ABSTRACT
Objective
To evaluate the effect of neck-specific exercise (NSE) compared to prescribed physical activity (PPA) on headache and dizziness in individuals with cervical radiculopathy (CR). Also, to investigate associations between headache or dizziness and pain, neck muscle endurance (NME), neck mobility, physical activity, and fear avoidance beliefs.
Methods
Individuals randomized to either NSE or PPA were selected to a headache subgroup (n = 59) and/or a dizziness subgroup (n = 73). Data were evaluated, according to headache and/or dizziness outcomes at baseline and at 3, 6, and 12-month follow-ups.
Results
No significant between-group differences were found between NSE and PPA in either subgroup. In the headache subgroup, significant within-group improvements were seen at all follow-ups for NSE (p < .001) and from baseline to 3 (p = .037) and 12 (p = .003) months for PPA. For dizziness, significant within-group improvements were seen from baseline to 3 months for NSE (p = .021) and from baseline to 3 (p = .001) and 6 (p = .044) months for PPA. Multiple regression models showed significant associations at baseline between headache intensity and neck pain (adjusted R-square = 0.35, p < .001), and for dizziness with neck pain and dorsal NME (adjusted R-square = 0.34, p < .001).
Conclusion
NSE and PPA show similar improvements in headache intensity and dizziness in individuals with CR. Headache intensity is associated with neck pain, and dizziness with neck pain and dorsal NME, highlighting the importance of these factors when evaluating headache and dizziness.
Introduction
Cervical radiculopathy is commonly characterized by pain, sensory disturbance, and weakness in structures innervated by the affected nerve root (Woods and Hilibrand, Citation2015) as well as moderate levels of disability (Wong et al., Citation2014). The condition may also be associated with headache in approximately 50–67% of individuals (Anderberg et al., Citation2006; Persson and Carlsson, Citation1999) and with dizziness in approximately 50% of individuals (Karlberg, Persson, and Magnusson, Citation1995).
Headache with its origin in the neck is commonly classified as cervicogenic headache (Persson and Carlsson, Citation1999) and can lead to impaired quality of life and physical function (Biondi, Citation2005). Changes in one or more structures in the neck, such as the nerve roots, joints, discs, bone, muscles, ligaments (Sjaastad, Fredriksen, and Pfaffenrath, Citation1998) or referred pain from neck and shoulder muscles are some underlying causes of cervicogenic headache (Biondi, Citation2005; Persson and Carlsson, Citation1999). Another cause of headache in individuals with frequent neck pain is tension-type headache and migraine (Ashina et al., Citation2015). Tension-type headache is commonly associated with tenderness and trigger points in the cranio-cervical muscles. Referred pain from trigger points may lead to acute headache with ongoing conditions leading to sensitization of the central nervous system and chronification (Bendtsen and Fernández-de-la-Peñas, Citation2011). A common explanation for individuals with neck pain and headache is that afferent input from C1-C3 nerves and trigeminal nerve converge in the trigeminocervical nucleus. This means that pain signals from the neck can be referred to areas in the head innervated by trigeminal nerve and/or C1-C3 nerves, and vice versa, as primary headache conditions like tension-type headache or migraine have been reported with frequent neck pain as their most prevalent symptom (Becker, Citation2010; Bogduk and Govind, Citation2009; Luedtke, Starke, and May, Citation2018).
Dizziness in individuals with neck dysfunction, with other possible explanations for dizziness excluded, is classified as cervicogenic dizziness (Jung, Mathew, Littmann, and MacDonald, Citation2017; Reiley et al., Citation2017). The most common explanation for cervicogenic dizziness is impaired proprioceptive function (Hain, Citation2015) due to disruption of the afferent input from the cervical spine to the vestibular nucleus (Reiley et al., Citation2017) which could be caused by neck pain (Reiley et al., Citation2017; Röijezon, Clark, and Treleaven, Citation2015) and muscle fatigue (Röijezon, Clark, and Treleaven, Citation2015). The sub-occipital muscles have a particularly high density of muscle spindles that act as proprioceptors (Liu, Thornell, and Pedrosa-Domellöf, Citation2003). Neck pain (Henderson, Hennessy, Shuey, and Shackelford, Citation1983; Woods and Hilibrand, Citation2015) and weakness in the neck muscles are common among individuals with cervical radiculopathy (Halvorsen, Abbott, Peolsson, and Dedering, Citation2014) and might be potential triggers for both headache and dizziness.
Physiotherapy including manual therapy and low-load endurance exercise may decrease the frequency and intensity of cervicogenic headache (Jull et al., Citation2002). Upper cervical manipulation in combination with neck-specific exercise for individuals with tension-type headache and neck pain can reduce headache frequency, severity, duration, and improve headache disability (Corum, Aydin, Medin Ceylan, and Kesiktas, Citation2021). Manual therapy, in combination with stretching, can increase the cervical pressure pain threshold and enhance patient satisfaction in individuals with migraine and associated headache (Bevilaqua-Grossi et al., Citation2016). In individuals with cervicogenic dizziness, the frequency and intensity of dizziness have been reported to decrease with physiotherapy, relaxation exercises, stabilization exercise (Karlberg et al., Citation1996), and manual therapy (Reid, Rivett, Katekar, and Callister, Citation2014).
Previous research has shown that neck-specific exercise targeting deep neck muscles, cognitive behavioral approach, and – to some extent – physical activity may be beneficial for reducing pain in individuals with chronic pain conditions including neck pain (Eccleston, Morley, and Williams, Citation2015; Geneen et al., Citation2017; Gross et al., Citation2015). However, there is currently a lack of studies investigating the effects of neck-specific exercise with a cognitive behavioral approach and prescribed physical activity on headache and dizziness in individuals with cervical radiculopathy. We believe that both neck-specific exercises and prescribed physical activity affect pain, which could potentially influence headache and dizziness. The aim was to evaluate the effect of neck-specific exercise compared to prescribed physical activity on headache and dizziness in individuals with cervical radiculopathy. We also investigated associations between headache or dizziness and pain, neck muscle endurance, neck mobility, physical activity, and fear avoidance beliefs.
Methods
This study consists of secondary analyses of a randomized clinical trial (RCT) including individuals with cervical radiculopathy (Dedering et al., Citation2018). These analyses focused on the intervention effects on participants’ headache and/or dizziness complaints during the trial. Two subgroups based on headache and dizziness at baseline were followed over the course of 12 months. The study has been approved by the Regional Board of Ethics in Stockholm (Dnr 2009/1756-31/4) and conducted in accordance with the Declaration of Helsinki. The RCT study protocol is published (Dedering et al., Citation2014) and registered at ClinicalTrials.gov (NCT01831271).
Participants
Individuals were recruited between October 2010 and November 2012 from a neurosurgery department in Stockholm, Sweden. All individuals had cervical radiculopathy and were referred to the clinic for a neurosurgeon to evaluate whether surgical intervention was an appropriate treatment. A total of 160 individuals who did not meet the criteria for surgery or were denied surgery were referred to a physiotherapist, test-leader, to undergo a standardized clinical assessment including a medical history and to be screened for inclusion and exclusion criteria (). Of these, 144 individuals met the criteria for participating and gave their informed consent to participate in the original trial (Dedering et al., Citation2018).
Table 1. Inclusion and exclusion criteria.
Individuals were randomized to either neck-specific exercise or prescribed physical activity by the principal investigator who did not perform any tests or interventions in the study. A computer-randomized table created by a statistician was used for randomization, and the allocation ratio was 1:1 in blocks of eight (Dedering et al., Citation2018).
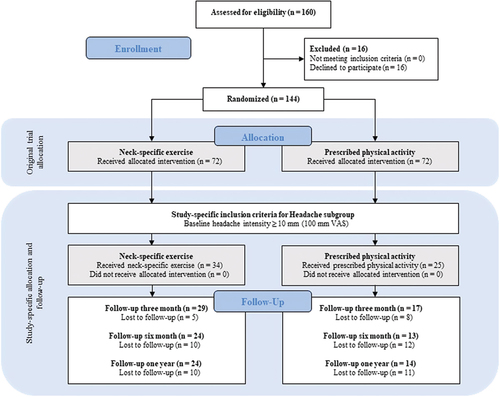
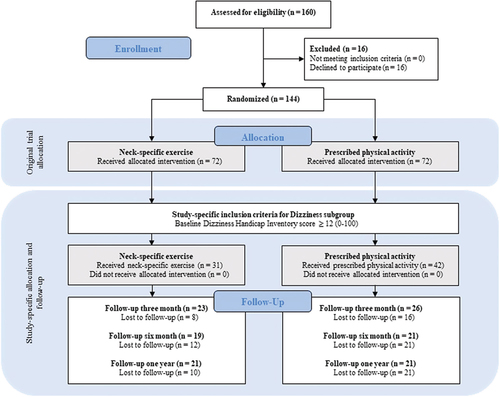
For analyses of headache and dizziness, we created two separate subgroups from the 144 included individuals in the original trial. For the headache subgroup, we included all individuals (n = 59) with a baseline headache intensity of ≥ 10 mm on a 0–100 mm visual analog scale (VAS) (), and for the dizziness subgroup we included all individuals (n = 73) with a Dizziness Handicap Inventory score ≥ 12 on a 0–100 score at baseline (). As some individuals suffered from both conditions, based on study-specific criteria for each subgroup, a total of 44 individuals were included in both subgroups.
Interventions
The intervention period in both groups was three months, and a cognitive behavioral approach was included in both interventions – continuous for the neck-specific exercise intervention, but only during the first session for the prescribed physical activity intervention. The treating physiotherapists were located in primary care, and received written standardized information and oral information by phone from the test-leader. Participants received standardized information and exercise diaries to document the training (Dedering et al., Citation2018). If necessary, participants in both groups received standard medication for cervical radiculopathy during the intervention period, and after the intervention ended they were free to receive other treatments.
Neck-specific exercise
The intervention consisted of neck-specific exercise with a cognitive behavioral approach, aiming to improve sensorimotor function, neck muscle strength, and neck muscle endurance, and to reduce pain (Dedering et al., Citation2018). The exercises started with isolated low-load sensorimotor exercises and progressed to endurance exercises (Landén-Ludvigsson, Peolsson, and Peterson, Citation2015). The participants met with the treating physiotherapist three times per week, and the exercise dosage was progressed individually within a predetermined standardized protocol. In addition to the physiotherapy visits, participants received a home-exercise program for daily execution (Dedering et al., Citation2018).
The cognitive behavioral approach began with an initial motivational interview and continued weekly with information on and guidance in physiology of pain, stress, breathing, relaxation, coping, pacing, and ergonomics (Dedering et al., Citation2018).
Based on the participant’s symptoms, vestibular rehabilitation was included in the neck-specific exercise, aiming to reduce dizziness and improve balance. Vestibular rehabilitation consisted of voluntary eye movements and fixation, and neck and body movements when lying down, sitting, standing, and walking.
Prescribed physical activity
Participants in the prescribed physical activity group received a tailored written prescription of an individual physical activity, based on the initial patient-centered counseling session, as well as a general prescription of physical activity to perform on their own. The goal of the intervention was to reduce pain and improve general health. The individual physical activity consisted of a recommendation of an aerobic and/or muscular physical activity or training, and the general prescription consisted of at least 30 minutes of physical activity at moderate intensity three times per week (Dedering et al., Citation2018). The written prescription of physical activity followed the guidelines from the National Institute for Public Health in Sweden (Statens Folkhälsoinstitut, Citation2011) and could consist of bicycling, walking, and running, for example. In addition to the initial session with a treating physiotherapist, participants had the opportunity to contact a physiotherapist within primary health care if any questions arose (Dedering et al., Citation2018). The cognitive behavioral approach consisted of one motivational interview, including an evaluation of current health state, history of physical activity, potential risk factors, assessment of motivation, readiness to change and need for support for physical activity (Dedering et al., Citation2018).
Data collection
Data were collected at baseline and at 3, 6, and 12-month follow-ups, including questions regarding sociodemographic variables, patient-reported outcomes, and clinical tests. All clinical tests of physical function were performed at a university hospital by the test-leader, who was blinded for randomization at baseline but not at follow-ups. Background characteristics and baseline variables included gender, age, frequency of headaches or dizziness, headache intensity, neck pain intensity, fear avoidance beliefs, physical activity, neck muscle endurance, active cervical range of motion, and in the dizziness subgroup the Dizziness Handicap Inventory ().
Table 2. Background characteristics and baseline variables for study participants.
Primary outcomes
The primary outcome in the headache subgroup was headache intensity measured on a VAS (0–100 mm), with the endpoints 0 (no pain) and 100 (worst possible pain). The VAS is a valid scale with good test-retest reliability for acute pain (intraclass correlation coefficients; ICC = 0.97–0.99) (Williamson and Hoggart, Citation2005) and good test-retest reliability (ICC = 0.85) for chronic pain (Lundeberg et al., Citation2001). The median minimum clinically important difference in chronic pain is 23 mm, and differs between clinical conditions (Olsen et al., Citation2018). There is no stated minimum clinically important difference for headache, but for individuals with cervical spine disorder it is 4.6–21.4 mm when evaluating neck pain (MacDowall, Skeppholm, Robinson, and Olerud, Citation2018).
The primary outcome in the dizziness subgroup was dizziness measured using the Dizziness Handicap Inventory, which is a self-rated 25-item questionnaire developed to evaluate the self-perceived impact on daily life regarding dizziness (Jacobson and Newman, Citation1990). The Dizziness Handicap Inventory is the most used self-perceived questionnaire for measuring dizziness (Mutlu, Serbetcioglu, and Cohen, Citation2013) and all questions can be answered in three ways: 1) yes (4 points); 2) sometimes (2 points); or 3) no (0 points) (Jacobson and Newman,Citation1990). The minimum score is 0 (no handicap), and the maximum score is 100 points (total handicap). Reference values for the Dizziness Handicap Inventory are: ≤ 30 = mild disability; 31 to 60 = moderate disability; and > 60 = severe disability (Whitney, Wrisley, Brown, and Furman, Citation2004). The original version has shown a high test-retest reliability (r = 0.97) (Jacobson and Newman, Citation1990) and the test-retest reliability (k = 0.63) and content validity for the Swedish version are good (Jarlsäter and Mattsson, Citation2003). The minimally important change for the Dizziness Handicap Inventory (Norwegian version) is 11 points (Tamber, Wilhelmsen, and Strand, Citation2009).
Secondary outcomes
Neck pain intensity was rated using the VAS (Williamson and Hoggart, Citation2005). Ventral neck muscle endurance was tested with the participants lying on a plinth in a supine position, and the dorsal neck muscle endurance was tested lying in prone position with a weight (2 kg for women and 4 kg for men) hanging from the participant’s head just above the ears. Neck muscle endurance was measured in seconds, and the test started with the participant lifting their head off the table. The test ended for one of three reasons: 1) the participant released their head back to the table; 2) was unable to sustain a good head position; or 3) experienced increasing radiating pain (Peolsson et al., Citation2007a). Dorsal neck muscle endurance test has shown good inter-rater reliability for healthy individuals (ICC 0.80) and individuals with neck disorders (ICC 0.94), and the intra-rater reliability are good (ICC 0.90) for both groups (Peolsson et al., Citation2007b). The ventral neck muscle endurance test has acceptable inter-rater reliability (ICC 0.57–1.0) and intra-rater reliability (ICC 0.76–0.96) (de Koning Ch et al., Citation2008b).
The active cervical range of motion was measured in the sagittal, transverse, and frontal planes, and was recorded in degrees using a cervical range of motion instrument (Performance Attainment Associates, Lindstrom, MN). The cervical range of motion instrument has shown good inter-rater reliability (ICC > 0.70) and intra-rater reliability (ICC > 0.85). The construct validity is positive (r > 0.65) (de Koning Ch et al., Citation2008a).
Physical activity was measured using two questions, one regarding active physical exercise (A = no activity to E = activities or competitions such as running or ball sports with regularity) and one regarding everyday physical activity (A = no everyday activity to D = almost daily or daily activity) in a typical week during the last 12 months. The answers were combined and converted to a 1–4-point score: 1 = inactivity; 2 = low activity; 3 = moderate activity; and 4 = high activity). The procedure has been used in the previous research to evaluate physical activity (Peolsson et al., Citation2007a).
Patients’ fear avoidance beliefs about how physical activity and work may affect their neck pain was measured using the Fear-Avoidance Beliefs Questionnaire (0–96, where 0 indicates no fear). The instrument consists of 16 questions, and each question can be answered with 0 (completely disagree) to 6 (completely agree) (Waddell et al., Citation1993). The test-rest reliability for the Swedish version is “moderate” to “good” (weighted Kappa 0.68), and the instrument can discriminate between healthy individuals and individuals with cervical radiculopathy (Dedering and Börjesson, Citation2013).
Blinding
The test-leader and the participants were blinded to the intervention at baseline. After baseline, neither test-leader, the participants, nor the treating physiotherapists were blinded. Data were entered by an independent individual who was blinded to the intervention, and all analyses were performed by an independent researcher who was not involved in data collection or randomization.
Statistical analysis
Sample size calculations were carried out for the original RCT and were based on data from the Swedish neck study. To detect a group mean difference of 15 mm for VAS, assuming a standard deviation of 28, an alpha level of 5%, and statistical power of 80%, each group required 56 individuals (Dedering et al., Citation2014).
Descriptive data are presented for numbers, percent, and mean and standard deviation. Within-group and between-group differences of neck-specific exercise and prescribed physical activity for primary outcomes were analyzed in each subgroup using a linear mixed model with restricted maximum likelihood estimates and the assumption of unstructured covariance structure. This model was used to include all available data at each time point. The results are presented as numbers, means, 95% confidence intervals (CI), Cohen’s D (d) and p-values.
Initial simple linear regression analyses were used to assess associations at baseline between each independent variables (i.e. headache subgroup: neck pain intensity, neck muscle endurance, active cervical range of motion, physical activity, and fear avoidance beliefs; dizziness subgroup: neck pain intensity, headache intensity, neck muscle endurance, active cervical range of motion, physical activity, and fear avoidance beliefs) and each dependent variables (i.e. headache intensity and Dizziness Handicap Inventory score) in each subgroup. A final multiple linear regression with a forward approach was conducted for each subgroup. All statistical assumptions for multiple regression were met and natural logarithm transformation was used on independent variables with skewed distribution. The results are presented as number, R-square, beta-coefficient, 95% CI, standardized beta coefficient, p-value, and in the multiple regression adjusted R-square. In all analyses, the significance level was set at p < .05 and IBM SPSS Statistics for Windows (Version 26.0, Armonk, NY: IBM Corp) was used.
Results
Of the 144 individuals in the original trial, 88 met the study-specific inclusion criteria (). Of these, 59 reported headache intensity of 10 or more and were included in the headache subgroup analyses, and 73 reported dizziness scores of 12 or more and were included in the dizziness subgroup analyses. Forty-four individuals were included in both subgroups which means that approximately 75% in the headache subgroup and 60% in the dizziness subgroup were suffering from both headache and dizziness based on the study-specific criteria. This also means, of all 88 individuals who met the study-specific criteria, 15 only had headache and 29 only had dizziness.
In the headache subgroup, 34 individuals were randomized to neck-specific exercise and 25 to prescribed physical activity (). In the dizziness subgroup, 31 individuals were randomized to neck-specific exercise and 42 to prescribed physical activity (). Of all possible observations in the linear mixed model analyses without any dropouts at each time point, there were 82% with neck-specific exercise and 69% with prescribed physical activity in the headache subgroup, and 84% with neck-specific exercise and 65% with prescribed physical activity in the dizziness subgroup. The most frequently given reasons for loss to follow-up were lack of interest or time, and no unintended effects or harm were reported for the interventions.
Effect on headache intensity and factors associated with headache intensity
There were no significant between-group differences in headache intensity at any time points (p > .05). However, headache intensity improved significantly within the neck-specific exercise intervention group from baseline to all follow-ups (p < .001) with a medium effect size (d = 0.641–0.754), and in the prescribed physical activity intervention group from baseline to 3 (p = .037, d = 0.338) and 12 months (p = .003, d = 0.473) with a small effect size (Sawilowsky, Citation2009) (). Of all available participants at each time point, more participants achieved the minimum clinically important difference of 23 mm in VAS (100 mm) in the neck-specific exercise intervention group (3-month, n = 11, 38%; 6-month, n = 11, 46%; 12-month, n = 11, 46%) compared with the prescribed physical activity intervention group (3-month, n = 5, 29%; 6-month, n = 2, 15%; 12-month, n = 6, 43%) at all follow-ups. There was no significant difference between the proportions of individuals who achieved minimum clinically important difference in each intervention group at any time point (p > .05).
Table 3. Change in headache intensity and Dizziness Handicap Inventory score from baseline to each time point; 3, 6, and 12 months (maximum likelihood estimates from linear mixed models with unstructured covariance structure).
Headache intensity at baseline was significantly associated with neck pain intensity (p < .001), active cervical range of motion sagittal plane (p = .013), and transverse plane (p = .027). Neck pain intensity (p < .001) was the only significant associated variable in the final multiple regression model, which explained 35% (adjusted R-square = 0.35) of the headache intensity variability at baseline ().
Table 4. Associations between pain, neck muscle endurance, neck mobility, physical activity, and fear avoidance beliefs with headache intensity at baseline.
Effect on dizziness and factors associated with dizziness
There were no significant between-group differences in the Dizziness Handicap Inventory score at any time points (p > .05), but the Dizziness Handicap Inventory showed significant within-group improvements in both neck-specific exercise intervention group (p = .021, d = 0.319) and prescribed physical activity intervention group (p = .001, d = 0.464) from baseline to 3 months with a small effect size (Sawilowsky, Citation2009). For the prescribed physical activity intervention group, a significant within-group improvement was found between baseline and six months (p = .044, d = 0.275) with a small effect size. No other significant changes could be seen in either intervention group (p > .05) (). Of all available participants at each time point, more participants achieved the minimum clinically important difference of 11 points in Dizziness Handicap Inventory score in the prescribed physical activity intervention group (3-month, n = 11, 42%; 6-month, n = 10, 48%; 12-month, n = 9, 43%) compared with neck-specific exercise intervention group (3-month, n = 9, 39%; 6-month; n = 6, 32%; 12-month, n = 5, 24%) at all follow-ups. There was no significant difference between the proportions of individuals who achieved minimum clinically important difference in each intervention group at any time point (p > .05).
The Dizziness Handicap Inventory score at baseline was significantly associated with neck pain intensity (p < .001), headache intensity (p < .001), neck muscle endurance ventral (p = .035) and dorsal (p < .001), active cervical range of motion (sagittal, frontal, and transverse plane) (p ≤ .007), and Fear-Avoidance Beliefs Questionnaire (p < .001). Neck pain (p < .001) and dorsal neck muscle endurance (p = .004) were the only significant associated variables in the final multiple regression model, which explained 34% (adjusted R-square = 0.34) of Dizziness Handicap Inventory variability at baseline ().
Table 5. Associations between pain, neck muscle endurance, neck mobility, physical activity, and fear avoidance beliefs with Dizziness Handicap Inventory score at baseline.
Discussion
The between-group analyses did not show any significant differences between neck-specific exercise and prescribed physical activity. Headache intensity significantly reduced over time in both neck-specific exercise and prescribed physical activity . Dizziness significantly improved in both neck-specific exercise and prescribed physical activity from baseline to 3 months and from baseline to 6 months in prescribed physical activity . This suggests that both interventions can be used for individuals with cervical radiculopathy who have headache or dizziness.
The neck-specific exercise training was individually progressed within a predetermined standardized protocol, and the intervention was designed to improve sensorimotor function, neck muscle strength, and neck muscle endurance, and to reduce pain. However, if the neck-specific exercises were better tailored to the patient’s individual needs, a greater improvement with neck-specific exercise may possibly be found.
The minimum clinically important difference in VAS for individuals with chronic pain is 23 mm (Olsen et al, Citation2018), and more participants achieved 23 mm in the neck-specific exercise intervention group compared with prescribed physical activity at all follow-ups. This means that more individuals in the neck-specific exercise intervention group experienced a meaningful difference compared with prescribed physical activity in the headache subgroup. In the dizziness subgroup it was the opposite, more individuals experienced a meaningful difference with prescribed physical activity. However, there was no significant difference between the proportions of individuals who achieved minimum clinically important difference in each intervention group at any time point in either subgroup.
Headache intensity could be explained by neck pain intensity, which has been observed in previous research (Svensson et al., Citation2020) and strengthens the explanation that referred neck pain can lead to headache (Bendtsen and Fernández-de-la-Peñas, Citation2011; Biondi, Citation2005; Persson and Carlsson, Citation1999). In contrast, some studies showed that neck pain can be a symptom of specific headache condition (Al-Khazali et al., Citation2022; Ashina et al., Citation2015). We could not exclude that individuals in this study had neck pain as a symptom of a specific headache condition. However, we know that all individuals in this study had magnetic resonance imaging (MRI) verified cervical disc disease showing cervical nerve root compression, as well as neck and/or arm pain verified with a neck extension test or a neurodynamic provocation test and have undergone a standardized clinical assessment including a medical history to verify their cervical radiculopathy.
In relation to headache intensity, dizziness could be explained by neck pain intensity but also by dorsal neck muscle endurance. Endurance has been shown to be an important function to consider in the rehabilitation of individuals with cervical radiculopathy (Halvorsen, Abbott, Peolsson, and Å, Citation2014). Cervicogenic dizziness can be explained by altered afferent input from the high number of muscle spindles present in the cervical spine (Liu, Thornell, and Pedrosa-Domellöf, Citation2003), by neck pain (Reiley et al., Citation2017; Röijezon, Clark, and Treleaven, Citation2015), and by muscle fatigue (Röijezon, Clark, and Treleaven, Citation2015). Previous research has shown that some physiotherapeutic interventions can reduce both dizziness and neck pain in individuals with dizziness of cervical origin (Karlberg et al., Citation1996). Our findings together with those from previous studies corroborate the notion that we can positively influence dizziness in individuals with cervical radiculopathy through interventions that reduce neck pain and increase neck muscle endurance.
The current paper supports findings of the original RCT (Dedering et al., Citation2018) that showed similar results for neck-specific exercise and prescribed physical activity, but with support from this paper we believe that reducing pain is an important part, at least in terms of affecting headache and dizziness. The findings are generalizable to the selected population.
Even if the original RCT showed no significant difference between neck-specific exercise and prescribed physical activity in the primary outcome neck and arm pain (VAS), one can explore post-priori if between-group difference can be found for individuals with cervical radiculopathy and headache or dizziness. The aim of the neck-specific exercise intervention was to improve sensorimotor function, neck muscle strength, and neck muscle endurance, and thereby to reduce headache and dizziness. For the prescribed physical activity, the aim of the intervention was to increase the physical activity, promote endogenous analgesia and thereby reduce headache and dizziness. The additional treatment with cognitive behavioral approach was aimed to handle stress and pain to reduce muscle tension and thereby reduce headache and dizziness. With the knowledge that neck pain (Henderson, Hennessy, Shuey, and Shackelford, Citation1983; Woods and Hilibrand, Citation2015) and weakness in the neck muscles are common among individuals with cervical radiculopathy (Halvorsen, Abbott, Peolsson, and Å, Citation2014) and are potential triggers for headache and dizziness (Bendtsen and Fernández-de-la-Peñas, Citation2011; Reiley et al., Citation2017; Röijezon, Clark, and Treleaven, Citation2015) we suspected that these interventions could have a better effect for individuals with headache and dizziness than those with only cervical radiculopathy.
Study limitations
The dropout rate, especially in the headache subgroup for prescribed physical activity, may affect the generalizability of the results. To deal with dropouts, we chose a linear mixed model with restricted maximum likelihood estimates in order to include all available data at each time point. Despite the dropouts, this study is unique as there are no earlier publications within the same area.
Two subgroups were created based on baseline values for headache intensity (≥ 10 mm on a 100 mm visual analog scale) and Dizziness Handicap Inventory score (≥ 12 on a 0–100 score), and the values were chosen based on the idea of including all individuals with headache and dizziness. This may be a limitation, as low baseline values make it more difficult to detect differences. However, the mean values for headache intensity at baseline were 52 (SD 26) in the headache subgroup and 40 (SD 21) for the Dizziness Handicap Inventory in the dizziness subgroup.
Another limitation of the present study is that the included individuals were not evaluated for specific headache and dizziness conditions such as cervicogenic headache, tension-type headache, migraine or cervicogenic dizziness. However, a strength is that we only included individuals with MRI-verified disc disease, which means that all individuals have structural changes of the cervical spine. The lack of proven structural changes is a common shortcoming in other studies evaluating individuals with cervical radiculopathy and headache or dizziness.
In the present study, we did not compare neck-specific exercise and prescribed physical activity with the natural course. From an ethical aspect, all individuals received an intervention because all individuals sought care. Therefore, it is still unknown whether neck-specific exercise and prescribed physical activity are more effective than the natural course. Despite this, both interventions can be considered ethical to use, because no adverse events were reported.
Conclusion
Neck-specific exercise and prescribed physical activity show similar improvements in headache intensity and dizziness in individuals with cervical radiculopathy. Headache intensity is associated with neck pain, and dizziness with neck pain and dorsal neck muscle endurance, highlighting the importance of these factors when evaluating headache and dizziness.
Acknowledgments
The authors acknowledge all participants and physiotherapists who participated in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Al-Khazali HM, Younis S, Al-Sayegh Z, Ashina S, Ashina M, Schytz HW 2022 Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia 42: 663–673. 10.1177/03331024211068073.
- Anderberg L, Annertz M, Rydholm U, Brandt L, Säveland H 2006 Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. European Spine Journal 15: 794–801. 10.1007/s00586-005-0931-5.
- Ashina S, Bendtsen L, Lyngberg AC, Lipton RB, Hajiyeva N, Jensen R 2015 Prevalence of neck pain in migraine and tension-type headache: A population study. Cephalalgia 35: 211–219. 10.1177/0333102414535110.
- Becker WJ 2010 Cervicogenic headache: Evidence that the neck is a pain generator. Headache 50: 699–705. 10.1111/j.1526-4610.2010.01648.x.
- Bendtsen L, Fernández-de-la-Peñas C 2011 The role of muscles in tension-type headache. Current Pain and Headache Reports 15: 451–458. 10.1007/s11916-011-0216-0.
- Bevilaqua-Grossi D, Gonçalves MC, Carvalho GF, Florencio LL, Dach F, Speciali JG, Bigal ME, Chaves T 2016 Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 97: 866–874. 10.1016/j.apmr.2015.12.006.
- Biondi DM 2005 Cervicogenic headache: A review of diagnostic and treatment strategies. Journal of the American Osteopathic Association 105: 16–22.
- Bogduk N, Govind J 2009 Cervicogenic headache: An assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurology 8: 959–968. 10.1016/S1474-4422(09)70209-1.
- Corum M, Aydin T, Medin Ceylan C, Kesiktas FN 2021 The comparative effects of spinal manipulation, myofascial release and exercise in tension-type headache patients with neck pain: A randomized controlled trial. Complementary Therapies in Clinical Practice 43: 101319. 10.1016/j.ctcp.2021.101319.
- Dedering Å, Börjesson T 2013 Assessing fear-avoidance beliefs in patients with cervical radiculopathy. Physiotherapy Research International 18: 193–202. 10.1002/pri.1545.
- Dedering Å, Halvorsen M, Cleland J, Svensson M, Peolsson A 2014 Neck-specific training with a cognitive behavioral approach compared with prescribed physical activity in patients with cervical radiculopathy: A protocol of a prospective randomized clinical trial. BMC Musculoskeletal Disorders 15: 274. 10.1186/1471-2474-15-274.
- Dedering Å, Peolsson A, Cleland JA, Halvorsen M, Svensson MA, Kierkegaard M 2018 The effects of neck-specific training versus prescribed physical activity on pain and disability in patients with cervical radiculopathy: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 99: 2447–2456. 10.1016/j.apmr.2018.06.008.
- de Koning Ch, van den Heuvel Sp, Staal J, Smits-Engelsman BC, Hendriks EJ, de Koning CH, Heuvel SPVD 2008b Clinimetric evaluation of methods to measure muscle functioning in patients with non-specific neck pain: A systematic review. BMC Musculoskeletal Disorder 19: 142. 10.1186/1471-2474-9-142.
- de Koning Ch, van den Heuvel Sp, Staal J, Smits-Engelsman BCM, Hendriks EJM, de Koning BC, van den Heuvel EJ 2008a Clinimetric evaluation of active range of motion measures in patients with non-specific neck pain: A systematic review. European Spine Journal 17: 905–921. 10.1007/s00586-008-0656-3.
- Eccleston C, Morley SJ, Williams AC 2015 Psychological approaches to chronic pain manage-ment: Evidence and challenges. British Journal of Anaesthesia 111: 59–63. 10.1093/bja/aet207.
- Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH 2017 Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 4: CD011279.
- Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, Christie T, Dupont G, Graham N, Burnie SJ, Gelley G, et al. 2015 Exercises for mechanical neck disorders. Cochrane Database of Systematic Reviews 1: CD004250. 10.1002/14651858.CD004250.pub5.
- Hain TC 2015 Cervicogenic causes of vertigo. Current Opinion in Neurology 28: 69–73. 10.1097/WCO.0000000000000161.
- Halvorsen M, Abbott A, Peolsson A, Dedering Å 2014 Endurance and fatigue characteristics in the neck muscles during sub-maximal isometric test in patients with cervical radiculopathy. European Spine Journal 23: 590–598. 10.1007/s00586-013-3060-6.
- Henderson CM, Hennessy RG, Shuey HM, Shackelford EG 1983 Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: A review of 846 consecutively operated cases. Neurosurgery 13: 504–512. 10.1227/00006123-198311000-00004.
- Jacobson GP, Newman CW 1990 The development of the dizziness handicap inventory. Archives of Otolaryngology – Head and Neck Surgery 116: 424–427. 10.1001/archotol.1990.01870040046011.
- Jarlsäter S, Mattsson E 2003 Test of reliability of the dizziness handicap inventory and the activities-specific balance confidence scale for use in Sweden. Advances in Physiotherapy 5: 137–144. 10.1080/14038190310004385.
- Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, Emberson J, Marschner I, Richardson C 2002 A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 27: 1845–1943. 10.1097/00007632-200209010-00004.
- Jung FC, Mathew S, Littmann AE, MacDonald CW linical decision making in the management of patients with cervicogenic dizziness: A case series. Journal of Orthopaedic and Sports Physical Therapy 47: 874–884. 10.2519/jospt.2017.7425.
- Karlberg M, Magnussen M, Malmstrom EM, Melander A, Moritz U 1996 Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Archives of Physical Medicine and Rehabilitation 77: 874–882. 10.1016/S0003-9993(96)90273-7.
- Karlberg M, Persson L, Magnusson M 1995 Impaired postural control in patients with cervico-brachial pain. Acta oto-laryngologica. Supplementum 520 Pt 2: 440–442.
- Landén-Ludvigsson M, Peolsson A, Peterson G 2015 Neck-specific exercise program. http://diva-portal.org/smash/record.jsf?aq=%5B%5B%5D%5D&aq2=%5B%5B%5D%5D&sf=all&aqe=%5B%5D&af=%5B%5D&searchType=LIST_LATEST&sortOrder=author_sort_asc&onlyFullText=false&noOfRows=50&language=sv&pid=diva2%3A785214&dswid=−4742.
- Liu JX, Thornell LE, Pedrosa-Domellöf F 2003 Muscle spindles in the deep muscles of the human neck: A morphological and immunocytochemical study. Journal of Histochemistry and Cytochemistry 51: 175–186. 10.1177/002215540305100206.
- Luedtke K, Starke W, May A 2018 Musculoskeletal dysfunction in migraine patients. Cephalalgia 38: 865–875. 10.1177/0333102417716934.
- Lundeberg T, Lund I, Dahlin L, Borg E, Gustafsson C, Sandin L, Rosén A, Kowalski J, Eriksson SV 2001 Reliability and responsiveness of three different pain assessments. Journal of Rehabilitation Medicine 33: 279–283. 10.1080/165019701753236473.
- MacDowall A, Skeppholm M, Robinson Y, Olerud C 2018 Validation of the visual analog scale in the cervical spine. Journal of Neurosurgery. Spine 28: 227–235.
- Mutlu B, Serbetcioglu B, Cohen H 2013 Discussion of the Dizziness Handicap Inventory. Journal of Vestibular Research 23: 271–277. 10.3233/VES-130488.
- Olsen MF, Bjerre E, Hansen MD, Tendal B, Hilden J, Hróbjartsson A 2018 Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: Systematic review of empirical studies. Journal of Clinical Epidemiology 101: 87–106. 10.1016/j.jclinepi.2018.05.007.
- Peolsson A, Almkvist C, Dahlberg C, Lindqvist PS, Pettersson S 2007a Age and sex-specific reference values of a test of neck muscle endurance. Journal of Manipulative and Physiological Therapeutics 30: 171–177. 10.1016/j.jmpt.2007.01.008.
- Peolsson A, Hamp C, Albinsson AK, Engdahl S, Kvist J 2007b Test position and reliability in measurements of dorsal neck muscle endurance. Advances in Physiotherapy 9: 181–189. 10.1080/14038190701702058.
- Persson LC, Carlsson JY 1999 Headache in patients with neck–shoulder–arm pain of cervical radicular origin. Headache 39: 218–224. 10.1046/j.1526-4610.1999.3903218.x.
- Reid SA, Rivett DA, Katekar MG, Callister R 2014 Comparison of Mulligan sustained natural apophyseal glides and Maitland mobilizations for treatment of cervicogenic dizziness: A randomized controlled trial. Physical Therapy 94: 466–476. 10.2522/ptj.20120483.
- Reiley AS, Vickory FM, Funderburg SE, Cesario RA, Clendaniel RA 2017 How to diagnose cervicogenic dizziness. Archives of Physiotherapy 7: 12. 10.1186/s40945-017-0040-x.
- Röijezon U, Clark NC, Treleaven J 2015 Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Therapy 20: 368–377. 10.1016/j.math.2015.01.008.
- Sawilowsky S 2009 New effect size rules of thumb. Journal of Modern Applied Statistical Methods 8: 597–599. 10.22237/jmasm/1257035100.
- Sjaastad O, Fredriksen TA, Pfaffenrath V 1998 Cervicogenic headache: Diagnostic criteria. The Cervicogenic Headache International Study Group. Headache 38: 442–445. 10.1046/j.1526-4610.1998.3806442.x.
- Statens Folkhälsoinstitut 2011 FaR: individanpassad skriftlig ordination av fysisk aktivitet [The Swedish public health institute 2011 Prescribed physical activity: individualized written prescription of physical activity]. Stockholm, Sweden: Östersund. https://nllplus.se/upload/IB/lg/fhc/FaR/R-2011-30-FaR-individanpassad-skriftlig-ordination-av-fysisk-aktivitet.pdf
- Svensson J, Hermansen A, Wibault J, Löfgren H, Dedering Å, Öberg B, Zsigmond P, Peolsson A 2020 Neck-related headache in patients with cervical disc disease after surgery and physio-therapy: A 1-year follow-up of a prospective randomized study. Spine 45: 952–959.
- Tamber AL, Wilhelmsen KT, Strand LI 2009 Measurement properties of the dizziness handicap inventory by cross-sectional and longitudinal designs. Health and Quality of Life Outcomes 7: 101. 10.1186/1477-7525-7-101.
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ 1993 A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52: 157–168. 10.1016/0304-3959(93)90127-B.
- Whitney SL, Wrisley DM, Brown KE, Furman JM 2004 Is perception of handicap related to functional performance in persons with vestibular dysfunction? Otology and Neurotology 25: 139–143. 10.1097/00129492-200403000-00010.
- Williamson A, Hoggart B 2005 Pain: A review of three commonly used pain rating scales. Journal of Clinical Nursing 14: 798–804. 10.1111/j.1365-2702.2005.01121.x.
- Wong JJ, Cote P, Quesnele JJ, Stern PJ, Silvano AM 2014 The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: A systematic review of the literature. The Spine Journal 14: 1781–1789. 10.1016/j.spinee.2014.02.032.
- Woods BI, Hilibrand AS 2015 Cervical radiculopathy epidemiology, etiology, diagnosis, and treatment. Journal of Spinal Disorders and Techniques 28: 251–259. 10.1097/BSD.0000000000000284.