ABSTRACT
Background
Falls are a leading cause of severe injury and death in older adults. Remote screening of fall risk may prevent falls and hence, advance health and wellness of older adults. While remote health care is becoming a common practice, we question if remote evaluation of fall risk is as reliable as face-to-face (FTF).
Objective
To assess the inter-tester reliability of synchronized remote and FTF fall risk assessment.
Methods
This inter-format, inter-rater reliability study included 48 home dwelling older adults aged 65 and over. Five valid functional and balance tests were conducted: 30 Second Sit-to-Stand (STS), MiniBESTest, Timed up and go (TUG), 4-Meter Walk (4MWT), and Berg Balance Scale (BBS). Instructions were provided via videoconferencing, and two physiotherapists scored performance simultaneously, one remotely, and one in the room. Inter-rater reliability between remote and FTF scores was analyzed using intraclass correlation coefficient (ICC2,1), standard error of measurement (SEM), minimal detectable change (MDC95) and Bland and Altman analysis.
Results
Excellent ICCs were found for STS, MiniBESTest, TUG, and BBS (0.90–0.99), and moderate for 4MWT (0.74). SEM and MDC95 values were STS (0.37,1.03 repetitions), MiniBESTest (1.43,3.97 scores), TUG (1.22,3.37 seconds), 4MWT (0.17,0.47 m/second), and BBS (1.79,4.95 scores). The Bland and Altman analysis showed excellent agreement between remote and FTF assessments of the STS. All other tests showed low to moderate agreement. Mean difference ± SD and 95%LOA were as follows: STS (−0.11 ± 0.52), (−1.13,0.91) repetitions, MiniBESTest (0.45 ± 1.98), (−3.43,4.32) scores, TUG (−0.35 ± 1.54), (−3.37,2.67) seconds, 4MWT (−0.08 ± 0.22), (−0.35,0.51) meter/second, and BBS (0.04 ± 2.53), (−4.93,5.01) scores.
Conclusions
The findings support the responsible integration of remote fall risk assessment in clinical practice, enabling large-scale screenings and referrals for early intervention to promote healthy aging and fall prevention.
Introduction
Over the past few years, older adults have shown significant improvements in their ability to control and access communication technologies (Elimelech et al., Citation2022). Specifically, remote health care has seen a significant rise among this population (Choi, DiNitto, Marti, and Choi, Citation2022). This presents a notable opportunity to address one of the most pressing challenges faced by aging individuals: the high incidence of falls. With the aging of world population, falls are anticipated to become increasingly prevalent, underscoring the urgency for proactive measures (Salari et al., Citation2022). Early and comprehensive screening of older adults for fall risks, coupled with prompt referrals for intervention, can markedly mitigate the frequency of falls (Avin et al., Citation2015; Montero-Odasso et al., Citation2021; Sherrington et al., Citation2019).
Fall risk assessments include tests of postural stability, functional strength, and walking ability as well as fall history intake (Avin et al., Citation2015). Existing assessment tests, e.g. Timed Up and Go (TUG), 30 Second Sit-to-Stand (STS), and Berg Balance Scale (BBS), were designed as face-to-face (FTF) procedures; however, many older adult individuals find it difficult to reach health care facilities due to limited mobility and other accessibility issues (Park, Citation2018). One method for addressing this, which has recently accelerated, is remote health care (Madhavan et al., Citation2022; Senderovich and Wignarajah, Citation2022). Remote physical assessments have been studied in various formats including synchronously via videoconferencing, or asynchronously through scoring prerecorded assessments (Buckinx et al., Citation2024; Cabana et al., Citation2010; Pelicioni, Waters, Still, and Hale, Citation2022; Peyrusqué et al., Citation2022).
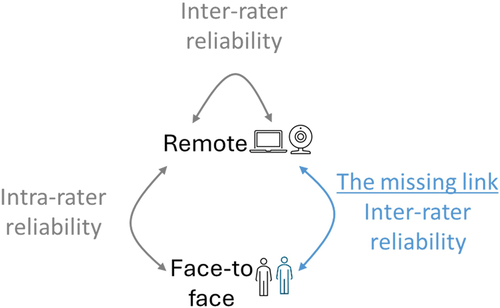
Reliability of remote fall risk assessment for home dwelling older adults has shown promising results (Buckinx et al., Citation2024; Pelicioni, Waters, Still, and Hale, Citation2022) but has not been completed (Madhavan et al., Citation2022) (). Remote synchronous assessment via videoconference compared to FTF showed very high intra-rater reliability (ICC >0.9) for several functional and balance tests (Buckinx et al., Citation2024) and good intra-rater reliability (ICC = 0.79–0.87) in another study (Pelicioni, Waters, Still, and Hale, Citation2022). Remote asynchronously prerecorded assessments compared to FTF, also showed good intra-rater reliability (ICC = 0.78–0.88) (Pelicioni, Waters, Still, and Hale, Citation2022).
Inter-rater reliability study of remote assessments via videoconference compared results by two assessors on two separate occasions and showed high reliability across all tests (ICC >0.9) (Buckinx et al., Citation2024). Another inter-rater study compared two assessors’ scorings of prerecorded tests and showed excellent reliability (ICC = 0.80–1.00) (Pelicioni, Waters, Still, and Hale, Citation2022). Furthermore, the inter-rater reliability between assessors on prerecorded assessments was shown to be higher than the intra-rater reliability of two assessments by the same assessor (Pelicioni, Waters, Still, and Hale, Citation2022). The researchers hypothesized that in scoring a prerecorded test, the assessor may concentrate on scoring the performance with attention to details without the need to interact with the individual assessed (Pelicioni, Waters, Still, and Hale, Citation2022).
One of the main limitations of repeated assessments is that they are performed on different occasions. Indeed, the performance of the subjects was found to improve over the previous performance for most tests, possibly due to practice and learning effects (Buckinx et al., Citation2024; Pelicioni, Waters, Still, and Hale, Citation2022). Therefore, performing remote assessment and FTF assessment in a simultaneous format may contribute to understand the reliability between formats without the effect of repeated assessments. A simultaneous scoring between assessors can adequately address the learning and fatigue effect bias of repeated assessments.
In summary, the remote assessment exhibits strong intra-rater reliability compared to FTF, and it also demonstrates high inter-rater reliability when comparing remote to remote. The inter-rater reliability of FTF assessment has long been established (Lima, Ricci, Nogueira, and Perracini, Citation2018; Marques et al., Citation2016; Rydwik, Bergland, Forsén, and Frändin, Citation2011; Shumway-Cook, Brauer, and Woollacott, Citation2000). Therefore, the missing link in reliability research of fall risk assessment, is the inter-rater reliability of remote assessments compared to FTF in a simultaneous assessment, which has yet to be determined (see ). This is the focus of our study. In this study, we investigate the reliability of five widely used fall risk assessment tests (STS, MiniBESTest, TUG, 4MWT, and BBS) using remote videoconferencing, comparing scoring to FTF raters, who assessed simultaneously, in a single clinical session.
Methods
Study design
This study was designed as a cross-section, inter-format and inter-tester reliability study, and was reported according to the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) (Kottner et al., Citation2011). The study was approved by the Ethics committee at the University of Haifa (#264/21).
Participants
The study population included home-dwelling older adults, aged 65 years and over, able to walk independently (with or without an assistive device). Exclusion criteria included more than two falls in the past year, inability to participate in physical assessment due to musculoskeletal disorder, or unstable cardiac or pulmonary disease. The presence of these conditions was based on self-report. The Centers for Disease Control and Prevention (CDC) STEADI fall risk screening algorithm, was used to determine fall risk, i.e., answering “yes” to any one of the three questions (falls in the past year, feeling unsteady when standing or walking, and worrying about falling) (Mielenz et al., Citation2020). Recruitment was performed during spring 2021 by publishing announcements in the social media of local municipalities, encouraging potential participants to undergo a battery of evidence-based functional and balance tests along with a cognitive assessment. A telephone interview was conducted with respondents to determine their eligibility.
Rater population
The assessors were two experienced and certified physiotherapists. The research team was assisted by five graduate students as part of their final research project. The research team underwent 4 hours of training including acquiring skills to perform the experimental procedure.
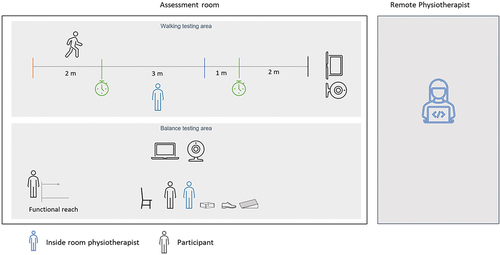
Procedure
Eligible participants were invited to attend the assessment hall, where they provided informed consent and underwent cognitive assessment. Subsequently, fall risk assessments were administered remotely, via videoconference in the following order: STS, MiniBESTest, TUG, 4MWT, and BBS. To optimize efficiency and minimize participant burden, tasks appearing in multiple assessments were performed only once and scored for each relevant test. Two assessors evaluated the subject’s performance. The remote assessor was positioned outside the room and in addition to scoring, provided the instructions for the tests from afar using the Zoom™ video communication platform. Concurrently, another assessor, the FTF assessor, was positioned in the room, next to the participant, and simultaneously scored the participant’s performance. The FTF assessor in the room refrained from communicating with the participant, to ensure test instruction was completely remote. The FTF assessor’s presence in the room also ensured participants’ safety. The physical testing procedure took 40 min. Each assessor was blinded to the other assessor’s rating. shows a schematic diagram of the assessing setup.
Figure 2. Testing setup of concurrent assessments in remote and face-to-face.
Outcome measures
Subjects were administered a cognitive assessment using the Montreal Cognitive Assessment score (MoCA), licensed (Julayanont and Nasreddine, Citation2017; Pinto et al., Citation2019) and then the following standard and validated functional and balance tests:
Thirty second Sit to Stand Test (STS) – counts the number of sit-to-stand transitions completed in 30 s. Threshold values indicating risk of fall are dependent on age and gender (Centers for Disease Control and Prevention, Citation2017).
Mini Balance Evaluation Systems Tests (MiniBESTest) – a 14 item balance test, scored from 0 to 28 points. A score of 20 points or below indicates a high fall risk (Marques et al., Citation2016).
Timed Up and Go Test (TUG) – measures the time required for a subject to stand up from sitting on a chair, walk for 3 m, turn, walk back, and sit down. Twelve seconds or more indicate risk of fall (Shumway-Cook, Brauer, and Woollacott, Citation2000).
Four Meter Walk Test (4MWT) – measures comfortable walking speed in meters per second (m/s). Speed lower than 1.00 m/s is considered a strong predictor of future falls (Kyrdalen, Thingstad, Sandvik, and Ormstad, Citation2019).
Berg Balance Scale (BBS) – a 14 item test, scored from 0 to 56 points. A score under 45 indicates risk of fall for older adults (Lima, Ricci, Nogueira, and Perracini, Citation2018).
Statistical analysis
Sample size calculation followed the recommendations by Walter et al. for reliability studies (Walter, Eliasziw, and Donner, Citation1998). This calculation considered two factors: achieving an inter-rater reliability of at least 0.80, indicating good agreement between FTF and remote assessments, and ensuring a minimum acceptable reliability of 0.60, which reflects a moderate level of chance agreement. Using these parameters (P0 = 0.60, P1 = 0.80, alpha = 0.05, and power = 0.80) in the Walter et al. formula, we calculated a sample size of 40.
To determine inter-rater reliability between FTF and remote assessment, we used a two-way mixed effects, absolute agreement, single measurement model for intraclass correlation coefficient calculations (ICC2,1). The level of consistency was interpreted by the following classification: ICC < 0.50 small, ICC = 0.50–0.75 moderate, ICC = 0.75–0.89 good, ICC = 0.90–1.00 excellent (Portney and Watkins, Citation2009). For absolute inter-rater reliability, we calculated the standard error of measurement [SEM= √(mean square error)] and the minimal detectable change (MDC95= SEM * 1.96*√2) (Bland and Altman, Citation1996).
The Bland and Altman (B&A) method was used to assess agreement between remote and FTF raters (Bland and Altman, Citation1986). Calculations included the mean difference between measures (mean∆=Remote-FTF) a 95% confidence interval (CI) for the mean difference, as well as the standard deviation of the differences (SD∆) and the 95% limits of agreement (LOA). Diagrams were plotted to illustrate the difference between remote and FTF assessments against the mean of the two measurements. The mean difference estimates the bias; if the line of equality (zero) is within the confidence interval of the mean difference, the bias is considered insignificant. The 95% LOA (computed as the mean difference ± 1.96 times the SD) indicates the likely difference between the two measures for most individuals. A priori limits of maximum acceptable differences were defined, based on previously reported MDC95 of each test, to estimate the agreement interval. For TUG and 4MWT MDC95 was calculated based on reported SEM. The limits were set at 1.15 repetitions for STS, 3.8 scores for MiniBESTest, 2.69 s for TUG, 0.28 m/s for 4MWT, and 5 scores for BBS (Beauchamp et al., Citation2021; Bhattacharya, Deka, and Roy, Citation2016; Donoghue and Stokes, Citation2009; Marques et al., Citation2016). If the 95% LOA exceeded the predefined LOA, the remote assessment cannot be supported as reliable (Bland and Altman, Citation1986; Giavarina, Citation2015). The association between the five functional and balance tests in each format (remote and FTF) was evaluated using Pearson correlation coefficient. This combination of statistical methods (ICC2,1 and B&A) in addition to correlation estimations among the five tests, was used in accordance with current recommendation for reliability studies (Lexell and Downham, Citation2005; Rankin and Stokes, Citation1998).
Results
Fifty-six adults were recruited from a local community, of whom eight declined to participate. The remaining 48 participants aged 65–86 years (mean 72.50 ± 4.66) were included in the study. The majority were females (68.75%), and 64.58% were at risk of fall according to the STEADI fall risk screening. describes the characteristics of the study’s population. The majority of participants were in their 70s, 3 participants (6.25%) used walking aid and 77.08% reported no falls in the past year.
Table 1. Characteristics of the study population.
Our reliability results are presented below in three parts – relative (ICC2,1) and absolute (SEM and MDC95) reliability results, B&A plots, and between-tests correlations. presents the relative and absolute reliability results (ICC2,1, SEM and MDC95) for the remote vs. FTF scores in each of the five physical assessments. ICC2,1 results show excellent correlation in the STS, MiniBESTest, TUG, and BBS (0.90–0.99), and only moderate ICC2,1 is shown in the 4MWT (0.74).
Table 2. Physical test results measured in remote and face-to-face settings, and their interclass correlation (N = 48).
Bland and Altman plots are presented in . shows that there is an excellent level of agreement between remote and FTF in STS results, as the zero-line lays within the CI of the mean difference, implying an insignificant bias. The predefined LOA of ± 1.15 (Bhattacharya, Deka, and Roy, Citation2016) is wider than the 95% LOA (−1.13, 0.91), indicating that 100% of subjects fall within the predefined acceptable differences.
Figure 3. Bland and Altman plots.
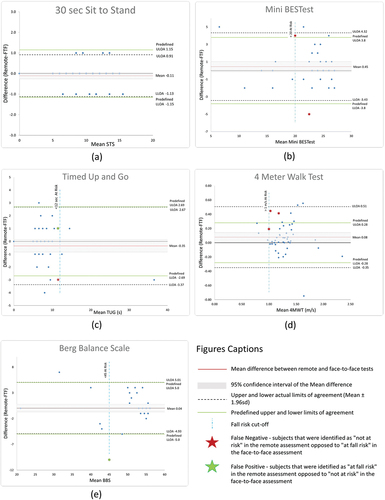
The MiniBESTest () shows a moderate level of agreement with the zero-line lays within the CI of the mean difference. The predefined lower LOA (−3.8) (Marques et al., Citation2016) is wider than the 95% lower LOA, however the predefined upper LOA (+3.8) is narrower than the 95% upper LOA. Eighty-nine percent of subjects fall within the predefined acceptable differences. According to the fall risk cutoff of 20 (Marques et al., Citation2016), two subjects, marked by a red star were “not at risk” in the remote assessment opposed to “at fall risk” in the FTF assessment (i.e., false negative).
TUG () shows a moderate level of agreement with the zero-line lays within the CI of the mean difference. The predefined lower LOA (−2.69) (Beauchamp et al., Citation2021) is narrower than the 95% lower LOA (−3.37), while the predefined upper LOA (2.69) is nearly identical to the 95% upper LOA (2.67). Eighty-six percent of subjects fall within the predefined acceptable differences. According to the fall risk cutoff of 12 s (Shumway-Cook, Brauer, and Woollacott, Citation2000), one subject, marked by a green star, was “at fall risk” in the remote assessment opposed to “not at risk” in the FTF assessment (i.e., false positive). Additionally, one subject, marked by a red star was “not at risk” in the remote assessment opposed to “at fall risk” in the FTF assessment (i.e., false negative).
Four Meter Walk Test (4MWT) () shows disagreement in all B&A parameters. The zero line is outside the CI of the mean difference, the predefined LOA (±0.28) (Beauchamp et al., Citation2021) is narrower than the 95% LOA (−0.35, 0.51) and includes 83% of the subjects. There is a systematic bias of overestimating the remote assessment compared to FTF. Moreover, according to the fall risk cutoff of 1 m/s (Kyrdalen, Thingstad, Sandvik, and Ormstad, Citation2019), three subjects were “not at risk” in the remote assessment opposed to “at fall risk” in the FTF assessment (i.e., false negative).
BBS () shows a good level of agreement with the zero-line lays within the CI of the mean difference and the predefined LOA (±5.00) (Donoghue and Stokes, Citation2009) is nearly similar to the 95% LOA (−4.93, 5.01). Ninety-six percent of subjects fall within the predefined acceptable differences. However, according to the fall risk cutoff of 45, one subject, marked by a green star, was “at fall risk” in the remote assessment opposed to “not at risk” in the FTF assessment (i.e., false positive).
The Pearson correlation across the five physical tests showed no statistical difference between the FTF correlation results and the remote correlation results. Therefore, only the correlation results are presented for the remote assessments in . All five tests were significantly correlated, with correlation coefficients ranging from 0.41 to 0.85. The highest correlation was between MiniBESTest and BBS which have common components, namely, the single-leg stance, sit to stand, and standing with eyes closed.
Table 3. Pearson Correlation results (r) between the five tests administered in the remote format (N = 48).
Discussion
This study provides evidence to support the reliability of remote fall risk assessment, as a step toward responsible clinical implementation in fall prevention. It will enable the possibility of large-scale screenings for risk of fall and consequently, referral to early intervention if necessary. Excellent reliability was found between FTF and remote assessments in four tests: STS, MiniBESTest, TUG, and BBS with ICC2,1 ranging from 0.90 to 0.99. Our results are consistent with prior reliability studies that compared FTF and remote assessments, establishing a good level of reliability, supporting the clinical application of remote fall risk assessment (Buckinx et al., Citation2024; Pelicioni, Waters, Still, and Hale, Citation2022; Peyrusqué et al., Citation2022). Our results for STS, TUG, and BBS (ICC2,1 = 0.99, 0.94, 0.93 respectively) align with prior studies on a different population comparing inter-rater reliability of FTF and remote assessments among 15 patients who underwent total knee arthroplasty: STS (Krippendorff’s α = 0.85), TUG (Krippendorff’s α = 0.86), and BBS (Krippendorff’s α = 0.76) (Cabana et al., Citation2010). Our results on inter-rater reliability, also align with intra-rater reliability among 15 older community dwelling adults: STS (ICC = 0.97) and TUG (ICC = 0.83) (Peyrusqué et al., Citation2022). We found the BBS to be reliable according to ICC2,1 and B&A results and feasible for remote assessment as was demonstrated by Venkataraman et al., (Citation2017). Nevertheless, previous and current findings indicate that the BBS suffers from a ceiling effect in home dwelling older adults, which limits its clinical applicability (Balasubramanian, Citation2015; Lima, Ricci, Nogueira, and Perracini, Citation2018). A few of the MiniBESTest items that were tested, are in fact not feasible to be performed remotely in a home setting. The reactive postural control tasks require physical contact between therapist and patient, which is not applicable remotely. Additional tasks in the MiniBESTest required space and special equipment unavailable in many homes (e.g., sponge pad, wedge, boxes). Finally, despite its high reliability according to ICC2,1 and B&A, two participants (4.17%) were misdiagnosed remotely as “not at risk” (i.e., false negative). The TUG test also showed excellent reliability (ICC2,1 = 0.94) but had a moderate level of agreement in B&A. In addition, one participant was misdiagnosed remotely as “not at risk” (false negative). The 4MWT demonstrated the lowest inter-rater reliability with ICC2,1 of 0.74, which is similar to Peyrusque et al’s intra rater remote assessment results (ICC = 0.77) (Peyrusqué et al., Citation2022), and lower than the results of Unver et al’s assessment of the FTF (ICC = 0.94) (Unver et al., Citation2017). The low reliability of the 4MWT which is also seen in the B&A results, may be explained by the inaccurate remote timing method. Timing was measured remotely using a manual timer, pressed at the start and end of the walk, when the subject steps on/over the markers on the floor. The direction of view and perspective distortions of the camera may have affected the remote visual estimate of when the subject’s feet align with the floor markings. However, assessing walking speed was recommended as an important indicator of fall risk, with reports that a slower walking speed increases falls risk (Espy, Yang, Bhatt, and Pai, Citation2010). Therefore, we recommend future studies to use automated devices to measure walking duration without relying on human response time, distraction, and remote distortions. Automated measurement applications for this purpose were already used successfully (Brooks et al., Citation2015; Gaspar and Lapão, Citation2021). The STS proved to be the most reliable test, showing excellent reliability by both B&A and ICC2,1 (0.99). STS is brief, easy, and requires no special equipment, making it ideal for home use. It provides a quantitative measure without a ceiling effect. Previous studies confirm STS as a strong predictor of recurrent falls in older adults (Buatois et al., Citation2010; Lin et al., Citation2022). A recent review by Madhavan et al. also recommended STS (Citation2022). Given these findings, STS is the preferred choice for remote fall risk assessment due to its simplicity, reliability, and ability to assess balance, strength, and power.
The MDC95 values of the physical tests in our study are aligned with previously reported values, excluding 4MWT. The current MDC95 values for STS, MiniBESTest, TUG, and BBS were 1.03 repetitions, 3.97 scores, 3.37 s, and 4.95 scores, and the previous were 1.15 repetitions, 3.8 scores, 2.69 s, and 5.0 scores, respectively, in older adults for the same tests (Beauchamp et al., Citation2021; Bhattacharya, Deka, and Roy, Citation2016; Donoghue and Stokes, Citation2009; Marques et al., Citation2016). However, the MDC95 values for 4MWT in our study (0.47 m/s) are higher than the MDC95 of 0.28 m/s, reported in another study of older adults (Beauchamp et al., Citation2021). These disparities may be attributed to the limitations identified in the method we employed for remotely measuring walking speed. Additionally, as MDC95 values from inter-rater reliability studies for the TUG, BBS, and 4MWT in community dwelling older adults were unavailable, we have presented previously reported MDC95 values from test–retest studies, acknowledging this limitation (Beauchamp et al., Citation2021; Donoghue and Stokes, Citation2009). Further research on inter-rater reliability is warranted to strengthen our MDC95 evidence.
While our study was conducted in a controlled environment, future research should replicate this approach in older adults’ homes to fully utilize remote assessments. The growing use of video conferencing technologies such as Zoom makes home-based assessments increasingly feasible. A remote pre-assessment of participants’ home environment, cameras, and stable internet connection can ensure safety and address setup challenges.
Conclusion
Our findings demonstrate the promise of remote fall risk assessment in older adults. Both the STS, TUG, and BBS tests achieved excellent reliability (ICC ≥0.93), suggesting their effective implementation in clinical practice. The BBS, however, showed a ceiling effect, limiting its usefulness for community-dwelling older adults. The STS test emerged as a standout for remote assessment. Its simplicity, requiring no equipment or specific space, and its maintained reliability in a remote setting make it a highly practical and accessible option for clinicians performing large-scale screenings. Early detection of fall risk through remote assessments, combined with prompt physical therapy referrals, has the potential to significantly reduce falls, improve quality of life and independence in older adults, and ultimately promote healthy aging.
Acknowledgments
The authors thank the following physiotherapists for their contribution in data collection: Zaharov Yulia, Ravicovich Leon, Pinsky Gali, Pisante Yaara, and Livshitz Nili. We also thank Nadav Eichler for his technical support, Dana Hadar for her statistical advice, and Naor Demeter for her writing review and editing assistance. Our sincere thanks goes out to the pensioners’ club in Kerem Maharal for their hospitality and participation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Avin KG, Hanke TA, Kirk-Sanchez N, McDonough CM, Shubert TE, Hardage J, Hartley G 2015 Management of falls in community-dwelling older adults: clinical guidance statement from the academy of geriatric physical therapy of the American physical therapy association. Physical Therapy 95: 815–834.
- Balasubramanian CK 2015 The community balance and mobility scale alleviates the ceiling effects observed in the currently used gait and balance assessments for the community-dwelling older adults. Journal of Geriatric Physical Therapy 38: 78–89.
- Beauchamp MK, Hao Q, Kuspinar A, D’Amore C, Scime G, Ma J, Mayhew A, Bassim C, Wolfson C, Kirkland S, et al. 2021 Reliability and minimal detectable change values for performance-based measures of physical functioning in the canadian longitudinal study on aging. Journals of Gerontology: Series A 76: 2030–2038.
- Bhattacharya PK, Deka K, Roy A 2016 Assessment of inter-rater variability of the senior fitness test in the geriatric population: a community based study. International Journal of Biomedical and Advance Research 7: 208–212.
- Bland JM, Altman D 1986 Statistical methods for assessing agreement between two methods of clinical measurement. The Lancet 327: 307–310.
- Bland JM, Altman DG 1996 Statistics notes: Measurement error. BMJ: British Medical Journal 312: 1654.
- Brooks GC, Vittinghoff E, Iyer S, Tandon D, Kuhar P, Madsen KA, Marcus GM, Pletcher MJ, Olgin JE 2015 Accuracy and usability of a self-administered 6-minute walk test smartphone application. Circulation: Heart Failure 8: 905–913.
- Buatois S, Perret-Guillaume C, Gueguen R, Miget P, Vançon G, Perrin P, Benetos A 2010 A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Physical Therapy 90: 550–560.
- Buckinx F, Rezoulat M, Lefranc C, Reginster J-Y, Bruyere O 2024 Comparing remote and face-to-face assessments of physical performance in older adults: A reliability study. Geriatric Nursing 55: 71–78.
- Cabana F, Boissy P, Tousignant M, Moffet H, Corriveau H, Dumais R 2010 Interrater agreement between telerehabilitation and face-to-face clinical outcome measurements for total knee arthroplasty. Telemedicine and E-Health 16: 293–298.
- Centers for Disease Control and Prevention 2017 Assessment 30-Second Chair Stand. Georgia, USA. https://www.cdc.gov/steadi/pdf/STEADI-Assessment-30Sec-508.pdf
- Choi NG, DiNitto DM, Marti CN, Choi BY 2022 Telehealth use among older adults during COVID-19: Associations with sociodemographic and health characteristics, technology device ownership, and technology learning. Journal of Applied Gerontology 41: 600–609.
- Donoghue D, Stokes EK 2009 How much change is true change? The minimum detectable change of the berg balance scale in elderly people. Journal of Rehabilitation Medicine 41: 343–346.
- Elimelech OC, Ferrante S, Josman N, Meyer S, Lunardini F, Gómez-Raja J, Galán C, Cáceres P, Sciama P, Gros M, et al. 2022 Technology use characteristics among older adults during the COVID-19 pandemic: A cross-cultural survey. Technology in Society 71: 102080.
- Espy DD, Yang F, Bhatt T, Pai Y-C 2010 Independent influence of gait speed and step length on stability and fall risk. Gait & Posture 32: 378–382.
- Gaspar AGM, Lapão LV 2021 Health for addressing balance disorders in the elderly: systematic review. Journal of Medical Internet Research 23: e22215.
- Giavarina D 2015 Understanding bland altman analysis. Biochemia Medica 25: 141–151.
- Julayanont P, Nasreddine ZS 2017 Montreal cognitive assessment (MoCA): concept and clinical review. In: Larner AJ (Ed) Cognitive screening instruments. pp. 139–195. New York City, United states: Springer.
- Kottner J, Audige L, Brorson S, Donner A, Gajewski BJ, Hrobjartsson A, Roberts C, Shoukri M, Streiner DL 2011 Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. International Journal of Nursing Studies 48: 661–671.
- Kyrdalen IL, Thingstad P, Sandvik L, Ormstad H 2019 Associations between gait speed and well‐known fall risk factors among community‐dwelling older adults. Physiotherapy Research International 24. 10.1002/pri.1743
- Lexell JE, Downham DY 2005 How to assess the reliability of measurements in rehabilitation. American Journal of Physical Medicine & Rehabilitation 84: 719–723.
- Lima C, Ricci N, Nogueira E, Perracini MR 2018 The berg balance scale as a clinical screening tool to predict fall risk in older adults: a systematic review. Physiotherapy 104: 383–394.
- Lin W-S, Hsu N-W, Lee M-J, Lin Y-Y, Tsai C-C, Pan P-J 2022 Correlation analysis of physical fitness and its impact on falls in 2130 community-dwelling older adults: a retrospective cross-sectional study. BMC Geriatrics 22: 1–11.
- Madhavan S, Sivaramakrishnan A, Bowden MG, Chumbler NR, Field-Fote EC, Kesar TM 2022 Commentary: Remote assessments of gait and balance-Implications for research during and beyond Covid-19. Topics in Stroke Rehabilitation 29: 74–81.
- Marques A, Almeida S, Carvalho J, Cruz J, Oliveira A, Jácome C 2016 Reliability, validity, and ability to identify fall status of the balance evaluation systems test, mini–balance evaluation systems test, and brief–balance evaluation systems test in older people living in the community. Archives of Physical Medicine and Rehabilitation 97: 2166–2173.
- Mielenz TJ, Kannoth S, Jia H, Pullyblank K, Sorensen J, Estabrooks P, Stevens JA, Strogatz D 2020 Evaluating a two-level vs. three-level fall risk screening algorithm for predicting falls among older adults. Frontiers in Public Health 8: 373. 10.3389/fpubh.2020.00373
- Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J, Hogan DB, Hunter SW, Kenny RA, Lipsitz LA, et al. 2021 Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Network Open 4: e2138911.
- Park SH 2018 Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Aging Clinical and Experimental Research 30: 1–16.
- Pelicioni PH, Waters DL, Still A, Hale L 2022 A pilot investigation of reliability and validity of balance and gait assessments using telehealth with healthy older adults. Experimental Gerontology 162: 111747.
- Peyrusqué E, Granet J, Pageaux B, Buckinx F, Aubertin-Leheudre M 2022 Assessing physical performance in older adults during isolation or lockdown periods: Web-based video conferencing as a solution. The Journal of Nutrition, Health & Aging 26: 52–56.
- Pinto TC, Machado L, Bulgacov TM, Rodrigues-Júnior AL, Costa ML, Ximenes RC, Sougey EB 2019 Is the montreal cognitive Assessment (MoCA) screening superior to the Mini-Mental State Examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s Disease (AD) in the elderly? International Psychogeriatrics 31: 491–504.
- Portney LG, Watkins MP 2009 Foundations of clinical research: applications to practice. Upper Saddle River, New Jersey: Pearson/Prentice Hall.
- Rankin G, Stokes M 1998 Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clinical Rehabilitation 12: 187–199.
- Rydwik E, Bergland A, Forsén L, Frändin K 2011 Psychometric properties of timed up and go in elderly people: a systematic review. Physical & Occupational Therapy in Geriatrics 29: 102–125.
- Salari N, Darvishi N, Ahmadipanah M, Shohaimi S, Mohammadi M 2022 Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research 17: 1–13.
- Senderovich H, Wignarajah S 2022 COVID-19 virtual care for the geriatric population: exploring two sides of the coin. Gerontology 68: 289–294.
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE 2019 Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2019: CD012424. 10.1002/14651858.CD012424.pub2
- Shumway-Cook A, Brauer S, Woollacott M 2000 Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Physical Therapy 80: 896–903.
- Unver B, Baris RH, Yuksel E, Cekmece S, Kalkan S, Karatosun V 2017 Reliability of 4-meter and 10-meter walk tests after lower extremity surgery. Disability and Rehabilitation 39: 2572–2576.
- Venkataraman K, Morgan M, Amis KA, Landerman LR, Koh GC, Caves K, Hoenig H 2017 Tele-assessment of the berg balance scale: effects of transmission characteristics. Archives of Physical Medicine and Rehabilitation 98: 659–664.
- Walter S, Eliasziw M, Donner A 1998 Sample size and optimal designs for reliability studies. Statistics in Medicine 17: 101–110.