ABSTRACT
Background
Physical inactivity is common during hospitalization. Physical activity has been described in different inpatient populations but never across a hospital.
Purpose
To describe inpatient movement behavior and associated factors throughout a single university hospital.
Methods
A prospective observational study was performed. Patients admitted to clinical wards were included. Behavioral mapping was undertaken for each participant between 9AM and 4PM. The location, physical activity, daily activity, and company of participants were described. Barriers to physical activity were examined using linear regression analyses.
Results
In total, 345 participants from 19 different wards were included. The mean (SD) age was 61 (16) years and 57% of participants were male. In total, 65% of participants were able to walk independently. On average participants spent 86% of observed time in their room and 10% of their time moving. A physiotherapist or occupational therapist was present during 1% of the time, nursing staff and family were present 11% and 13%, respectively. Multivariate regression analysis showed the presence of an intravenous line (p = .039), urinary catheter (p = .031), being female (p = .034), or being dependent on others for walking (p = .016) to be positively associated with the time spent in bed. Age > 65, undergoing surgery, receiving encouragement by a nurse or physician, reporting a physical complaint or pain were not associated with the time spent in bed (P > .05).
Conclusion
As family members and nursing staff spend more time with patients than physiotherapists or occupational therapists, increasing their involvement might be an important next step in the promotion of physical activity.
Introduction
A low amount of inpatient physical activity is common during hospitalization (Baldwin, van Kessel, Phillips, and Johnston, Citation2017; Fazio et al., Citation2020; Zisberg et al., Citation2015). Patients spend up to 83% of their time lying in bed, even when there is no medical reason to stay in bed (Brown, Redden, Flood, and Allman, Citation2009; Mudge et al., Citation2016; Pedersen et al., Citation2013; van de Port, Valkenet, Schuurmans, and Visser-Meily, Citation2012). As a result, patients frequently develop functional decline which is associated with complications like pneumonia, urinary tract infections, increased length of stay, institutionalization, mortality, and recovery that extends for months to years (Boyd et al., Citation2008; Brown, Redden, Flood, and Allman, Citation2009; Portegijs et al., Citation2012).
To address this problem, there is a need to identify enablers and reduce barriers to inpatient mobilization in hospitals. While several qualitative studies reported patient factors, like having symptoms or a catheter that may influence physical activity during hospital stay (Brown et al., Citation2007; Kalisch, Landstrom, and Williams, Citation2009; Koenders et al., Citation2020), quantitative studies of patient mobility have focused on specific patient groups (Anaker et al., Citation2017; Bernhardt, Dewey, Thrift, and Donnan, Citation2004; Covinsky et al., Citation2003; Koenders et al., Citation2021). Insight into patient behavior, related to physical activity across a hospital, is needed to establish an objective and comprehensive picture of the mobility culture throughout hospitals. Therefore, the aims of this study were to describe inpatient movement behavior across a large university hospital, and to explore factors associated with the proportion of time patients spent in bed.
Methods
Design and setting
This prospective observational study was performed at the University Medical Center Utrecht in the Netherlands, a university city hospital with the capacity for more than 800 adult inpatients. The study protocol (no. 16–250) was approved by the Medical Ethics Committee of the University Medical Center Utrecht. No funding was received for this study.
Participants
Patients were eligible for inclusion if they were aged ≥18 years and were admitted to a clinical ward of the hospital. Patients were excluded if they were admitted to the Intensive Care Unit (ICU); had a cognitive impairment defined as an acute disorder of attention and cognition (e.g. delirium); were on strict bedrest orders; were receiving end-of-life care; or were planned for discharge on the day of data collection. Verbal informed consent was obtained from all participants.
Study procedures
Since September 2016, as part of a program to assess and improve movement behavior across the hospital, direct patient observations were planned on all non-ICU wards every six months to assess and evaluate movement behavior over time. The day before the observations were planned, a physiotherapist-researcher compiled a list of eligible patients after consulting the head nurse of the ward being observed. Patients on the list were approached for participation by the physiotherapist-researcher. A maximum of eight patients could be included per ward, per observation day. Inclusion stopped when eight patients wanted to participate, or when no more eligible patients were available. Participants were informed that the activities during an average day in the hospital were being observed, they were not told exactly what was recorded.
Direct patient observations
Observations were performed according to a behavioral mapping method (Bernhardt, Dewey, Thrift, and Donnan, Citation2004; Valkenet, Bor, van Delft, and Veenhof, Citation2019). Participants were observed at set intervals over one day of their hospital admission. Per participant, a 1-min observation was performed every 10 min between 9AM and 4PM (Bernhardt, Dewey, Thrift, and Donnan, Citation2004).
During each 1-min observation, four categories were observed and recorded in an Excel spreadsheet: 1) location of the participant; 2) body position of the participant; 3) daily activity undertaken by the participant; and 4) persons in direct contact with the participant. Each category contained multiple predefined items (Table A1). The item that was observed for the longest period within the 1-min observation was recorded. If two or more items were observed for the same amount of time, the one with the highest intensity was recorded.
For this study, movement behavior was defined as the percentage of the total observed time that a participant spent in a specific body position. A distinction was made between lying in bed, sitting (i.e. bedside or chair), and moving (i.e. standing, transferring, walking, and cycling). The level of agreement with an accelerometer for identifying these three physical activity levels is strong (Valkenet, Bor, van Delft, and Veenhof, Citation2019). The proportion of time spent lying in bed was defined as the primary outcome.
The observations were performed by undergraduate physiotherapy students. The students received paper instructions and a face-to-face training by a physiotherapist-researcher about the assessment to be performed. During the first observation day of a student, a physiotherapist-researcher guided the student during the first observation round. Furthermore, a physiotherapist-researcher remained on standby for questions during the observation days.
Additional data collection
The following characteristics were collected per participant by the observers during the day of observation: gender, age, ward, medical specialty, date of admission, reason for admission, surgery (yes/no), intravenous catheter (yes/no), and urinary catheter (yes/no).
Physical function levels of the participants were assessed with the Activity Measure for Post-Acute Care (AM-PAC) “6-Clicks” inpatient Basic Mobility (Jette et al., Citation2014). This short form has six items that were scored by the observers on a 4-point ordinal scale based on patient report, direct observation, clinical judgment, or after consultation with the patient or nurse in charge (Hoyer et al., Citation2018). Total score ranges from 6 to 24 with higher scores indicating better function (Jette et al., Citation2014). The reliability and validity of this short form is excellent in acute hospitalized patients (Geelen, Valkenet, and Veenhof, Citation2019; Jette et al., Citation2014).
Furthermore, participants were asked by the observer which physical symptom (i.e. pain, fatigue, fear of falling, weakness, nausea, other, or none) they perceived to be the main barrier to undertake physical activity. The level of encouragement participants perceived from nursing and medical staff to be physically active in the past two days was investigated with two statements. The statements were defined as follows: ‘You have been encouraged by a nurse/physician to be physically active (i.e. getting out of bed as much as possible, sitting up or walking).’ These statements could be answered on a 5-point scale (i.e. strongly disagree; disagree; undecided; agree; and strongly agree). The date of discharge was retrieved retrospectively from the electronic patient records.
Data analyses
All data were recorded directly in a Microsoft (Redmond, USA) Excel spreadsheet using a tablet computer. The spreadsheets per observer were merged, and imported into the Statistical Package for the Social Sciences (SPSS) version 25 (IBM, New York, USA) by a physiotherapist-researcher. Missing behavioral mapping observations were not included in the analyses. The proportion of time observed per behavioral map item, was calculated per participant. Following, the average proportion of time per item was calculated for the total population. The category ’body position’ was further categorized into lying, sitting, and moving (Valkenet, Bor, van Delft, and Veenhof, Citation2019). The patterns of location, movement behavior, daily activity, and company of patients during the day were visualized by plotting the percentages of observed time per item against each 1-min observation over the total observation period.
Linear regression was used to examine factors associated with the proportion of time spent lying. Univariate linear regression was used to assess the association of 10 variables that were selected based on earlier studies (Brown et al., Citation2007; De Klein, Valkenet, and Veenhof, Citation2021; Koenders et al., Citation2021): 1) gender (male/female); 2) age > 65 years (yes/no); 3) level of dependence (i.e. needing assistance with walking) (yes/no); 4) presence of pain during physical activity (yes/no); 5) presence of one or more physical complaints during physical activity (yes/no); 6) presence of urinary catheter (yes/no); 7) presence of intravenous catheter (yes/no); 8) underwent surgery (yes/no); 9) received encouragement from a nurse to be physically active (yes/no); and 10) received encouragement from a physician to be physically active (yes/no). Variables with a p-value < 0.2 were entered in a multivariable linear model. Variables in the multivariable analyses with a p < .05 were considered statistically significant. The adjusted R2 was used to estimate the variance in time spent lying by the variables in the multivariable model.
Results
The data of four observation periods, between September 2016 and June 2018, were included. In total 345 participants (period 1: n = 85; period 2: n = 83; period 3: n = 106; and period 4: n = 71) from 19 different non-ICU wards were included in the analyses. The gynecology ward was excluded in period 3 and 4 as this ward did not find direct observations appropriate for their population. Table A2 shows the number of participants, movement behavior, and physical functional levels per ward.
The mean age of the participants was 61 ± 16 years (SD) and 57% were male. In total, 65% of participants were independently mobile, while 70% reported a physical symptom as a barrier to perform physical activity ().
Table 1. Participant characteristics.
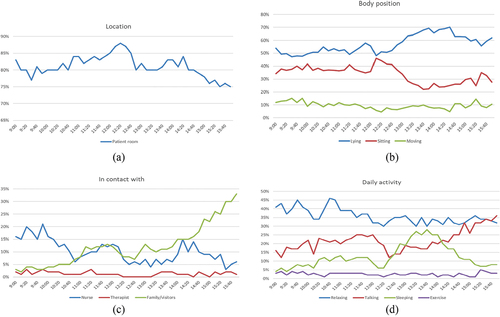
Across our sample participants spent on average 86% of the observed time in their room, and 55% of their time lying in bed, 35% sitting, and 10% moving (). Participants were alone 56% of the observed time, in direct contact with family or visitors for 13% of the time, with nursing staff 11% of the time, with physicians 3% of the time, and with a physiotherapist or occupational therapist 1% of the time. In total, 30% of the daytime was spent relaxing (doing nothing or reading) and 2% was spent on physical exercises.
Table 2. Average percentage of the time observed per behavioral map item.
In the patterns of movement behavior throughout the day are shown. It was observed that patients were in their room around lunchtime the most. A high proportion of patients returned to bed after lunchtime. Family/visitors were present more in the afternoon compared to the morning. The presence of nursing staff peaked during three times (9.00–10.00 h, 11.30–12.00 h, 14.00–14.30 h). Physiotherapists or occupational therapists were infrequently observed throughout the day. The proportion of participants sleeping peaked directly after lunchtime, and the proportion of participants observed talking increased steadily during the afternoon. During most observations, the participants were observed relaxing (i.e. doing nothing or reading/using tablet or phone).
Figure 1. Patterns of key observed items throughout the day. 1a. Pattern throughout the day of the proportion of patients observed in their room. 1b. Patterns throughout the day of the proportion of patients spending their time lying, sitting or moving. 1c. Patterns throughout the day of the proportion of patients observed in direct contact with a nurse, therapist or family/visitors. 1d. Patterns throughout the day of the proportion of patients observed relaxing, talking, sleeping or performing exercise.
In the results of the regression analyses are shown. All independent variables had a positive association with the time spent lying in the univariable analyses (P < .2). After entering these variables into a multivariable model the presence of an intravenous catheter, a urinary catheter, being female, and needing any help with walking were found to be positively associated with the time spent in lying in bed (P < .05). The adjusted R2 of the multivariable model was 0.114.
Table 3. Associations between proportion of time spent lying in bed and factors of interest*.
Discussion
This study is the first to describe inpatient movement behavior across all clinical non-ICU wards of a hospital. Our results show that patients remain in their room for the majority of the day. Our results also show and patients are moving for only 10% of daytime hours. They only spend 2% of the daytime participating in supervised or self-directed exercise. Physiotherapists or occupational therapists were only in contact with patients during 1% of the observed time, while nursing staff and family members were present for 11% and 13% of the time, respectively.
It was observed that a higher proportion of patients were sitting and moving in the morning, and that patients returned to bed in the afternoon. This is consistent with the findings in a rehabilitation setting (McRae, Bew, Smith, and Mudge, Citation2020). Visitors were present more in the afternoon than the morning, coinciding with visiting hours in our hospital. This indicates that patients are less active when their family members or visitors are present.
Currently, patients and health-care professionals rely on physiotherapists or occupational therapists for patient mobility. Our results show that 65% of patients are independently mobile, which highlights the importance of the involvement of others in patient mobility. To integrate physical activity in daily care, it may be important to better involve family members and nursing staff. Recent research shows the potential of family participation in physiotherapy-related tasks (van Delft, Valkenet, Slooter, and Veenhof, Citation2021a). Understanding how to increase family participation in promoting physical activity may be an important next step (van Delft, Valkenet, Slooter, and Veenhof, Citation2021b). Additionally, understanding how to involve nursing staff in the promotion of inpatient physical activity, given their limited time, is important (Dermody and Kovach, Citation2017; Kneafsey, Clifford, and Greenfield, Citation2013).
Increasing patient awareness about the hazards of bedrest, and the importance of physical activity during hospitalization, is suggested as an important step to improve movement behavior (De Klein, Valkenet, and Veenhof, Citation2021; Koenders et al., Citation2020). However, our results show that participants who reported receiving encouragement to be physically active by nursing or medical staff did not spend less time lying in bed. Although the causal relationship was not investigated, and the actual amount of encouragement participants received is unknown, encouragement to be physically active on its own may be inadequate to achieve higher levels of physical activity and may likely relate to other barriers.
We found the presence of an intravenous line, a urinary catheter, and being dependent on others for walking to be positively associated with the time spent lying in bed. This in line with earlier studies and confirms that these factors need to be addressed to promote physical activity (Brown et al., Citation2007; Koenders et al., Citation2021). Identifying the barriers and enablers to physical activity may help to design interventions. To achieve long-term changes previous literature highlights that unimodal interventions might not be sufficient (Craig et al., Citation2013; Moore et al., Citation2015). Programs like Hospital in Motion, Eat Walk Engage and the Johns Hopkins Activity and Mobility Promotion are good examples of multimodal interventions (Hoyer et al., Citation2016; Mudge, McRae, and Cruickshank, Citation2015; van Delft et al., Citation2020). These programs target multiple barriers (e.g. individual, inter-personal, and institutional) and use multi-disciplinary teams to improve physical activity and change culture (McLeroy, Bibeau, Steckler, and Glanz, Citation1988). In the Table A2 we report the amount of physical activity per ward. These numbers might serve as guide to specific wards for determining if additional actions are necessary.
Strengths and limitations
A limitation of this study is that, by using the behavioral mapping method, participants were only observed during the daytime, and only while they were present on the ward. Other limitations of this study are that the reasons for missing behavioral mapping data were not recorded, and that there are no data available of patients who were ineligible or unwilling to participate. While only patients with strict bed rest orders or receiving end-of-life care were excluded from the observations, patients feeling severely ill were likely approached less often, and declined participation more frequently, compared to patients feeling less ill. Therefore, selection bias cannot be ruled out. Furthermore, across our sample we found a median length of hospital stay of 10 days while the average of our hospital is 6 days (unpublished hospital data). We hypothesize that this is a result of the exclusion of patients who were due to be discharged on the observation day, resulting in more frequent exclusion of patients with shorter lengths of stay.
In conclusion, our findings confirm high levels of physical inactivity across the hospital. Our results show that family members and nursing staff spend more time with patients than physiotherapists or occupational therapists. Increasing the involvement of family members and nursing staff, making them key enablers of physical activity, might be an important next step in the promotion and support of physical activity. In this study, a higher proportion of participants were lying in bed during the afternoon which highlights the opportunity for additional physical activity in this part of the day. Addressing factors such as intravenous lines and the need for assistance remain important to facilitate physical activity.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anaker A, von Koch L, Sjostrand C, Bernhardt J, Elf M, Martinuzzi A 2017 A comparative study of patients’ activities and interactions in a stroke unit before and after reconstruction-The significance of the built environment. PLoS One 12:e0177477. 10.1371/journal.pone.0177477.
- Baldwin C, van Kessel G, Phillips A, Johnston K 2017 Accelerometry shows inpatients with acute medical or surgical conditions spend little time upright and are highly sedentary: Systematic review. Physical Therapy 97:1044–1065.
- Bernhardt J, Dewey H, Thrift A, Donnan G 2004 Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke 35:1005–1009. 10.1161/01.STR.0000120727.40792.40.
- Boyd CM, Landefeld CS, Counsell SR, Palmer RM, Fortinsky RH, Kresevic D, Covinsky KE, Covinsky KE 2008 Recovery of activities of daily living in older adults after hospitalization for acute medical illness. Journal of the American Geriatrics Society 56:2171–2179. 10.1111/j.1532-5415.2008.02023.x.
- Brown CJ, Redden D, Flood K, Allman RM 2009 The under recognized epidemic of low mobility during hospitalization of older adults. Journal of the American Geriatrics Society 57:1660–1665. 10.1111/j.1532-5415.2009.02393.x.
- Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM 2007 Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. Journal of Hospital Medicine 2:305–313. 10.1002/jhm.209.
- Covinsky K, Palmer R, Fortinsky R, Counsell S, Stewart A, Kresevic D, Burant C, Landefeld C 2003 Loss of Independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. Journal of the American Geriatrics Society 51:451–458. 10.1046/j.1532-5415.2003.51152.x.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M 2013 Developing and evaluating complex interventions: The new medical research council guidance. International Journal of Nursing Studies 50:587–592. 10.1016/j.ijnurstu.2012.09.010.
- De Klein K, Valkenet K, Veenhof C 2021 Perspectives of patients and health-care professionals on physical activity of hospitalized patients. Physiotherapy Theory and Practice 37:307–314. 10.1080/09593985.2019.1626517.
- Dermody G, Kovach C 2017 Nurses’ experience with and perception of barriers to promoting mobility in hospitalized older adults: A descriptive study. Journal of Gerontological Nursing 43:22–29. 10.3928/00989134-20170518-01.
- Fazio S, Stocking J, Kuhn B, Doroy A, Blackmon E, Young HM, Adams JY 2020 How much do hospitalized adults move? A systematic review and meta-analysis. Applied Nursing Research 51:151189. 10.1016/j.apnr.2019.151189.
- Geelen SJG, Valkenet K, Veenhof C 2019 Construct validity and inter-rater reliability of the Dutch activity measure for post-acute care “6-clicks” basic mobility form to assess the mobility of hospitalized patients. Disability and Rehabilitation 41:2563–2569. 10.1080/09638288.2018.1471525.
- Hoyer EH, Friedman M, Lavezza A, Wagner-Kosmakos K, Lewis-Cherry R, Skolnik JL, Byers SP, Atanelov L, Colantuoni E, Brotman DJ, et al. 2016 Promoting mobility and reducing length of stay in hospitalized general medicine patients: A quality-improvement project. Journal of Hospital Medicine 11:341–347. 10.1002/jhm.2546.
- Hoyer E, Young D, Klein L, Kreif J, Shumock K, Hiser S, Friedman M, Lavezza A, Jette A, Chan K, et al. 2018 Toward a common language for measuring patient mobility in the hospital: Reliability and construct validity of interprofessional mobility measures. Physical Therapy 98:133–142. 10.1093/ptj/pzx110.
- Jette DU, Stilphen M, Ranganathan V, Passek S, Frost F, Jette A 2014 Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Physical Therapy 94:379–391. 10.2522/ptj.20130199.
- Kalisch BJ, Landstrom G, Williams RA 2009 Missed nursing care: Errors of omission. Nursing Outlook 57:3–9. 10.1016/j.outlook.2008.05.007.
- Kneafsey R, Clifford C, Greenfield S 2013 What is the nursing team involvement in maintaining and promoting the mobility of older adults in hospital? A grounded theory study. International Journal of Nursing Studies 50:1617–1629. 10.1016/j.ijnurstu.2013.04.007.
- Koenders N, van Oorsouw R, Seeger JP, Nijhuis-van der Sanden MW, van de Glind I, Hoogeboom T 2020 “I’m not going to walk, just for the sake of walking … ”: A qualitative, phenomenological study on physical activity during hospital stay. Disability and Rehabilitation 42:78–85. 10.1080/09638288.2018.1492636.
- Koenders N, Weenk M, van de Belt TH, van Goor H, Hoogeboom TJ, Bredie SJ 2021 Exploring barriers to physical activity of patients at the internal medicine and surgical wards: A retro-spective analysis of continuously collected data. Disability and Rehabilitation 43:1883–1889. 10.1080/09638288.2019.1685013.
- McLeroy KR, Bibeau D, Steckler A, Glanz K 1988 An ecological perspective on health promotion programs. Health Education Quarterly 15:351–377. 10.1177/109019818801500401.
- McRae P, Bew P, Smith S, Mudge A 2020 An observational study of physical, cognitive and social activities in rehabilitation inpatients. Australasian Journal of Ageing 39:217–222. 10.1111/ajag.12785.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, Moore L, O’Cathain A, Tinati T, Wight D, et al. 2015 Process evaluation of complex interventions: Medical research council guidance. British Medical Journal 350:h1258. 10.1136/bmj.h1258.
- Mudge A, McRae P, Cruickshank M 2015 Eat walk engage: An interdisciplinary collaborative model to improve care of hospitalized elders. American Journal of Medical Quality 30:5–13. 10.1177/1062860613510965.
- Mudge A, McRae P, McHugh K, Griffin L, Hitchen A, Walker J, Cruickshank M, Morris N, Kuys S 2016 Poor mobility in hospitalized adults of all ages. Journal of Hospital Medicine 11:289–291. 10.1002/jhm.2536.
- Pedersen M, Bodilsen A, Petersen J, Beyer N, Andersen O, Lawson-Smith L, Kehlet H, Bandholm T 2013 Twenty-four-hour mobility during acute hospitalization in older medical patients. Journals of Gerontology Series A Biological Sciences and Medical Sciences 68:331–337. 10.1093/gerona/gls165.
- Portegijs E, Buurman BM, Essink-Bot ML, Zwinderman AH, de Rooij SE 2012 Failure to regain function at 3 months after acute hospital admission predicts institutionalization within 12 months in older patients. Journal of the American Medical Directors Association 13:567–569. 10.1016/j.jamda.2012.04.003.
- Valkenet K, Bor P, van Delft L, Veenhof C 2019 Measuring physical activity levels in hospitalized patients: A comparison between behavioural mapping and data from an accelerometer. Clinical Rehabilitation 33:1233–1240. 10.1177/0269215519836454.
- van de Port IG, Valkenet K, Schuurmans M, Visser-Meily JM 2012 How to increase activity level in the acute phase after stroke. Journal of Clinical Nursing 21:3574–3578. 10.1111/j.1365-2702.2012.04249.x.
- van Delft LM, Bor P, Valkenet K, Slooter A, Veenhof C 2020 The effectiveness of hospital in motion, a multidimensional implementation project to improve patients’ movement behavior during hospitalization. Physical Therapy 100:2090–2098. 10.1093/ptj/pzaa160.
- van Delft LM, Valkenet K, Slooter AJ, Veenhof C 2021a Family participation in physiotherapy related tasks of critically ill patients: A mixed methods systematic review. Journal of Critical Care 62:49–57. 10.1016/j.jcrc.2020.11.014.
- van Delft LM, Valkenet K, Slooter AJ, Veenhof C 2021b Perceptions and ideas of critically ill patients, their family and staff members regarding family participation in the physiotherapy-related care of critically ill patients: A qualitative study. Physiotherapy Theory and Practice Online ahead of print. 1–18. 10.1080/09593985.2021.1990451.
- Zisberg A, Shadmi E, Gur-Yaish N, Tonkikh O, Sinoff G 2015 Hospital-associated functional decline: The role of hospitalization processes beyond individual risk factors. Journal of the American Geriatrics Society 63:55–62. 10.1111/jgs.13193.
