ABSTRACT
Visual agnosia and Balint’s syndrome are complex neurological disorders of the higher visual system that can have a remarkable impact on individuals’ lives. Rehabilitation of these individuals is important to enable participation in everyday activities despite the impairment. However, the literature about the rehabilitation of these disorders is virtually silent. Therefore, the aim of this systematic review is to give an overview of available literature describing treatment approaches and their effectiveness with regard to these disorders. The search engines Psychinfo, Amed, and Medline were used, resulting in 22 articles meeting the criteria for inclusion. Only articles describing acquired disorders were considered. These articles revealed that there is some information available on the major subtypes of visual agnosia as well as on Balint’s syndrome which practising clinicians can consult for guidance. With regard to the type of rehabilitation, compensatory strategies have proven to be beneficial in most of the cases. Restorative training on the other hand has produced mixed results. Concluding, although still scarce, a scientific foundation about the rehabilitation of visual agnosia and Balint’s syndrome is evolving. The available approaches give valuable information that can be built upon in the future.
Introduction
Due to the complexity of neurological disorders and the individual nature of impairments, neuropsychological rehabilitation is a difficult endeavour. Especially the rehabilitation of visual (perceptual) disorders is multifaceted, since visual disturbances may take place at lower and/or at higher function levels. Vision is often affected in patients with neurological disorders. For example, about 30% of the patients with acquired brain injury show deficits in vision (Zihl, Citation2003) and 20–40% of the patients with cerebrovascular acquired brain injury or traumatic brain injury (TBI) have higher visual disorders (Zihl & Kennard, Citation2003). Visual perceptual disorders can have a tremendous impact on an individual’s spatial orientation, learning, and motor activities (Zihl, Citation2003), which in turn can affect a person’s independence, social participation, and vocational life. Therefore, rehabilitation of visual perceptual disorders is a central topic in clinical practice.
Two approaches can be distinguished in neuropsychological rehabilitation (Spikman & Fasotti, Citation2017). The first type, restoration, aims to improve a particular function by training the impaired function and thereby the damaged brain structure directly and repetitively. The second type, compensation, refers to using an intact function to compensate for the loss of the other one. Thus, the impaired function itself is not targeted, but functioning on an activity and participation level is rather attempted to be improved. Depending on the level of impairment of the patient, environmental adaptation, for example signposting a route, could also be implemented if the patient’s ability to learn compensatory strategies is limited. Often, a combination of these approaches may be necessary in a rehabilitation regime. The type of treatment chosen should also consider the type of brain injury the patient suffers from.
Visual (perceptual) disorders such as visual field defects, neglect, or difficulties with contrasts and colours may arise from either acquired brain injury (ABI; e.g., stroke) or neurodegenerative disorders (e.g., dementia, Parkinson’s disease, and multiple sclerosis). Although there are several treatment options available for the more frequent disorders like hemianopia and neglect (Bowen, Hazelton, Pollock, & Lincoln, Citation2013; De Haan, Heutink, Melis-Dankers, Tucha, & Brouwer, Citation2014; Pollock et al., Citation2011), some visual disorders have received only little attention regarding their rehabilitation. Two disorders for which the latter is true are visual agnosia and Balint’s syndrome, which can manifest in patients following ABI as well as in neurodegenerative diseases.
According to Zihl (Citation2003), visual agnosia is a difficulty or inability to identify familiar stimuli via the visual modality, although the patient possesses sufficient visual perceptual, cognitive, and verbal functioning, and is able to recognise the stimulus using other modalities. Pure visual agnosia is a relatively rare condition, with an estimated prevalence of about 1–3% (Zihl & Kennard, Citation2003). At least four types of visual agnosia can be differentiated: prosopagnosia (the inability to recognise familiar faces and to learn new faces); object agnosia (the inability to identify stimuli in the same class or differentiate between classes of stimuli); topographical agnosia (difficulties with geographical orientation); and letter agnosia or pure alexia (inability to recognise individual letters and their combinations; Damasio, Tranel, & Rizzo, Citation2000; Roberts, Citation1992; Zihl, Citation2003). However, also finer distinctions can be made and very specific agnosias can be found in the literature as well (e.g., colour agnosia; Nijboer & Heutink, Citation2017).
A remarkable syndrome arising from disturbances to the higher visual system is Balint’s syndrome (Balint, Citation1909). Balint’s syndrome usually occurs after damage to bilateral posterior-parietal brain areas, and can occur after ABI or due to neurodegenerative diseases, usually dementia (Kerkhoff & Heldmann, Citation1999). Damasio et al. (Citation2000), define Balint’s syndrome as
An acquired disturbance of the ability to perceive the visual field as a whole, resulting in the unpredictable perception and recognition of only parts of it (simultanagnosia); which is accompanied by an impairment of target pointing under visual guidance (optic ataxia) and an inability to shift gaze at will toward new visual stimuli (ocular apraxia). (p. 353)
Individuals with acquired visual agnosia or Balint’s syndrome require intensive rehabilitation to help them to overcome their deficits. In addition to that, spontaneous recovery in both visual agnosia and Balint’s syndrome is assumed to be low (Zihl & Kennard, Citation2003). This emphasises the importance of rehabilitation as an invaluable tool for affected individuals. However, due to the much lower prevalence of these visual-perceptual disorders compared to hemianopia or neglect, there are not many studies on the rehabilitation of visual agnosia and Balint’s syndrome available. The purpose of this article is therefore to conduct a systematic literature review on the rehabilitation of acquired visual agnosia and Balint’s syndrome to explore the available treatment approaches and their effectiveness, and to give an indication of which sources to pursue for those interested in further detail. Thereby, we aim to provide a status update on the rehabilitation of visual agnosia and Balint’s syndrome and give directions for future research.
Method
A comprehensive systematic literature search was conducted to retrieve literature addressing cognitive rehabilitation of acquired visual agnosia and Balint’s syndrome.
Search strategy
This study utilised the academic databases Psychinfo, Medline, and Amed to search for peer-reviewed publications published in either English or German. Keywords used were “treatment” or “rehabilitation” in combination with each of the terms “visual agnosia,” “simultanagnosia,” “object agnosia,” “prosopagnosia,” “associative agnosia,” “apperceptive agnosia,” “colour agnosia,” “form agnosia,” “semantic agnosia,” “topographical agnosia,” and “Balint’s syndrome” in either English or German translation. We did not define a certain time period for the inclusion of the listed results and did not include unpublished data. Abstracts of the listed results were reviewed to identify those articles addressing the topic at hand.
Study selection
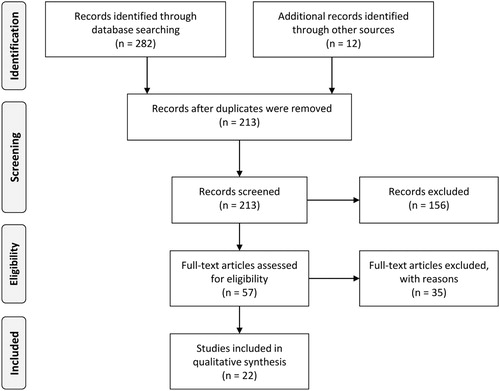
The time period of the listed results ranged from 1948 until 2017. shows the steps followed during the literature search (PRISMA flow diagram; Moher, Liberati, Tetzlaff, Altman & The PRISMA Group Citation2009). Exclusion criteria were: (a) if the deficit was caused by a congenital condition, meaning the visual system had not developed normally before the occurrence of the impairment; (b) if the rehabilitation was on pure alexia as there have been publications reviewing the current status of rehabilitation (e.g., Starrfelt, Ólafsdóttir, & Arendt, Citation2013); and (c) if the sections dealing with the rehabilitation of visual agnosia and Balint’s syndrome only did so by describing other researchers’ work. We included studies: (a) providing evidence about the effectiveness of a rehabilitation by empirically evaluating it; (b) giving recommendations for rehabilitation based on scientific foundations or clinical experience as long as the recommendations were specific enough to give guidance to practising clinicians; (c) describing the impairment as part of a more global deficit or in conjunction with other impairments (as we expected the literature to be too scarce to only consider “pure” impairments); and (d) investigating cases in which neurodegenerative disorders gave rise to visual agnosia or Balint’s syndrome. In case of doubt whether an article should be included in the review or not, the authors discussed them in the light of the purpose of the paper and whether the given information would be useful in guiding practising clinicians. We did not apply any criteria concerning the methodological quality of the studies, since we expected mostly studies with small sample sizes or case studies due to the rare occurrence of the deficits. A total of 22 sources published between 1992 and 2017 met the inclusion criteria, and are thus listed in the results.
Data synthesis
To differentiate between the rehabilitation of the different visual perceptual disorders, we divided the articles into three sections. The first section considers the rehabilitation of Balint’s syndrome, the second section describes the rehabilitation of prosopagnosia and object agnosia, and the third section deals with the rehabilitation of topographical agnosia. This division enabled us to separate all the articles except for one (Roberts, Citation1992), which addresses the rehabilitation of both Balint’s syndrome and visual agnosia. This article was therefore included in both the respective sections. Per article we further determined the rehabilitation approaches described (restorative or compensatory).
Results
Balint’s syndrome
A total of 10 articles addressing the rehabilitation of Balint’s syndrome met our criteria. Seven of these articles presented a case study including empirical validation of a treatment, while three articles gave suggestions and recommendations for treatment (). Generally, it can be observed that most rehabilitation approaches were multifaceted, and led to variable improvements in the treated patients. Compensatory strategies seemed to be widely applied and usually relatively successful. A small number of studies attempted to train the specific deficits arising from Balint’s syndrome (Perez, Tunkel, Lachmann, & Nagler, Citation1996; Rosselli, Ardila, & Beltran, Citation2001; Zgaljardic, Yancy, Levinson, Morales, & Masel, Citation2011), with for example eye movement exercises or convergence exercises, which proved to be successful in some patients (Rosselli et al., Citation2001). Yet, some attempts remained less successful (Zgaljardic et al., Citation2011), allowing for little conclusiveness about the effectiveness of neuropsychological training or eye movement exercises. Several authors emphasised the importance of psychoeducation, strategies to promote the transfer from training situations to real-life situations, functional abilities, as well as building on strengths. Importantly, the choice for a rehabilitation approach and the expectations for an outcome depended heavily on the aetiology of Balint’s syndrome. Perez et al. (Citation1996) proposed to focus on learning and using strategies for neurodegenerative disorders that increase participation in everyday activities to increase coping and confidence in patients.
Table 1. Articles addressing the rehabilitation of Balint’s s syndrome.
Based on the results of this search, we can conclude that a certain degree of rehabilitation of Balint’s syndrome is possible for most patients, in so far as to regain functional capabilities and quality of life. A necessary condition might be that the treatment is individually tailored to the patient and the therapists maintain flexibility throughout the process.
Prosopagnosia and object agnosia
Much research on prosopagnosia has focused on the mechanisms by which we recognise faces and how these might be damaged. With regard to rehabilitation, two literature reviews could be found. The 12 case studies already reviewed by these two articles were not included in the present study. Instead, we added eight studies on the rehabilitation of prosopagnosia that were not included in these literature reviews ().
Table 2. Articles addressing the rehabilitation of prosopagnosia and object agnosia.
Both literature reviews concluded that restorative training has not yet proven to be very successful and that compensatory strategies appeared to be a more effective approach for the rehabilitation of acquired prosopagnosia (Bate & Bennetts, Citation2014; DeGutis, Chiu, Grosso, & Cohan, Citation2014). The additional eight articles appeared to be in line with the outcome of the literature reviews, especially with regard to transferring the training to real-life face recognition (Bate et al., Citation2015). The study by Davies-Thompson et al. (Citation2017) describes a promising restorative approach, however training is very intense and does not improve real-life facial recognition in all participants involved. Concluding, compensation strategies seemed to be most promising for the rehabilitation of prosopagnosia.
With regard to object agnosia, the literature search revealed seven articles, describing the rehabilitation of object agnosia either in the context of other impairments (four studies) or as suggestions for rehabilitation strategies without clinical data (three studies; ). Generally, compensating for the deficit via tactile and auditory modes, as well as via verbal description and kinaesthetic information was frequently recommended (Tanemura, Citation1999). Zihl (Citation2011) trained object recognition in two patients using a restorative approach, which led to improvements in both patients with some generalisation to non-trained objects. Seniow, Polanowska, Mandat, and Laudanski (Citation2003) achieved improvements using both restorative and compensatory training. Therefore, it is hard to draw conclusions about which the effective component was. To summarise, there is only limited data available on effective rehabilitation of object agnosia, but evidence is beginning to emerge for the usefulness of both restorative and compensatory strategies.
Topographical agnosia
Literature on the rehabilitation of topographical agnosia is scarce; only two studies giving information on treatment approaches could be included (). In the first study, Bouwmeester, Van de Wege, Haaxma, and Snoek (Citation2015) described a patient with a relatively severe clinical presentation who benefited from an individualised training programme. The patient did not improve much in location recognition, but nevertheless learned to reach desired destinations. This outcome provides evidence that training can significantly increase independence and quality of life even in patients with severe deficits. The second study described a generally more highly functioning individual, who suffered severely from topographical disorientation (Davis & Coltheart, Citation1999). By focusing on the patient’s relevant environment and common routes, the patient was taught to use mnemonic techniques and a map to reach desired destinations independently and more securely. To conclude, both studies used compensatory strategies for the rehabilitation and offered some specific ideas about what may have been effective in these two cases.
Table 3. Articles addressing the rehabilitation of topographical disorientation.
Discussion
The aim of the present literature review was to systematically collect information or recommendations for the rehabilitation of visual agnosia and Balint’s syndrome. The results show that especially compensatory strategies have proven to be beneficial in most cases, whereas restorative training has produced mixed results. Evidence for the effectiveness of restorative training in acquired prosopagnosia is currently not very persuasive. For the other subtypes of agnosia, it is not possible to draw conclusions about the effectiveness of restorative training as there is too little and contradictory research available. In Balint’s syndrome, restorative training has been shown to be more successful, but there is also not enough research available to give a clear indication. Altogether, though still very scarce, a scientific foundation about the rehabilitation of these disorders is evolving and there are approaches giving valuable information that can be built upon in the future. Yet, a few issues require some further consideration.
First, for the treatment of agnosia, Groh-Bordin and Kerkhoff (Citation2010) suggested that, based on their clinical experience, it might be more effective to treat deficits that co-occur with agnosia (e.g., hemianopia) rather than focusing on the agnosia itself. This approach is based on the view that, if other visual deficits are enhanced, recognition will likely be improved as well. However, Zihl (Citation2011) failed to prove this approach. He attempted to improve identification and recognition by training oculomotor scanning in patients with homonymous visual field loss and disorientation, which resulted in improvement of the trained skill, yet none for recognition. Nevertheless, it seems plausible that improved lower visual functions will increase the chances to rehabilitate recognition as well. We would argue that clinicians need to consider how much the patients are – subjectively and objectively – impaired by the agnosia. If the agnosia dominates impairment caused by other deficient visual functions, rehabilitation should target the specific agnostic deficit at least by training compensatory strategies.
Another factor to consider in clinical rehabilitation is the cost-effectiveness of a certain approach. As mentioned before, the effectiveness of restorative training in visual agnosia and Balint’s syndrome has not been fully proven. In addition to that, successful rehabilitation using restorative training usually follows an extensive period of training, sometimes up to hundreds of hours of practice with often only small improvements in daily life (e.g., Zihl, Citation2011). This might lead to potential frustration in patients. Compensatory strategies on the other hand have been shown to achieve meaningful progress in the patients’ daily functioning and might therefore be more cost-effective. Yet, one pitfall may be that patients may not be ready to “accept” the impairment in early stages of the rehabilitation, decreasing the motivation to attempt compensation rather than training the deficit itself (Finauer, Citation2009). Most important, decisions about rehabilitation approaches need to be individualised, taking the circumstances and unique impairments of the patients into consideration.
Future research and clinical practice
Based on the current literature available, an evidence-based rehabilitation programme cannot be established. We therefore encourage clinicians to share any cases of visual agnosia and Balint’s syndrome with the scientific community, and to make detailed rehabilitation plans available to benefit other practitioners. Especially the addition of more details about the rehabilitation approach, including pre- and post-measurements, would be helpful to establish an evidence-based practice. Future publications may take this literature review as a basis for further research to confirm the effectiveness of particular rehabilitation approaches and fill in further knowledge gaps. For example, existing cognitive rehabilitation software that was created to train people with visual agnosia and Balint’s syndrome (for example, visual exploration exercises), could be incorporated into future rehabilitation programmes to be systematically evaluated. Furthermore, the literature described in the present manuscript rarely explored how well trained skills transferred into the relevant context for the patient. It is important for future research to not overlook this crucial step in determining the effectiveness of a certain rehabilitation approach.
Conclusion
The current article provides a basis and starting point for more systematic progress towards an evidence-based treatment approach for patients with visual agnosia and Balint’s syndrome. Researchers and clinicians can use the information this article revealed to guide their research and fill in the knowledge gaps identified in the present literature review.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Joost Heutink http://orcid.org/0000-0002-4811-968X
References
- Al-Khawaja, I., Haboubi, N. H. J., & Kerkhoff, G. (2001). Neurovisual rehabilitation in Balint’s syndrome. Journal of Neurology, Neurosurgery & Psychiatry, 70, 416–416. doi: 10.1136/jnnp.70.3.416
- Anderson, S. W., & Rizzo, M. (1995). Recovery and rehabilitation of visual cortical dysfunction. NeuroRehabilitation, 5(2), 129–140. doi:10.3233/NRE-1995-5204 doi: 10.1016/1053-8135(94)00111-7
- Balint, R. (1909). Seelenlähmung des “Schauens”: Optische Ataxie, räumliche Störung der Aufmerksamkeit [Paralysis of “seeing”: Optical ataxia, spatial disorder of attention]. Monatszeitschift Für Psychiatrie Und Neurologie, 25(1), 51–66. doi: 10.1159/000210464
- Bate, S., & Bennetts, R. J. (2014). The rehabilitation of face recognition impairments: A critical review and future directions. Frontiers in Human Neuroscience, 8, 491–491. doi: 10.3389/fnhum.2014.00491
- Bate, S., Bennetts, R., Mole, J. A., Ainge, J. A., Gregory, N. J., Bobak, A. K., & Bussunt, A. (2015). Rehabilitation of face-processing skills in an adolescent with prosopagnosia: Evaluation of an online perceptual training programme. Neuropsychological Rehabilitation, 25(5), 733–762. doi: 10.1080/09602011.2014.973886
- Bouwmeester, L., Van de Wege, A., Haaxma, R., & Snoek, J. W. (2015). Rehabilitation in a complex case of topographical disorientation. Neuropsychological Rehabilitation, 25(1), 1–14. doi: 10.1080/09602011.2014.923318
- Bowen, A., Hazelton, C., Pollock, A., & Lincoln, N. B. (2013). Cognitive rehabilitation for spatial neglect following stroke. Cochrane Database of Systematic Reviews, 7, CD003586. doi: 10.1002/14651858.CD003586.pub3
- Burns, M. S. (2004). Clinical management of agnosia. Topics in Stroke Rehabilitation, 11(1), 1–9. doi: 10.1310/N13K-YKYQ-3XX1-NFAV
- Damasio, A. R., Tranel, D., & Rizzo, M. (2000). Disorders of complex visual processing. In M. M. Mesualm (Ed.), Principles of behavioral and cognitive neurology (pp. 332–364). New York: Oxford University Press.
- Davies-Thompson, J., Fletcher, K., Hills, C., Pancaroglu, R., Corrow, S. L., & Barton, J. J. S. (2017). Perceptual learning of faces: A rehabilitative study of acquired prosopagnosia. Journal of Cognitive Neuroscience, 29, 573–591. doi: 10.1162/jocn_a_01063
- Davis, S. J. C., & Coltheart, M. (1999). Rehabilitation of topographical disorientation: An experimental single case study. Neuropsychological Rehabilitation, 9(1), 1–30. doi: 10.1080/713755586
- DeGutis, J. M., Chiu, C., Grosso, M. E., & Cohan, S. (2014). Face processing improvements in prosopagnosia: Successes and failures over the last 50 years. Frontiers in Human Neuroscience, 8, 561–561. doi: 10.3389/fnhum.2014.00561
- De Haan, G. A., Heutink, J., Melis-Dankers, B. J. M., Tucha, O., & Brouwer, W. H. (2014). Spontaneous recovery and treatment effects in patients with homonymous visual field defects: A meta-analysis of existing literature in terms of the ICF framework. Survey of Ophthalmology, 59(1), 77–96. doi: 10.1016/j.survophthal.2013.02.006
- Finauer, G. (2009). Therapiemanuale für die neuropsychologische Rehabilitation: Kognitive und kompetenzorientierte Therapie für die Gruppen- und Einzelbehandlung [Manual for neuropsychological rehabilitation: Cognitive and competence-oriented therapy for group- and indivudual treatment]. Berlin: Springer.
- Gillen, J. A., & Dutton, G. N. (2003). Balint’s syndrome in a 10-year-old male. Developmental Medicine & Child Neurology, 45(5), 349–352. doi: 10.1111/j.1469-8749.2003.tb00407.x
- Groh-Bordin, C., & Kerkhoff, G. (2010). Recovery and treatment of sensory perceptual disorders. In J. Gurd, U. Kischka, & J. Marshall (Eds.), Handbook of clinical neuropsychology (pp. 139–158). New York: Oxford University Press.
- Kerkhoff, G., & Groh-Bordin, C. (2010). Höhere visuelle Funktionen: Neglect, Raumorientierung, Balint-Holmes Syndrom und Agnosien [Higher visual functions: Neglect, spatial orientation, balint-holmes syndrome and agnosias]. In P. Frommelt & H. Lösslein (Eds.), NeuroRehabilitation (pp. 207–221). Berlin: Springer.
- Kerkhoff, G., & Heldmann, B. (1999). Balint syndrome and associated disorders. Anamnesis–diagnosis–approaches to treatment. Der Nervenarzt, 70(10), 859–869. doi: 10.1007/s001150050589
- Kerkhoff, G., & Marquardt, C. (2009a). EYEMOVE. Standardized assessment and treatment of visual search disorders. Der Nervenarzt, 80(10), 1190. doi: 10.1007/s00115-009-2811-4
- Kerkhoff, G., & Marquardt, C. (2009b). Erworbene, visuell bedingte Lesestörungen: Standardisierte Diagnostik und Therapie mit READ [Acquired, visually based reading disorders: Standardised assessment and treatment with READ]. Der Nervenarzt, 80(12), 1424–1439. doi: 10.1007/s00115-009-2723-3
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. doi: 10.1371/journal.pmed.1000097
- Nijboer, T., & Heutink, J. (2017). Visual perception. In R. Kessels, P. Eling, R. Ponds, J. Spikman, & Van M. Zandvoort (Eds.), Clinical neuropsychology (pp. 137–157). Amsterdam: Boom.
- Perez, F. M., Tunkel, R. S., Lachmann, E. A., & Nagler, W. (1996). Balint’s syndrome arising from bilateral posterior cortical atrophy or infarction: Rehabilitation strategies and their limitation. Disability and Rehabilitation, 18(6), 300–304. doi: 10.3109/09638289609165884
- Pollock, A., Hazelton, C., Henderson, C. A., Angilley, J., Dhillon, B., Langhorne, P., … Shahani, U. (2011). Interventions for visual field defects in patients with stroke. Cochrane Database of Systematic Reviews, (10), CD008388. doi: 10.1002/14651858.CD008388.pub2
- Roberts, S. P. (1992). Visual disorders of higher cortical function. Journal of the American Optometric Association, 63(10), 723–732.
- Roca, M., Gleichgerrcht, E., Torralva, T., & Manes, F. (2010). Cognitive rehabilitation in posterior cortical atrophy. Neuropsychological Rehabilitation, 20(4), 528–540. doi: 10.1080/09602011003597408
- Rosenthal, O., & Behrmann, M. (2006). Acquiring long-term representations of visual classes following extensive extrastriate damage. Neuropsychologia, 44(5), 799–815. doi: 10.1016/j.neuropsychologia.2005.07.010
- Rosselli, M., Ardila, A., & Beltran, C. (2001). Rehabilitation of balint’s syndrome: A single case report. Applied Neuropsychology, 8(4), 242–247. doi:10.1207/09084280152829093 doi: 10.1207/S15324826AN0804_7
- Seniow, J., Polanowska, K., Mandat, T., & Laudanski, K. (2003). The cognitive impairments due to the occipito-parietal brain injury after gunshot. A successful neurorehabilitation case study. Brain Injury, 17(8), 701–713. doi: 10.1080/0269905031000088621
- Spikman, J., & Fasotti, L. (2017). Recovery and treatment. In R. Kessels, P. Eling, R. Ponds, J. Spikman, & M. Van Zandvoort (Eds.), Clinical neuropsychology (pp. 113–133). Amsterdam: Boom.
- Starrfelt, R., Ólafsdóttir, R. R., & Arendt, I.-M. (2013). Rehabilitation of pure alexia: A review. Neuropsychological Rehabilitation, 23(5), 755–779. doi: 10.1080/09602011.2013.809661
- Tanemura, R. (1999). Awareness in apraxia and agnosia. Topics in Stroke Rehabilitation, 6(1), 33–42. doi: 10.1310/U9KU-M4X8-DMRQ-9TR7
- Zgaljardic, D. J., Yancy, S., Levinson, J., Morales, G., & Masel, B. E. (2011). Balint’s syndrome and post-acute brain injury rehabilitation: A case report. Brain Injury, 25(9), 909–917. doi: 10.3109/02699052.2011.585506
- Zihl, J. (2003). Recovery and rehabilitation of cerebral visual disorders. In M. Fahle & M. Greenlee (Eds.), The neuropsychology of vision (pp. 319–338). New York: Oxford University Press.
- Zihl, J. (2011). Rehabilitation of visual disorders after brain injury. New York: Psychology Press.
- Zihl, J., & Kennard, C. (2003). Disorders of higher visual function. In T. Brandt (Ed.), Neurological disorders: Course and treatment (pp. 255–261). Amsterdam: Academic Press.