ABSTRACT
Background
There is a relationship between low back pain (LBP) and central nervous system dysfunction. Needling therapies (e.g. acupuncture, dry needling) are proposed to impact the nervous system, however their specific influence is unclear.
Purpose
Determine how needling therapies alter functional connectivity and LBP as measured by functional magnetic resonance imaging (fMRI).
Methods
Databases were searched following PRISMA guidelines. Studies using fMRI on individuals with LBP receiving dry needling or acupuncture compared to control or sham treatments were included.
Results
Eight studies were included, all of which used acupuncture. The quality of studies ranged from good (n = 6) to excellent (n = 2). After acupuncture, individuals with LBP demonstrated significant functional connectivity changes across several networks, notably the salience, somatomotor, default mode network (DMN) and limbic networks. A meta-analysis demonstrated evidence of no effect to potential small effect of acupuncture in reducing LBP (SMD −0.28; 95% CI: −0.70, 0.13).
Conclusion
Needling therapies, like acupuncture, may have a central effect on patients beyond the local tissue effects, reducing patients’ pain and disability due to alterations in neural processing, including the DMN, and potentially other central nervous system effects. The meta-analysis should be interpreted with caution due to the narrow focus and confined sample used.
Introduction
Low back pain (LBP) costs approximately $100 billion in healthcare dollars annually in the United States (Oliveira et al., Citation2018). LBP is one of the chief contributors to days lived with disability and time lost from work (Delitto et al., Citation2012; Hides, Jull, and Richardson, Citation2001; Oliveira et al., Citation2018). Globally the biomedical model of medicine has established many clinical practice guidelines to direct rehabilitation for those living with LBP (Chenot et al., Citation2017; Delitto et al., Citation2012; Oliveira et al., Citation2018). Rates of recurrent episodes of LBP and development of chronic LBP are high with medical management compared to trunk stability exercises (Hides, Jull, and Richardson, Citation2001). This has led to a shift from the biomedical model toward the biopsychosocial model for the treatment of LBP to address the mind-body connection and the influence of the central nervous system (CNS) on pain perception (Langevin, Citation2021; Lin et al., Citation2020).
Alterations in brain activity and functional connectivity in individuals with LBP at rest have been identified using functional magnetic resonance imaging (fMRI) (Apkarian, Bushnell, Treede, and Zubieta, Citation2005; Konno and Sekiguchi, Citation2018; Kregel et al., Citation2015). For example, individuals with LBP showed greater activation in the prefrontal cortex (PFC) in response to pain compared to their healthy counterparts (Apkarian, Bushnell, Treede, and Zubieta, Citation2005; Konno and Sekiguchi, Citation2018; Kregel et al., Citation2015). The PFC is a pivotal brain region that supports top-down cognitive control playing a key role in the coding of contextual information and goal representations (Miller and Cohen, Citation2001; Tamber-Rosenau, Esterman, Chiu, and Yantis, Citation2011) which subsequently influences attention, memory, and impulse control (Ott and Nieder, Citation2019). This area of the brain was made famous by a railroad accident when an iron rod penetrated the skull of Phineas Gage, and damaged his left frontal lobe. This injury caused him to be aggressive, engage in risky, and inappropriate behavior (García-Molina, Citation2012). In contrast, healthy controls demonstrated activation in the primary and secondary somatosensory cortices, the anterior cingulate cortex, and the thalamus under the same painful conditions (Apkarian, Bushnell, Treede, and Zubieta, Citation2005). The somatosensory cortices play a key role in processing sensory information, as well as emotional processing (Kropf, Syan, Minuzzi, and Frey, Citation2019). The anterior cingulate cortex connects rewards to actions and is involved with emotion (Kropf, Syan, Minuzzi, and Frey, Citation2019). The thalamus plays a key role in relaying sensory and motor signals (Torrico and Munakomi, Citation2021). The literature supporting changes in the activity of critical regions in the brain in those with LBP-led researchers to explore treatments that may influence these neurological effects of pain processing in this population (Apkarian, Bushnell, Treede, and Zubieta, Citation2005; Konno and Sekiguchi, Citation2018; Kregel et al., Citation2015).
There are many types of needling therapies practiced across the world. Traditional acupuncture, western medical acupuncture, and dry needling are all techniques that involve inserting a small gauge traditional acupuncture needle into the skin (Zhou, Ma, and Brogan, Citation2015). Traditional acupuncture is used by acupuncturists using Eastern medicine concepts to treat musculoskeletal pain, gastrointestinal discomfort, and neurological dysfunction (Zhou, Ma, and Brogan, Citation2015). Western medical acupuncture is practiced primarily in Europe by physicians, chiropractors, and physical therapists and involves inserting a needle into the body based on biomedical principles (Zhou, Ma, and Brogan, Citation2015). Dry needling is popular among physical therapists in the United States, but other healthcare professionals (i.e. chiropractors, athletic trainers, and physicians) also practice it, and the purpose of its use is less broad than traditional acupuncture or western medical acupuncture with the goal of inserting a needle based on the location of pain, and anatomy to treat various musculoskeletal conditions (Zhou, Ma, and Brogan, Citation2015).
Pain reduction following the mechanical stimulation of local tissue using small gauge dry needles (e.g. dry needling and acupuncture) has been established (Furlan et al., Citation2005; Yuan et al., Citation2016). One of the proposed mechanisms of needling therapies is that stimulating nociceptors within a myofascial trigger point or taut band of muscular tissue via insertion of a monofilament needle propagates sensory input to the spinal cord subsequently inducing a spinal reflex that results in alpha motor neuron output (Dunning et al., Citation2014). This ultimately elicits a twitch response or reflexive contraction that breaks the pattern of continued tension within a myofascial trigger point to relieve pain (Dunning et al., Citation2014). There is moderate evidence to support the use of dry needling into local tissue to treat LBP (Lin et al., Citation2020). In addition to this local effect on myofascial trigger points, there is evidence that needling therapies can also modulate pain from a “top-down” mechanism beyond the spinal cord by influencing the higher processing centers in the CNS (Audette, Feng, and Howard, Citation2004; Dunning et al., Citation2014).
Research on needling therapies, in particular, traditional acupuncture, has not been limited to just the musculoskeletal and peripheral nervous system, but investigating changes in brain activity and connectivity following needling therapy (Cagnie et al., Citation2013; Chae et al., Citation2013; Fang et al., Citation2009; Hui et al., Citation2009; Kucyi et al., Citation2014; Otti et al., Citation2013). Acupuncture treatment has been shown to result in changes in activation of the: default mode network (DMN); amygdala; cingulate cortices; sensorimotor network (SMN); limbic-paralimbic-neocortical network (LPNN); and salience network (SN) (Chae et al., Citation2013; Fang et al., Citation2009; Hui et al., Citation2009; Kucyi et al., Citation2014; Otti et al., Citation2013). However, it is unclear if needling a body region has an effect both at the site of insertion and at the CNS level (i.e. brain and spinal cord) that significantly influences clinical outcomes, especially since it is difficult for studies to adequately blind the participant to whether or not they received real or sham needling. This systematic review aims to consolidate the literature regarding how needling therapies may modulate pain perception at the CNS level by inserting a monofilament needle into the local tissues in patients with LBP compared to healthy controls and sham treatments.
Methods
This systematic review was performed under the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher, Liberati, Tetzlaff, and Altman, Citation2009). The review was registered through PROSPERO, an International Prospective Register of Systematic Reviews (#CRD42020197995).
Selection and description of participants
PICO (i.e. population, intervention, controls, and outcomes) guidelines were used to guide this review that investigated the following two questions: 1) Do those with LBP have different brain activation and connectivity patterns compared to healthy controls following needling therapies; and 2) Do those with LBP have different brain activation and connectivity patterns following “real” needling therapies compared to “sham”?
All studies were eligible for inclusion in the systematic review if they met the inclusion criteria and satisfied our PICO questions (). Needling therapies were defined as any acupuncture or dry needling procedure where a needle was inserted into the body and no solution was injected, which would exclude medical injections. Sham acupuncture and sham dry needling were operationally defined as a procedure where the needle did not pierce the skin or was purposefully inserted into a part of the body where there was no expected therapeutic intent. Low back pain was operationally defined as any condition affecting the low back, including any condition likely responsible for radicular symptoms in the legs (i.e. sciatica, disc herniation, and lumbar stenosis).
Table 1. Inclusion and exclusion criteria.
Data sources
After consulting with a librarian (AB), the following nine databases were systematically searched from database inception to June 2022: Pubmed, Cinahl Plus with Full-Text, Biosys Previews, Scopus, EMBase, APA PsychInfo, AltHealthWatch, Web of Science, and Google Scholar. Most databases were selected as sources due to their relationships to medicine, physical medicine, physical therapy, and other interventions like the eastern medicine practice of acupuncture. Some databases, like APA PsychInfo, were selected because studies using fMRI are more commonly published in psychology-based journals.
Search strategy
Search terms were developed based on Medical Subject Headings (MeSH) Terms from PubMed and keywords from studies of interest. The following search terms were inserted into each of the nine databases: (Needling OR Dry Needling OR Acupuncture OR Acupuncture therapy) AND (Electroencephalography OR Electroencephalogram OR EEG, OR Magnetic Resonance Imaging OR fMRI OR Neuroimaging OR functional neuroimaging OR Brain imaging OR Brain Mapping).
Study selection and eligibility
Data management
All citations were downloaded into Mendeley, a free online citation manager (https://www.mendeley.com). Next, all sources were uploaded to the program Covidence (https://www.covidence.org). The duplicates were removed in the Covidence program.
Selection process
Two reviewers (NK, CM) independently screened all titles and abstracts using Covidence. A third reviewer (MB) resolved discrepancies between the two reviewers. In the next phase, full-text studies were procured and uploaded to Covidence by two reviewers (NK, JM). The two independent reviewers (NK, ES) assessed all full-text articles for inclusion and exclusion criteria (). Any disagreements between the two reviewers were resolved independently by a third reviewer (CM).
Data collection process
Once the final studies were selected, two reviewers (NK, ES) extracted all pertinent data. A third reviewer confirmed the accuracy of the extracted data by reviewing each full-text article.
Quality assessment and risk of bias assessment
The risk of bias in individual studies and the quality of studies were assessed with the PEDro scale (https://www.pedro.org.au/english/downloads/pedro-scale/) for any randomized controlled trials (RCTs) included. For the studies that were not RCTs, NIH quality assessment tools (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) and JBI tools (https://jbi.global/critical-appraisal-tools) were utilized according to the specific article type.
Data analysis/synthesis
For this review, two subgroupings were established based on comparison groups: healthy controls or sham treatment. Actual needling was compared to these two sub-groupings about their resultant fMRI findings. fMRI measures the Blood Oxygen Level Dependent (BOLD) signal which is an indirect measure of neuronal activity through changes in metabolic activity (Jenkinson, Chappell, and Okell, Citation2018). The smallest unit of measurement in functional MRI is a three-dimensional voxel, which includes thousands of neurons, firing actional potentials to communicate with one another. If a given cortical area plays a role in supporting cognitive operation, the firing of action potential leads to an increase in the consumption of oxygen in the brain region. It is this metabolic activity in the cortical region that results in an increase in blood supply to the brain resulting in greater oxygenated to deoxygenated blood, which then can be measured through fMRI. Brain imaging studies often involve the administration of cognitive, affective, or social tasks to capture the BOLD signal in regions that show an increase in metabolic activity in response to the task. Using traditional general linear modeling, these studies identify coordinates of brain regions that show an increase in activity following the task induction. Additionally, neuroimaging studies can also examine patterns of functional connectivity (i.e. temporal coherence between brain regions) either during task or rest using a wide variety of approaches such as: seed-based functional connectivity; identification of connectivity patterns in canonical networks using independent components analysis; or local connectivity patterns using regional homogeneity analyses (Smitha et al., Citation2017; Zang et al., Citation2004). For the studies included in the review, we identified specific coordinates of the regions of the brain that were significantly activated and reported the results in a conceptual figure as a dichotomous value of (+) or (-).
A meta-analysis of behavioral data such as reporting of pain was performed using Review Manager 5 (RevMan 5) software. Statistical heterogeneity was assessed with the I2 statistic and considered low if under 50% (Israel and Richter, Citation2011).
Results
Study selection
The database search yielded 16,909 studies. There was 95% agreement among reviewers during the screening phase and 75% agreement after the full-text review phase. Eight studies were ultimately included after an abstract and full-text review () with three studies investigating functional connectivity changes after acupuncture between individuals with LBP and healthy controls, and five studies investigating differences between real and sham acupuncture in individuals with LBP (). Included studies either used resting-state fMRI or task-based fMRI. All eight studies utilized acupuncture (). None of the studies used dry needling by a physical therapist, physician, chiropractor, or athletic trainer.
Table 2. Characteristics of included studies.
Quality and risk of bias assessment
The quality of randomized controlled trials and observational study designs ranged from good (n = 6) to excellent (n = 2), with a low risk of bias based on the JBI Risk of Bias Assessment for one article ().
Table 3. Methodological quality/risk of bias assessments.
Study characteristics
Seven of the eight studies selected were RCTs (Lee et al., Citation2019; Li et al., Citation2014; Makary et al., Citation2018; Tu et al., Citation2019; Xiang et al., Citation2021; Ye and Liu, Citation2012; Yu et al., Citation2020) and a prospective observational study (Liu et al., Citation2020). It is important to note that Lee et al. (Citation2019) and Makary et al. (Citation2018) came from the same clinical trial (registration #KCT0002253), and Tu et al. (Citation2019) and Yu et al. (Citation2020) came from the same clinical trial (registration # NCT01595451) thus resulting in a total of six independent clinical trials that have been conducted to evaluate the effect of needling therapies using fMRI.
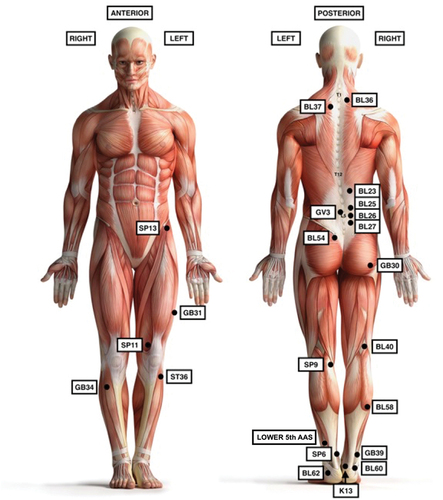
There was an overlap in acupuncture protocols, and types of LBP investigated. Three studies (37.5%) utilized acupuncture protocols that followed similar procedures (Lee et al., Citation2019; Sherman and Cherkin, Citation2003; Tu et al., Citation2019; Yu et al., Citation2020) (Appendix 1). Two studies used a different protocol addressing the following acupoints: Left stomach-36 (ST36); Left spleen-11 (SP11); and bilateral spleen-13(SP13) (Lee et al., Citation2019; Makary et al., Citation2018) (Appendix 2). The specific anatomical location of all needling interventions utilized can be found in . The duration of LBP ranged from acute (<1 month) (Ye and Liu, Citation2012) to chronic (up to 6 ± 4.1 years) (Tu et al., Citation2019) although most studies (n = 6) reported on chronic LBP (Li et al., Citation2014; Liu et al., Citation2020; Tu et al., Citation2019; Ye and Liu, Citation2012; Yu et al., Citation2020) ().
Low back pain neural response compared to healthy controls before needling
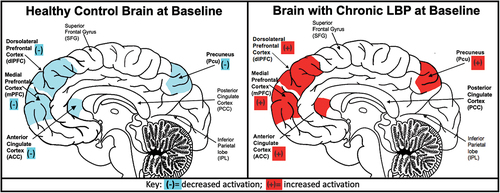
A few studies examined differences between individuals with LBP and healthy controls before acupuncture. Although these studies do not include the entire range of studies examining differences between individuals with LBP and healthy controls (Ng et al., Citation2018) data included in these acupuncture studies supports prior research highlighting notable differences between LBP individuals and controls. Specifically, within this literature, individuals with LBP were observed to have altered functional connectivity patterns compared to healthy controls as measured by resting state fMRI using analytic techniques such as regional homogeneity analyses that measures local functional connectivity and seed-based functional connectivity (Li et al., Citation2014; Liu et al., Citation2020) (). For example, Li et al. (Citation2014) examined network connectivity of the DMN in individuals with chronic LBP and found reduced connectivity in the dorsolateral PFC, the medial PFC, the anterior cingulate cortex, and the precuneus compared to healthy controls. Individuals with sciatica, however, demonstrated hyperconnectivity within the DMN (p < .05) (Liu et al., Citation2020). Specifically, Liu et al. (Citation2020) found evidence of increased connectivity between the posterior cingulate cortex (PCC) and bilateral insular cortices, inferior parietal lobes, cerebellum, the right orbitofrontal cortex, and left dorsal anterior cingulate cortex in individuals experiencing sciatica compared to healthy controls (p < .05) ().
Low back pain neural response compared to healthy controls after needling
Acupuncture significantly changed functional connectivity as measured by fMRI and reduced LBP as measured by the visual analogue scale (VAS) (p < .001) (Li et al., Citation2014; Liu et al., Citation2020). In contrast to notable differences in the DMN observed before acupuncture, after four weeks of acupuncture, Li et al. (Citation2014) reported no between-group differences in functional connectivity between those with LBP and healthy controls. These results suggest that the reduced connectivity of the DMN observed in individuals with LBP was altered through acupuncture with neural connectivity patterns in patients similar to that of controls following four weeks of needling therapy (Li et al., Citation2014). Moreover, Xiang et al. (Citation2021) noted similar brain responses across all five frequency bands to actual needling at the ankle in both healthy and chronic LBP patients within the DMN (i.e. increases in the medial PFC and decreases in the cerebellum, PCC, and parahippocampal gyrus). Similarly, individuals with sciatica after acupuncture treatment, twice a week for four weeks, demonstrated significantly reduced connectivity between the PCC-seeded functional connectivity and the right cerebellum, the left precuneus, and the dorsal medial PFC (p = .005) (Liu et al., Citation2020) ().
These changes in functional brain connectivity were accompanied by a significant self-reported reduction in pain as assessed through the VAS (mean ± SD = 5.42 ± 1.83 to 3.92 ± 1.83; p = .032) and a reduction in functional disability, as assessed through the Roland Disability Questionnaire for individuals with sciatica (mean ± SD 10.75 ± 4.85 to 7.17 ± 5.04 52.68; p = .036) (Liu et al., Citation2020). A minimal clinically important change on the VAS has been reported as 2 cm (Ostelo and de Vet, Citation2005). Xiang et al. (Citation2021) demonstrated multiple correlations between frequency-specific bands and pain-relief in VAS when slow-5 and slow-3 band frequency decreased in the cerebellum so did VAS scores after actual needling (r = 0.65, p = .003 and r = 0.48, p = .04), whereas norm-2 and slow-4 (r = −0.048, p = .04) frequency bands showed a negative correlation in the right insula to changes in the VAS after real ankle needling (). There were no changes reported in the Sciatica Bothersome Index or quality of life as measured by the World Health Organization Quality of Life (Liu et al., Citation2020). Importantly, changes in functional connectivity patterns were not correlated with gains in either pain ratings or functional disability (Liu et al., Citation2020). Overall, acupuncture appears to elicit more functional connectivity changes in both physical and cognitive/affective pain-processing regions.
Table 4. Summary of significant correlations between fMRI and pain rating.
Real and sham acupuncture altered different brain regions in individuals with low back pain
Six studies included real acupuncture and sham procedure (). Apart from Makary et al. (Citation2018) who used task-based fMRI where neural activation was measured during the needling procedure, the other studies (n = 5) measured functional connectivity using resting-state fMRI (Lee et al., Citation2019; Tu et al., Citation2019; Xiang et al., Citation2021; Ye and Liu, Citation2012; Yu et al., Citation2020).
There was significant heterogeneity in the comparison of real versus sham acupuncture. Real acupuncture was used for clinically relevant points for LBP in three studies (Tu et al., Citation2019; Ye and Liu, Citation2012; Yu et al. Citation2020). With participants lying supine, four acupuncture needles were inserted medial to the anterior superior iliac spine bilaterally, left anteromedial thigh, and left anterolateral proximal aspect of the lower leg near the tibial plateau (Lee et al., Citation2019; Makary et al., Citation2018), and the ankle (Xiang et al., Citation2021).
There was also variability in the sham procedures used. Two studies used a phantom acupuncture technique where the acupuncturist mimicked the protocol for inserting the needle but never pierced the skin (Lee et al., Citation2019; Makary et al., Citation2018). Similarly, Xiang et al. (Citation2021) held a needle to the skin for 5 s at the same acupuncture points as the real acupuncture phase of the study without inserting the needle. Tu et al. (Citation2019) and Yu et al. (Citation2020) from the same clinical trial inserted Streitberger placebo acupuncture needles into 12 sham acupuncture points, where the needle retracts into the shaft when it contacts the skin. Lastly, for Ye and Liu (Citation2012) a needle was inserted into a lumbago acupoint at the center of the forehead.
Only three studies used methods of blinding (Tu et al., Citation2019; Xiang et al., Citation2021; Yu et al., Citation2020). Tu et al. (Citation2019) and Yu et al. (Citation2020) published data from the same single-blinded clinical trial where patients and study staff were blinded to treatment groups, but the acupuncturists were not blinded. Xiang et al. (Citation2021) blinded participants with LBP and no back pain to the order they received ankle acupuncture stimulation and tactile sham acupuncture.
Overall, the majority of the studies (n = 4) found no difference in functional connectivity between real acupuncture and sham acupuncture groups (Lee et al., Citation2019; Tu et al., Citation2019; Xiang et al., Citation2021; Yu et al., Citation2020). Ye and Liu (Citation2012) found a statistical difference in functional connectivity between groups, and Makary et al. (Citation2018) found a statistical difference in neural activation. Even though there was conflicting evidence if there was a difference in functional connectivity among the studies, all of the studies (n = 6) found that acupuncture resulted in statistically significant lower pain as measured by the VAS when compared to sham needling (Lee et al., Citation2019; Makary et al., Citation2018; Tu et al., Citation2019; Xiang et al., Citation2021; Ye and Liu, Citation2012; Yu et al., Citation2020).
Meta-analysis
Meta-analysis of neuroimaging data was not possible due to the heterogeneity of methodology used in the included studies. However, meta-analysis was possible in three of the included studies that used the VAS. It was not possible in all studies due to VAS not being measured, and some of the included studies are from the same clinical trial.
In the meta-analysis when examining the standardized mean difference [−0.28], there appears to be potential for a small effect of acupuncture reducing LBP (). However, when examining the 95% confidence intervals [95% CI: −0.70, 0.13] the lower bound does cross “0,” which would be indicative of no effect of acupuncture reducing LBP. When interpreting all this information, there is evidence of no effect to potential small effect of acupuncture reducing LBP.
Figure 4. A meta-analysis demonstrated evidence of no effect to potential small effect of acupuncture in reducing low back pain.
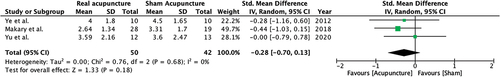
This should be analyzed with caution due to the narrow focus and confined sample used. Another reason we recommend caution is that the included studies have small sample sizes, which may be contributed to the high cost of using fMRI. The observation of no effect of acupuncture should be analyzed under the context of LBP acupuncture studies that used neuroimaging, and not the entirety of the acupuncture LBP literature.
Discussion
This review aimed to examine changes in functional brain organization in individuals with various types of LBP compared with healthy controls, and the subsequent impact of needling therapies on functional connectivity patterns. Overall, findings from this review suggest that individuals with LBP demonstrated significant alterations in functional connectivity in the nodes of the DMN before acupuncture. These changes are due to LBP, not due to being about to receive acupuncture. However, the application of acupuncture was associated with a reduction in between-group differences between patients and healthy controls. Moreover, across these studies, there was evidence linking changes in the functional organization of canonical networks following needling therapies with short-term changes in pain reduction.
There was conflicting evidence if brain connectivity patterns were significantly different between real and sham needling, but there was potential for a small effect of acupuncture to reduce LBP relative to sham based on the meta-analysis. A contributing factor to these results might be the significant variability in the methodology of sham acupuncture across studies, thus making it challenging to differentiate between the real versus placebo effects of acupuncture. This review highlights the need for future well-powered, rigorous studies investigating the effects of real acupuncture on connectivity patterns of the canonical networks of the brain.
Low back pain response to needling was altered compared to healthy controls
Acupuncture may normalize the brain activation patterns of individuals with LBP to that of the brain activation patterns of those without LBP. Patients with LBP demonstrated unique functional inter-network (within the DMN) and intra-network connectivity (PCC connectivity to other networks) compared to healthy controls before needling therapies. However, after needling treatments, those with LBP demonstrated inter- and intra-network connectivity patterns like healthy controls (Li et al., Citation2014; Liu et al., Citation2020; Xiang et al., Citation2021). The DMN is one of the most important central networks of the brain and is related to complex cognitive performance (Prakash et al., Citation2013). Within the DMN are nodes that span between the posterior cingulate cortex, medial temporal lobe, and medial prefrontal cortex (Prakash et al., Citation2013). Given the importance of the DMN in the human brain, it is interesting to observe that individuals with LBP have unique connectivity patterns compared to healthy controls and that acupuncture may alter this.
Change in functional connectivity resulting from needling therapies
There was an inverse correlation between inter-network normalization of DMN and pain reduction after needing and a positive correlation between intra-network changes and pain reduction (Li et al., Citation2014; Liu et al., Citation2020) (). Although there was variation in functional brain organization changes, evidence suggests a relationship between both inter-network and intra-network changes of the DMN, potentially resulting in decreased pain perception after acupuncture treatment for both patient populations (Li et al., Citation2014; Liu et al., Citation2020; Xiang et al., Citation2021). These studies support the use of traditional acupuncture for short-term clinical pain reduction in patients with LBP, CNS modulation on pain processing with network changes of the DMN (Li et al., Citation2014; Liu et al., Citation2020).
Comparing sham acupuncture to real acupuncture in patients with low back pain
There was significant variability in real and sham acupuncture techniques in the included studies. Four studies found no difference in functional connectivity (Lee et al., Citation2019; Tu et al., Citation2019; Xiang et al., Citation2021; Yu et al., Citation2020) between sham and real acupuncture. However, Ye and Liu (Citation2012) did find a difference in functional connectivity, and Makary et al. (Citation2018) found a statistical difference in neural activation. These conflicting results may be due to methodological differences, variability in the real and sham acupuncture, and lack of blinding.
The studies that investigated functional connectivity that was of higher methodological quality and had a better sham acupuncture technique demonstrated no difference between real and sham acupuncture (Lee et al., Citation2019; Tu et al., Citation2019; Xiang et al., Citation2021; Yu et al., Citation2020) compared to Ye and Liu (Citation2012) where the sham technique involved inserting an acupuncture needle into the middle of the forehead and did not involve any blinding procedures. Makary et al. (Citation2018) were from the same clinical trial as Lee et al. (Citation2019) where resting-state and task-based fMRI were performed. The analysis reported by Makary et al. (Citation2018) was from the task-based fMRI where neural activation was measured while acupuncture was performed and a significant difference in neural activation was reported between real acupuncture and phantom acupuncture.
It is difficult to understand the true effect of acupuncture since most acupuncture studies struggle to include blinding in their methods and fail to use a convincing sham acupuncture technique. A strong sham technique was utilized by Tu et al. (Citation2019) and Yu et al. (Citation2020) with the use of Streitberger placebo needles where the needle retracts once it touches the skin, giving the participant the sensation that they are in the real acupuncture group. Makary et al. (Citation2018) and Lee et al. (Citation2019) were from the same clinical trial and performed acupuncture and phantom acupuncture while the participant lay supine in the fMRI scanner. They chose acupoints on the front of the body since the participants were supine. This could be a limitation since these participants are complaining of LBP and would likely receive acupuncture to the low back while lying prone if seen clinically. Also, phantom acupuncture involved the acupuncturist going through the procedure but without a needle. Xiang et al. (Citation2021) did something similar, where they held a needle to the skin for 5 s but did not pierce it. The nature of acupuncture makes it impossible to blind the person performing the procedure, but stronger studies need to be developed that use single-blinded methods and convincing sham procedures to fully elucidate the effects acupuncture may have on the nervous and musculoskeletal systems. Interestingly even though most studies did not have a good sham technique, our meta-analysis of the pain data demonstrated evidence of only a small effect of acupuncture compared to sham at reducing LBP with the lower bound 95% confidence interval demonstrating evidence of no effect.
Overall, regardless of whether the individual received real or sham acupuncture, there was a significant increase in functional connectivity of the DMN (Lee et al., Citation2019; Tu et al., Citation2019; Xiang et al., Citation2021; Yu et al., Citation2020). Further research should examine potential patient bias and whether an individual’s expectation of acupuncture being beneficial would affect functional connectivity of the DMN, and if a positive expectation of acupuncture may have a significant enough effect to overcome between-group differences.
Study limitations
There are several limitations in this review to be considered. First, only studies in English were included, which may limit the scope of inclusion of the eastern medicine literature. Another systematic review was completed on acupuncture and LBP with a focus on searching PubMed and several Chinese databases, which yielded more articles due to the ability to include articles written in English and Chinese (Wen et al., Citation2021). This may highlight the importance of including studies that are written in Chinese if completing a review on acupuncture-based studies. Regardless, similar conclusions were met, and a generalized conclusion could not be reached due to the heterogeneity of included studies. Secondly, all the studies focused on traditional acupuncture treatments, and none utilized the western medicine concepts/technique of “dry needling.” Further, the acupuncture studies did not use the same treatment plan, time course, or even needle placement. Therefore, making any definitive recommendations were difficult due to the heterogeneity of the studies, which prohibited us from conducting a meta-analysis of the neuroimaging data. The meta-analysis performed should be interpreted with caution due to the narrow focus and confined sample used. Especially since this analysis was limited to acupuncture and neuroimaging studies. Other reviews with a broader focus have found dry needling and acupuncture to be beneficial in reducing LBP (Furlan et al., Citation2005).
Future research
Examining brain activation patterns and functional connectivity effects from acupuncture-type interventions may provide vital information when managing patients with LBP. More high-quality studies are needed to study the effects of needling therapies, precisely the western medicine technique of dry needling, on multiple conditions of LBP that control for the placebo effect. Although it is difficult to control for the placebo effect in acupuncture studies, consideration should be given to enhancing the blinding procedures of the participants and study personnel, the selection of sham needles, and the interaction between the participant and the needler to improve future study designs. Future research should follow these changes temporally to understand better how time since treatment may influence the CNS changes in these patients. Western medicine-based dry needling and physical therapy trials may consider replicating fMRI approaches of traditional acupuncture studies to identify if different needling therapies have similar or different central effects on the brain.
Conclusion
This limited evidence suggests that actual acupuncture treatment may alter the brain connectivity patterns of individuals with LBP to mimic that of healthy controls in the DMN. Evidence demonstrates that acupuncture elicits more functional connectivity changes in both physical and cognitive/affective pain-processing regions. In contrast, sham treatments alter functional connectivity mostly in cognitive/affective areas. Although the functional connectivity changes were different following real and sham acupuncture in most studies, both groups can correlate their respective pain-reduction to these alterations. Thus, it may be inferred that individuals with LBP will likely note pain reduction immediately after acupuncture, partly by the modulation of an individual’s pain perception at a CNS level.
Acknowledgments
We acknowledge Anna Bizsaha for consulting on the search strategy as part of her role as a librarian.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Apkarian AV, Bushnell MC, Treede RD, Zubieta JK 2005 Human brain mechanisms of pain perception and regulation in health and disease. European Journal of Pain 9: 463–484. doi:10.1016/j.ejpain.2004.11.001.
- Audette JF, Feng W, Howard S 2004 Bilateral activation of motor unit potentials with unilateral needle stimulation of active myofascial trigger points. American Journal of Physical Medicine and Rehabilitation 83: 368–374. doi:10.1097/01.PHM.0000118037.61143.7C.
- Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M 2013 Physiologic effects of dry needling topical collection on myofascial pain. Current Pain and Headache Reports 17: 348. doi:10.1007/s11916-013-0348-5.
- Chae Y, Chang DS, Lee SH, Jung WM, Lee IS, Jackson S, Kong J, Lee HH, Park HJ, Lee HH, et al. 2013 Inserting needles into the body: A meta-analysis of brain activity associated with acupuncture needle stimulation. Journal of Pain 14: 215–222. doi:10.1016/j.jpain.2012.11.011.
- Chenot JF, Greitemann B, Kladny B, Petzke F, Pfingsten M, Schorr SG 2017 Clinical practice guideline: Non-specific low back pain. Deutsches Arzteblatt International 114: 883–890. doi:10.3238/arztebl.2017.0883.
- Delitto A, George SZ, Van Dillen L, Whitman JM, Gwendolyn DS, Shekelle P, Denninger TR, Godges JJ, et al. 2012 Clinical guidelines low back pain recommendations. Journal of Orthopaedic and Sports Physical Therapy 42: A1–A57. doi:10.2519/jospt.2012.42.4.A1.
- Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T 2014 Dry needling: A literature review with implications for clinical practice guidelines. Physical Therapy Reviews 19: 252–265. doi:10.1179/108331913X13844245102034.
- Fang J, Jin Z, Wang Y, Li K, Kong J, Nixon EE, Zeng Y, Ren Y, Tong H, Wang Y, et al. 2009 The salient characteristics of the central effects of acupuncture needling: Limbic-paralimbic-neocortical network modulation. Human Brain Mapping 30: 1196–1206. doi:10.1002/hbm.20583.
- Furlan AD, van Tulder M, Cherkin D, Tsukayama H, Lao L, Koes BW, Berman B 2005 Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews 1: CD001351.
- García-Molina A 2012 Phineas Gage and the enigma of the prefrontal cortex. Neurología 27: 370–375. doi:10.1016/j.nrl.2010.07.015.
- Hides JA, Jull GA, Richardson CA 2001 Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine 26: E243–248. doi:10.1097/00007632-200106010-00004.
- Hui KK, Marina O, Claunch JD, Nixon EE, Fang J, Liu J, Li M, Napadow V, Vangel M, Makris N, et al. 2009 Acupuncture mobilizes the brain’s default mode and its anti-correlated network in healthy subjects. Brain Research 1287: 84–103. doi:10.1016/j.brainres.2009.06.061.
- Israel H, Richter RR 2011 A guide to understanding meta-analysis. Journal of Orthopaedic and Sports Physical Therapy 41: 496–504. doi:10.2519/jospt.2011.3333.
- Jenkinson M, Chappell M, Okell T 2018 Short introduction to MRI physics for neuroimaging. Oxord, UK: Oxford University Press.
- Konno S, Sekiguchi M 2018 Association between brain and low back pain. Journal of Orthopaedic Science 23: 3–7. doi:10.1016/j.jos.2017.11.007.
- Kregel J, Meeus M, Malfliet A, Dolphens M, Danneels L, Nijs J, Cagnie B 2015 Structural and functional brain abnormalities in chronic low back pain: A systematic review. Seminars in Arthritis and Rheumatism 45: 229–237. doi:10.1016/j.semarthrit.2015.05.002.
- Kropf E, Syan SK, Minuzzi L, Frey BN 2019 From anatomy to function: The role of the somato-sensory cortex in emotional regulation. Brazilian Journal of Psychiatry 41: 261–269. doi:10.1590/1516-4446-2018-0183.
- Kucyi A, Moayedi M, Weissman-Fogel I, Goldberg MB, Freeman BV, Tenenbaum HC, Davis KD 2014 Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. Journal of Neuroscience 34: 3969–3975. doi:10.1523/JNEUROSCI.5055-13.2014.
- Langevin HM 2021 Reconnecting the brain with the rest of the body in musculoskeletal pain research. Journal of Pain 22: 1–8. doi:10.1016/j.jpain.2020.02.006.
- Lee J, Eun S, Kim J, Lee JH, Park K 2019 Differential influence of acupuncture somatosensory and cognitive/affective components on functional brain connectivity and pain reduction during low back pain state. Frontiers in Neuroscience 13: 1062. doi:10.3389/fnins.2019.01062.
- Lin LL, Li HP, Yang JW, Hao XW, Yan SY, Wang LQ, Yu FT, Shi GX, Liu CZ 2020 Acupuncture for psychological disorders caused by chronic pain: A review and future directions. Frontiers in Neuroscience 14: 626497. doi:10.3389/fnins.2020.626497.
- Liu CH, Yeh TC, Kung YY, Tseng HP, Yang CJ, Hong TY, Cheng CM, Yang JL, Wu TP, Hsieh JC, et al. 2020 Changes in resting-state functional connectivity in nonacute sciatica with acupuncture modulation: A preliminary study. Brain and Behavior 10: e01494. doi:10.1002/brb3.1494.
- Li J, Zhang JH, Yi T, Tang WJ, Wang SW, Dong JC 2014 Acupuncture treatment of chronic low back pain reverses an abnormal brain default mode network in correlation with clinical pain relief. Acupuncture in Medicine 32: 102–108. doi:10.1136/acupmed-2013-010423.
- Makary MM, Lee J, Lee E, Eun S, Kim J, Jahng GH, Kim K, Youn YS, Lee JH, Park K 2018 Phantom acupuncture induces placebo credibility and vicarious sensations: A parallel fMRI study of low back pain patients. Scientific Reports 8: 930. doi:10.1038/s41598-017-18870-1.
- Miller EK, Cohen JD 2001 An integrative theory of prefrontal cortex function. Annual Review of Neuroscience 24: 167–202. doi:10.1146/annurev.neuro.24.1.167.
- Moher D, Liberati A, Tetzlaff J, Altman DG 2009 Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine 6: e1000097. doi:10.1371/journal.pmed.1000097.
- Ng SK, Urquhart DM, Fitzgerald PB, Cicuttini FM, Hussain SM, Fitzgibbon BM 2018 The relationship between structural and functional brain changes and altered emotion and cognition in chronic low back pain brain changes: A systematic review of MRI and fMRI studies. Clinical Journal of Pain 34: 237–261. doi:10.1097/AJP.0000000000000534.
- Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CW, Chenot JF, van Tulder M, Koes BW 2018 Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. European Spine Journal 27: 2791–2803. doi:10.1007/s00586-018-5673-2.
- Ostelo RW, de Vet HC 2005 Clinically important outcomes in low back pain. Clinical Rheumatology 19: 593–607. doi:10.1016/j.berh.2005.03.003.
- Otti A, Guendel H, Wohlschläger A, Zimmer C, Noll-Hussong M 2013 Frequency shifts in the anterior default mode network and the salience network in chronic pain disorder. BMC Psychiatry 13: 84. doi:10.1186/1471-244X-13-84.
- Ott T, Nieder A 2019 Dopamine and cognitive control in prefrontal cortex. Trends in Cognitive Sciences 23: 213–234.
- Prakash RS, De Leon AA, Klatt M, Malarkey W, Patterson B 2013 Mindfulness disposition and default-mode network connectivity in older adults. Social Cognitive and Affective Neuroscience 8: 112–117. doi:10.1093/scan/nss115.
- Sherman KJ, Cherkin DC 2003 Developing methods for acupuncture research: Rationale for and design of a pilot study evaluating the efficacy of acupuncture for chronic low back pain. Alternative Therapies in Health and Medicine 9: 54–60.
- Smitha KA, Akhil Raja K, Arun KM, Rajesh PG, Thomas B, Kapilamoorthy TR, Kesavadas C 2017 Resting state fMRI: A review on methods in resting state connectivity analysis and resting state networks. Neuroradiology Journal 30: 305–317. doi:10.1177/1971400917697342.
- Tamber-Rosenau BJ, Esterman M, Chiu YC, Yantis S 2011 Cortical mechanisms of cognitive control and shifting attention in vision and working memory. Journal of Cognitive Neuroscience 23: 2905–2919. doi:10.1162/jocn.2011.21608.
- Torrico TJ, Munakomi S 2021 Neuroanatomy, Thalamus. Treasure Island (FL): StatPearls Publishing.
- Tu Y, Ortiz A, Gollub RL, Cao J, Gerber J, Lang C, Park J, Wilson G, Shen W, Chan ST, et al. 2019 Multivariate resting-state functional connectivity predicts responses to real and sham acupuncture treatment in chronic low back pain. NeuroImage Clinical 23: 101885. doi:10.1016/j.nicl.2019.101885.
- Wen Q, Ma P, Dong X, Sun R, Lan L, Yin T, Qu Y, Liu Y, Xiao Q, Zeng F 2021 Neuroimaging studies of acupuncture on low back pain: A systematic review. Frontiers in Neuroscience 15: 730322. doi:10.3389/fnins.2021.730322.
- Xiang A, Chen M, Qin C, Rong J, Wang C, Shen X, Liu S 2021 Frequency-specific blood oxygen level dependent oscillations associated with pain relief from ankle acupuncture in patients with chronic low back pain. Frontiers in Neuroscience 15: 786490. doi:10.3389/fnins.2021.786490.
- Ye Y, Liu B 2012 Analgesic effects of balanced acupuncture versus body acupuncture in low-back and leg pain patients with lumbar disc herniation, as assessed by resting-state functional magnetic resonance imaging. Neural Regeneration Research 7: 1624–1629. doi:10.3969/j.1673-5374.2012.21.004.
- Yuan QL, Wang P, Liu L, Sun F, Cai YS, Wu WT, Ye ML, Ma JT, Xu BB, Zhang YG 2016 Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Scientific Reports 6: 30675. doi:10.1038/srep30675.
- Yu S, Ortiz A, Gollub RL, Wilson G, Gerber J, Park J, Huang Y, Shen W, Chan ST, Wasan AD, et al. 2020 Acupuncture treatment modulates the connectivity of key regions of the descending pain modulation and reward systems in patients with chronic low back pain. Journal of Clinical Medicine 9: 1719. doi:10.3390/jcm9061719.
- Zang Y, Jiang T, Lu Y, He Y, Tian L 2004 Regional homogeneity approach to fMRI data analysis. NeuroImage 22: 394–400. doi:10.1016/j.neuroimage.2003.12.030.
- Zhou K, Ma Y, Brogan MS 2015 Dry needling versus acupuncture: The ongoing debate. Acupuncture in Medicine 33: 485–490. doi:10.1136/acupmed-2015-010911.
Appendix
Appendix 1. Acupuncture treatment details for each individual study delineating total number of treatments, treatment length, the type of needles utilized, and how many needles were utilized, as well as where the needles were placed and with what technique.
Appendix 2.
This chart describes the anatomical location of each of the acupoints utilized in all seven studies, as well as providing their traditional Chinese names.