ABSTRACT
Spatial neglect has profound implications for quality of life after stroke, yet we lack consensus for screening/diagnosing this heterogeneous syndrome. Our first step in a multi-stage research programme aimed to determine which neglect tests are used (within four categories: cognitive, functional, neurological and neuroimaging/neuromodulation), by which stroke clinicians, in which countries, and whether choice is by professional autonomy or institutional policy. 454 clinicians responded to an online survey: 12 professions (e.g., 39% were occupational therapists) from 33 countries (e.g., 38% from the UK). Multifactorial logistic regression suggested inter-professional differences but fewer differences between countries (Italy was an outlier). Cognitive tests were used by 82% (particularly by psychologists, cancellation and drawing were most popular); 80% used functional assessments (physiotherapists were most likely). 20% (mainly physicians, from Italy) used neuroimaging/ neuromodulation. Professionals largely reported clinical autonomy in their choices. Respondents agreed on the need for a combined approach to screening and further training. This study raises awareness of the translation gap between theory and practice. These findings lay an important foundation to subsequent collaborative action between clinicians, researchers and stroke survivors to reach consensus on screening and diagnostic measures. The immediate next step is a review of the measures’ psychometric properties.
Introduction
Spatial neglect is a multifaceted and disabling cognitive syndrome that commonly follows stroke and other brain injury or neurodegenerative disease (Andrade et al., Citation2010; Bender, Citation2011). It is clinically characterized as no or insufficient attention especially towards contralesional space, and manifests in many stroke survivors – particularly those with right hemisphere damage (Corbetta & Shulman, Citation2011; Rode et al., Citation2017). The academic literature provides distinctions between “subtypes” of spatial neglect, usually depending on the domain and/or the spatial frame(s) in which symptoms manifest (although it is not obvious that this knowledge has translated into routine clinical practice of screening for neglect). One example that describes subtypes of neglect is a study of 166 inpatients and outpatients with right hemisphere stroke, which found that 48% of these patients had spatial neglect (Buxbaum et al., Citation2004). 1% exhibited signs of personal (i.e., bodily reference frame) neglect, 27% of peripersonal (i.e., visual space within an arm’s reach) neglect, 17% motor neglect, and 21% showed perceptual (i.e., allocentric) neglect. The authors also found that 12 different combinations of subtype signs were present in the sample.
Halligan and Robertson (Citation1999) note that the incidence of neglect varies widely across studies, between 12% and 95%. Of course incidence will depend on the operational definition of neglect used, along with the assessment or combination of assessments to identify neglect and, the marked heterogeneity of neglect presentation (Ting et al., Citation2011).
Identifying spatial neglect and separating it into different subtypes might help clinicians and researchers to target treatment approaches. For example, we know that egocentric and allocentric neglect have a different impact on functional independence and recovery pathways (Bickerton et al., Citation2012; Chechlacz et al., Citation2010, Citation2012). The presence of post-stroke neglect is associated with longer stays in hospital and poorer functional outcomes (Chen, Hreha, et al., Citation2015; Nijboer et al., Citation2013; Wilkinson et al., Citation2012). Data collected from 88,000 UK hospital admissions with stroke suggested that those with neglect had an increased length of stay (27 vs. 10 days) and on discharge were “dependent” (76% vs. 57%) on the modified Rankin scale (Hammerbeck et al., Citation2019). Although neglect impedes active participation in stroke rehabilitation, it decreases independence in activities of daily living (ADLs), and has an adverse impact on quality of life there is no compelling evidence for specific interventions that improve life after stroke (Bowen et al., Citation2013). Evidence also suggests that neglect is a potential safety hazard with respect to falls (Chen, Chen, et al., Citation2015; Wee & Hopman, Citation2008).
Many national clinical guidelines recommend the comprehensive and timely screening and diagnosis of neglect as an essential part of post-stroke clinical care planning, e.g., the Royal College of Physicians London (Intercollegiate Stroke Working Party, Citation2016), the Canadian Stroke Association (Hebert et al., Citation2016), the American Heart Association (Winstein et al., Citation2016), and the National Stroke Foundation of Australia’s clinical guidelines for stroke management (National Stroke Foundation, Citation2019). However, these lack specific guidance on which of the many neglect tests to choose, for which subtypes of neglect and at which timepoints.
Various standardized assessments of neglect, or of functions that could be affected by neglect, are available. Anecdotally we know that those chosen by clinicians mostly fall into four broad but unequal categories: cognitive/neuropsychological assessment, functional assessment, neurological assessment, and (in some countries) neuroimaging/neuromodulation. Cognitive assessment is the measurement of abilities and processes such as attention and memory by means of standardized assessments. An example of a cognitive assessment for neglect is the Behavioural Inattention Test (BIT; Wilson et al., Citation1987), comprising 15 subtests involving target cancellation, drawing, line bisection, text reading, clock reading, and visual description – all assessing neglect in peri-personal space. Functional assessment is the structured appraisal of a patient’s ability to perform everyday tasks, such as dressing or making a hot drink. The Catherine Bergego Scale (CBS; Bergego et al., Citation1995) is a 10 item structured functional assessment, and focuses on personal space and performance of activities of daily living (ADLs) in extra-personal space. Each item is scored by direct observation from 0-3, giving a maximum possible score of 30. There is also a self-evaluation and anosognosia scale, which mirrors the functional assessment checklist and provides a self-awareness score between 0-30; an anosognosia score can be obtained by calculating the difference between the observer's and the patient’s scores. Neurological assessment is the clinical examination of signs and symptoms including, but not specific to, those indicative of neglect. The National Institutes of Health Stroke Scale (NIHSS; Brott et al., Citation1989) is primarily used in the acute phase post-stroke to inform immediate treatment and subsequent rehabilitation. Certain NIHSS subscales are used to screen for neglect, e.g., horizontal gaze, sensation, and extinction/neglect subscales. Neuroimaging is another important approach in the acute phase to initially detect lesion location and extent, and to guide assessment. Some professionals use neuroimaging findings for a first prediction of cognitive and functional deficits by lesion location and/or damage to distributed neural networks (Vuilleumier, Citation2013), although it is not known whether neuroimaging is commonly used in clinical practice for screening or diagnosis.
Currently it is unknown how different clinical professional groups screen, assess, or diagnose neglect and whether they use any or all of these four categories. Previous attempts to understand the selection of neglect assessments focused on identifying the gap between best and current practice within a profession, rather than similarities or differences between professional groups or countries. For example, a survey of 253 Canadian occupational therapists conducted by Menon-Nair et al. (Citation2007) found that while identification of neglect-related problems was high, the use of evidence-based, standardized assessments was less than optimal. This is consistent with a previous retrospective study of medical records, that found standardized neglect assessment was not standard clinical practice amongst participating hospitals in Canada (Menon-Nair et al., Citation2006). Furthermore, it is not uncommon for clinicians to assess neglect informally – that is, without use of standardized tests (Halligan & Robertson, Citation1999). The selection of neglect assessments varies widely across research studies (Chen, Chen, et al., Citation2015) due to the varied operational definition of the syndrome and its symptom presentations (Verdon et al., Citation2010) and probably its severity in the patient population. Reflecting the wide range of assessments available, a Cochrane review of cognitive rehabilitation for stroke acknowledged that there was no one neglect assessment that was common across included studies (Bowen et al., Citation2013).
The various approaches to measuring neglect require clarification for clinicians and researchers alike, with the ultimate goal of forming a consensus on the best approaches to use. We acknowledge there is also a considerable psychometric literature comparing the sensitivity and specificity of cognitive versus functional tests of neglect and comparing tests within a category (e.g., cancelling bells or stars versus cancelling apples (Basagni et al., Citation2017; Bickerton et al., Citation2011)). Before exploring the psychometric literature we aimed to take the first of several steps in an international, multidisciplinary, multi-stage consensus process beginning by scoping clinical practice across a range of professionals, countries and clinical settings. We hypothesized that selection of neglect assessments differs according to professional background, role in a multidisciplinary team, and/or local and national policies.
We designed this study to answer the following research questions:
Which assessments of neglect after stroke are used by which clinical professionals, and in which countries?
Are assessments selected on the basis of professional choice or institutional policy?
Are there assessments not listed in the study that are deemed to be useful?
Methods
Participants
Respondents were recruited by email invitations via professional organizations or key individuals worldwide, and opportunity sampling on Twitter. This study was approved by an ethics review committee (The University of Manchester, 2018-3901-7379) and hosted on the online platform SelectSurvey. The survey was open from 19th November 2018 to 24th February 2019.
Survey development
The list of assessments was collaboratively developed through iterative discussion amongst the authors, and in consultation with local stroke clinicians otherwise not involved with the study design process. Assessments were included if they were informally appraised to be either specific to the detection of USN, or non-specific to USN detection but potentially used during routine examination and assessment as more general neurocognitive or functional probes. The survey was developed in a 4-stage sequential, multimethod approach. At stage 1, authors held initial in-person meetings followed by video conferences and email communications to determine the objectives and research questions. At stage two, the first author (MC) created the first draft of the survey to collect comments and suggestions on its design from the other authors. After multiple iterations the survey was converted into online format and at stage 3, co-authors and local research collaborators pilot-tested the functionality of the survey and the utility of the format in which data were rendered by the survey software. At this stage, the survey reached its current format of four assessment categories (cognitive, functional, neurological, and neuroimaging/neuromodulation), where the first three contained a non-exhaustive list of assessments with three response options each: “Use – Professional Choice,” “Use – Institutional Policy,” and “Do Not Use,” with only one option available per assessment. The neuroimaging/neuromodulation section contained free text options for respondents to indicate their choice of assessment(s). Stage 4 consisted of final tweaking of the online survey design as well as the compilation of target organizations and email addresses before distribution of the survey advertisement (survey content is provided as supplementary material).
The main rationale for including a non-exhaustive list of assessments in the main body of the survey was to avoid over-burdening respondents, to maximize the response rate and accuracy of responses. For the same reason we did not ask respondents to repeat the questions for each neglect subtype (e.g., egocentric, allocentric), severity or setting/timescale (e.g., in acute phase and chronic phases). Instead, at the end of the questions we included the opportunity to respond with free choice, narrative data. The main rationale for not including a list of neuroimaging/neuromodulation techniques was our assumption that the technologies used between professional groups and countries would not vary (e.g., MRI and CT use is prolific in the diagnosis of stroke). Rather, we sought to uncover more specifically which, if any, aspects of these scanning procedures are used to screen and diagnose neglect, by which professionals and in which countries. Inclusion of items was not a recommendation. We sought to find out what is being done in clinical practice not what should be done. We focused this initial work on clinicians, mindful that clinical and research practice may be very different.
Procedures
Demographic questions
Those clinicians not currently practising (i.e., treating patients with neglect in the preceding 12 months) were ineligible and removed from the survey. Other demographic questions collected information on country of practice, profession/discipline, practice setting (e.g., inpatient), length of service in stroke medicine/rehabilitation, and whether or not respondents were active in neglect research (either as an investigator or assisting in recruiting for someone else’s research). The survey did not collect any health information, internet protocol addresses, or other data that would potentially be personally identifiable.
Assessments for neglect
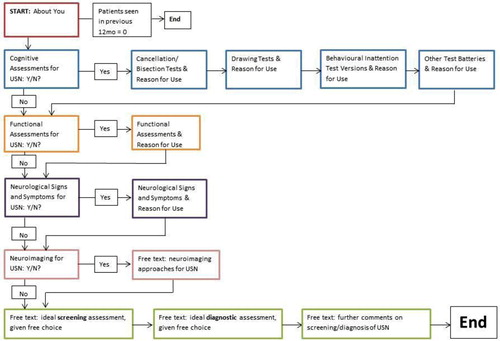
After answering preliminary questions, participants responded to questions on the screening and diagnosis of neglect organized into the four categories described above. The flowchart () depicts a respondent’s passage through the survey. For each individual assessment, respondents indicated whether or not they use it for the screening or diagnosis of neglect. Respondents could select only one of the following: Use – Institutional Policy, Use – Professional Choice, Do Not Use. There was no limit to the number of assessments a respondent could select. If respondents’ most frequently used assessment(s) did not appear in the list, they were asked to provide the name(s) of such assessments in a comment box underneath the original question. At the end of the four categories, there was a final page of three open questions. Here we asked what respondents would use, given a free choice, as (i) a screening assessment, (ii) as a diagnostic assessment, and finally (iii) asked if they had any further comments.
Analysis
Raw, fully anonymized data were downloaded in Excel format from the SelectSurvey platform in March 2019. Participant characteristics and relationships with assessment tools were analysed with descriptive and frequency statistics.
After visualizing the data, a multi-factorial logistic regression model was designed to assess the independent associations of “profession” and “country” after adjustment for the potentially confounding influences of experience, research activity, and clinical setting (question one). For clinical setting, respondents could choose more than one of these three options, which were handled in regression models as individual factors in their own right rather than as levels within one factor. The first level, usually the most prevalent, served as the reference for each categorical factor with odds ratio (OR) = 1.0 by definition (with the exception of clinical setting). For example, OTs serve as the reference for “profession” with the other professional categories shown relative to OTs (see ).
Table 1. Characteristics of respondents.
Further multifactorial logistic regression was undertaken to answer question two, limited to respondents who used each specific assessment. For all analyses 95% confidence intervals (CIs) are given and statistical significance was concluded using the threshold of p ≤ 0.05. We also summarized the most popular individual assessments within the categories.
Results
Participant characteristics
Out of a total number of 476 responses, we excluded 22 that indicated no experience in treating patients with neglect in the preceding 12 months. Therefore, after meeting the criteria, 454 responses were included in the study (see ).
presents the numbers of respondents according to their profession, geographical location, months of experience, number of patients with neglect seen in the past twelve months, clinical setting, and research involvement. Occupational therapists (OTs) represent the most frequent professional group within this survey (39%), followed by psychologists (19%), medical doctors/physicians (15%), and physiotherapists (12%). For the purpose of analysis, the small number of respondents from speech & language therapists, orthoptists, and other self-reported professional backgrounds form a single “other” category (15%). The greatest number of respondents was from the United Kingdom (UK, 38%), followed by the United States of America (USA, 22%) and Italy (17%). Similarly, for the purpose of analysis, responses from other European countries (including Denmark, France, Germany, Luxembourg, Sweden, and Switzerland) and responses from other countries excluding Europe and the USA (including Australia, Canada, Japan, and South Korea) were combined to form “Other Europe” (13%) and “Other Non-Europe, Non-USA” (11%) groups respectively. The majority of respondents reported spending time with seven or more patients with symptoms of neglect in the preceding twelve months (67%), and the overall median length of clinical experience was ten years.
Assessment categories
represents the percentage of respondents within each professional group who indicated their use of the four potential assessment categories – cognitive assessments, functional assessments, neurological assessments, and neuroimaging/neuromodulation techniques. There is variation between professional groups. For example, similar proportions of occupational therapists report using both cognitive and functional assessments. In contrast, psychologists predominantly select cognitive assessments, followed by functional assessments, and no more than 50% use neurological assessment and neuroimaging/neuromodulation techniques. Physicians and physiotherapists select assessments that reflect their training and practice, with physicians using cognitive and neurological assessments more than other categories, and physiotherapists more often selecting assessments from the functional and neurological categories.
Figure 2. Percentage of respondents from each professional group who use each category of neglect assessment.
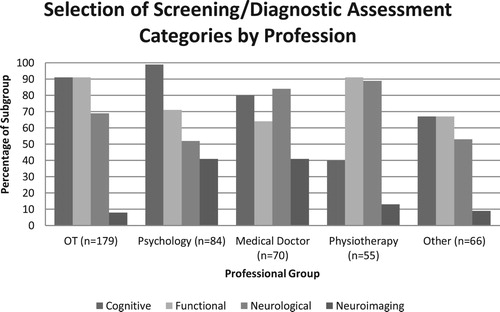
represents the proportion of respondents from each country or country category per assessment category. There is comparatively little variation between different countries with the possible exception of Italy. Respondents from each country exhibit similar patterns, with cognitive and functional assessments the most popular and neuroimaging/neuromodulation the least ().
Figure 3. Number of respondents from each country who indicate their use of each category of neglect assessment.
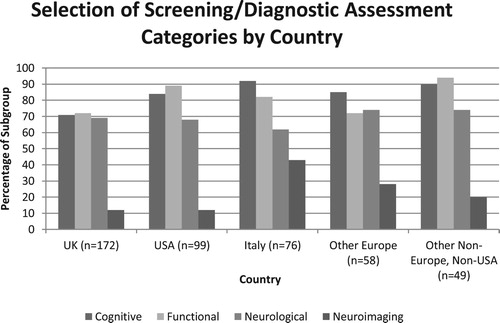
Figure 4. Forest plots depicting logistic regression results for selection of each assessment category. Note: x-axes are on a logarithmic scale. Logistic regression results are presented as odds ratios with 95% confidence intervals.
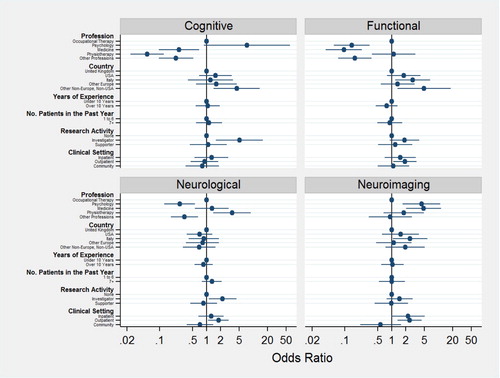
Three hundred and sixty-eight (82%) respondents reported use of cognitive assessments to identify neglect. Psychologists were most likely to use these, OR (95% CI) = 7.2 (0.90 to 60). Other professionals were significantly less likely to use cognitive assessments: physicians, OR (95% CI) = 0.2 (0.10 to 0.70), physiotherapists, OR (95% CI) = 0.05 (0.02 to 0.10), and “others,” OR (95% CI) = 0.2 (0.10, 0.50). Respondents outside of Europe and the USA were significantly more likely to use cognitive assessments: OR (95% CI) = 4.4 (1.40 to 14). Respondents active in research were also more likely to use cognitive tools: OR (95% CI) = 5.04 (1.60 to 16).
Three hundred and sixty-one (80%) respondents reported use of functional assessments to identify neglect. Physiotherapists were more likely than all others: OR (95% CI) = 1.1 (0.40 to 3.2), and psychologists, OR (95% CI) = 0.14 (0.06 to 0.34), physicians, OR (95% CI) = 0.1 (0.04 to 0.23), and “other” professions, (95% CI) = 0.16 (0.07 to 0.37), were significantly less likely. Respondents outside of Europe and the USA were the most likely: OR (95% CI) = 4.9 (1.3 to 18), followed by those in Italy: OR (95% CI) = 2.8 (1.2 to 6.6).
Three hundred and eleven (69%) respondents reported use of neurological signs and symptoms to identify neglect symptoms. Physiotherapists were the most likely, recording OR (95% CI) = 3.5 (1.4 to 8.8). Psychologists and “other” professionals were less likely to use neurological signs and symptoms, recording OR (95% CI) = 0.27 (0.13 to 0.56) and OR (95% CI) = 0.34 (0.17 to 0.65) respectively. Clinicians working in the outpatient setting were also significantly more likely to use neurological signs and symptoms: OR (95% CI) = 1.8 (1.1 to 3.0), as were clinicians involved in research: OR (95% CI) = 2.2 (1.1 to 4.3).
Finally, a fairly high number of respondents (91, 20%) reported using neuroimaging/neuromodulation techniques. Physicians were most likely, recording OR (95% CI) = 4.8 (2.0 to 11.2), followed by psychologists, recording OR (95% CI) = 4.3 (1.7 to 10). Use was also significantly higher in Italy: OR (95% CI) = 2.5 (1.1 to 5.8). Clinicians working in the outpatient setting were also significantly more likely to use neuroimaging/neuromodulation: OR (95% CI) = 2.4 (1.3 to 4.3).
Selection of specific assessments
As well as asking what categories of assessment stroke clinicians use, we also wanted to find out which individual assessments are most frequently used. The ultimate goal in our research programme, of which this is stage one, is an international, multi-professional consensus on the best approach to screen and diagnose neglect, where frequency and feasibility of assessment use are two of potentially several influencing factors along with psychometric properties that will be investigated in stage two. – display the percentage of selections per professional group for individual screening/diagnostic assessments for neglect. Each figure is sub-divided into profession and country.
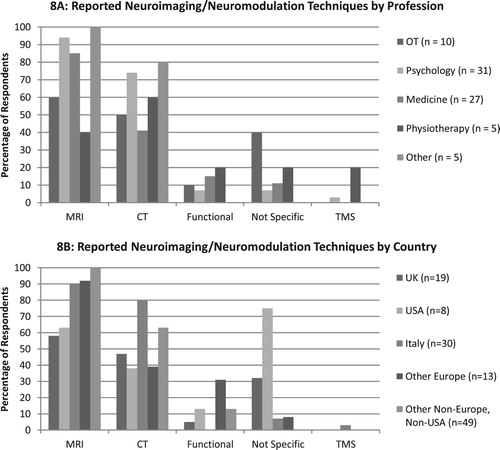
Figure 8. Reported neuroimaging/neuromodulation techniques by professional group (8A) and by country (8B).
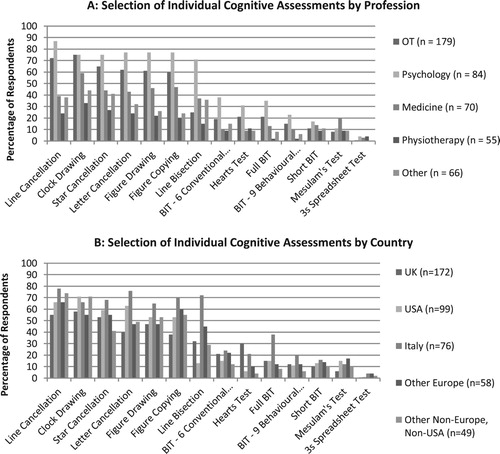
Cognitive assessments
shows the percentage of respondents who reported use of each individual screening/diagnostic cognitive assessment, categorized by profession (5A) and country (5B).
The most popular cognitive assessment selected by 292 clinicians was the line cancellation test (Albert, Citation1973). Six assessments – line cancellation, clock drawing, star cancellation, letter cancellation, figure drawing and figure copying – were reported by at least 60% of OTs and 70% of psychologists. Line bisection was similarly popular amongst psychologists but not OTs. No other assessment was used by more than 40% of any professional group.
(B) suggests that a greater proportion of respondents from Italy select specific cognitive assessments, compared to their colleagues from other countries. For example, greater proportions of clinicians from Italy select line, star, and letter cancellation tests, as well as figure copying and drawing, and all presented versions of the BIT.
At the end of each cognitive assessment sub-category, respondents were asked about any other cognitive assessments that were not provided in the survey list. One hundred additional assessments, including 39 cancellation and bisection tests, 26 drawing tests, and 35 test batteries, were reported by participants. The Bells Test (Gauthier et al., Citation1989) was more popular than one test included in the survey question – the 3s spreadsheet test (Chen et al., Citation2017) with 38 versus 8 responses respectively.
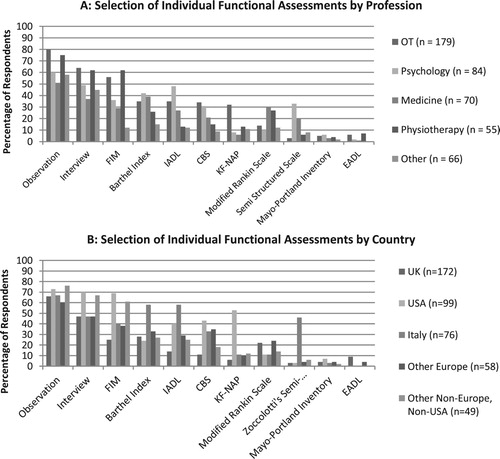
Functional assessments
Observation (clinical, unstructured) was the most commonly selected assessment from the functional category, with 309 positive responses. The distribution for functional assessments ((A)) is comparatively more varied. The two most popular assessments – observation and interview – are selected by the majority of OTs compared to other professional groups, however standardized generic (non-neglect specific) approaches such as the functional independence measure (FIM; Keith et al., Citation1987), the Barthel index (BI; Mahoney & Barthel, Citation1965) and the instrumental activities of daily living scale (IADL; Lawton & Brody, Citation1969) are selected by greater proportions of psychologists (e.g., FIM) and physicians (e.g., BI and IADL). Neglect-specific approaches based on observation of functional activities such as the Catherine Bergego Scale (CBS) and the Kessler Foundation Neglect Assessment Process (KF-NAP; Chen et al., Citation2012) are selected by greater proportions of OTs.
(B) suggests that a greater proportion of USA clinicians favour interviews, the FIM, the CBS and the KF-NAP. Clinicians from Italy appear to more frequently use the BI, the IADL and Zoccolotti’s semi-structured scale for the functional evaluation of hemi-inattention in personal space (Zoccolotti et al., Citation1992). The most popular functional assessment, observation, was selected by a greater proportion of respondents from “other worldwide” countries.
When asked if they wished to outline any other functional assessments that were not listed, respondents reported 60 additional assessments, but none were as popular as those listed in the survey.
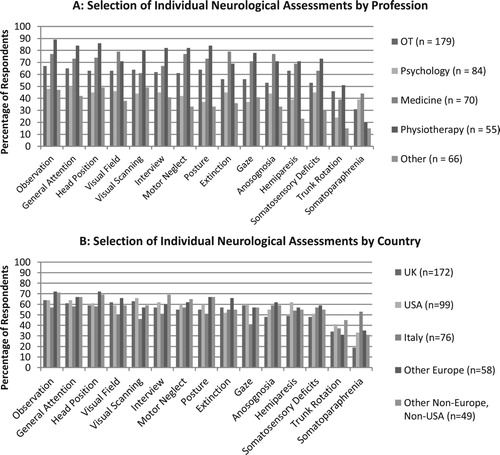
Neurological assessments and neuroimaging/neuromodulation
For the third category (neurological/clinical examination), observation (unstructured) was the most popular assessment choice, with 293 positive responses. In the case of neurological assessments ((A)), the majority of these are favoured by greater proportions of physiotherapists, except in the case of screening for visual field loss, extinction, anosognosia, and somatoparaphrenia, which were favoured by physicians.
(B) suggests that there appears to be fewer differences in the proportions of respondents from country subgroups in terms of assessment selection. The greatest agreement between countries seems to be in the selection of examination of general attention, motor neglect, and somatosensory deficits. However, the least agreement is in the selection of screening for somatoparaphrenia, which is clearly favoured by clinicians from Italy.
When asked if they would like to provide additional information about other neurological approaches unlisted within the survey 25 additional assessments were reported, none of which were as popular as those already included in the survey.
Finally, of the 91 (20%) respondents who indicated their preferred neuroimaging/neuromodulation technique, 78 respondents provided further detail. The responses are summarized in .
Neuroimaging/neuromodulation was most popular amongst psychologists (n = 31) and physicians (n = 27), and clinicians based in Italy (n = 30) but far less so in the UK. The most frequently reported neuroimaging assessment was use of magnetic resonance imaging (MRI) with 61 occurrences in-text, followed by computerized tomography (CT) with 42. Other functional techniques were reported (primarily electroencephalography and functional MRI [fMRI]), as were neuromodulation paradigms such as transcranial magnetic stimulation (TMS). (A and B) suggest that conventional structural scanning is the most popular tool used by clinicians in the identification of neglect. The “non-specific” category incorporates responses that do not explicitly mention a particular technique but refer to concepts such as “structural scans,” or “lesion mapping.”
Within the free-text data, there appeared to be a distinction between some respondents depending on whether neuroimaging/neuromodulation is used to deduce the presence of neglect by lesion location (for example, “[I] look at the location of the stroke to see if the areas are consistent with areas of the brain that are more common to have neglect after a stroke”), or whether it is used in differential diagnosis (for example, “I would use imaging results to guide my thoughts over whether I was looking for a neglect or a hemianopia, or if a patient that looked like they had neglect had brain damage consistent with neglect”). Some respondents also employ more specific neuroimaging procedures, particularly in the case of MRI; these include diffusion tensor imaging (DTI) for the visualization of white matter tracts and/or visualization of vascular tissue, and voxel-based lesion mapping to visualize the extent of lesions. Few respondents selected functional neuroimaging approaches (e.g., functional MRI, EEG, MEG) or transcranial magnetic stimulation (TMS); however, more often than not, these approaches appeared in combination with structural scanning procedures. Several respondents made the distinction between the use of neuroimaging as a standalone diagnostic assessment and the use of neuroimaging as one source of additional information, which is combined with other approaches to inform tailored rehabilitation programmes for patients.
Reasons for using screening/diagnostic assessments
presents the relative proportions of the two “reasons for use” responses for individual assessments – professional choice versus institutional policy.
Figure 9. Proportions of “use” responses according to reason for selection – institutional policy or professional choice.
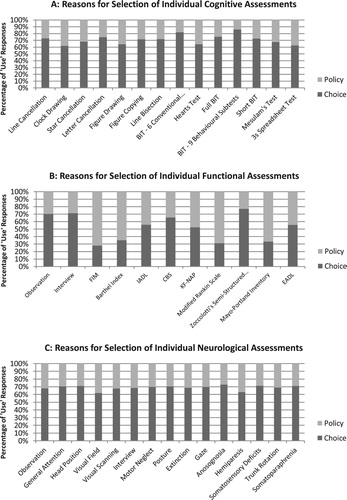
suggests that for cognitive assessments (9A), approximately 20% to 40% of assessment selections are driven by institutional policy. In the functional assessment category (9B), there is greater variation between specific assessments in terms of reasons for their selection: between 20% and 70% of selections of specific tools here are made on the basis of institutional policy. (B) suggests that assessments not specific to neglect but that are used for multiple different purposes (e.g., the FIM, BI, and mRS) are selected the most based on institutional policy, with neglect-specific assessments (e.g., the CBS and KF-NAP) exhibiting the inverse pattern. For neurological assessments (9C), approximately 30% to 40% of assessment selections are driven by institutional policy.
Narrative data
Screening assessments – free choice
One hundred and ninety-eight (44%) respondents commented on their ideal screening assessment, given free choice. Of these 198 respondents, 36% were OTs, 21% were psychologists, 34% were physicians, 9% were physiotherapists, and 7% were “others.”
displays examples of screening assessments as chosen by clinicians in their “ideal” scenario. The most common theme arising was with regard to cognitive assessments, yielding 75 references among respondents. The reasons for these selections were either: the rapid nature of cognitive screening (e.g., paper-and-pencil tests) or the respondent only being aware of the particular assessments they suggested. Only one respondent mentioned the screening of spatial neglect subtypes, without any detail on specific assessments.
Table 2. Self-reported “ideal” screening assessments as reported by 176 respondents.
Diagnostic assessments – free choice
One hundred and seventy-six (39%) respondents commented on their ideal diagnostic assessment, given free choice. Of these 176 respondents, 31% were OTs, 25% were psychologists, 17% were physicians, 14% were physiotherapists, and 13% were “others.”
displays examples of diagnostic assessments as chosen by clinicians in their “ideal” scenario. The most common theme arising from reading of these responses was with regard to combinatorial approaches, yielding 43 references among respondents.
Table 3. Self-reported “ideal” diagnostic assessments as reported by 176 respondents.
Further comments
One hundred (22%) respondents provided further comments at the end of their participation in the survey. Of these 100 respondents, 31% were OTs, 16% were psychologists, 17% were physicians, 15% were physiotherapists, and 21% were “others.”
displays the results of the final question in the survey, which asked clinicians for their general comments on the screening and diagnosis of neglect. The most common theme identified was that of a desire for further training (27 respondents). Other themes were tangentially related in that they allude to information-gathering from various sources to inform good clinical practice in the screening and diagnosis of neglect. Four respondents here mentioned the assessment of spatial neglect subtypes. Of these, two respondents mentioned the utility of functional assessments (including the KF-NAP) in addressing “types and sequelae” of spatial neglect, one respondent advocated combined cognitive and motor assessment to dissociate motor neglect from other subtypes, and one respondent commented on a lack of education provided on various subtypes of spatial neglect.
Table 4. Additional comments on the screening and diagnosis of neglect as provided by 100 respondents.
Discussion
Before we can build consensus on the approaches that should be used for the screening and diagnosis of spatial neglect, this study identified which assessments are being used in clinical practice, by which professional groups and in which countries, whether these selections are determined by professional choice or institutional policy, and whether clinical professionals suggest alternative methods. This preparatory study raises awareness of the translational gap between academic theory in neglect research and application into clinical practice, and suggests the next steps to bridge that gap, including a review of psychometric properties of tests and consensus-building activities such as Delphi and an expert panel. The study also highlights positive signs of an emerging consensus within clinical professional groups and, to an extent, between countries. Less surprising is the evidence of inter-professional differences. The latter raise the interesting possibility that these differences are not a limitation but cue the need for contributions from the multidisciplinary stroke team, with formulation led by the psychologist or OT.
There was strong interest in this topic, attracting 454 responses over three months, from 12 healthcare professional groups from 33 countries, and it was encouraging to see the greatest response was from OTs and psychologists as expected. The number and type of respondents supports the external validity of this study. The findings provide a rich data source on current clinical practice per professional groupings, and at a higher level reveal inter-professional differences in assessment category selection and individual assessment selection. There are also modest differences between countries. We found that individual neglect-specific assessments are more often than not selected based on professional choice rather than institutional policy. The reverse was true for generic functional assessments, e.g., FIM, which are not neglect-specific. We did not ask respondents to distinguish between specific and non-specific assessments, choosing to keep the survey neutral to capture what is actually happening in clinical practice. Free text responses indicated clinicians’ willingness to combine assessments and adopt a multidisciplinary approach to screening and diagnosis of neglect; this is a particular strength of current clinical practice and allows for the tailoring of assessment selection based on the patient’s profile, and what they can be realistically expected to perform. There is a need for training in understanding neglect and how to screen for and diagnose it, especially given differences in the initial training of different members of multidisciplinary healthcare teams, e.g., psychologists, physicians and therapists. Naturally, this leads to differences in neglect assessment approaches employed within stroke teams, which must be knitted together for patient-centred care. Overall, whilst the anticipated diversity in current practice is an issue, given the huge number of assessments in use, it is encouraging to see the appetite for harmonization. This supports our plan to proceed to the next stages of consensus-building, including: a systematic review of the psychometric and other properties of assessments such as their cost (financial and time required), Delphi exercises and an expert panel. These activities are more appropriate than this survey for examining the important issues of screening and diagnosis of neglect subtypes, severity and chronicity.
Cognitive assessments
Cognitive assessments were the most frequently used by psychologists and OTs (>90%) but only 40% of physiotherapists reported using these. The selection of cognitive assessments is slightly modulated by country, with those from other countries worldwide (non-Europe, non-USA) being more likely to select cognitive assessments. Respondents who reported being active in research as an investigator were also more likely to select cognitive assessments.
A previous review of patient notes by Menon-Nair et al. (Citation2006) highlighted that cognitive assessments are popular selections in the Canadian stroke inpatient setting. A subsequent survey found that cognitive assessments are a very popular selection amongst Canadian OTs, particularly assessments that are not specific to neglect, including the OSOT perceptual evaluation (Boys et al., Citation1988), the Motor-Free Visual Perception Test (MVPT, Colarusso & Hammill, Citation1972, Citation2003), the Chessington Occupational Therapy Neurological Assessment Battery (COTNAB, (Tyerman et al., Citation1986), and non-standardized visual perception testing (Menon-Nair et al., Citation2007). The Canadian authors found that assessments that are specific to neglect are also used, albeit to a lesser extent, e.g., the Bells test and clock drawing test. The use of standardized assessment batteries was particularly low amongst these OTs. However the present study concluded that cognitive assessments are highly popular among OTs worldwide, both standardized and non-standardized assessments.
The present survey found that selection of cognitive tests that include cancellation, bisection, or drawing are highly popular among OTs but rarely used by physiotherapists. Standardized batteries are more likely to be used by psychologists than therapists. The differences in research involvement and in professional training may help to explain this professional difference, together with specificities and goals of each of these activities (e.g., diagnostic evaluation versus delivering therapy). The majority of OTs in the present study reported no involvement in research, whereas the majority of psychologists reported some. The clinical training of psychologists, which advocates a brain-behaviour approach to defining and measuring neuropsychological syndromes, and their exposure to clinical research, which often uses cognitive test batteries such as the BIT and OCS, may predispose psychologists to using batteries. Conversely, those OTs who report no involvement in research may be more inclined to select individual tests that are used routinely on stroke wards. This is corroborated by free-text responses, where an emergent theme from clinician responses was a need for enhanced training in neglect aetiology and how to use screening and diagnostic assessments more comprehensively. Data in also suggests that selection of assessments is down to clinical and professional experience, with most individual cognitive assessments selected on the basis of professional choice, rather than some institutional policy.
Similarly, respondents often reported that subtests of batteries are generally found to be easier to administer than complete batteries, which were often felt to require too much time. A potential outcome from this finding regarding cognitive assessments is also reflected in the free-text responses. Respondents suggested further research is needed to either update or develop comprehensive cognitive assessments to generate results with potential clinical impact. However, given the number of individual assessments and batteries that already exist, further research might identify the most optimal combinations of these. Indeed, in free text responses detailing the “ideal” scenario for neglect assessment, several respondents highlighted the combinatorial approach taken. This is a key strength of current clinical practice and complies with the current UK national clinical guideline for stroke (see section 4.3.7.1 (B)) which advocates use of a standardized test battery and related effects on activities of daily living and mobility (Intercollegiate Stroke Working Party, Citation2016).
Functional assessments
OTs and physiotherapists most often selected the functional assessment category compared to physicians and psychologists. Respondents from other worldwide (non-Europe, non-USA) countries and from Italy were significantly more likely to select functional assessments, as were those working in outpatient settings.
The use of functional assessments was high in Menon-Nair et al.’s, Citation2006 review of clinical notes from Canadian inpatient settings. Indeed, the prevalence of use of assessments such as observation (during clinical care, examination, or ADL assessment) was relatively high at 48%, 57%, and 46% respectively. This is in line with our findings, where functional observation, interview, and the generic FIM were extremely popular. Observation and interview approaches were particularly favoured by OTs, whereas the FIM was overall selected by a greater proportion of physiotherapists. The FIM is the exception within this trio whereby it was generally selected as a result of institutional policy rather than professional choice. The use of the FIM in isolation to identify neglect is not usually recommended (please note our reservation in using the FIM as a neglect diagnostic measure below), since various neglect-specific assessments have been developed that identify the presence and severity of neglect in different domains (Chen, Chen, et al., Citation2015; Gialanella & Ferlucci, Citation2010; Luukkainen-Markkula et al., Citation2011). It is not surprising that OTs and physiotherapists are more inclined to select observational and/or interview approaches as they are feasible to integrate into routine clinical care, particularly if assessments are conducted away from inpatient wards. However, the common co-occurrence of anosognosia potentially results in an interview that does not identify the presence of neglect. Similarly, training for OTs and physiotherapists tends to focus on functional recovery and supporting activity, whereas physicians and psychologists are likely to be trained in terms of neurological and/or cognitive impairments at the neural level.
There was greater variation between functional assessments in terms of reasons for their selection, compared to responses generated for the cognitive and neurological categories. The individual assessments selected due to institutional policy in the functional category were generally not neglect-specific and are used as general assessments to quantify stroke severity and outcome in the acute and post-acute settings (i.e., the FIM, MPI, mRS and BI). Whilst these assessments are undoubtedly useful in planning clinical care for stroke patients with neglect, these measures in isolation do not adequately capture the profile of the neglect syndrome for individual patients. Respondents selected a number of neglect-specific tools above, and it seems likely that institutionally dictated assessment choices such as the FIM, MPI, mRS and BI are part of routine assessment upon admission and continued inpatient care and are applied in conjunction with neglect-specific assessments as and when required. As mentioned, use of these broader functional assessments in isolation to identify neglect is not usually recommended. Institutions must be made aware that they risk not providing the best care for people with neglect if they do not mandate specific measures.
The results from Menon-Nair et al.’s (Citation2007) study of Canadian OTs differ from those of the present survey study. The 2007 survey found that use of standardized assessment that incorporates assessment of function was extremely low compared to standardized cognitive assessments, regardless of whether these are specific or non-specific to neglect. The focus of OT respondents to the 2007 survey appears to be heavily skewed in the direction of cognition and perception, with only the A1 – Árnadóttir neurobehavioural evaluation (Árnadóttir, Citation1990) representing any assessment of function in the screening and diagnosis of USN. However, for our study, and specific to OTs, our results demonstrate that function is a major consideration for neglect identification. This was demonstrated by the proportion of OTs selecting functional assessments, as well as the free-text responses that emphasize incorporating functional assessment in neglect detection. This either represents a paradigm shift within the OT profession in the past twelve years, or could be due to the present survey offering assessment options divided by category of assessment, rather than allowing a series of open-ended responses based on case vignettes as previously. In either case, current screening and diagnosis by international OTs clearly has a focus on functional assessments.
Neurological assessments and neuroimaging/neuromodulation
Neurological assessments/clinical examination were popular amongst all countries, with between 60% and 75% of respondents indicating their use of these. They were most popular amongst physicians and physiotherapists, with psychologists and “other” professional groups significantly less likely to select this category. In terms of individual neurological assessments, there is a highly consistent pattern between them in terms of which professionals (and from which countries) select them. Selection of visual scanning and trunk rotation are exceptions to this general rule, which OTs are slightly more likely than physicians to use. Another exception is somatoparaphrenia, which physiotherapists rarely screen for. Physiotherapists were more likely to select all but four of the individual neurological assessments provided within the survey. The physiotherapists’ assessments mostly used observation, general attention, head position, motor neglect, trunk rotation, and posture.
Given the marked heterogeneity in the clinical presentation of neglect (Ting et al., Citation2011; Verdon et al., Citation2010), clinicians may be of the view that a number of different neurological signs are necessary to provide adequate neurocognitive profiling of the syndrome. Relatedly, neglect may manifest alongside various co-morbidities. Neglect and visual field loss often co-occur, as can hemiplegia (Gallagher et al., Citation2013), delirium (Boukrina & Barrett, Citation2017), and anosognosia (Bisiach et al., Citation1986; Chen & Toglia, Citation2019; Vocat et al., Citation2010). The use of neurological assessments that are not specific to neglect (see list of assessments in appendix) could be a useful approach for the detection of co-morbidities.
We were curious to discover whether neuroimaging/neuromodulation played a role in screening and diagnosing neglect and found they were selected the most by psychologists and physicians, although not by a majority in either category. Neuroimaging/neuromodulation were also selected by a greater proportion of respondents from Italy and other Non-Europe, Non-USA, but this is a small proportion of the overall sample. Neuroimaging is standard for newly admitted stroke patients for hyperacute treatments. However, reading neuroimaging reports is not within the scope of practice by therapy staff (e.g., OTs, PTs, and speech therapists) in many countries, including the UK and USA.
We found that MRI is particularly popular amongst this sample. The benefit of this technology is its extremely good spatial resolution of cortical and subcortical structures, which lends itself naturally to voxel-based lesion mapping (VBLM), which appeared in free-text responses to the neuroimaging question in the survey. VBLM is used to assess the extent of lesions to predict likely cognitive and functional impairments. Importantly, several respondents clarified that this was not used as a primary method for neglect detection. MRI and other neuroimaging methods were reported to be used alongside other neurological assessments, as well as cognitive and functional assessments.
Limitations
Despite its many strengths in laying a foundation for subsequent collaborative action towards consensus the study’s limitations should be acknowledged. We sought to identify the most commonly used neglect assessments by stroke clinicians worldwide. To do this, a non-exhaustive list of assessments was categorized into cognitive, functional, and neurological approaches. Whilst this list allowed us to more easily quantify their use (and for which reason), the free-text responses after each category highlighted more assessments that could have been included in the main quantitative analyses. Similarly, to avoid overburdening respondents and elicit high quality data we did not ask whether clinicians differentiated between neglect subtypes (e.g., personal vs peri-personal), severity or setting nor whether they considered the sensitivity and specificity of measures although respondents had opportunities to include these issues in their free text responses. The category least likely to be used (neuroimaging/neuromodulation category) was left entirely as a free-text response, instead of providing neuroimaging techniques that respondents could select as per the other categories.
The reported use of the non-neglect specific measures such as the FIM and BI (and, in a minority, neuroimaging/neuromodulation) raises the possibility that survey respondents misread the survey question as being about screening for stroke disability in general. We do not think it is very likely that there was a widespread failing across the large sample given that the participant information sheet specified that the study was about screening for neglect, we carefully avoided overburdening respondents with too many questions and laid them out clearly and the respondents’ free text answers suggested this focus on neglect had been communicated. Instead, reported use of these measures seemed to be mandated by institutional policy. Although we are too early in the consensus-making process to make recommendations about what should be used we can and do say above that we do not believe these general measures adequately capture the profile of the neglect syndrome for individual patients.
There is a possible limitation related to the wording of our response options to uncover reasons for assessment use. We asked participants to indicate whether they used an assessment based on institutional policy or professional choice. The former term was not defined and might have served as a catch-all categorization that encompassed clinical guidelines, insurance requirements, local or national policy in stroke. However, the inclusion of this wording against the alternative “professional choice” is, we feel, intuitive for the clinicians we targeted, and has revealed interesting differences between free choice and policy, even if the specific reasons for policy are not known.
A methodological consideration for this study was the use of an online, rather than paper, platform to host the survey. Whilst this approach brings many benefits in terms of convenience for both respondents and researchers, there is always the issue of accessibility. We did not have any information regarding the potential size of our target population (i.e., international stroke clinicians of different specialities), and thus cannot comment on response rate. Our approach of targeting clinicians online via professional bodies, organizations, and personal networks may not have reached some clinicians. Similarly, some clinicians may not have been able to access the SelectSurvey platform – due to institutional restrictions on external web access, or the device they were using. Balanced against this is that we elicited the participation of 454 valid, clinically active respondents from a large number of countries and from the key professional groups, strengthening the external validity of our findings. It is possible that some respondents were unsure about the screening and diagnosis of spatial neglect and therefore participated in this survey as a means of gaining more information. However, the magnitude of interest supports our view that there is a clinical need and moves us forward to the next stage of reaching consensus.
A final consideration is that this survey was written in English. The rationale for not seeking professional translation was the assumption that most international clinicians will have working knowledge of written English to consume clinical research, receive and/or undertake clinical training, and attend conferences. The existence of the survey only in English could have limited the sample. Although online translation tools are readily available, low- and middle-income countries may have had less opportunities to participate.
Conclusion
This study, designed by our interdisciplinary and international collaboration, confirms and quantifies the large number of methods that healthcare professionals use to screen for and diagnose spatial neglect after stroke. Whilst there are interesting differences in the approaches chosen by key professional groups such as occupational therapy and psychology, there is intra-professional consistency and less variability between countries. Despite the differences, there are tentative signs of an emerging consensus, an identified need for a combined approach to screening and diagnosis, and for further training. Although it is too early in our research programme to say what should be used, healthcare professionals can use these initial findings as a benchmark against which to evaluate their own practice. As professionals largely reported that they have clinical autonomy in choice of approaches rather than being bound by institutional policy, there is potential to engage in a collaborative action to finalize consensus for a core screening set and ultimately a core outcome set. We welcome interest from clinicians, researchers and stroke survivors in participating in the next steps towards reaching consensus. Several projects are in progress or in planning. These include an ongoing review using PRISMA-ScR guidelines, led by colleagues in Adelaide, of the psychometric properties of screening and diagnostic methods, including sensitivity and specificity. We will also seek differentiation for neglect subtypes, severities and settings. An interesting direction for future work is the design of valid and reliable tests to evaluate treatment outcomes for spatial neglect. The findings from the present survey and ongoing systematic review will feed into consensus-building activities such as Delphi and an expert panel of key stakeholders, moving us from what is used in clinical practice to agreeing what should be used in practice and research.
Supplemental Material
Download PDF (402.9 KB)Acknowledgements
The project was funded by the University of Manchester Research Impact Scholarship (MC) and Stroke Association (AB). Co-authors acknowledge financial support from: National Institute on Disability, Independent Living, and Rehabilitation Research, the New Jersey Commission on Brain Injury Research and the Wallerstein Foundation (PC); National Institutes of Health Eunice Kennedy Shiver National Institute of Child Health and Human Development Rehabilitation Researcher Career Development Program (KH), Swiss National Science Foundation (PV). Funding bodies had no role in study design, data collection, data analysis, data interpretation or writing of the paper. The views expressed are those of the authors, and not necessarily those of their institutions or funding bodies. The authors thank all the participants and the professional bodies worldwide who helped to distribute the survey.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Albert, M. L. (1973). A simple test of visual neglect. Neurology, 23(6), 658–664. https://doi.org/10.1212/WNL.23.6.658
- Andrade, K., Samri, D., Sarazin, M., de Souza, L. C., Cohen, L., de Schotten, M. T., Dubois, B., & Bartolomeo, P. (2010). Visual neglect in posterior cortical atrophy. BMC Neurology, 10(1), https://doi.org/10.1186/1471-2377-10-68
- Árnadóttir, G. (1990). The brain and behaviour: Assessing cortical dysfunction through activities of daily living. Mosby.
- Basagni, B., De Tanti, A., Damora, A., Abbruzzese, L., Varalta, V., Antonucci, G., Bickerton, W. L., Smania, N., & Mancuso, M. (2017). The assessment of hemineglect syndrome with cancellation tasks: A comparison between the Bells test and the apples test. Neurological Sciences, 38(12), 2171–2176. https://doi.org/10.1007/s10072-017-3139-7
- Bender, M. B. (2011). Disorders in perception: With particular reference to the phenomena of extinction and displacement. In Disorders in perception: With particular reference to the phenomena of extinction and displacement. https://doi.org/10.1037/13218-000
- Bergego, C., Azouvi, P., Samuel, C., Marchal, F., Louis-Dreyfus, A., Jokic, C., Morin, L., Renard, C., Pradat-Diehl, P., & Deloche, G. (1995). Validation d’une échelle d’évaluation fonctionnelle de l’héminégligence dans la vie quotidienne: L’échelle CB. Annales de Réadaptation et de Médecine Physique, 38(4), 183–189. https://doi.org/10.1016/0168-6054(96)89317-2
- Bickerton, W.-L., Riddoch, M. J., Samson, D., Balani, A. B., Mistry, B., & Humphreys, G. W. (2012). Systematic assessment of apraxia and functional predictions from the Birmingham cognitive screen. Journal of Neurology, Neurosurgery, Psychiatry, 83(5), 513–521. https://doi.org/10.1136/jnnp-2011-300968
- Bickerton, W. L., Samson, D., Williamson, J., & Humphreys, G. W. (2011). Separating forms of neglect using the Apples test: Validation and functional prediction in chronic and acute stroke. Neuropsychology, 25(5), 567–580. https://doi.org/10.1037/a0023501
- Bisiach, E., Vallar, G., Perani, D., Papagno, C., & Berti, A. (1986). Unawareness of disease following lesions of the right hemisphere: Anosognosia for hemiplegia and anosognosia for hemianopia. Neuropsychologia, 24(4), 471–482. https://doi.org/10.1016/0028-3932(86)90092-8
- Boukrina, O., & Barrett, A. M. (2017). Disruption of the ascending arousal system and cortical attention networks in post-stroke delirium and spatial neglect. Neuroscience & Biobehavioral Reviews, 83, 1–10. https://doi.org/10.1016/j.neubiorev.2017.09.024
- Bowen, A., Hazelton, C., Pollock, A., & Lincoln, N. B. (2013). Cognitive rehabilitation for spatial neglect following stroke. The Cochrane Database of Systematic Reviews, 7, CD003586. https://doi.org/10.1002/14651858.CD003586.pub3
- Boys, M., Fisher, P., Holzberg, C., & Reid, D. W. (1988). The OSOT perceptual evaluation: A research perspective. The American Journal of Occupational Therapy. : Official Publication of the American Occupational Therapy Association, 42(2), 92–98. https://doi.org/10.5014/ajot.42.2.92
- Brott, T., Adams, H. P., Olinger, C. P., Marler, J. R., Barsan, W. G., Biller, J., Spilker, J., Holleran, R., Eberle, R., & Hertzberg, V. (1989). Measurements of acute cerebral infarction: A clinical examination scale. Stroke, 20(7), 864–870. https://doi.org/10.1161/01.STR.20.7.864
- Buxbaum, L. J., Ferraro, M. K., Veramonti, T., Farne, A., Whyte, J., Ladavas, E., Frassinetti, F., & Coslett, H. B. (2004). Hemispatial neglect: Subtypes, neuroanatomy, and disability. Neurology, 62(5), 749–756. https://doi.org/10.1212/01.WNL.0000113730.73031.F4
- Chechlacz, M., Rotshtein, P., Bickerton, W.-L., Hansen, P. C., Deb, S., & Humphreys, G. W. (2010). Separating neural correlates of allocentric and egocentric neglect: Distinct cortical sites and common white matter disconnections. Cognitive Neuropsychology, 27(3), 277–303. https://doi.org/10.1080/02643294.2010.519699
- Chechlacz, M., Rotshtein, P., Roberts, K. L., Bickerton, W.-L., Lau, J. K. L., & Humphreys, G. W. (2012). The prognosis of allocentric and egocentric neglect: Evidence from clinical scans. PLoS One, 7(11), 11. https://doi.org/10.1371/journal.pone.0047821
- Chen, P., Caulfield, M. D., Hartman, A. J., O’Rourke, J., & Toglia, J. (2017). Assessing viewer-centered and stimulus-centered spatial bias: The 3s spreadsheet test version 1. Applied Neuropsychology: Adult, 24(6), 532–539. https://doi.org/10.1080/23279095.2016.1220382
- Chen, P., Chen, C. C., Hreha, K., Goedert, K. M., & Barrett, A. M. (2015). Kessler foundation neglect assessment process uniquely measures spatial neglect during activities of daily living. Archives of Physical Medicine and Rehabilitation, 96(5), 869–876. https://doi.org/10.1016/j.apmr.2014.10.023
- Chen, P., Hreha, K., Fortis, P., Goedert, K. M., & Barrett, A. M. (2012). Functional assessment of spatial neglect: A review of the Catherine Bergego scale and an introduction of the Kessler foundation neglect assessment process. Topics in Stroke Rehabilitation, 19(5), 423–435. https://doi.org/10.1310/tsr1905-423
- Chen, P., Hreha, K., Kong, Y., & Barrett, A. M. (2015). Impact of spatial neglect on stroke rehabilitation: Evidence from the setting of an inpatient rehabilitation Facility. Archives of Physical Medicine and Rehabilitation, 96(8), 1458–1466. https://doi.org/10.1016/j.apmr.2015.03.019
- Chen, P., & Toglia, J. (2019). Online and offline awareness deficits: Anosognosia for spatial neglect. Rehabilitation Psychology, 64(1), 50. https://doi.org/10.1037/rep0000207
- Colarusso, R. P., & Hammill, D. D. (1972). Motor-free visual perception test. Academic Therapy Publications.
- Colarusso, R. P., & Hammill, D. D. (2003). Motor-free perception test (MVPT-3). Academic Therapy Publications.
- Corbetta, M., & Shulman, G. L. (2011). Spatial neglect and attention networks. Annual Review of Neuroscience, 34(1), 569–599. https://doi.org/10.1146/annurev-neuro-061010-113731
- Gallagher, M., Wilkinson, D., & Sakel, M. (2013). Hemispatial neglect: Clinical features, assessment and treatment. British Journal of Neuroscience Nursing, 9(6), 273–277. https://doi.org/10.12968/bjnn.2013.9.6.273
- Gauthier, L., Dehaut, F., & Joanette, Y. (1989). The bells test: A quantitative and qualitative test for visual neglect. International Journal of Clinical Neuropsychology, 11, 49–54.
- Gialanella, B., & Ferlucci, C. (2010). Functional outcome after stroke in patients with aphasia and neglect: Assessment by the motor and cognitive functional independence measure instrument. Cerebrovascular Diseases, 30(5), 440–447. https://doi.org/DOI/10.1159/000317080
- Halligan, P. W., & Robertson, I. (1999). Spatial neglect: A clinical handbook for diagnosis and treatment. Psychology Press.
- Hammerbeck, U., Gittins, M., Vail, A., Paley, L., Tyson, S. F., & Bowen, A. (2019). Spatial neglect in stroke: Identification, disease process and association with outcome during inpatient rehabilitation. Brain Sciences, 9(12), 374. https://doi.org/10.3390/brainsci9120374
- Hebert, D., Lindsay, M. P., McIntyre, A., Kirton, A., Rumney, P. G., Bagg, S., Bayley, M., Dowlatshahi, D., Dukelow, S., & Garnhum, M. (2016). Canadian stroke best practice recommendations: Stroke rehabilitation practice guidelines, update 2015. International Journal of Stroke, 11(4), 459–484. https://doi.org/10.1177/1747493016643553
- Intercollegiate Stroke Working Party. (2016). National clinical guideline for stroke. London, UK: Royal College of Physicians. https://www.strokeaudit.org/Guideline/Full-Guideline.aspx
- Keith, R. A., Granger, C. V., Hamilton, B. B., & Sherwin, F. S. (1987). The functional independence measure: A new tool for rehabilitation. Advances in Clinical Rehabilitation, 1, 6–18.
- Lawton, M. P., & Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3_Part_1), 179–186. https://doi.org/10.1093/geront/9.3_Part_1.179
- Luukkainen-Markkula, R., Tarkka, I. M., Pitkänen, K., Sivenius, J., & Hämäläinen, H. (2011). Comparison of the behavioural inattention test and the Catherine Bergego scale in assessment of hemispatial neglect. Neuropsychological Rehabilitation, 21(1), 103–116. https://doi.org/10.1080/09602011.2010.531619
- Mahoney, F. I., & Barthel, D. W. (1965). Functional evaluation: The Barthel index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Medical Journal, 14, 61–65.
- Menon-Nair, A., Korner-Bitensky, N., & Ogourtsova, T. (2007). Occupational therapists’ identification, assessment, and treatment of unilateral spatial neglect during stroke rehabilitation in Canada. Stroke, 38(9), 2556–2562. https://doi.org/10.1161/STROKEAHA.107.484857
- Menon-Nair, A., Korner-Bitensky, N., Wood-Dauphinee, S., & Robertson, E. (2006). Assessment of unilateral spatial neglect post stroke in Canadian acute care hospitals: Are we neglecting neglect? Clinical Rehabilitation, 20(7), 623–634. https://doi.org/10.1191/0269215506cr974oa
- National Stroke Foundation. (2019). Clinical guidelines for stroke management. Melbourne, Australia: National Stroke Foundation. https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management
- Nijboer, T., van de Port, I., Schepers, V., Post, M., & Visser-Meily, A. (2013). Predicting functional outcome after stroke: The influence of neglect on basic activities in daily living. Frontiers in Human Neuroscience, 7, 182. https://doi.org/10.3389/fnhum.2013.00182
- Rode, G., Pagliari, C., Huchon, L., Rossetti, Y., & Pisella, L. (2017). Semiology of neglect: An update. Annals of Physical and Rehabilitation Medicine, 60(3), 177–185. https://doi.org/10.1016/j.rehab.2016.03.003
- Ting, D. S. J., Pollock, A., Dutton, G. N., Doubal, F. N., Ting, D. S. W., Thompson, M., & Dhillon, B. (2011). Visual neglect following stroke: Current concepts and future focus. Survey of Ophthalmology, 56(2), 114–134. https://doi.org/10.1016/j.survophthal.2010.08.001
- Tyerman, R., Tyerman, A., Howard, P., & Hadfield, C. (1986). The Chessington OT neurological assessment battery. Nottingham Rehabilitation.
- Verdon, V., Schwartz, S., Lovblad, K.-O., Hauert, C.-A., & Vuilleumier, P. (2010). Neuroanatomy of hemispatial neglect and its functional components: A study using voxel-based lesion-symptom mapping. BRAIN, 133(3), 880–894. https://doi.org/10.1093/brain/awp305
- Vocat, R., Staub, F., Stroppini, T., & Vuilleumier, P. (2010). Anosognosia for hemiplegia: A clinical-anatomical prospective study. Brain, 133(12), 3578–3597. https://doi.org/10.1093/brain/awq297
- Vuilleumier, P. (2013). Mapping the functional neuroanatomy of spatial neglect and human parietal lobe functions: Progress and challenges. Annals of the New York Academy of Sciences, 1296(1), 50–74. https://doi.org/10.1111/nyas.12161
- Wee, J. Y. M., & Hopman, W. M. (2008). Comparing consequences of right and left unilateral neglect in a stroke rehabilitation population. American Journal of Physical Medicine and Rehabilitation, 87(11), 910–920. https://doi.org/10.1097/PHM.0b013e31818a58bd
- Wilkinson, D., Sakel, M., Camp, S.-J., & Hammond, L. (2012). Patients with hemispatial neglect are more prone to limb spasticity, but this does not prolong their hospital stay. Archives of Physical Medicine and Rehabilitation, 93(7), 1191–1195. https://doi.org/10.1016/j.apmr.2012.01.010
- Wilson, B., Cockburn, J., & Halligan, P. (1987). Development of a behavioral test of visuospatial neglect. Archives of Physical Medicine and Rehabilitation, 68(2), 98–102.
- Winstein, C. J., Stein, J., Arena, R., Bates, B., Cherney, L. R., Cramer, S. C., Deruyter, F., Eng, J. J., Fisher, B., & Harvey, R. L. (2016). Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 47(6), e98–e169. https://doi.org/10.1161/STR.0000000000000098
- Zoccolotti, P., Antonucci, G., & Judica, A. (1992). Psychometric characteristics of two semi-structured scales for the functional evaluation of hemi-inattention in extrapersonal and personal space. Neuropsychological Rehabilitation, 2(3), 179–191. https://doi.org/10.1080/09602019208401407