy: A longitudinal study. Developmental Medicine and Child Neurology 62(9): 1061–1067. doi:10.1111/dmcn.14561.
- Cabiddu R, Borghi-Silva A, Trimer R, Trimer V, Ricci PA, Monteiro CI, Maniglia M, Pereira A, Rodrigues das Chagas G, Carvalho E 2016 Hippotherapy acute impact on heart rate variability non-linear dynamics in neurological disorders. Physiology & Behavior 159: 88–94. doi:10.1016/j.physbeh.2016.03.012.
- Champagne D, Dugas C 2010 Improving gross motor function and postural control with hippo-therapy in children with down syndrome: Case reports. Physiotherapy Theory and Practice 26(8): 564–571. doi:10.3109/09593981003623659.
- Chan F, Gelman J, Ditchman N, Kim J, Chiu C 2009 The World Health Organization ICF model as a conceptual framework of disability. New York: Springer Publishing Company.
- Cook CE 2008 Clinimetrics corner: The minimal clinically important change score (MCID): A necessary pretense. Journal of Manual and Manipulative Therapy 16(4): E82–E83. doi:10.1179/jmt.2008.16.4.82E.
- Dumas H, Fragala-Pinkham M, Haley S, Ni P, Coster W, Kramer J, Kao Y, Moed R, Ludlow L 2012 Computer adaptive test performance in children with and without disabilities: Prospective field study of the PEDI-CAT. Disability and Rehabilitation 34(5): 393–401. doi:10.3109/09638288.2011.607217.
- Dumas H, Fragala-Pinkham M, Rosen E, Lombard K, Farrell C 2015 Pediatric Evaluation of Disability Inventory Computer Adaptive Test (PEDI-CAT) and Alberta Infant Motor Scale (AIMS): Validity and responsiveness. Physical Therapy 95(11): 1559–1568. doi:10.2522/ptj.20140339.
- Dumas H, Fragala-Pinkham M, Rosen E, Ni P 2021 A content validity evaluation of the PEDI-CAT speedy mobility domain. Physiotherapy Theory and Practice 37(4): 517–526. doi:10.1080/09593985.2019.1633716.
- Durlak J 2009 How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology 34(9): 917–928. doi:10.1093/jpepsy/jsp004.
- Fragala-Pinkham M, Dumas H, Lombard K, O’Brien JE 2016 Responsiveness of the pediatric evaluation of disability inventory - computer adaptive test in measuring functional outcomes for inpatient pediatric rehabilitation. Journal of Pediatric Rehabilitation Medicine 9(3): 215–222. doi:10.3233/PRM-160382.
- Gencheva N, Ivanova I, Stefanova D 2015 Evaluation of hippotherapy in the course of multiple sclerosis treatment. Activities in Physical Education and Sport 5: 183–187.
- Goldstein D, Cohn E, Coster W 2004 Enhancing participation for children with disabilities: Application of the ICF enablement framework to pediatric physical therapist practice. Pediatric Physical Therapy 16(2): 114–120. doi:10.1097/01.PEP.0000127567.98619.62.
- Gonzalez S, Alvarez V, Nelson EL 2019 Do gross and fine motor skills differentially contribute to language outcomes? A systematic review. Frontiers in Psychology 10: 2670. doi:10.3389/fpsyg.2019.02670.
- Haley S, Coster W, Dumas H, Frangala-Pinkham M, Moed R 2012 PEDI-CAT: Development, standardization, and administration manual. Boston: CRE Care.
- Hargraves I, LeBlanc A, Shah N, Montori V 2016 Shared decision making: The need for patient-clinician conversation, not just information. Health Affairs 35(4): 627–629. doi:10.1377/hlthaff.2015.1354.
- Homem R, Oliveira R 2015 Influence of hippotherapy on the sleep of patients with Parkinson’s disease at advanced stage. Sleep Medicine 16: S181. doi:10.1016/j.sleep.2015.02.1363.
- Hsieh Y, Yang C, Sun S, Chan S, Wang T, Luo H 2017 Effects of hippotherapy on body functions, activities and participation in children with cerebral palsy based on ICF-CY assessments. Disability and Rehabilitation 39(17): 1703–1713. doi:10.1080/09638288.2016.1207108.
- Huang H, Mercer V 2001 Dual-task methodology: Applications in studies of cognitive and motor performance in adults and children. Pediatric Physical Therapy 13(3): 133–140. doi:10.1097/00001577-200113030-00005.
- Iverson J 2010 Developing language in a developing body: The relationship between motor development and language development. Journal of Child Language 37(2): 229–261. doi:10.1017/S0305000909990432
- Kang H, Jung J, Yu J 2012 Effects of hippotherapy on the sitting balance of children with cerebral palsy: A randomized control trial. Journal of Physical Therapy Science 24(9): 833–836. doi:10.1589/jpts.24.833.
- Kao YC, Kramer J, Liljenquist K, Tian F, Coster W 2012 Comparing the functional performance of children and youth with autism, developmental disabilities, and without disabilities using the revised Pediatric Evaluation of Disabilitiy Inventory (PEDI) item banks. American Journal of Occupational Therapy 66(5): 607–616. doi:10.5014/ajot.2012.004218.
- Kenyon LK, Farris JP, Gallagher C, Hammond L, Webster L, Aldrich N 2016 Power mobility training for young children with multiple, severe impairments: A case series. Physical & Occupational Therapy in Pediatrics 37(1): 19–34. doi:10.3109/01942638.2015.1108380.
- Kim S, Lee C 2014 The effects of hippotherapy on elderly persons’ static balance and gait. Journal of Physical Therapy Science 26(1): 25–27. doi:10.1589/jpts.26.25.
- Koca TT, Ataseven H 2015 What is hippotherapy? The indications and effectiveness of hippotherapy. Northern Clinics of Istanbul 2(3): 247–252 doi:10.14744/nci.2016.71601.
- Kwon J, Chang H, Yi S, Lee J, Shin H, Kim Y 2015 Effect of hippotherapy on gross motor function in children with cerebral palsy: A randomized controlled trial. Journal of Alternative and Complementary Medicine 21(1): 15–21 doi:10.1089/acm.2014.0021.
- Kwon T, Yi S, Kim T, Chang H, Kwon J 2013 Relationship between gross motor function and daily functional skill in children with cerebral palsy. Annals of Rehabilitation Medicine 37(1): 41–49. doi:10.5535/arm.2013.37.1.41.
- Lindroth J, Sullivan J, Silkwood-Sherer D 2015. Does hippotherapy effect use of sensory information for balance in people with multiple sclerosis?. Physiotherapy Theory and Practice 31: 575–581. doi:10.3109/09593985.2015.1067266.
- Lucena-Antón D, Rosety-Rodríguez I, Moral-Munoz J 2018 Effects of a hippotherapy intervention on muscle spasticity in children with cerebral palsy: A randomized controlled trial. Complementary Therapies in Clinical Practice 31: 188–192. doi:10.1016/j.ctcp.2018.02.013.
- Maenner M, Shaw K, Baio J, Wiggins L, Christensen D, Daniels J, Warren Z, Kurzius-Spencer M, Zahorodny W, White T, et al. 2020 Prevelance of autism spectrum disorder among children aged 8 years - Autism and developmental disabilities monitoring network, 11 sites, United States 2016. Morbidity and Mortality Weekly Report. Surveillance Summaries 69: 1–12.
- Maresca G, Portaro S, Naro A, Crisafulli R, Raffa A, Scarcella I, Aliberti B, Gemelli G, Calabro RS 2020 Hippotherapy in neurodevelopmental disorders: A narrative review focusing on cognitive and behavioral outcomes. Applied neuropsychology: Child Online ahead of print. [accessed 2022 Apirl 18]. doi:10.1080/21622965.2020.1852084.
- McGee M, Reese N 2009 Immediate effects of a hippotherapy session on gait parameters in children with spastic cerebral palsy. Pediatric Physical Therapy 21(2): 212–218. doi:10.1097/PEP.0b013e3181a39532.
- McGibbon N, Benda W, Duncan B, Silkwood-Sherer D 2009 Immediate and long-term effects of hippotherapy on symmetry of adductor muscle activity and functional ability in children with spastic cerebral palsy. Archives of Physical Medicine and Rehabilitation 90(6): 966–974. doi:10.1016/j.apmr.2009.01.011.
- Menezes K, Copetti F, Wiest M, Trevisan C, Silveira A 2013 Effect of hippotherapy on the postural stability of patients with multiple sclerosis: A preliminary study. Fisioterapia e Pesquisa 20(1): 43–49. doi:10.1590/S1809-29502013000100008.
- Merbah S, Meulemans T 2011 Learning a motor skill: Effects of blocked versus random practice a review. Psychologica Belgica 51(1): 15–48. doi:10.5334/pb-51-1-15.
- Muentener P, Herrig E, Schulz L 2018 The efficiency of infants’ exploratory play is related to longer-term cognitive development. Frontiers in Psychology 9: 635. doi:10.3389/fpsyg.2018.00635.
- Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, Hines A, Langdon K, Namara M, Paton M, Popat H, et al. 2020 State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Current Neurology and Neuroscience Reports 20(2): 3. doi:10.1007/s11910-020-1022-z.
- Pasternak A, Sideridis G, Fragala-Pinkham M, Glanzman A, Montes J, Dunaway S, Salazar R, Quigley J, Pandya S, O’Riley S, et al. 2016 Rasch analysis of the Pediatric Evaluation of Disability Inventory - Computer Adaptive Test (PEDI-CAT) item bank for children and young adults with spinal muscular atrophy. Muscle & Nerve 54(6): 1097–1107. doi:10.1002/mus.25164.
- Peters BC, Wood W, Hepburn S, Moody EJ 2021 Preliminary efficacy of occupational therapy in an equine environment for youth with autism spectrum disorder. Journal of Autism and Developmental Disorders Online ahead of print. doi:10.1007/s10803-021-05278-0.
- Pham C 2016 Bitonte R hippotherapy: Remuneration issues impair the offering of this therapeutic strategy at Southern California rehabilitation centers. Neurological Rehabilitation 38: 411–417.
- Rigby B, Gloeckner A, Sessums S, Lanning B, Grandjean P 2017 Changes in cardiorespiratory responses and kinematics with hippotherapy in youth with and without cerebral palsy. Research Quarterly for Exercise and Sport 88(1): 26–35. doi:10.1080/02701367.2016.1266458.
- Sadowska M, Sarecka-Hujar B, Kopyta I 2020 Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatric Disease and Treatment 16: 1505–1518. doi:10.2147/NDT.S235165.
- Shore B, Allar B, Miller P, Matheney T, Snyder B, Fragala-Pinkham M 2019 Measuring the reliability and construct validity of the Pediatric Evaluation of Disability Inventory - Computer Adaptive Test (PEDI-CAT) in children with cerebral palsy. Archives of Physical Medicine and Rehabilitation 100(1): 45–51. doi:10.1016/j.apmr.2018.07.427.
- Srinivasan S, Cavagnino D, Bhat A 2018 Effects of equine therapy on individuals with autism spectrum disorder: A systematic review. Review Journal of Autism and Developmental Disorders 5: 156–175. doi:10.1007/s40489-018-0130-z.
- Stiggelbout A, Van der Weijden T, De Wit M, Frosch D, Légaré F, Montori V, Trevena L, Elwyn G 2012 Shared decision making: Really putting patients at the centre of healthcare. British Medical Journal 344: 256. doi:10.1136/bmj.e256.
- Thompson S, Cech D, Cahill S, Krzak J 2018 Linking the Pediatric Evaluation of Disability Inventory-Computer Adaptive Test (PEDI-CAT) to the international classification of function. Pediatric Physical Therapy 30: 113–118. doi:10.1097/PEP.0000000000000483.
- Thompson F, Ketcham C, Hall E 2014 Hippotherapy in children with developmental delays: Physical function and psychological benefits. Advances in Physical Education 4(2): 60–69. doi:10.4236/ape.2014.42009.
- Westfall J, Mold J, Fagnan L 2007 Practice-based research - “Blue Highways” on the NIH Roadmap. JAMA 297(4): 403–406. doi:10.1001/jama.297.4.403.
- Wood W, Fields B 2021 Hippotherapy: A systematic mapping review of peer-reviewed research, 1980 to 2018. Disability and Rehabilitation 43(10): 1463–1487. doi:10.1080/09638288.2019.1653997.
- World Health Organization 2007 International classification of functioning, disability and health: Children and youth version: ICF- CY. Geneva: World Health Organization.
- Zadnikar M, Kastrin A 2011 Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: A meta-analysis. Developmental Medicine and Child Neurology 53(8): 684–691. doi:10.1111/j.1469-8749.2011.03951.x.
Appendix
The following questions guided discussions between the primary investigator and the 5 participating therapists during once-per-month translational team meetings. Questions appear in no specific order.
