?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
In this multicentre randomised controlled trial (RCT), 43 patients with Parkinson’s disease (PD) were randomly allocated to either the experimental condition receiving cognitive rehabilitation including strategy training (ReSET; Strategic Executive Treatment, n = 24) or to the control condition receiving computerised repetitive practice training for attention (Cogniplus, n = 16). We expected that strategy training (ReSET) would be more effective than cognitive training (Cogniplus) in improving patients’ everyday life executive functioning. Neuropsychological assessment was administered at baseline, at 2 weeks and 3–5 months post-treatment. Primary outcome measure was the Role Resumption List (RRL). Secondary outcome measures were treatment goal attainment (TGA), Dysexecutive Questionnaire (DEX), Parkinson’s Disease Questionnaire (PDQ-39), Zarit Burden Interview (ZBI) and neuropsychological tests. No effects of treatment were found on the primary outcome measure and on neuropsychological tests, except for one test of attention. At 2 weeks and 3–5 months post-treatment, PD patients in both the ReSET and Cogniplus group reported a significant improvement in everyday life executive functioning, as measured with TGA and the DEX-self, with an advantage for ReSET only shortly after treatment. Given these results and that PD patients were able to adhere to these treatments despite their motor symptoms and fatigue (i.e., the drop-out rate was small), we conclude that both strategy training and cognitive training for impairments in EF might be beneficial and feasible for PD patients.
Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder that is characterised by motor symptoms. Impairments in cognitive domains such as attention, memory visuospatial functions and executive functions (EF) are also common in PD (Elgh et al., Citation2009; Muslimovic, Post, Speelman, & Schmand, Citation2005). In particular, impairments of executive functions (EF) are frequently found and can already be present in the early stages of the disease (Kudlicka, Clare, & Hindle, Citation2011; McKinlay, Grace, Dalrymple-Alford, & Roger, Citation2010).
EF are higher order functions that control more basic cognitive processes like attention or memory. EF is an umbrella term that incorporates several functions such as planning, regulation and initiation of behaviour, time management and self-awareness (Vlagsma et al., Citation2015; Ylvisaker, Citation1998). These functions enable us to behave in a goal-directed way in non-routine and complex everyday life tasks and to anticipate unforeseen circumstances. Previous studies have shown that impairments in EF can lead to reduced independence in everyday life functioning and to a lower quality of life (QoL) (Kudlicka, Clare, & Hindle, Citation2014; Lawson et al., Citation2014).
In neurological populations other than PD, e.g., acquired brain injury (ABI), it is common practice to offer patients neuropsychological rehabilitation programmes for impairments in executive functioning (Krasny-Pacini, Chevignard, & Evans, Citation2013). For patients with PD, neuropsychological rehabilitation is not part of standard therapy. This is surprising as the profile of executive dysfunctions and reported needs and aims regarding neuropsychological rehabilitation of PD patients are comparable to patients with ABI (Vlagsma et al., Citation2015). Moreover, because PD patients report that their impairments in EF are at least as restrictive as their motor symptoms (Klepac, Trkulja, Relja, & Babic, Citation2008) and since they have to cope with these impairments for a large part of their life, neuropsychological rehabilitation for impairments in EF could be particularly valuable to maintain patients’ independence in everyday life for as long as possible.
In the last decade an increasing number of studies were conducted on neuropsychological rehabilitation in PD. However, to date only four studies investigated the effectiveness of cognitive interventions that specifically aimed to improve impairments in EF in PD patients (Mohlman et al., Citation2010; Mohlman, Chazin, & Georgescu, Citation2011; Reuter, Mehnert, Sammer, Oechsner, & Engelhardt, Citation2012; Sammer, Reuter, Hullmann, Kaps, & Vaitl, Citation2006). These studies focused primarily on cognitive training, which involves repetitive practice of (computerised) tasks aimed at enhancing underlying cognitive functions. Importantly, these studies unanimously concluded that cognitive training for deficits in EF is feasible and beneficial for PD patients (Calleo et al., Citation2012). Another five RCT studies were conducted on cognitive training in PD. These more general studies targeted a broader range of cognitive functions including EF (Cerasa et al., Citation2014; Paris et al., Citation2011; Pena et al., Citation2014; Petrelli et al., Citation2014; Zimmermann et al., Citation2014). The results of these randomised controlled trials showed that cognitive training led to an overall significant improvement of PD patients’ performance on neuropsychological test measures for EF. However, no evidence was found for generalisation of improvement to patients’ everyday life functioning (Calleo et al., Citation2012; Leung et al., Citation2015). In two recent studies of Pena et al. (Citation2014) and Reuter et al. (Citation2012) PD patients received a skill training in addition to cognitive training. The skill training involved guided and repetitive practice of specific activities in everyday life. Only Reuter et al. (Citation2012) included in addition to neuropsychological test measures, outcome measures that were related to functioning in everyday life. They found that after treatment, PD patients had improved in terms of their QoL, functioning on treatment goals, self-confidence and employment of a more active life style. For patients with TBI, the use of cognitive rehabilitation programmes that are based on strategy training is highly recommended for improving impairments in EF in everyday life, whereas cognitive training solely based on repetitive practice is not (Cicerone et al., Citation2011). Strategy training aims at teaching patients cognitive strategies that help them compensate the cognitive impairments they encounter in their everyday life activities. A large number of studies found solid evidence for the effectiveness of such intervention programmes, even in the long term (Tate et al., Citation2014). For example, Spikman, Boelen, Lamberts, Brouwer, and Fasotti (Citation2010) showed effectiveness of EF strategy training that lasted at least six months post-treatment. They found that ABI patients who received strategy training resumed their previous roles in everyday life more often, showed more improvement with regard to setting and accomplishing realistic goals and showed better planning and regulation abilities than patients who received computerised cognitive training. However, patients in both groups showed no improvement on neuropsychological tests for EF or attention, which led the authors to conclude that although these tests may be sensitive to impairments, they are not sensitive to changes due to treatment. Recently, Foster, Spence, and Toglia (Citation2017) investigated the feasibility of an individualised cognitive strategy training in a case series of seven non-demented patients with PD. Patients evaluated this intervention as being acceptable and engaging, corroborating its feasibility. Although this study did not aim to evaluate the effectiveness of the intervention, patients also reported improvement on a scale for performance and satisfaction of everyday life tasks, which is promising. However, the cognitive targets for treatment were not specified in this study. Given that strategy training has a positive effect on indications of everyday life EF in ABI patients and the findings of the study of Foster et al. (Citation2017) in PD patients, it is surprising that the effect of strategy training on everyday life executive impairments has not yet been examined in PD patients. Therefore, the main goal of the present study was to investigate the effectiveness of a cognitive rehabilitation programme based on strategy training (ReSET; Strategic Executive Treatment) on everyday life executive functioning, level of participation and QoL in patients with PD, both immediately after treatment and in the longer term. In a RCT design we compared this cognitive rehabilitation programme based on strategy training to a computerised cognitive training for attention and working memory (Cogniplus). Attention and working memory are basic cognitive functions, which are also necessary when performing complex executive tasks. We hypothesise that Cogniplus may lead to improved performance on neuropsychological tests for aspects of EF, but will not translate into improved executive functioning in everyday life. This is in contrast to ReSET of which we expect that it will lead to improvement in everyday life executive functioning. A second goal was to investigate whether cognitive rehabilitation based on strategy training was also feasible for PD patients. When compared to ABI patients, motor impairments and fatigue might have a stronger negative impact on their abilities to follow outpatient treatment and to practice with assignments at home.
Methods
Study design and procedure
This study was conducted in three medical centres in the Netherlands: University Medical Center Groningen (UMCG), Maastricht University Medical Center (MUMC) and Nij Smellinghe Drachten. The study was approved by the ethics review board (ERB) of the UMCG and was conducted in accordance with the declaration of Helsinki.
Patients were eligible for participation in this study when they were aged between 18 and –80 years, diagnosed with PD according to the UK Parkinson’s Disease Brain Bank Criteria and had a disease severity ≤ Hoehn & Yahr (H&Y: Hoehn & Yahr, Citation1967) stage 3, i.e., patients had to be mobile in order to visit one of the medical centres on a weekly basis for at least three months. Furthermore, patients had to be 1) motivated for treatment; 2) had to report problems with EF in everyday life they experienced as burdensome (based on semi-structured interview and/or a total score of ≥18 on the Dysexecutive Questionnaire (DEX: Burgess, Wilson, Evans, & Emslie, Citation1996); and/or 3) had impairments on objective neuropsychological tests of EF. Impairments were defined as: a standard score of ≤2 on the subtests Zoo Map Test or Six Elements Test of the Behavioural Assessment of the Dysexecutive Syndrome (BADS: Burgess et al., Citation1996) and/or a standard age total score on the BADS categorised as ‘low average’ or lower and/or a discrepancy of 15 points between standard age score and premorbid IQ as measured with the short version of the Dutch Groninger Intelligence Test (Luteijn & van der Ploeg, Citation1983). Exclusion criteria were severe neurological and psychiatric comorbidity including dementia (i.e., SCales for Outcomes in PArkinson’s disease-COGnition scale score ≤17 (Verbaan et al., Citation2011)). The above-mentioned tests and questionnaires were part of an extensive neuropsychological assessment. Results of this assessment were used as the baseline measurement (T0) when patients were found to be eligible for participation in accordance with the inclusion criteria.
Eligible patients were randomly assigned to either the experimental (ReSET) or control (Cogniplus) treatment by drawing lots. In order to balance the allocation of patients to both treatment conditions, lots were drawn per 4 patients (i.e., 2 experimental and 2 control condition). A coworker who was not actively involved in the study was responsible for the drawing of lots.
Both ReSET and Cogniplus consisted of 14 one-hour sessions; once a week or if possible twice a week. Patients were assessed with a neuropsychological test battery (i.e., interview, tests and questionnaires) at three time- points: baseline (T0), 2 weeks post-treatment (T1) and 3–5 months after the last treatment session (T2). Well-trained test assistants, who were blind for the treatment condition, administered the tests.
Participants
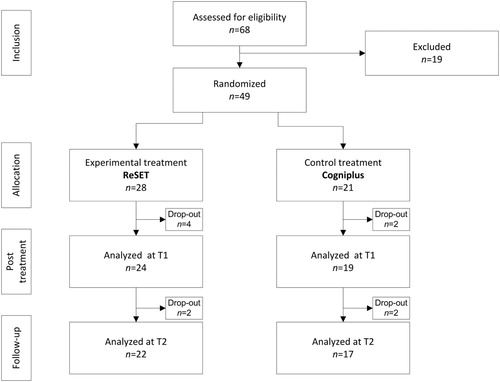
Forty-nine PD patients were included (UMCG: n = 33,MUMC: n = 8,Nij Smellinghe: n = 8). Six patients dropped out during the treatment period: two because of physical disabilities and four patients because of loss of motivation. Therefore, 43 patients (ReSET:n = 24, Cogniplus:n = 19) completed the treatment and post-treatment assessment (T1; ). Another four patients dropped out 3–5 months post-treatment assessment (T2): one patient had developed severe psychiatric comorbidity, one patient stated after four sessions that he considered himself to be sufficiently improved as he had no complaints anymore and therefore felt no necessity to continue the treatment and two patients could not complete assessment because of logistic reasons. Thirty-nine patients thus completed the study protocol ().
Disease severity was determined with the Unified Parkinson’s Disease Rating Scale motor part (UPDRS-III) and H&Y scale. A Levodopa Equivalent Daily Dose (LEDD; Esselink et al., Citation2004) score was calculated for all patients who were on dopaminergic treatment. Three patients were not on dopaminergic treatment, for two patients medication use was not reported and four patients received Deep Brain Stimulation (DBS) in addition to dopaminergic treatment. Surgery was performed at least one year prior to study inclusion. Patients on dopaminergic treatment were in the on phase during treatment and neuropsychological assessment. presents descriptive variables and disease characteristics of both treatment groups. No differences were found between treatment groups regarding age, disease duration and disease severity.
Table 1. Descriptive and disease characteristics of PD patients in both treatment groups.
Furthermore, a healthy control group (n = 90) was included to determine whether the PD patients showed impairments in EF at baseline compared to healthy controls. shows that both groups were comparable as there were no differences with regard to age, gender, premorbid IQ and level of education. However, at baseline PD patients reported significantly more symptoms of anxiety and depression on the Hospital Anxiety and Depression Scale (HADS: Zigmond & Snaith, Citation1983) than healthy controls.
Table 2. Descriptive characteristics of PD patients and healthy controls.
Experimental treatment ReSET: strategic executive treatment
ReSET is an individual treatment, given by experienced neuropsychologists. The aim is to improve or stabilise the level of independence and QoL, by teaching patients strategies to compensate for impairments in EF in everyday life situations. These strategies allow patients to tackle everyday life situations in a systematic and structured way, by formulating their intentions and actions explicitly in terms of goals and sub goals (planning) and effectively executing these plans, while monitoring their behaviour.
The content of the treatment protocol is based on the ‘Multifaceted treatment program’ of Spikman et al. (Citation2010) and targets several aspects of EF as defined by Ylvisaker (Citation1998): self-awareness, goal setting, planning, initiation and monitoring of behaviour, flexibility and strategic behaviour. Adjustments were made to the protocol of Spikman et al. (Citation2010) in order to make it more feasible for patients with PD. The number of sessions was reduced from 24 to 14. There were also fewer exercises per session as PD patients’ psychomotor tempo is often reduced (Vlagsma et al., Citation2016).
The ReSET protocol consisted of 14 one-hour sessions that were grouped into three modules. The first module ‘Information and awareness’ consisted of three sessions aimed at increasing patients’ insight into their executive dysfunctions and the consequences of these dysfunctions in everyday life. This was achieved by giving psycho-education to patients and their relatives and evaluating patients’ strengths and weaknesses based on their performance on the neuropsychological assessment. In the third session, patients were asked to formulate three individual goals related to executive functioning that could be improved through the treatment (Vlagsma et al., Citation2015) and were asked to rate their level of functioning regarding these goals.
The second module ‘Goal setting and planning' consisted of six sessions based on the General Planning Approach (GPA: Spikman et al., Citation2010). The GPA teaches patients to structure the planning and execution of activities by formulating a concrete goal and explicitly describing the actions that need to be carried out in order to achieve the goal in a step-by-step manner, the estimated time per action and the materials needed for accomplishing the goal. Furthermore, patients were taught to make a realistic and energy balanced day-to-day and week planning and learned to adjust their planning to their individual fluctuating energy level. Also they were taught how to use an organiser properly. Therapists’ assistance was gradually reduced over sessions. Homework involved mostly the execution of activities that were planned during the session. The homework assignments were evaluated at the beginning of each session.
The third module ‘Initiative, execution and regulation”’ consisted of five sessions. While in the second module the emphasis lay on the planning process, this module focused more on the execution of the plan. During these sessions, Goal Management Training (GMT; Levine et al., Citation2000) plays a central role in which patients are taught to build in a self-control mechanism that helps them to ‘keep on track’ and actually achieve their goals as planned. Furthermore, attention was given to making the initiation of a plan easier by using external aids (e.g., organiser, alarm).
Control treatment cogniplus
The training protocol of Cogniplus (Schuhfried, Citation2007) consisted of 14 one-hour sessions. Within these sessions six subtests of the computer training programme Cogniplus were individually administered to patients. Five subtests aimed at training aspects of attention (i.e., alertness, selective attention, divided attention and vigilance) and one subtest aimed at training working memory. For the rest of this paper, the control treatment is referred to as ‘Cogniplus’. The programme is basically self-supporting; however, a psychological test assistant was present to provide technical support if necessary. Each aspect of attention and working memory was trained with a separate task. During each session, patients performed three different tasks and trained different aspects of attention and working memory. This ensured that sessions remained challenging. Patients who received the computer training were also asked to formulate three individual executive goals during the third session and were asked to rate their level of functioning regarding their goals at baseline and post-treatment assessments.
Measures
All measures were administered at baseline, 2 weeks and 3–5months post-treatment, with exception of the Rey Auditory Learning Test (RAVLT: Deelman, Brouwer, van Zomeren, & Saan, Citation1980), which was only used at baseline.
Primary outcome measure
Interview
The Role Resumption list (RRL: Spikman et al., Citation2010) is a semi-structured interview that measures patients’ level of participation in different societal domains (i.e., work, social relations, leisure activities and mobility; max. score = 16). At all time-points patients were asked to compare their current level of participation to their participation level before diagnosis. A higher score reflects a lower level of participation.
Other outcome measures
Neuropsychological test measures EF
EF were assessed with the Trail Making Test B/A ratio (TMT B/A: Reitan, Citation1958), the Visual Elevator subtest of the Test of Everyday Attention (TEA; number correct: Robertson, Ward, Ridgeway, & Nimmo-Smith, Citation1994) and the Behavioural Assessment of the Dysexecutive Syndrome (BADS; age score: Wilson, Alderman, Burgess, Emslie, & Evans, Citation1996). Of the BADS subtests, the complex Zoo map subtest (total score) was also independently analyzed.
Attention and memory functions
The Trail Making Test A (TMT A: Reitan, Citation1958) was used to measure selective attention and the RAVLT (Deelman et al., Citation1980), a verbal memory test, measured immediate recall (IR) and delayed recall (DR).
Rating of goal attainment
Treatment goal attainment (TGA; Spikman et al., Citation2010) was used to measure treatment effectiveness as experienced by the patients. During the third session of each treatment, patients had formulated three personal goals which were related to executive dysfunctions in everyday life. Pre- and post-treatment, patients rated their level of functioning on these goals on a 10-point scale (10 = max., per assessment the mean score of three goals was used). At both post-treatment assessments, patients rated their level of functioning again (TGA: per assessment the mean score of three goals).
Questionnaires
The Dysexecutive Questionnaire (DEX; total score: (Burgess et al., Citation1996) was used to assess problems in executive functioning in everyday life. The questionnaire was completed by participants (i.e., self-version) and patients’ significant others (i.e., proxy version). Healthy controls completed only the self-version of the DEX. A higher score reflects more problems with executive functioning in everyday life.
The Brock Adaptive Functioning Questionnaire (BAFQ: Dywan, Citation1996) was used to measure aspects of adaptive functioning. Both a self and a proxy version were used. For the purpose of this study, only the scales related to EF were used (i.e., ‘Planning’, ‘Initiative’, ‘Flexibility’, ‘Excess caution’ and ‘Impulsivity’). A mean total score of these subscales was calculated. A higher score represented more complaints.
In order to assess patients’ health-related QoL, the Parkinson Disease Questionnaire (PDQ-39; total score (Jenkinson, Fitzpatrick, Peto, Greenhall, & Hyman, Citation1997)) was used. A higher score indicated a lower level of QoL.
Caregiver burden was assessed with the short form of the Zarit Burden Interview (ZBI; total score: Zarit, Orr, & Zarit, Citation1985), which was completed by patients’ significant others. A higher score was related to a higher caregiver burden.
Statistical analyses
IBM Statistical Package for the Social Sciences version 22 was used for data analyses. Independent samples t-tests and non-parametric tests were used to compare descriptive and disease characteristics between PD patients and controls and between treatment groups. Independent samples t-tests were also used to compare performances on neuropsychological tests of 1) PD patients in the experimental condition and patients in the control condition at T0; and 2) PD patients and healthy controls at T0. Treatment effects were analyzed with repeated measures ANOVAs. This univariate analysis was chosen in order to minimise data loss due to missing values. The dependent variables were the RRL, TGA, DEX-self, DEX-proxy, BAFQ EF-self, BAFQ EF-proxy, TMT B/A, BADS age score, TEA visual elevator, TMT A, PDQ-39 and ZBI. Possible time and interaction effects of the treatment conditions with respect to these outcome measures were analyzed in two steps: T1 versus T0 and T2 versus T0. In addition, the effect sizes (partial-eta-squared) were calculated. An effect size of 0.01 was labelled as small, 0.06 as medium and 0.14 as large (Fritz, Morris, & Richler, Citation2012). For statistical analyses an alpha of 0.05 was applied. At T2 the percentage of missing values was 15.4% for the primary outcome measure (RRL), 17.9% for the ZBI, 15.4% for the TEA map search, 10.3% for the BAFQ proxy version and 2.6% at maximum for the other outcome measures. This was mainly due to logistic reasons within one of the participating centres.
Results
Comparisons at baseline
shows that PD patients reported significantly more problems at baseline (T0) with executive functioning in everyday life than healthy controls. Furthermore, it was found that PD patients’ performance was significantly lower on objective tests of EF and attention compared to healthy controls.
and show that there were no significant differences at T0 between the experimental (ReSET) and control (Cogniplus) group with regard to descriptive and disease characteristics, global level of cognitive functioning (SCOPA-COG), symptoms of anxiety and depression and any of the outcome measures.
Table 3. Baseline performance of PD patients in both treatment conditions on primary and secondary outcome measures.
Effects of treatment
shows the results of the repeated measures analyses of T1 versus T0. No difference was found between T0 and T1 or between groups on the primary outcome measure (RRL). Also, small effect sizes were found for these comparisons. Patients in both treatment conditions reported a significant improvement of functioning related to their treatment goals (TGA) at T1, with patients in the ReSET condition showing a significantly greater improvement than patients in the Cogniplus condition (large to medium effect sizes, respectively). Furthermore, at T1 both treatment groups showed a significant reduction of problems on the DEX-self compared with T0, with patients in the ReSET condition showing a significantly larger reduction than patients in the control condition (medium effect size). In both groups at T1, patients’ significant others did not report a reduction of problems on the DEX-proxy compared with T0. No differences were found regarding the performances on the neuropsychological tests, BAFQ-self and proxy version, PDQ-39 and Zarit.
Table 4. Results of repeated measures analyses comparing performances on all outcome measures between T1 and T0 for the experimental and control groups.
shows the results of the repeated measures analyses of T2 versus T0. No difference was found between T0 and T2 and between groups on the RRL (medium and small effect sizes, respectively). Furthermore, patients in both treatment conditions still reported a significant improvement at T2 of TGA compared with T0 (large effect sizes). However, there is no difference between the groups (medium effect size). At T2 the number of problems reported on the DEX-self in both treatment groups was also significantly reduced compared with T0, but there was no significant difference between the groups (large to small effect sizes, respectively). In both groups, patients’ significant others did not report a reduction of the problems on the DEX-proxy at T2 compared with T0 (medium effect size). Regarding the performances on neuropsychological tests, only a significant interaction was found for the Visual elevator. For both treatment groups no time or interaction effects were found on the BAFQ-self and proxy version, PDQ-39 and Zarit at T2.
Table 5. Results of repeated measures analyses comparing performances on all outcome measures between T2 and T0 for the experimental and control groups.
Discussion
This is the first RCT that studied the effectiveness of a strategy training (ReSET) for improving EF in everyday life, level of participation and QoL in patients with PD. Recent studies concluded that cognitive training is feasible and beneficial for PD patients with EF deficits. However, these studies evaluated protocols that were primarily based on cognitive training (i.e., repetitive practice of (computerised) tasks in order to strengthen EF) but restricted their measurement of treatment outcome to performances on neuropsychological tests. Hence, it remained unclear whether there was an effect of treatment on everyday life executive functioning of PD patients and whether this lasted over time. Foster et al. (Citation2017) recently showed that also strategy training is feasible for PD patients; however, the effectiveness of their intervention was not investigated. The primary aim of the current study was to investigate whether a strategy training for EF, called Reset, would improve PD patients’ functioning in everyday life more than a cognitive training (Cogniplus) and whether this effect would last over time.
Unfortunately, ReSET did not lead to overall improvement on measures of everyday life executive functioning in the long term. However, immediately after treatment patients in the strategy training group (ReSET) reported to have attained their goals to a larger extent and to have experienced fewer executive complaints than patients in the control condition receiving cognitive computerised training (Cogniplus). At follow-up this group difference had disappeared although both patient groups still reported improvement compared to pre-treatment functioning on both, relatively subjective measures (i.e., goals and DEX questionnaire). We found no changes on other measures of everyday life executive functioning or on neuropsychological tests for EF for both treatment groups after treatment. The drop-out rate during treatment was relatively small (n = 6), showing that the majority of PD patients with a relatively mild disease severity (H&Y I-III) were able to complete the treatment programmes in an outpatient setting. This underlines the finding of Foster et al. (Citation2017) that, as with cognitive training, also cognitive rehabilitation programmes based on strategy training can be feasible for PD patients.
We did not find significant effects of ReSET and Cogniplus on the primary outcome measure, the RRL. This measure was chosen because it had been proved to be a valid measure of the effectiveness of EF strategy training on participation level of ABI patients in a previous study (Spikman et al., Citation2010). In the present study, however, PD patients showed no improvement with regard to their level of participation (work, social relations, leisure and mobility) irrespective of the type of treatment they received. There are several explanations for this lack of result. First, the RRL assesses participation by requiring patients to compare their current participation level to a previous level in the period prior to the diagnosis of PD. In contrast to patients with ABI, for PD patients the moment of onset of the disease is not always clear-cut since the majority of patients were diagnosed after a long period (sometimes years) of having gradually progressing symptoms. Furthermore, for many patients reporting a decreased participation with regard to work, social activities, leisure or mobility this was not always clearly related to cognitive dysfunction; patients indicated that motor impairments and fatigue had a significant negative influence as well. In addition, the majority of patients were already unemployed pre-treatment, either because they had already reached their retirement age (the PD patients were on average older than the ABI group in the study of Spikman et al., Citation2010) or because they had quit their job before retirement age because of Parkinson related symptoms. For these patients, functioning on the work-subscale of the RRL could not be rated, narrowing the score range substantially. For these reasons, we deem the RRL far less suitable and less sensitive to measure changes in participation in PD patients than had been the case for ABI patients.
At baseline, the PD patients showed impairments on all neuropsychological tests for EF and attention, when compared to healthy controls. PD patients also reported significantly more problems with executive functioning in everyday life (DEX) than healthy controls. Furthermore, at baseline the ReSET and Cogniplus group did not differ with regard to demographic and disease characteristics, performance on objective neuropsychological tests and the number of problems with EF in everyday life, level of participation and QoL. Thus, prior to treatment both treatment groups did not differ from each other, which indicates that differences between groups found after treatment cannot be explained by differences between the groups at baseline.
The finding that patients in both treatment groups reported some improvement on two subjective indications of executive functioning, with a slight advantage for the ReSET group directly after treatment but that disappeared at follow-up, strongly suggests that patients subjectively experienced some benefit of treatment. However, for both groups the significant others of the PD patients did not report to have observed a reduction of the EF problems that patients exhibit in everyday life. This contrast suggests that the reduction of problems that patients experience is not visible to others and may indicate merely that patients have attained a higher level of control and self-efficacy, i.e. that they have gained more confidence in their ability to plan and execute everyday life tasks, regardless of whether this is actually the case. Since previous studies have demonstrated that perceived self-control and self-efficacy matter when it comes to dealing with a chronic illness such as PD in relation to well-being, we deem this a relevant finding (Kuijer & De Ridder, Citation2003; Rosqvist et al., Citation2016; Thombs, Kwakkenbos, Riehm, Saadat, & Fedoruk, Citation2017).
Nevertheless, we could not demonstrate that ReSET or Cogniplus resulted in significant improvement of PD patients’ QoL or in a decrease of their caregivers’ burden. Given that PD patients’ functioning will gradually deteriorate over time because of the neurodegenerative character, one could also argue that finding no change in QoL and caregivers’ burden over time is in fact a positive outcome. An additional explanation for lack of change regarding caregiver burden may be that the average caregivers’ reported burden before treatment was already rather low (M = 8.92–11.00; max. 48), which reduces the possibility to find improvement on this measure.
With regard to neuropsychological tests for EF, a significant interaction effect was found at 3–5 months post-treatment on the TEA Visual elevator test. Contrary to our expectation, patients who received ReSET showed a slightly better performance than at baseline, whereas the performance of the control group had worsened. This finding is hard to explain, because if improvement on such a task was expected this would be the case for those patients who received the attention training in the Cogniplus protocol. Furthermore, for both treatment groups we did not find improved performance after treatment on the other neuropsychological tests for EF and attention. Previous studies that examined cognitive training in PD sometimes showed improvement on neuropsychological tests (Calleo et al., Citation2012; Leung et al., Citation2015). However, it has been demonstrated that cognitive training that primarily aims at improving specific cognitive functions only leads to improvement on neuropsychological measures that bear great resemblance to the tasks that were used in the treatment (near-effects), whereas only rarely has improvement been found on other neuropsychological tests or on measures for everyday life functionig (far-effects) (Cicerone et al., Citation2011). However, the primary aim of ReSET in this study was to teach patients compensatory strategies in order to better cope with their impairments in EF in everyday life. Hence, we expected not to find changes on neuropsychological tests for EF. Even more so, these tests are considered to be less sensitive to changes in functioning because they have to be complex and new to require the use of EF, which will not be the case when used for repeated assessment.
The current study has some limitations that need to be mentioned. First, only patients with a mild to moderate disease severity (H&Y stage 1 to 3) were included. However, in more severely impaired patients (H&Y stage 4 and 5) it is very likely that cognitive impairments will become more frequent and more severe, and that the percentage of patients who develop dementia will increase. We expect that cognitive rehabilitation aimed to learn and apply a strategy will be too demanding for the cognitive capacities of this subgroup. Possibly, these patients can still benefit from skill training (i.e., training of specific activities), which offers more structure. This is an interesting topic for future studies. In general, the sample size was small, which had a negative influence on the power. However, compared to previous studies on neuropsychological rehabilitation in PD patients, the sample sizes are relatively large. Another limitation is that at T2 the percentage of missing values was unfortunately high for some outcome measures. Consequently, it might be that significant results were not found due to a lack of power. Furthermore, another limitation pertaining to the amount of time spent on training was not equal for both conditions. Even though both ReSET and Cogniplus consisted of 14 one-hour sessions, patients in the ReSET group had to spend additional time because practising the planning and execution of everyday activities in their home environment was an important element of the strategy training, whereas patients in the Cogniplus group could only practise during the session itself.
In conclusion, this study demonstrates that PD patients with a mild disease severity (H&Y ≤ 3) were able to adhere to a neuropsychological rehabilitation programme, despite otheir motor symptoms and fatigue, as indicated by the low drop-out rate. This indicates that participating in the treatment programmes ReSET, and Cogniplus, is feasible for this group of PD patients. With regard to the effectiveness of both treatment programmes, the results of the present study show that both cognitive rehabilitation including strategy training (ReSET) and cognitive training (Cogniplus) lead to some self-reported subjective improvement of executive functioning in everyday life, with a slight advantage of ReSET directly after treatment compared to the Cogniplus. This suggests that patients subjectively experienced some benefit of neuropsychological rehabilitation in general (i.e., may seem to have attained a higher level of control and self-efficacy regarding executive functioning in everyday life), even though this was not visible to their significant others.
Because of the neurodegenerative character of PD, future research should focus on determining up to which point in the progression of the disease patients are actually able to learn and benefit from cognitive rehabilitation programmes based on strategy training. A large number of patients will eventually develop a dementia (Vasconcellos & Pereira, Citation2015), which means that providing external structure will become more and more important when the disease progresses. Therefore, we deem it worthwhile to involve caregivers more intensively during treatment sessions, so they can gradually increase their assistance in structuring patients’ everyday life activities over time. Furthermore, because of the heterogeneity and complexity of the disease, it is highly important to tailor treatment programmes to patients’ individual needs for use in clinical practice. Finally, because of the progressive character of PD, which leads to deterioration of patients’ physical and cognitive functioning in everyday life, not only improvement of PD patient’ level of everyday life functioning should be considered a desirable outcome of neuropsychological rehabilitation, but also a stabilisation of their level of functioning for a longer time-period than would be the case for patients who do not receive treatment would be advantageous.
Geolocation information
This study was conducted in three medical centres in the Netherlands: 1) the University Medical Center Groningen located in Groningen, the Netherlands; 2) Nij Smellinghe a medical centre located in Drachten, the Netherlands; and 3) Maastricht University Medical Center located in Maastricht, the Netherlands.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Burgess, P. W., Wilson, B. A., Evans, J. J., & Emslie, H. (1996). In B. A. Wilson, N. Alderman, P. W. Burgess, H. Emslie, & J. J. Evans (Eds.), The dysexecutive questionnaire. Bury St. Edmunds: Thames Valley Test Company.
- Calleo, J., Burrows, C., Levin, H., Marsh, L., Lai, E., & York, M. K. (2012). Cognitive rehabilitation for executive dysfunction in Parkinson’s disease: Application and current directions. Parkinson’s Disease, 2012, 512892. doi: 10.1155/2012/512892
- Cerasa, A., Gioia, M. C., Salsone, M., Donzuso, G., Chiriaco, C., Realmuto, S., … Quattrone, A. (2014). Neurofunctional correlates of attention rehabilitation in Parkinson’s disease: An explorative study. Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology, 35(8), 1173–1180. doi: 10.1007/s10072-014-1666-z
- Cicerone, K. D., Langenbahn, D. M., Braden, C., Malec, J. F., Kalmar, K., Fraas, M., … Ashman, T. (2011). Evidence-based cognitive rehabilitation: Updated review of the literature from 2003 through 2008. Archives of Physical Medicine and Rehabilitation, 92(4), 519–530. doi: 10.1016/j.apmr.2010.11.015
- Deelman, B. G., Brouwer, W. H., van Zomeren, A. H., & Saan, R. J. (1980). Functiestoornissen na trauma capitis. In A. Jennekens-Schinkel, J. J. Diamant, H. F. A. Diesfelt, & R. Haaxma (Eds.), Neuropsychologie in nederland (pp. 253–281). Deventer: Van Loghum Slaterus.
- Dywan, J. (1996). Self- and family ratings of adaptive behavior after traumatic brain injury: Psychometric scores and frontally generated ERPs. Journal of Head Trauma Rehabilitation, 11(2), 79–95. doi: 10.1097/00001199-199604000-00008
- Elgh, E., Domellof, M., Linder, J., Edstrom, M., Stenlund, H., & Forsgren, L. (2009). Cognitive function in early Parkinson’s disease: A population-based study. European Journal of Neurology : The Official Journal of the European Federation of Neurological Societies, 16(12), 1278–1284. doi: 10.1111/j.1468-1331.2009.02707.x
- Esselink, R. A., de Bie, R. M., de Haan, R. J., Lenders, M. W., Nijssen, P. C., Staal, M. J., … Speelman, J. D. (2004). Unilateral pallidotomy versus bilateral subthalamic nucleus stimulation in PD: A randomized trial. Neurology, 62(2), 201–207. doi: 10.1212/01.WNL.0000103235.12621.C3
- Foster, E. R., Spence, D., & Toglia, J. (2017). Feasibility of a cognitive strategy training intervention for people with Parkinson’s disease. Disability and Rehabilitation, 1–8. doi: 10.1080/09638288.2017.1288275
- Fritz, C. O., Morris, P. E., & Richler, J. J. (2012). Effect size estimates: Current use, calculations, and interpretation. Journal of Experimental Psychology.General, 141(1), 2–18. doi: 10.1037/a0024338
- Hoehn, M. M., & Yahr, M. D. (1967). Parkinsonism: Onset, progression and mortality. Neurology, 17(5), 427–442. doi: 10.1212/WNL.17.5.427
- Jenkinson, C., Fitzpatrick, R., Peto, V., Greenhall, R., & Hyman, N. (1997). The Parkinson’s disease questionnaire (PDQ-39): Development and validation of a Parkinson’s disease summary index score. Age and Ageing, 26(5), 353–357. doi: 10.1093/ageing/26.5.353
- Klepac, N., Trkulja, V., Relja, M., & Babic, T. (2008). Is quality of life in non-demented Parkinson’s disease patients related to cognitive performance? A clinic-based cross-sectional study. European Journal of Neurology : The Official Journal of the European Federation of Neurological Societies, 15(2), 128–133. doi: 10.1111/j.1468-1331.2007.02011.x
- Krasny-Pacini, A., Chevignard, M., & Evans, J. (2013). Goal management training for rehabilitation of executive functions: A systematic review of effectivness in patients with acquired brain injury. Disability and Rehabilitation, doi: 10.3109/09638288.2013.777807
- Kudlicka, A., Clare, L., & Hindle, J. V. (2011). Executive functions in Parkinson’s disease: Systematic review and meta-analysis. Movement Disorders : Official Journal of the Movement Disorder Society, 26(13), 2305–2315. doi:10.1002/mds.23868; 10.1002/mds.23868
- Kudlicka, A., Clare, L., & Hindle, J. V. (2014). Quality of life, health status and caregiver burden in Parkinson’s disease: Relationship to executive functioning. International Journal of Geriatric Psychiatry, 29(1), 68–76. doi:10.1002/gps.3970; 10.1002/gps.3970
- Kuijer, R. G., & De Ridder, D. T. D. (2003). Discrepancy in illness-related goals and quality of life in chronically ill patients: The role of self-efficacy. Psychology & Health, 18(3), 313–330. doi: 10.1080/0887044031000146815
- Lawson, R. A., Yarnall, A. J., Duncan, G. W., Khoo, T. K., Breen, D. P., Barker, R. A., … Burn, D. J. (2014). Severity of mild cognitive impairment in early Parkinson’s disease contributes to poorer quality of life. Parkinsonism & Related Disorders, 20(10), 1071–1075. doi: 10.1016/j.parkreldis.2014.07.004
- Leung, I. H., Walton, C. C., Hallock, H., Lewis, S. J., Valenzuela, M., & Lampit, A. (2015). Cognitive training in Parkinson disease: A systematic review and meta-analysis. Neurology, 85(21), 1843–1851. doi: 10.1212/WNL.0000000000002145
- Levine, B., Robertson, I. H., Clare, L., Carter, G., Hong, J., Wilson, B. A., … Stuss, D. T. (2000). Rehabilitation of executive functioning: An experimental-clinical validation of goal management training. Journal of the International Neuropsychological Society, 6(3), 299–312. doi: 10.1017/S1355617700633052
- Luteijn, F., & van der Ploeg, F. A. E. (1983). Groninger intelligentie test. Lisse: Swets & Zeitlinger.
- McKinlay, A., Grace, R. C., Dalrymple-Alford, J. C., & Roger, D. (2010). Characteristics of executive function impairment in Parkinson’s disease patients without dementia. Journal of the International Neuropsychological Society: JINS, 16(2), 268–277. doi: 10.1017/S1355617709991299
- Mohlman, J., Chazin, D., & Georgescu, B. (2011). Feasibility and acceptance of a nonpharmacological cognitive remediation intervention for patients with Parkinson disease. Journal of Geriatric Psychiatry and Neurology, 24(2), 91–97. doi: 10.1177/0891988711402350
- Mohlman, J., Reel, D. H., Chazin, D., Ong, D., Georgescu, B., Tiu, J., & Dobkin, R. D. (2010). A novel approach to treating anxiety and enhancing executive skills in an older adult with Parkinson’s disease. Clinical Case Studies, 9(1), 74–90. doi: 10.1177/1534650109351305
- Muslimovic, D., Post, B., Speelman, J. D., & Schmand, B. (2005). Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology, 65(8), 1239–1245. doi: 10.1212/01.wnl.0000180516.69442.95
- Paris, A. P., Saleta, H. G., de la Cruz Crespo Maraver, M., Silvestre, E., Freixa, M. G., Torrellas, C. P., … Bayes, A. R. (2011). Blind randomized controlled study of the efficacy of cognitive training in Parkinson’s disease. Movement Disorders: Official Journal of the Movement Disorder Society, 26(7), 1251–1258. doi: 10.1002/mds.23688
- Pena, J., Ibarretxe-Bilbao, N., Garcia-Gorostiaga, I., Gomez-Beldarrain, M. A., Diez-Cirarda, M., & Ojeda, N. (2014). Improving functional disability and cognition in Parkinson disease: Randomized controlled trial. Neurology, 83(23), 2167–2174. doi: 10.1212/WNL.0000000000001043
- Petrelli, A., Kaesberg, S., Barbe, M. T., Timmermann, L., Fink, G. R., Kessler, J., & Kalbe, E. (2014). Effects of cognitive training in Parkinson’s disease: A randomized controlled trial. Parkinsonism & Related Disorders, 20(11), 1196–1202. doi: 10.1016/j.parkreldis.2014.08.023
- Reitan, R. M. (1958). Validity of the trail making test as an indicator of organic brain damage. Perceptual and Motor Skills, 8, 271–276. doi:10.2466/PMS.8.7.271-276 doi: 10.2466/pms.1958.8.3.271
- Reuter, I., Mehnert, S., Sammer, G., Oechsner, M., & Engelhardt, M. (2012). Efficacy of a multimodal cognitive rehabilitation including psychomotor and endurance training in Parkinson’s disease. Journal of Aging Research, 2012, 235765. doi: 10.1155/2012/235765
- Robertson, I. H., Ward, T., Ridgeway, V., & Nimmo-Smith, I. (1994). Manual: The test of everyday attention. Bury St. Edmunds: Thames Valley Test Company.
- Rosqvist, K., Hagell, P., Odin, P., Ekstrom, H., Iwarsson, S., & Nilsson, M. H. (2016). Factors associated with life satisfaction in Parkinson’s disease. Acta Neurologica Scandinavica, doi: 10.1111/ane.12695
- Sammer, G., Reuter, I., Hullmann, K., Kaps, M., & Vaitl, D. (2006). Training of executive functions in Parkinson’s disease. Journal of the Neurological Sciences, 248(1–2), 115–119. doi: 10.1016/j.jns.2006.05.028
- Schuhfried, G. (2007). Cogniplus. Mödling: Schuhfried GmbH.
- Spikman, J. M., Boelen, D. H., Lamberts, K. F., Brouwer, W. H., & Fasotti, L. (2010). Effects of a multifaceted treatment program for executive dysfunction after acquired brain injury on indications of executive functioning in daily life. Journal of the International Neuropsychological Society: JINS, 16(1), 118–129. doi: 10.1017/S1355617709991020
- Tate, R., Kennedy, M., Ponsford, J., Douglas, J., Velikonja, D., Bayley, M., & Stergiou-Kita, M. (2014). INCOG recommendations for management of cognition following traumatic brain injury, part III: Executive function and self-awareness. The Journal of Head Trauma Rehabilitation, 29(4), 338–352. doi: 10.1097/HTR.0000000000000068
- Thombs, B. D., Kwakkenbos, L., Riehm, K. E., Saadat, N., & Fedoruk, C. (2017). Comparison of self-efficacy for managing chronic disease between patients with systemic sclerosis and other chronic conditions: A systematic review. Rheumatology International, 37(2), 281–292. doi: 10.1007/s00296-016-3602-4
- Vasconcellos, L. F., & Pereira, J. S. (2015). Parkinson’s disease dementia: Diagnostic criteria and risk factor review. Journal of Clinical and Experimental Neuropsychology, 37(9), 988–993. doi: 10.1080/13803395.2015.1073227
- Verbaan, D., Jeukens-Visser, M., Van Laar, T., van Rooden, S. M., Van Zwet, E. W., Marinus, J., & van Hilten, J. J. (2011). SCOPA-cognition cutoff value for detection of Parkinson’s disease dementia. Movement Disorders : Official Journal of the Movement Disorder Society, 26(10), 1881–1886. doi: 10.1002/mds.23750
- Vlagsma, T. T., Koerts, J., Fasotti, L., Tucha, O., van Laar, T., Dijkstra, H., & Spikman, J. M. (2015). Parkinson’s patients’ executive profile and goals they set for improvement: Why is cognitive rehabilitation not common practice? Neuropsychological Rehabilitation, 26(2), 1–20.
- Vlagsma, T. T., Koerts, J., Tucha, O., Dijkstra, H. T., Duits, A. A., van Laar, T., & Spikman, J. M. (2016). Mental slowness in patients with Parkinson’s disease: Associations with cognitive functions? Journal of Clinical and Experimental Neuropsychology, 38(8), 844–852. doi: 10.1080/13803395.2016.1167840
- Wilson, B. A., Alderman, N., Burgess, P. W., Emslie, H., & Evans, J. J. (1996). Behavioural assessment of the dysexecutive syndrome. Bury St. Edmunds: Thames Valley Test Company.
- Ylvisaker, M. (1998). Traumatic brain injury rehabilitation: Children and adolescents. Boston: Butterworth Heinemann.
- Zarit, S. H., Orr, N. K., & Zarit, J. M. (1985). The memory and behavior problems checklist in families under stress: Caring for the patient with Alzheimer’s disease and related disorders. New York: University Press.
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x
- Zimmermann, R., Gschwandtner, U., Benz, N., Hatz, F., Schindler, C., Taub, E., & Fuhr, P. (2014). Cognitive training in Parkinson disease: Cognition-specific vs nonspecific computer training. Neurology, 82(14), 1219–1226. doi: 10.1212/WNL.0000000000000287