ABSTRACT
Subjective Cognitive Complaints (SCC) are common after stroke and adversely affect quality of life. In the present study, we determined the associations of depression, anxiety, perceived stress and fatigue with post-stroke SCC, and whether these associations were independent of objective cognitive functioning, stroke characteristics and individual differences in personality traits and coping styles. Using a cross-sectional design, SCC and psychological measures were obtained in 208 patients (mean 3.3 ± 0.5 months after stroke; 65.9% men; mean age 64.9 ± 12.4 years). SCC were assessed using the Checklist for Cognitive and Emotional consequences following stroke (CLCE) inventory. Validated questionnaires were used to measure depression and anxiety (Hospital Anxiety and Depression Scale), perceived stress (Perceived Stress Scale), fatigue (Fatigue Assessment Scale), personality traits (Eysenck Personality Questionnaire Revised Short Scale) and coping style (Utrecht Coping List). Multivariate hierarchical linear regression analyses were used to adjust for covariates. Depression (β = 0.35), anxiety (β = 0.38), perceived stress (β = 0.39), and fatigue (β = 0.39) were associated with CLCE scores, independent of demographic, cognitive performance and stroke-related covariates. After including personality traits and coping styles in the model, independent associations with CLCE scores were found for fatigue (β = 0.26, p = .003) and neuroticism (β = 0.21, p = .05). Interventions aimed at improving psychological resilience and increasing energy levels might be a worthwhile addition to stroke rehabilitation programmes by reducing SCC and improving quality of life.
Introduction
Subjective Cognitive Complaints (SCC) are common after stroke, with prevalence estimates ranging between 28.6% and 92.0% (van Rijsbergen, Mark, de Kort, & Sitskoorn, Citation2014, Citation2015). These complaints occur early after stroke and often remain present until years after the event (Carlsson, Moller, & Blomstrand, Citation2003; Duits, Munnecom, van Heugten, & van Oostenbrugge, Citation2008; Nijsse et al., Citation2017; Wendel, Risberg, Pessah-Rasmussen, Stahl, & Iwarsson, Citation2008). The most commonly reported SCC in this population include mental slowness, concentration difficulties and memory problems (van Rijsbergen et al., Citation2014). The biomedical and psychological factors that play a role in post-stroke SCC are not well understood. Evidence suggests that objective indices of cognitive performance based on neuropsychological testing show correlations with post-stroke SCC as well as functioning after stroke as assessed using measures of activities of daily living (ADL) (Davis, Cockburn, Wade, & Smith, Citation1995; Narasimhalu, Wiryasaputra, Sitoh, & Kandiah, Citation2013; van Heugten, Rasquin, Winkens, Beusmans, & Verhey, Citation2007; Winkens, Van Heugten, Fasotti, & Wade, Citation2009; Xiong et al., Citation2011). However, the reported associations are relatively weak, and these factors do not explain the high prevalence of SCC in post-stroke patients (van Rijsbergen et al., Citation2014).
Multiple studies indicate that psychological factors are related to SCC, particularly post-stroke depression (Aben et al., Citation2011; Duits et al., Citation2008; Lamb, Anderson, Saling, & Dewey, Citation2013; Maaijwee et al., Citation2014; Martin, Dellatolas, Viguier, Willadino-Braga, & Deloche, Citation2002; Nijsse et al., Citation2017; Winkens et al., Citation2009; Xiong et al., Citation2011). Most studies demonstrated that post-stroke depressive symptoms are associated with more SCC (Aben et al., Citation2011; Duits et al., Citation2008; Lamb et al., Citation2013; Maaijwee et al., Citation2014; Martin et al., Citation2002; Nijsse et al., Citation2017; Winkens et al., Citation2009; Xiong et al., Citation2011), although one study did not find such a relationship (Narasimhalu et al., Citation2013). Other psychosocial aspects known to occur frequently after stroke (e.g., anxiety and fatigue) have also been examined. Two studies reported that post-stroke anxiety was associated with SCC, but these associations were attenuated in multivariate adjusted models (Maaijwee et al., Citation2014; Nijsse et al., Citation2017). The relationship between post-stroke fatigue and SCC has also revealed mixed results (two studies found an association (Maaijwee et al., Citation2014; Winkens et al., Citation2009) and one did not (Lamb et al., Citation2013)). Symptoms of depression, anxiety and fatigue are interrelated after stroke and are an indication of psychological distress (Galligan, Hevey, Coen, & Harbison, Citation2016). Which of these aspects is the most important in relation to SCC is yet unknown. It is also possible that depression, anxiety and fatigue reflect a general factor of psychological distress that is associated with SCC in post-stroke patients.
Studies on SCC in the general population have shown that personality traits, neuroticism in particular, are strongly associated with SCC (Comijs, Deeg, Dik, Twisk, & Jonker, Citation2002; Pearman & Storandt, Citation2004). Whether this is also true for patients who had a stroke is less well established. Aben et al. (Citation2011) found a relationship between neuroticism and memory-related SCC, which became non-significant in covariate-adjusted models. An association with extraversion or coping style with post-stroke SCC was not found in that study (Aben et al., Citation2011). Nijsse et al. (Citation2017) reported an independent association between coping style (proactive coping) with the total number of SCC after stroke, whereas no relationships between neuroticism or extraversion with SCC were found. As personality traits and coping styles are known to be associated with measures of psychological distress such as anxiety and depressive symptoms (see for example Aben et al., Citation2002), these factors may play an additional role in post-stroke SCC.
The inconsistent results in the literature may partly be explained by the differences in stroke samples (e.g., primary focus on patients discharged home (Aben et al., Citation2011; Duits et al., Citation2008; Martin et al., Citation2002; van Heugten et al., Citation2007), or patients with a minor stroke (Narasimhalu et al., Citation2013; Xiong et al., Citation2011)), variability in the time interval after stroke used to assess SCC (e.g., early (Duits et al., Citation2008; Narasimhalu et al., Citation2013; Xiong et al., Citation2011) or chronic phase (Aben et al., Citation2011; Maaijwee et al., Citation2014)) and how SCC was defined and measured (van Rijsbergen et al., Citation2014). We defined SCC as a psychological construct with two components, a primary content component referring to the nature of cognitive difficulties, and an impact or worry component describing whether individuals report that their specific content-related SCC have an impact on their daily lives (van Rijsbergen et al., Citation2014, Citation2015).
In the present study, we examined: (1) to what extent distress-related psychological factors that are common in post-stroke patients (depression, anxiety, perceived stress and fatigue) were related to SCC at three months after a stroke, and (2) whether the association between these distress-related psychological measures and SCC changed after taking demographic characteristics, stroke severity, objective cognitive performance, ADL, personality traits and coping style into account. We also explored whether the psychological variables related to the SCC-worry component differed from those related to the SCC-content component.
Methods
Design and procedure
The current cross-sectional study reports data from the three months post-stroke assessment of the COMplaints After Stroke (COMPAS) study (van Rijsbergen, Mark, de Kort, & Sitskoorn, Citation2013). Between October 2009 and August 2012, patients were recruited from the Elisabeth-TweeSteden Hospital and the Maxima Medical Centre, the Netherlands. The Medical Ethics Committees of these hospitals approved the protocol and written informed consent was obtained from all individuals participating in this study.
Three months after a stroke (mean 3.3 ± 0.5 months), participants were invited to one of the hospitals for the assessment of SCC and neuropsychological test performance on multiple cognitive domains. Psychological questionnaires were completed at home and returned by mail. A reminder was sent when questionnaires were not returned within two weeks.
Participants
Patients with a clinical diagnosis of stroke (either ischemic or hemorrhagic, first-ever or recurrent) and aged ≥18 years were eligible for this study. Exclusion criteria were: premorbid health problems interfering with cognitive functioning (e.g., cognitive decline, as defined by a score of > 3.6 on the short version of the Informant Questionnaire on Cognitive Decline in the Elderly; IQCODE (de Jonghe, Schmand, Ooms, & Ribbe, Citation1997)), life-threatening progressive diseases (e.g., terminal cancer or kidney failure), a recent history of psychopathology and/or severe communication difficulties.
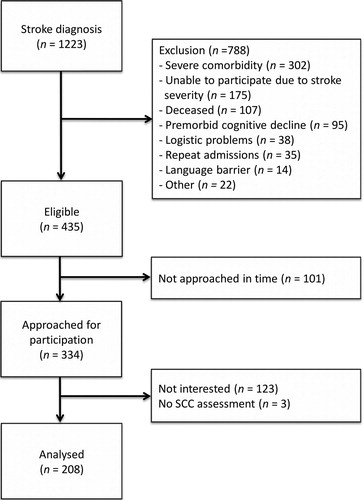
Four hundred and thirty-five patients were eligible, of whom 208 (47.8%) agreed to participate and had an SCC assessment (). Non-participants (i.e., patients who refused inclusion, N = 123, or could not be approached in time for the assessment, N = 101) and those who had no SCC assessment, N = 3, did not differ from participants regarding stroke type (ischemic or hemorrhagic), but they more often had a left-sided lesion (56.5% versus 42.9%, p = .01) and were less severely affected by their stroke at time of admission (National Institutes of Health Stroke Scale, NIHSS, (Brott et al., Citation1989) median NIHSS score = 2, interquartile range (IQR) = 1–4 versus median score = 3 (IQR = 2–5; p = .03). Non-participants were also older (69.6 ± 12.4 versus 64.9 ± 12.4 years, p < .001) and were more often female (44.5% versus 34.1%, p = .03).
Materials
SCC
Assessments of SCC were obtained using the Checklist for Cognitive and Emotional consequences following stroke (CLCE) inventory (van Heugten et al., Citation2007). The CLCE is a standardised interview exploring post-stroke cognitive, emotional and behavioural complaints. Thirteen of the 24 items focus on self-reported cognitive problems and were used in the present study. Each item was scored on presence and interference in daily life: 0 (SCC not present), 1 (doubtful presence), 2 (present, but not affecting daily life), 3 (present and negatively affecting daily life). The CLCE-content score, defined as the number of SCC present irrespective of whether these interfered with daily life, was calculated by dichotomising each item score into “absent” (original item score 0) and “present” (item score 1 through 3) and summing the items (score range CLCE-content score = 0–13). In addition, the CLCE-worry score, defined as the number of SCC having an impact on daily life, was calculated by dichotomising each item into “absence of interference” (item score 0 through 2) or “presence of interference” (item score 3) and summed over the 13 items (range CLCE-worry score = 0–13). This procedure for analysing the CLCE has been used before (Duits et al., Citation2008; Nijsse et al., Citation2017). We furthermore calculated the total CLCE-cognitive score by summing the original item scores (range 0–39). The CLCE has previously been validated in stroke patients (van Heugten et al., Citation2007). The internal consistency was found to be good (Cronbach’s α = 0.81 based on 22 items) (van Heugten et al., Citation2007). In the present study Cronbach’s α was 0.71 for CLCE-content, 0.75 for CLCE-worry, and 0.74 for total CLCE-cognitive score.
Depressive symptoms and anxiety
The Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, Citation1983) was used to assess current self-reported symptoms of depression (seven items, HADS-D) and anxiety (seven items, HADS-A). The total score for both subscales ranges between 0 and 21, with higher scores indicating more symptoms of depression or anxiety. The HADS has demonstrated good psychometric properties as a screening instrument both after a stroke and in several other populations with Cronbach’s α above 0.80 (Sagen et al., Citation2009; Spinhoven et al., Citation1997).
Perceived stress
The Perceived Stress Scale (PSS-4) (Cohen, Kamarck, & Mermelstein, Citation1983) explores the degree to which recent situations in life are perceived as stressful. The items are answered on a 5-point scale ranging from 0 (never) to 4 (very often). The total score ranges between 0 and 16, with a higher score indicating more perceived stress. The psychometric properties of the PSS-4 were found to be satisfactory in previous studies (Warttig, Forshaw, South, & White, Citation2013).
Fatigue
The Fatigue Assessment Scale (FAS) (Michielsen, De Vries, & Van Heck, Citation2003) (10 items) focuses on self-reported symptoms of fatigue. The items are rated on a 5-point scale ranging from 1 (never) to 5 (always). The total score ranges between 10 and 50, with higher scores indicating more fatigue. The FAS is a useful measure of post-stroke fatigue because of its adequate face validity, feasibility, high test–retest reliability and high construct validity (Mead et al., Citation2007). The internal consistency of the FAS is usually relatively low because the instrument measures different aspects of fatigue (i.e., mental and physical fatigue) (Mead et al., Citation2007).
Personality traits
Neuroticism and extraversion were assessed using the two corresponding subscales of the Eysenck Personality Questionnaire Revised Short Scale (EPQ-RSS) (Sanderman, Arrindell, Ranchor, Eysenck, & Eysenck, Citation1995). Each scale consists of 12 dichotomised items (yes/no), with a total score ranging from 0 to 12. A higher score indicates more characteristics of the specific personality trait. The EPQ-RSS has demonstrated good internal consistency, test–retest reliability and concurrent validity (Sato, Citation2005).
Coping style
The Utrecht Coping List (UCL; 15-item version) was used to evaluate coping styles (Sanderman & Ormel, Citation1992; Schreurs, Van de Willege, Brosschot, Tellegen, & Graus, Citation1993; van den Akker, Buntinx, Metsemakers, & Knottnerus, Citation2000). The UCL assesses four coping styles: (1) active problem solving (i.e., intervening directly when there are difficulties; considering different solutions to a problem; seeing problems as a challenge); (2) social support seeking (i.e., sharing problems with family and friends; asking for help); (3) avoiding (i.e., trying to avoid difficult situations; hope the problem may solve itself; resigning from the situation); and (4) palliative coping (i.e., looking for distraction; using other activities to keep the mind off a problem; trying to feel better by smoking, drinking alcohol, eating or doing physical exercise). Each item is rated on a 4-point rating scale ranging from 1 (never) to 4 (very often). Total scores are computed for each domain with higher scores indicating a greater tendency to adopt the particular coping style. The UCL has moderate to good internal consistency and test–retest reliability (Schreurs et al., Citation1993).
Covariates
Demographics and stroke-related measures were obtained from the patients’ medical records. Stroke characteristics (type, side and stroke severity, assessed by the National Institutes of Health Stroke Scale (NIHSS) (Brott et al., Citation1989) and discharge destination were recorded by the treating neurologists during hospitalisation for stroke. Standardised neuropsychological testing was used to determine objective cognitive performance and to calculate the Objective Cognitive Impairment (OCI) index score (i.e., total number of impaired (sub-)test scores, range 0–20; a procedure previously described by Davis, Axelrod, McHugh, Hanks, and Millis, Citation2013) and modified for purposes of this study (van Rijsbergen, Mark, Kop, de Kort, & Sitskoorn, Citation2017). The rationale for using this composite index is to reduce the number of covariates in the statistical models and because this index showed a significant association with SCC (van Rijsbergen et al., Citation2013). Self-report data were used to determine the estimated pre-stroke intelligence quotient (IQ) (Dutch version of the National Adult Reading Test (D-NART) (Schmand, Bakker, Saan, & Louman, Citation1991)) and instrumental ADL functioning was assessed using the Frenchay Activities Index (FAI) (Holbrook & Skilbeck, Citation1983).
Statistical analysis
Data are presented as mean ± standard deviation (SD) or frequencies and percentage. The associations between the psychological variables and post-stroke SCC were determined using Pearson product-moment correlations (r). In order to determine which factors were independently associated with SCC, multiple linear hierarchical regression analysis was used. The variables age, sex, IQ (D-NART), stroke severity (NIHSS), objective cognitive performance (OCI-index) and ADL (FAI) scores were included in the first block, and then the added predictive value of each of the four psychological measures was examined in the second block (i.e., four separate covariate-adjusted models for depression, anxiety, perceived stress and fatigue (Models 1a–d). To establish which of the four psychological measures was independently associated with SCC, we tested a model that included these four measures together combined with the aforementioned covariates (Model 2). The additive role of personality traits and coping style was tested in the fully adjusted model, including the background covariates, distress-related psychological factors (depression, anxiety, perceived stress and fatigue), and the personality traits and coping style measures (Model 3). In this fully adjusted model, the four distress-related psychological variables were forced-entered into the model, instead of only the significant variables in less complex models, because we aimed to examine whether the observed association between the distress-related psychological factors and post-stroke SCC (Model 2) changed after multiple psychological covariates (including personality traits and coping styles) were taken into account. To minimise artefacts related to multicollinearity or model overfitting, the background covariates and distress-related psychological measures were first included in the model (forced entry) and forward stepwise procedures were used to examine the role of personality traits and coping style indices. We also conducted exploratory follow-up analyses to examine the independent associations of significant psychological correlates of SCC (obtained Model 2) when adjusting for personality and coping style factors (i.e., “restricted models”).
Regression coefficients (standardised β) are presented to indicate the strengths of the association for each of the separate variables and R2 to describe the amount of variance explained by the model. Two-sided p-values are reported and a p value ≤ .05 was considered to indicate statistical significance. All analyses were performed using SPSS 22.0 software for Windows.
Results
Study sample
Demographic and clinical characteristics are shown in . Most patients had a first-ever ischemic stroke and the severity of symptoms at admission to hospital was generally mild (median NIHSS score 3). The majority of patients (86%) recovered well enough to be discharged to their home environment.
Table 1. Characteristics of the stroke sample.
The mean CLCE scores were 3.3 ± 2.5 for SCC-content, 2.2 ± 2.3 for SCC-worry and 8.6 ± 6.9 for total CLCE-cognitive score. The levels of depression and anxiety were relatively low (mean HADS-D = 5.1 ± 3.8 and mean HADS-A = 4.7 ± 3.9), and the mean perceived stress (PSS-4) score was 5.0 ± 2.7. The mean fatigue (FAS) score was 24.7 ± 6.8. Descriptive statistics of the personality and coping style measures are provided in supplemental Table S1 (supplemental data for this article can be accessed at http://dx.doi.org/10.1080/09602011.2018.1441720). The correlations for demographic and clinical variables with CLCE scores (content, worry and total cognitive score) are shown in supplemental Table S2 (supplemental data for this article can be accessed at http://dx.doi.org/10.1080/09602011.2018.1441720). Pre-stroke IQ, the objective cognitive performance index, and ADL were significantly related to SCC and these factors are adjusted for in multivariate models.
Psychological factors associated with post-stroke SCC (CLCE-content)
Depressive symptoms, anxiety, perceived stress and fatigue were all significantly associated with the CLCE content score in unadjusted analyses ().
Table 2. Associations between psychological factors and SCC (CLCE-content score).
Multivariate linear regression analyses adjusting for age, sex, estimated IQ, stroke severity, OCI-index score and ADL functioning in the first block and each of the distress-related psychological variables in the second block indicated that depression (β = 0.35), anxiety (β = 0.38), perceived stress (β = 0.39) and fatigue (β = 0.39) were associated with the CLCE-content score independent of these covariates (see ; Models 1a–1d).
We then examined which of these four distress-related psychological measures remained independently associated with the CLCE-content score (i.e., when including these four measures together; see , Model 2). This model explained approximately one-third of the variance in CLCE content score (R2 = 0.32; F (10, 146) = 6.99, p < .001), with anxiety (β = 0.23, p = .02) and fatigue (β = 0.27, p = .002) showing independent associations with the CLCE-content score. The association between perceived stress and SCC was in the same direction but was not statistically significant (p = .053).
The role of personality traits and coping styles in SCC
Regarding personality factors, both neuroticism (r = 0.44, p < .001) and extraversion (r = −0.19, p = .01) were correlated with the CLCE-content score in unadjusted models. Significant correlations with the CLCE-content scores were also found for the coping styles avoidance (r = 0.30, p < .001) and an inverse association with active handling (r = −0.32, p < .001), but not social support seeking (r = 0.01 p = .87) and palliative coping (r = 0.12, p = .11). Adjustment for background factors minimally changed the strength of these associations (data not shown).
shows the full multivariate linear regression model (Model 3), examining background factors (age, sex, estimated IQ, stroke severity, objective cognitive impairment and ADL), distress-related psychological factors (depression, anxiety, perceived stress and fatigue), personality traits and coping styles as related to the CLCE-content score. The background covariates were included in the first block (forced entry method), depression, anxiety, perceived stress and fatigue forced in the second block (also using forced entry, parallel to Model 2, see ), and personality factors and coping styles in the third block (forward stepwise method). The overall model explained 34.2% of the variance in CLCE-content scores (R2 = 0.34; F (11, 145) = 6.86, p < .001). Fatigue (β = 0.26, p = .003) and neuroticism (β = 0.21, p = .05) were the only psychological variables that were independently associated with CLCE-content scores in the fully adjusted model, as well as the covariate objective cognitive performance (OCI-index β = 0.20, p = .03).
Table 3. Model 3: full multivariate linear regression model examining background factors, distress-related psychological factors, personality traits and coping styles as related to SCC.
Exploratory follow-up analyses were performed by not including the variables that were non-significantly associated with CLCE-content scores in Model 2 (i.e., only forced entering anxiety and fatigue but not depression and perceived stress). The results of this analysis were essentially the same as the findings of the fully adjusted multivariate model that included these two measures. Specifically, the overall model explained 33.4% of the variance in CLCE-content scores (R2 = 0.33; F (9, 147) = 8.20, p < .001) and the same variables that were significant in the fully adjusted Model 3 remained significant in this “restricted” model, i.e., fatigue (β = 0.27, p = .001), neuroticism (β = 0.24, p = .01) and OCI-index (β = 0.20, p = .03).
Psychological variables associated with the impact of SCC (CLCE-worry)
Significant correlations with CLCE-worry scores were found for depression (r = 0.35, p < .001), anxiety (r = 0.39, p < .001), perceived stress (r = 0.42, p < .001) and fatigue (r = 0.35, p < .001) (see supplemental Table S1; supplemental data for this article can be accessed at http://dx.doi.org/10.1080/09602011.2018.1441720). These associations remained significant when adjusting for age, sex, estimated IQ, stroke severity, objective cognitive impairment and ADL. As for personality factors, only neuroticism (β = 0.41, p < .001) and the coping styles avoidance (β = 0.17, p = .04) and active handling (β = −0.23, p = .01) were related to the CLCE-worry scores after adjustment for the covariates.
In the full multivariate model (Model 3), anxiety (β = 0.27, p = .01), perceived stress (β = 0.25, p = .01) and the objective cognitive performance (OCI-index β = 0.33, p = .001) were the only variables independently associated with CLCE-worry (overall R2 = 0.31; F (10, 147) = 6.53, p < .001) (see ).
Exploratory follow-up analyses excluding the non-significant psychological variables from Model 2 (for CLCE-worry this was depression), revealed similar results (overall R2 = 0.31; F (9, 147) = 7.16, p < .001) with significant variables in this “restricted” model being identical to those in the full multivariate model (anxiety: β = 0.23, p = .01; perceived stress: β = 0.22, p = .02; OCI-index: β = 0.32, p = .001).
Discussion
We found that depression, anxiety, perceived stress and fatigue were all associated with SCC three months after a stroke. When examining these distress-related psychological variables together with personality traits and coping style using multivariate analyses, fatigue and neuroticism were independently related to SCC (content component), in addition to objective cognitive performance. These findings indicate that psychological distress plays a role in SCC and that personality factors, particularly neuroticism, may be a critical factor in the association between these measures of psychological distress with SCC after stroke. This study also shows that the association between fatigue and SCC is independent of personality factors.
Unique to this study is that we explored the relationship of depression in combination with anxiety, perceived stress and fatigue with SCC. Previous studies in this area have primarily focused on depression (Aben et al., Citation2011; Duits et al., Citation2008; Lamb et al., Citation2013; Maaijwee et al., Citation2014; Martin et al., Citation2002; Nijsse et al., Citation2017; Winkens et al., Citation2009; Xiong et al., Citation2011). We confirmed the common finding that post-stroke depressive symptoms are associated with more SCC (Aben et al., Citation2011; Duits et al., Citation2008; Lamb et al., Citation2013; Maaijwee et al., Citation2014; Martin et al., Citation2002; Nijsse et al., Citation2017; Winkens et al., Citation2009; Xiong et al., Citation2011). We add to the literature that anxiety, perceived stress and fatigue are also important in post-stroke SCC. These variables are all markers of psychological distress. When examining these psychological distress-related measures conjointly in one multivariate model, we found that fatigue and anxiety were of particular relevance to SCC, independent of depression (see , Model 2). People with high anxiety levels are more likely to score high on personality traits associated with negative affectivity, such as neuroticism (Jylha & Isometsa, Citation2006). Anxiety was highly correlated with neuroticism in this study (r = 0.71). Date shown in indicate that neuroticism may be a common background factor that partially explains the associations between anxiety, perceived stress and depression with SCC, whereas the relationship between fatigue and SCC was not explained by personality traits. These findings remained consistent when examining alternative statistical models focusing on the distress-related psychological variables that were independently associated with SCC (see Model 2 in ). The present data are consistent with observations by Maaijwee et al. (Citation2014) who found associations between fatigue and SCC in univariate and multivariate models in patients evaluated more than 10 years after a stroke. These findings may suggest that the association between fatigue and SCC is consistent over time. We also found that avoidance coping and active handling were associated with SCC, but these associations were not significant in the fully adjusted multivariate model. Future research is needed to determine whether post-stroke fatigue and psychological traits are potential targets for treatment in stroke patients.
The results related to the impact and worry component of SCC were generally in the same direction as those observed for the content component of SCC. One difference was that for SCC content, the personality trait neuroticism had additive value in explaining SCC, whereas for the worry component of SCC it did not. Anxiety and perceived stress were more important in SCC worry and this might suggest that these two variables are conceptually closely linked to worry and impact of SCC.
In addition to the psychological measures, we also found that the OCI-index, a global measure of cognitive impairment derived from a number of neuropsychological tests, was significantly related to SCC. This association has been reported in previous studies (Narasimhalu et al., Citation2013; van Heugten et al., Citation2007; Xiong et al., Citation2011), but results have been inconsistent, including several studies that did not find a correspondence between objective neuropsychological test performance and SCC (Duits et al., Citation2008; Lamb et al., Citation2013; Wendel et al., Citation2008). Our findings demonstrate that psychological factors play an important role in SCC, also when measures of objective cognitive functioning are taken into account.
The present findings need to be considered in the context of a few limitations of this study. We used a cross-sectional design to explore the associations between psychological factors and SCC. Conclusions about causal pathways can therefore not be drawn. The present study can therefore not disentangle whether psychological distress (as indicated by depression, anxiety, perceived stress and fatigue) represents a reactive state to the stroke, the perceived cognitive impairments or more longstanding personality traits such as neuroticism. The multivariable models indicated that neuroticism may be a common factor for some but not all patients. Many psychological (and biological) factors are mutually reinforcing and linear causal models may not be optimal to understand and intervene in these complex interrelated patient characteristics. Longitudinal follow-up studies and intervention studies are needed to disentangle causal pathways. We considered using structural equation models to determine associations among higher-order factors, but elected to focus on multivariate regression models using psychological measures that can be readily implemented in clinical practice. The present results cannot be generalised to all stroke patients, since the patient sample consisted primarily of individuals with a relatively mild stroke severity (median NIHSS score 3 out of 42), a good outcome (86% of the patients were discharged home) and those with severe communication difficulties (e.g., severe aphasia) were not included. Previous studies, however, found no associations between stroke severity or lesion size and SCC (Xiong et al., Citation2011). There are also several strengths of this study, including the sample size that enabled multivariate analyses of psychological variables relevant to post-stroke SCC and the differentiation between distress-related psychological measures from stable personality traits and coping styles. Furthermore, we used a comprehensive instrument for the assessment of SCC that has been specifically validated in stroke patients.
In conclusion, anxiety, perceived stress and fatigue are strongly and independently associated with post-stroke SCC, in addition to the known relationship between depression and SCC. These associations are stronger than those of stroke-related factors and objective cognitive functioning with SCC. These findings therefore underscore the importance of psychological distress in SCC (Duits et al., Citation2008; Lamb et al., Citation2013). We also found evidence that part of the interrelation between measures of psychological distress and SCC is explained by stable personality traits, particularly neuroticism, that are independent of stroke. The present study also suggests that fatigue may be an important additional target for treatment of post-stroke SCC. Targeted treatment programmes for post-stroke patients with SCC could be patient-tailored based on the patient’s accompanying psychological characteristics. In cases where SCC coincides with depression or other manifestations of psychological distress (e.g., anxiety) cognitive behavioural therapy may be beneficial, focusing on resilience and setting realistic expectations for cognitive functioning based on objective neuropsychological test performance and patients’ past cognitive abilities. If fatigue is a primary factor associated with SCC, interventions with a focus on improving energy levels such as relaxation techniques and improving physical activity may be considered. In patients where personality factors (e.g., neuroticism) are the predominant background factor in SCC (and also psychological distress) it is probably best to initially focus on improving adaptive coping strategies as personality traits per se are often difficult to modify. In many patients, it may be preferable to consider a combination of these interventions, possibly combined with other psychological or pharmacological treatment strategies. In addition, all patients may benefit from psycho-education, physical therapy and cognitive rehabilitation in areas where neuropsychological deficits are found. Such interventions might prove a worthwhile addition to stroke rehabilitation programmes by reducing SCC and improving quality of life.
Supplementary_File
Download PDF (321.3 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aben, I., Denollet, J., Lousberg, R., Verhey, F., Wojciechowski, F., & Honig, A. (2002). Personality and vulnerability to depression in stroke patients: A 1-year prospective follow-up study. Stroke, 33, 2391–2395. doi: 10.1161/01.STR.0000029826.41672.2E
- Aben, L., Ponds, R. W., Heijenbrok-Kal, M. H., Visser, M. M., Busschbach, J. J., & Ribbers, G. M. (2011). Memory complaints in chronic stroke patients are predicted by memory self-efficacy rather than memory capacity. Cerebrovascular Diseases, 31, 566–572. doi: 10.1159/000324627
- Brott, T., Adams, H. P., Olinger, C. P., Marler, J. R., Barsan, W. G., Biller, J., et al. (1989). Measurements of acute cerebral infarction: A clinical examination scale. Stroke, 20, 864–870. doi: 10.1161/01.STR.20.7.864
- Carlsson, G. E., Moller, A., & Blomstrand, C. (2003). Consequences of mild stroke in persons <75 years -- a 1-year follow-up. Cerebrovascular Diseases, 16, 383–388. doi: 10.1159/000072561
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. doi: 10.2307/2136404
- Comijs, H. C., Deeg, D. J., Dik, M. G., Twisk, J. W., & Jonker, C. (2002). Memory complaints; the association with psycho-affective and health problems and the role of personality characteristics. A 6-year follow-up study. Journal of Affective Disorders, 72, 157–165. doi: 10.1016/S0165-0327(01)00453-0
- Davis, A. M., Cockburn, J. M., Wade, D. T., & Smith, P. T. (1995). A subjective memory assessment questionnaire for use with elderly people after stroke. Clinical Rehabilitation, 9(3), 238–244. doi: 10.1177/026921559500900310
- Davis, J. J., Axelrod, B. N., McHugh, T. S., Hanks, R. A., & Millis, S. R. (2013). Number of impaired scores as a performance validity indicator. Journal of Clinical and Experimental Neuropsychology, 35, 413–420. doi: 10.1080/13803395.2013.781134
- de Jonghe, J. F., Schmand, B., Ooms, M. E., & Ribbe, M. W. (1997). Abbreviated form of the informant questionnaire on cognitive decline in the elderly. Tijdschrift voor Gerontologie en Geriatrie, 28, 224–229.
- Duits, A., Munnecom, T., van Heugten, C., & van Oostenbrugge, R. J. (2008). Cognitive complaints in the early phase after stroke are not indicative of cognitive impairment. Journal of Neurology, Neurosurgery, and Psychiatry, 79, 143–146. doi: 10.1136/jnnp.2007.114595
- Galligan, N. G., Hevey, D., Coen, R. F., & Harbison, J. A. (2016). Clarifying the associations between anxiety, depression and fatigue following stroke. Journal of Health Psychology, 21, 2863–2871. doi: 10.1177/1359105315587140
- Holbrook, M., & Skilbeck, C. E. (1983). An activities index for use with stroke patients. Age and Ageing, 12, 166–170. doi: 10.1093/ageing/12.2.166
- Jylha, P., & Isometsa, E. (2006). The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depression and Anxiety, 23, 281–289. doi: 10.1002/da.20167
- Lamb, F., Anderson, J., Saling, M., & Dewey, H. (2013). Predictors of subjective cognitive complaint in post-acute older adult stroke patients. Archives of Physical Medicine and Rehabilitation, 94, 1747–1752. doi: 10.1016/j.apmr.2013.02.026
- Maaijwee, N. A., Schaapsmeerders, P., Rutten-Jacobs, L. C., Arntz, R. M., Schoonderwaldt, H. C., van Dijk, E. J., … de Leeuw, F. E. (2014). Subjective cognitive failures after stroke in young adults: Prevalent but not related to cognitive impairment. Journal of Neurology, 261, 1300–1308. doi: 10.1007/s00415-014-7346-3
- Martin, C., Dellatolas, G., Viguier, D., Willadino-Braga, L., & Deloche, G. (2002). Subjective experience after stroke. Applied Neuropsychology, 9, 148–158. doi: 10.1207/S15324826AN0903_3
- Mead, G., Lynch, J., Greig, C., Young, A., Lewis, S., & Sharpe, M. (2007). Evaluation of fatigue scales in stroke patients. Stroke, 38, 2090–2095. doi: 10.1161/STROKEAHA.106.478941
- Michielsen, H. J., De Vries, J., & Van Heck, G. L. (2003). Psychometric qualities of a brief self-rated fatigue measure: The fatigue assessment scale. Journal of Psychosomatic Research, 54, 345–352. doi: 10.1016/S0022-3999(02)00392-6
- Narasimhalu, K., Wiryasaputra, L., Sitoh, Y. Y., & Kandiah, N. (2013). Post-stroke subjective cognitive impairment is associated with acute lacunar infarcts in the basal ganglia. European Journal of Neurology, 20, 547–551. doi: 10.1111/ene.12032
- Nijsse, B., van Heugten, C. M., van Mierlo, M. L., Post, M. W., de Kort, P. L., & Visser-Meily, J. M. (2017). Psychological factors are associated with subjective cognitive complaints 2 months post-stroke. Neuropsychological Rehabilitation, 27, 99–115. doi: 10.1080/09602011.2015.1065280
- Pearman, A., & Storandt, M. (2004). Predictors of subjective memory in older adults. The Journals of Gerontology, 59, 4–6. doi: 10.1093/geronb/59.1.P4
- Sagen, U., Vik, T. G., Moum, T., Morland, T., Finset, A., & Dammen, T. (2009). Screening for anxiety and depression after stroke: Comparison of the hospital anxiety and depression scale and the Montgomery and Asberg depression rating scale. Journal of Psychosomatic Research, 67, 325–332. doi: 10.1016/j.jpsychores.2009.03.007
- Sanderman, R., Arrindell, W. A., Ranchor, A., Eysenck, H. J., & Eysenck, S. B. G. (1995). Measurement of personality traits using the Eysenck personality questionnaire: A manual. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken, Rijksuniversiteit Groningen.
- Sanderman, R., & Ormel, J. (1992). The Utrecht Coping List (UCL): Validity and reliability. Gedrag en Gezondheid, 20, 32–37.
- Sato, T. (2005). The Eysenck personality questionnaire brief version: Factor structure and reliability. The Journal of Psychology, 139, 545–552. doi: 10.3200/JRLP.139.6.545-552
- Schmand, B., Bakker, D., Saan, R., & Louman, J. (1991). The Dutch adult reading test: A measure of premorbid intelligence. Tijdschrift Voor Gerontologie en Geriatrie, 22, 15–19.
- Schreurs, P. J. G., Van de Willege, G., Brosschot, J. F., Tellegen, B., & Graus, G. M. H. (1993). The Utrechtse coping list: UCL manual [Dutch]. Utrecht: Swets en Zeitlinger.
- Spinhoven, P., Ormel, J., Sloekers, P. P., Kempen, G. I., Speckens, A. E., & Van Hemert, A. M. (1997). A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychological Medicine, 27, 363–370. doi: 10.1017/S0033291796004382
- van den Akker, M., Buntinx, F., Metsemakers, J. F., & Knottnerus, J. A. (2000). Marginal impact of psychosocial factors on multimorbidity: Results of an explorative nested case-control study. Social Science & Medicine, 50, 1679–1693. doi: 10.1016/S0277-9536(99)00408-6
- van Heugten, C., Rasquin, S., Winkens, I., Beusmans, G., & Verhey, F. (2007). Checklist for cognitive and emotional consequences following stroke (CLCE-24): Development, usability and quality of the self-report version. Clinical Neurology and Neurosurgery, 109, 257–262. doi: 10.1016/j.clineuro.2006.10.002
- van Rijsbergen, M. W., Mark, R. E., de Kort, P. L., & Sitskoorn, M. M. (2013). The COMPlaints after stroke (COMPAS) study: Protocol for a Dutch cohort study on poststroke subjective cognitive complaints. BMJ Open, 3, e003599. doi: 10.1136/bmjopen-2013-003599
- van Rijsbergen, M. W., Mark, R. E., de Kort, P. L., & Sitskoorn, M. M. (2014). Subjective cognitive complaints after stroke: A systematic review. Journal of Stroke and Cerebrovascular Diseases, 23, 408–420. doi: 10.1016/j.jstrokecerebrovasdis.2013.05.003
- van Rijsbergen, M. W., Mark, R. E., de Kort, P. L., & Sitskoorn, M. M. (2015). Prevalence and profile of poststroke subjective cognitive complaints. Journal of Stroke and Cerebrovascular Diseases, 24, 1823–1831. doi: 10.1016/j.jstrokecerebrovasdis.2015.04.017
- van Rijsbergen, M. W. A., Mark, R. E., Kop, W. J., de Kort, P. L., & Sitskoorn, M. M. (2017). The role of objective cognitive dysfunction in subjective cognitive complaints after stroke. European Journal of Neurology, 24, 475–482. doi: 10.1111/ene.13227
- Warttig, S. L., Forshaw, M. J., South, J., & White, A. K. (2013). New, normative, English-sample data for the short form perceived stress scale (PSS-4). Journal of Health Psychology, 18, 1617–1628. doi: 10.1177/1359105313508346
- Wendel, K., Risberg, J., Pessah-Rasmussen, H., Stahl, A., & Iwarsson, S. (2008). Long-term cognitive functional limitations post stroke: Objective assessment compared with self-evaluations and spouse reports. International Journal of Rehabilitation Research, 31, 231–239. doi: 10.1097/MRR.0b013e3283021912
- Winkens, I., Van Heugten, C. M., Fasotti, L., & Wade, D. T. (2009). Reliability and validity of two new instruments for measuring aspects of mental slowness in the daily lives of stroke patients. Neuropsychological Rehabilitation, 19, 64–85. doi: 10.1080/09602010801913650
- Xiong, Y. Y., Wong, A., Mok, V. C., Tang, W. K., Lam, W. W., Kwok, T. C., … Wong, L. K. (2011). Frequency and predictors of proxy-confirmed post-stroke cognitive complaints in lacunar stroke patients without major depression. International Journal of Geriatric Psychiatry, 26, 1144–1151.
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x