ABSTRACT
Many stroke patients and partners suffer from anxiety, depression, and low life satisfaction. Psychological factors such as coping style and self-efficacy can be protective factors within individuals. The close relationship between stroke patients and partners suggests that there may be interdependence in psychological functioning. The aim of this study was to examine intra- and interpersonal effects of coping style and self-efficacy on anxiety, depression, and life satisfaction in patient–partners couples. In this prospective cohort study, pro-active coping (UPCC), general self-efficacy (GSES), anxiety (HADS-A), depression (HADS-D), and life satisfaction (1–6 scale) were assessed in 215 couples at 2 and 12 months post-stroke. Effects within couples were assessed using structural equation modelling. Several intra- and interpersonal effects of coping style and self-efficacy at 2 months post-stroke were related to emotional health at 12 months post-stroke. Most effects were intrapersonal effects. The interpersonal effects were small but showed that pro-active coping by the patient was associated with lower anxiety of the partner. Higher self-efficacy of the partner was associated with lower depression scores and higher life satisfaction of the patient. This study underscores the importance of a dyadic approach to post-stroke functioning. It supports a family-based approach for treating post-stroke emotional problems.
Introduction
Surviving stroke has a profound impact on the lives of patients and their partners.
This is reflected in an increased prevalence of mood disorders in patients after stroke, both in the acute and chronic phase (Mitchell et al., Citation2017; Rafsten et al., Citation2018; Schöttke & Giabbiconi, Citation2015). More than a third of patients report symptoms of anxiety and depression, even years after stroke (Ayerbe et al., Citation2013; Ayerbe, Ayis, Crichton, Wolfe, et al., Citation2014; Hackett & Pickles, Citation2014; Rafsten et al., Citation2018; Robinson & Jorge, Citation2016). Anxiety in patients with stroke is associated with lower quality of life (Ayerbe, Ayis, Crichton, Wolfe, et al., Citation2014; Donnellan et al., Citation2010). They are more dependent and have restricted participation compared to patients without anxiety (Chun et al., Citation2018).
Depression in patients with stroke is associated with decreased functional outcomes (Donnellan et al., Citation2010; Kutlubaev & Hackett, Citation2014) and increased mortality, most notable in young patients (<65 years) (Ayerbe, Ayis, Crichton, Rudd, et al., Citation2014). Depression is a determinant of life satisfaction, which is also reduced in patients with stroke (Carlsson et al., Citation2007; Oosterveer et al., Citation2017; Röding et al., Citation2010).
There is also a major impact of stroke on the patient's partner and their psychosocial functioning (Visser-Meily et al., Citation2009). As in patients with stroke, symptoms of anxiety (Kruithof et al., Citation2016; Wilz & Kalytta, Citation2008) and depression (Haley et al., Citation2015; Loh et al., Citation2017) have an increased prevalence in their partners or primary care-takers. Studies have shown that in the period following stroke, around 30% of partners report feelings of anxiety (Kruithof et al., Citation2016; Wilz & Kalytta, Citation2008). The global pooled prevalence of depression in care-takers was 40.2% as shown in a meta-analysis (Loh et al., Citation2017). Life satisfaction in partners is also reduced (Carlsson et al., Citation2007), with one study indicating that three years after stroke, 50% of partners are dissatisfied with their life as a whole (compared to 28% of patients) (Achten et al., Citation2012).
Psychological factors might play a protective role or constitute risk factors in the increased prevalence of anxiety, depression, and decreased life satisfaction in stroke patients and their partners. This can be understood through theoretical models regarding coping and stress, such as the transactional model of stress and coping (Folkman et al., Citation1986). In this model, stress is conceptualized as “a relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and as endangering well-being”, whereas coping refers to “the person's cognitive and behavioural efforts to manage the internal and external demands of [stress]” (Folkman et al., Citation1986, p. 572). This means that no situation is inherently stressful; it is a subjective appraisal of the situation that deems it harmful or threatening. This model theorizes that when coping is adequate it can reduce the impact of stressful circumstances. However, when coping is inadequate, it may fail to reduce stress or might even exacerbate stress (Panicker & Ramesh, Citation2019).
There is also empirical evidence for the importance of psychological factors in psychosocial outcomes in patients with stroke and their partners. Psychological factors such as an active coping style and higher self-efficacy are associated with decreased prevalence of depressive symptoms, lower anxiety scores, and better quality of life in patients after stroke (Tielemans et al., Citation2015; van Mierlo et al., Citation2015), whereas passive coping styles were associated with post-stroke depression in patients (Visser et al., Citation2015). For partners of patients with stroke, having a passive coping style was identified as an important predictor of life satisfaction and depressive symptoms (Visser-Meily et al., Citation2005). Low pro-active coping and low self-efficacy of the partner were associated with anxiety and depression in the partner (Kruithof et al., Citation2016).
The daily, close relationship between patient and partner implies interdependence in functioning. However, research on the effect of psychological factors on mood disorders and well-being using a dyadic perspective is sparse (Chung et al., Citation2016; Scholten et al., Citation2020; Wan-Fei et al., Citation2017). To get a better understanding of the effect of psychological factors in a dyad we need to examine intra- and interpersonal effects on both individuals at the same time and take into account their interdependence. A conceptual and statistical method that is well equipped for the dyadic perspective is the actor–partner interdependence model (Cook & Kenny, Citation2005). In this model, intrapersonal (actor) effects represent how an exposure variable affects the individual's own outcome, whereas the interpersonal (partner) effects represent how an exposure variable affects the other individual's outcome. Exposure variables and outcomes of both individuals are included in the same analysis to account for their interdependence. To our knowledge, the actor–partner interdependence model has not yet been used to examine the intra- and interpersonal effects of pro-active coping and self-efficacy on anxiety, depression, and life satisfaction.
We believe more knowledge concerning stroke patients–partner couples and their dyadic functioning could guide family-centred rehabilitation care, and hopefully, ameliorate the detrimental effects of mental health problems on patients’ and partners’ functioning.
The main aim of this study was to determine the intra- and interpersonal effects of coping style and self-efficacy on anxiety, depression, and life satisfaction in stroke patient–partner couples. The prevalence of clinically relevant levels of anxiety and depression and low life satisfaction was also determined in these couples at 2 and 12 months post-stroke. We expected to find intrapersonal but also interpersonal effects of these factors in patients and partners, as suggested by their intimate relationship.
Methods
Participants
This study used data collected in the Restore4Stroke Cohort study, a general hospital-based multi-centre longitudinal study, in which patients with stroke, at least 18 years old, with a clinically confirmed diagnosis of stroke, were included within seven days after their stroke (van Mierlo et al., Citation2014).
The patients were recruited consecutively from six general hospitals across the Netherlands between March 2011 and March 2013. Their partners were also included and were also at least 18 years old. The couples were married or in a steady relationship. Exclusion criteria for patients and their partners were: having another serious health condition that could be expected to interfere with study outcomes (such as neuromuscular disease), a Barthel index (BI) of 17 or lower, indicating pre-stroke dependency in activities of daily living, and having insufficient command of Dutch to complete the questionnaires. Patients were also excluded if they had shown signs of cognitive decline before their stroke, as measured by the Heteroanamnesis List Cognition (Meijer et al., Citation2006).
The Restore4Stroke Cohort study was approved by the Medical Ethics Committee of the St. Antonius Hospital, Nieuwegein. Informed consent was obtained from all participants.
Variables
Outcome variables
Symptoms of anxiety and depression were assessed with the Hospital Anxiety and Depression Scale (HADS) (Snaith & Zigmond, Citation1986). This questionnaire consists of seven items on anxiety (HADS-A) and seven items on depression (HADS-D), and each item is rated on a four-point scale, ranging from “0” (no symptoms) to “3” (maximum impairment). When a score of 8 or more is reached on either subscale, this can be interpreted as indicative of a high level of anxiety or high depressive symptoms (De Wit et al., Citation2008). The HADS is known to have good psychometric properties in stroke and other populations (Ayis et al., Citation2018; Sagen et al., Citation2009; Spinhoven et al., Citation1997). In our study, internal consistency (Cronbach's α) for the HADS-anxiety in stroke patients and partners was 0.83 and 0.86 respectively at 2 months and 0.84 and 0.85, respectively, at 12 months post-stroke. Internal consistency for the HADS-depression in stroke patients was 0.80 at both 2 and 12 months post-stroke. Internal consistency for the HADS-depression in partners was 0.81 at 2 months and 0.79 at 12 months post-stroke.
Life satisfaction was determined by having patients and partners rate their current life satisfaction on a single item with a 6-point scale ranging from “1” (very dissatisfied) to “6” (very satisfied). This is the first question of the 2-item Life Satisfaction Questions questionnaire (LS Questions). This questionnaire has shown good validity in a population with spinal cord injury (Post et al., Citation2012). In the current study, only the first question was used as this measures current life satisfaction (the second question asked participants to compare current life satisfaction to previous life satisfaction). This score was dichotomized, in which a score of “3” (somewhat dissatisfied) or lower is classified as “dissatisfied”, whereas as a score of “4” (somewhat satisfied) or higher is classified as “satisfied”.
Independent variables
At baseline, data on age, gender, education level, stroke characteristics, and pre-stroke functioning were collected.
Coping style was determined using the Utrecht Proactive Coping Competence Scale (UPCC). This questionnaire consists of 21 items that are assessed on a 4-point scale ranging from “1” (not competent at all) to “4” (very competent). A higher score indicates higher levels of self-perceived pro-active coping styles (Bode et al., Citation2007). The UPCC is known to have good internal consistency and test-retest reliability when used in middle and late adulthood (Bode et al., Citation2007) and has been shown to have excellent reliability in stroke populations (Tielemans et al., Citation2014). Cronbach's α of the UPCC score in this study was 0.93 for stroke patients and 0.95 for their partners.
Self-efficacy was measured using the General Self-Efficacy Scale (GSES). This questionnaire consists of 10 items that are assessed on a four-point scale, ranging from “1” (not at all true) to “4” (completely true). Higher scores indicate higher levels of self-efficacy (Scholz et al., Citation2002). Psychometric properties of the GSES in the Dutch[ population are good (Scholz et al., Citation2002). The GSES is often used in stroke populations.
Internal consistency of the GSES score in stroke patients in this study was excellent (Cronbach’s α = 0.92), internal consistency of the GSES in their partners in this study was good (Cronbach’s α = 0.89).
Procedure
Patients and their partners were included within the first week post-stroke. Demographic characteristics such as age, gender, and educational levels as well as stroke characteristics were documented at inclusion. The UPCC and GSES were administered at 2 months post-stroke, the HADS and life satisfaction were administered at 2 and 12 months post-stroke, for both patients and partners. Patients and their partners were visited by a research assistant 2 months post-stroke, to administer observational measurements and questionnaires. Questionnaires were completed by patients and partners independently from each other. At 12 months post-stroke, patients and partners were given the choice to complete the questionnaires online or on paper.
Statistical analysis
Descriptive statistics were used to describe patient and partner characteristics.
For each couple, the outcomes were determined at 2 and 12 months post-stroke. Using the cut-off points for the HADS-A, HADS-D, and life satisfaction as described above, percentages of couples with and without clinically significant levels of symptoms of anxiety, depression, or low life satisfaction were calculated (e.g., a couple with symptoms has at least one member of the dyad who scores above the cut-off point).
An actor–partner interdependence model (APIM) was used to determine the intrapersonal and interpersonal effects of coping style and self-efficacy of patient and partner measured at 2 months post-stroke on anxiety, depression, and life satisfaction measured at 12 months post-stroke (Cook & Kenny, Citation2005). This allowed us to calculate intrapersonal effects (effects of one individual's variables on that same individual's outcomes, i.e., effects of patient variables on patient outcomes and effects of partner variables on partner outcomes), but also of interpersonal effects (effects of one individual's variables on the other person's outcomes, i.e., effects of patient variables on partner outcomes, and effects of partner variables on patient outcomes). This statistical method is well suited to test for dyadic correlations, as it takes into account the interdependence between the two members of a dyad. The APIM was performed using structural equation modelling as this allowed us to determine all effects sizes in the same model, as opposed to simple regression analysis, while also fitting well with the structure of our data. We did not use multilevel modelling because our data concerned dyads with distinguishable members, and the SEM allowed us to more easily estimate the inter- and interpersonal effects between these members. Effect sizes were reported as unstandardized beta-coefficients. R2 indicates the amount of variance explained by determinants included in the model. Models were corrected for the age and sex of the patient. We did not correct for stroke severity or cognitive symptoms as correlation analysis did not show that the score on the National Institutes of Health Stroke Scale (NIHSS) or Montreal Cognitive Assessment (MOCA) were significantly correlated to scores on the outcome measures (HADS-A, HADS-D, life satisfaction question).
SPSS version 24 was used for descriptive statistics. Mplus version 6.1 was used for the structural equation modelling.
In all statistical analyses, a p-value of <.05 was considered statistically significant.
If the relevant questionnaire was not completed in either patient or partner, the couple was excluded from the analysis for that outcome measure. Therefore the number of included couples varied per measure.
Results
Patient and partner characteristics
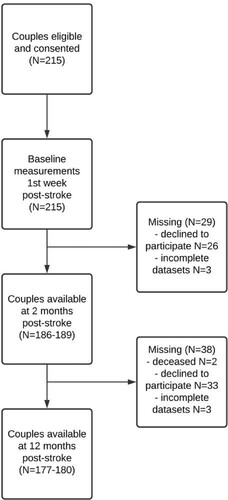
A total of 215 couples were included in the study. At 2 months post-stroke, 189 couples (87.9%) completed at least one of the questionnaires regarding the three outcome measures. At 12 months post-stroke, 180 couples (83.7%) completed at least one of the questionnaires regarding the three outcome measures. 177 couples (82.3%) had complete outcome measures at 12 months post-stroke. See for a flow chart of drop out during the study.
displays demographic and stroke characteristics of the couples that completed the questionnaires and the (partial) dropouts. There were no significant differences in the baseline characteristics or stroke characteristics between these groups.
Table 1. Baseline characteristics of patients and partners.
Patients were on average almost 64 years (SD = 10.9) old, and the majority (78.5%) were male. Partners were on average slightly younger, 62 years (SD = 10.7), and 22.0% were male. The vast majority of patients (94.9%) had suffered an ischaemic stroke.
The mean scores on the HADS-anxiety, HADS-depression, and life satisfaction question in patients and partners at 2 and 12 months post-stroke is shown in . Two months post-stroke, 18.5% of patients showed clinical levels of symptoms of anxiety and 18.0% showed clinical levels of symptoms of depression. One-year post-stroke, these proportions increased to 25.0% of patients with clinical levels of symptoms of anxiety and 25.6% of patients with clinical levels of depressive symptoms. The proportion of stroke patients with low life satisfaction decreased from 20.4% at 2 months post-stroke to 14.1% at 12 months post-stroke. In partners, the prevalence of clinical levels of symptoms of anxiety decreased from 29.1% at 2 months post-stroke to 19.4% at 12 months post-stroke, whereas the prevalence of clinical levels of symptoms of depression appeared to be stable (10.6% and 12.8%). The proportion of partners dissatisfied with life increased slightly from 12.4% at 2 months post-stroke to 18.1% at 12 months post-stroke.
Table 2. 12 months post-stroke.
Symptoms of anxiety or depression and dissatisfaction with life in couples after stroke
shows the percentages of couples with none, one or both individuals experiencing symptoms of anxiety, depression, or decreased life satisfaction. At 2 months post-stroke, 37.6% of couples had at least one individual experiencing clinical levels of symptoms of anxiety, this proportion decreased slightly to 33.9% at 12 months post-stroke.
Table 3. Prevalence of anxiety, depression, and life satisfaction in patient–partner couples.
At 2 months post-stroke, 25.4% of couples had at least one individual experiencing clinical levels of symptoms of depression, this proportion increased to 31.1% at 12 months post-stroke. At 2 months post-stroke, 25.3% of couples had at least one individual dissatisfied with life. At 12 months post-stroke, this was true for 24.9% of the couples.
Dyadic relationships between patients with stroke and their partner
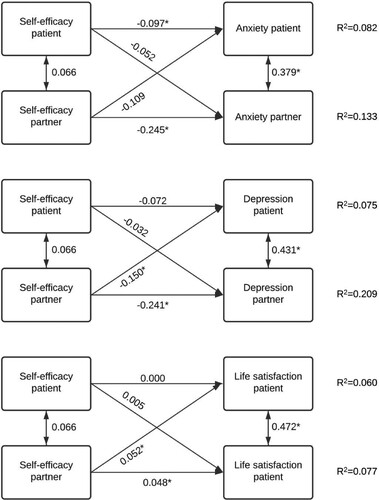
and show the dyadic relationships between pro-active coping and self-efficacy at 2 months post-stroke and anxiety, depression, and life satisfaction scores at 12 months post-stroke. Horizontal arrows indicate intrapersonal effects (effects of patient variables on patient outcomes, or effects of partner variables on partner outcomes). Diagonal arrows indicate interpersonal effects (effects of partner variables on patient outcomes, or effects of patient variables on partner outcomes). Correlations between the same independent variables and outcome variables of patients and partners are indicated with vertical arrows. All outcome variables in patients and partners were significantly correlated (anxiety r = 0.379, p = <.001, depression r = 0.431, p = <.001, life satisfaction r = 0.472, p = <.001).
Figure 2. Dyadic relationships of pro-active coping at 2 months with anxiety, depression, and life satisfaction at 12 months in the patient–partner couple. Results were adjusted for the age and sex of the patient. Single-headed arrows indicate inter- or intrapersonal effects in unstandardized beta-coefficients. Double-headed arrows indicate correlations between independent and outcome variables. *p < .05.
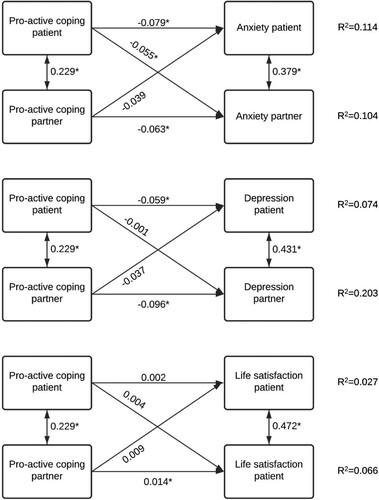
Figure 3. Dyadic relationships of self-efficacy at 2 months with anxiety, depression, and life satisfaction at 12 months in the patient–partner couple. Results were adjusted for the age and sex of the patient. Single-headed arrows indicate inter- or intrapersonal effects in unstandardized beta-coefficients. Double-headed arrows indicate correlations between independent and outcome variables. *p < .05.
Pro-active coping
Pro-active coping had multiple significant intrapersonal effects. Pro-active coping by the patient 2 months post-stroke was associated with lower anxiety scores (β = −0.079, SE = 0.026 p = .003) and lower depression scores (β = −0.059, SE = 0.028, p = 0.039) of the patient 12 months post-stroke. Pro-active coping by the partner was associated with lower anxiety scores (β = −0.063, SE = 0.023, p = .005), lower depression scores (β = −0.096, SE = 0.019, p < .001) and greater life satisfaction of the partner (β = 0.014, SE = 0.007, p = .039). A significant interpersonal effect also occurred; pro-active coping by the patient 2 months post-stroke was associated with lower anxiety scores of the partner (β = −0.055, SE = 0.026, p = .031) 12 months post-stroke. The other five partner effects of pro-active coping that were tested showed no significant associations (see ).
Self-efficacy
Higher self-efficacy had multiple significant intrapersonal effects. Self-efficacy of the patient 2 months post-stroke was associated with less anxiety of the patient 12 months post-stroke (β = −0.097, SE = 0.045, p = .031) and self-efficacy of the partner 2 months post-stroke was associated with less anxiety (β = −0.245, SE = 0.057, p < .001), less depression (β = −0.241, SE = 0.049, p<.001) and higher life satisfaction (β = 0.048, SE = 0.017, p = .005) of the partner 12 months post-stroke. Two significant interpersonal effects occurred; self-efficacy of the partner 2 months post-stroke was associated with less depression (β = −0.150, SE = 0.061, p = .014) and higher life satisfaction (β = 0.052, SE = 0.017, p = .002) of the patient 12 months post-stroke. The other four partner effects of self-efficacy that were tested showed no statistical significance (see ).
Discussion
In the current study, we reported prevalence rates of anxiety, depression, and life satisfaction per couple. We showed that in 37.6% of couples, one or both members showed clinically relevant symptoms of anxiety at 2 months post-stroke. At 12 months post-stroke, this proportion had decreased slightly, to 33.9%. As regards depression, 25.4% and 31.1% of couples showed clinically relevant symptoms at 2 and 12 months, respectively. In 25.3% of couples, at least one member was dissatisfied with life at 2 months post-stroke, while at 12 months post-stroke this was true for 24.9% of couples. To our knowledge, prevalence rates for anxiety and depression per couple have not been reported in earlier research. However, the prevalence of clinically significant symptoms of anxiety and depression that we reported for the individual members of the dyad (patients or partners) is in accordance with literature (Hackett & Pickles, Citation2014; Knapp et al., Citation2020; Loh et al., Citation2017; Rafsten et al., Citation2018), except for the prevalence for clinically relevant depressive symptoms in the partner which was markedly lower in our research population (10.6% at 2 months and 12.8% at 12 months). Pooled prevalence rates above 40% are reported in the literature for informal caregivers (Loh et al., Citation2017). This may be explained by differences in the characteristics of the study populations, differences in the timing of measurements after stroke or the use of other assessment methods to determine the presence of depressive symptoms.
For life satisfaction in couples, previous studies showed that in 29–41% of couples, both partners were satisfied with life (Achten et al., Citation2012; Carlsson et al., Citation2007; Eriksson et al., Citation2005). These are lower rates than we found in our study, which may be explained by the use of different follow-up times and the use of a different outcome measure and cut-off value.
The actor–partner interdependence model (APIM) showed 12 significant intra- and interpersonal effects of coping style and self-efficacy in couples. Intrapersonal effects were more numerous and overall had a larger effect size compared to the interpersonal effects. They indicate the importance of psychological factors in emotional health within the same individual. This is consistent with earlier studies, where pro-active coping and self-efficacy have been linked to lower anxiety and depression scores and passive coping has been associated with lower quality of life in patients after stroke (Gregorio et al., Citation2015; Tielemans et al., Citation2015). In partners of stroke patients, similar associations have been identified (Gregório et al., Citation2011; Visser-Meily et al., Citation2005).
The use of the APIM model allows us to compare effects in stroke patients and partners in the same model: in partners of stroke patients, all intrapersonal effects that were tested were significant. The psychological factors also explain more of the variance in outcome measures in the partners compared to the stroke patients.
Dyadic relationships in stroke research
An actor–partner interdependence model to determine the intra- and interpersonal effects of coping style and self-efficacy on symptoms of anxiety, depression, and life satisfaction in stroke patient–partner couples has not been used before to our current knowledge.
Although the effects of psychological factors within an individual are stronger than between individuals, we did show that interpersonal effects occur even when taking the intrapersonal effects into account. This is in line with findings from earlier studies that have looked specifically at the role that psychological factors play within the stroke patient–partner couple. Researchers found that stroke survivors’ perceived stress affected caregivers’ perceived stress in a significant interpersonal effect (Godwin et al., Citation2013). Patient distress was shown to be associated with both patients’ and caregivers’ illness representations (Twiddy et al., Citation2012). Another dyadic approach to quality of life research in stroke patient-caregiver couples showed that higher caregiver depression scores were associated with poorer quality of life in patients (Wan-Fei et al., Citation2017). Associations have also been found between partners with lower self-esteem and low optimism and higher depression scores of stroke survivors. Similarly, low self-esteem in patients was associated with higher depression scores in spouses (Chung et al., Citation2016). A linear regression study found associations between partners’ high burden and depression and patients’ depressive symptoms (Kruithof et al., Citation2016).
Overall, our current study and earlier studies show that patients and partners who appear to be handling their new situation well (e.g., through pro-active coping, high self-efficacy and self-esteem, or high optimism) can influence themselves but also their partner in a positive way. While intrapersonal effects are especially important, they do not give the complete picture of the effects of psychological factors within the stroke patient–partner couple.
Thus far, dyadic models have not been used extensively in stroke research. The use of actor–partner interdependence models for a dyadic approach to the functioning of patient–partner couples has been used more extensively and in large studies in other research fields, such as dementia research (Gellert et al., Citation2018; Lingler et al., Citation2016; Rippon et al., Citation2020; Wong & Hsieh, Citation2019).
Strengths and limitations of the study
A strength of the study is the inclusion of a large number of patients and their partners, shortly after a stroke, independent of discharge destination. The one-year follow-up allowed us to compare results in the subacute and chronic phases post-stroke. In this way, emotional health, and life satisfaction in the chronic phase can be related to coping style and self-efficacy measured in the subacute phase.
Furthermore, our study involved a couple-based perspective of the emotional health and life satisfaction of both patients and their partners. The APIM using SEM analysis gave us the opportunity to investigate the intra- and interpersonal effects within the dyad in one comprehensive model. Our study adds to the understanding of post-stroke functioning of not only the patient but of the patient–partner dyad.
A limitation of our study is that both patients and partners were relatively young compared to most stroke populations, with our patients having a mean age of 64. Also, there were few very young stroke patients under the age of 40 in our study population. A large proportion of the patients were male, whereas partners were mostly female. Almost 95% of patients had suffered from ischaemic stroke. These characteristics of our study population could limit generalizability to the general stroke population of patients and partners.
Also, we used an author-derived measure for life satisfaction that was not validated in stroke populations. This measure was also a single-item scale, which is not ideal in assessing psychological constructs.
The model is limited in the predictors that were included. Baseline (at the time of stroke) measurements of anxiety, depression, and life satisfaction were not conducted and thus not included in the APIM analyses. However, anxiety, depression, and life satisfaction at baseline could well be important predictors of anxiety, depression, and life satisfaction at 12 months. Not including these baseline measurements might contribute to the small amount of variance (R2) that the model explained. There are also other factors that could be well worth exploring, including other psychological factors such as self-esteem, optimism (Chung et al., Citation2016) and caregiver mastery (Cameron et al., Citation2011), or medical factors such as a previous history of mood disorders (Mitchell et al., Citation2017) or certain cognitive problems after stroke (Mitchell et al., Citation2017), and biological characteristics not included in our current model.
Clinical implications for a family-based approach to stroke rehabilitation care
The current study has added to the growing body of evidence for the high prevalence of clinically relevant levels of symptoms of anxiety and depression and low life satisfaction in stroke patient–partner couples, the importance of psychological factors with regards to mental health, and the interdependence of patient and partner functioning. This implies that a family-based approach by clinicians is vital; not just patients, but also partners are at risk for mood disorders. Health professionals also need to be aware that although an individual may not suffer from symptoms of anxiety or depression him- or herself, problems with mental health may still play an important role in his or her well-being through the relationship with their partner. For example, a mood disorder in the partner may greatly affect his or her ability to provide informal care.
Our study showed associations between coping style and self-efficacy measured at 2 months post-stroke, and anxiety, depression, and life satisfaction measured at 12 months post-stroke for both patients and partners. These points to an opportunity for early screening, assisting in identifying patients and partners at risk and possibly leading to early intervention. In our study, we identified many intrapersonal effects. Care interventions should therefore primarily be focused on the individual suffering from symptoms of anxiety, depression, or low life satisfaction and may focus on improving coping style and self-efficacy. Our study also suggests that improving coping style and self-efficacy may also improve the health outcomes of the other individual of the patient–partner dyad. This is why it can be relevant to use dyad-based interventions when appropriate.
In 2014, the American Heart Association and American Stroke Association released a statement regarding evidence for a family caregiver and dyad interventions post-stroke (Bakas et al., Citation2014). This statement was updated in 2017 (Bakas et al., Citation2017). Although many of the studies they reviewed had methodological limitations, they recommended that caregiver and dyad interventions should combine a psychoeducational component with a skill-building component, to improve psychosocial outcomes such as depression. A high refusal rate for support group formats was found, implying that large numbers of sessions with face-to-face contact may not be feasible for busy caregivers. Delivery of family-based approaches (partly) through telephone or web-based contacts may be easier to integrate with post-stroke care (Bakas et al., Citation2014, Citation2017).
A recent review evaluating the effect of dyadic psychoeducational interventions for stroke patients and their informal caregivers showed that these interventions can improve caregivers’ burden in the short term and patients’ quality of life in the long term, although more research into other psychosocial outcomes is needed (Mou et al., Citation2021).
In conclusion, this study provides further insight into the dyadic functioning of stroke patient and partner couples. Clinically relevant levels of symptoms of anxiety and depression and decreased life satisfaction are prevalent in these couples. When emotional functioning is viewed from a couple's perspective, both patient's and partner's psychological characteristics can play an important role. Intrapersonal effects dominate in number and effect size, but do not paint a complete picture; interpersonal effects of coping style and self-efficacy on anxiety and depression were also demonstrated.
We used coping and self-efficacy as the psychological determinants, and did not use other, sometimes related, psychological constructs, such as optimism, self-esteem, mastery, self-stigma, or personality traits. Furthermore, genetic and biological factors, apart from sex and age, were not included in the models.
More research is needed to better understand stroke patients and partners from a dyadic perspective, to identify other relevant factors for early screening, and to investigate if interventions aimed at psychological factors in both dyad members are clinically useful and effective.
Acknowledgements
The authors would like to thank all of the patients and their partners for their contribution to the Restore4Stroke Cohort study. The authors also want to thank the staff of the participating hospitals, as well as all the research assistants who collected the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Achten, D., Visser-Meily, J. M. A., Post, M. W. M., & Schepers, V. P. M. (2012). Life satisfaction of couples 3 years after stroke. Disability and Rehabilitation, 34(17), 1468–1472. https://doi.org/10.3109/09638288.2011.645994
- Ayerbe, L., Ayis, S., Crichton, S., Wolfe, C. D. A., & Rudd, A. G. (2013). The natural history of depression up to 15 years after stroke: The South London Stroke Register. Stroke, 44(4), 1105–1110. https://doi.org/10.1161/STROKEAHA.111.679340
- Ayerbe, L., Ayis, S., Crichton, S. L., Rudd, A. G., & Wolfe, C. D. A. (2014). Explanatory factors for the increased mortality of stroke patients with depression. Neurology, 83(22), 2007–2012. https://doi.org/10.1212/WNL.0000000000001029
- Ayerbe, L., Ayis, S. A., Crichton, S., Wolfe, C. D. A., & Rudd, A. G. (2014). Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: The South London Stroke Register. Age and Ageing, 43(4), 542–547. https://doi.org/10.1093/ageing/aft208
- Ayis, S. A., Ayerbe, L., Ashworth, M., & Wolfe, C. D. A. (2018). Evaluation of the Hospital Anxiety and Depression Scale (HADS) in screening stroke patients for symptoms: Item Response Theory (IRT) analysis. Journal of Affective Disorders, 228, 33–40. https://doi.org/10.1016/j.jad.2017.11.037
- Bakas, T., Clark, P. C., Kelly-Hayes, M., King, R. B., Lutz, B. J., & Miller, E. L. (2014). Evidence for stroke family caregiver and dyad interventions: A statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke, 45(9), 2836–2852. https://doi.org/10.1161/STR.0000000000000033
- Bakas, T., McCarthy, M., & Miller, E. T. (2017). Update on the state of the evidence for stroke family caregiver and dyad interventions. Stroke, 48(5), e122–e125. https://doi.org/10.1161/STROKEAHA.117.016052
- Bode, C., de Ridder, D., Kuijer, R., & Bensing, J. (2007). Effects of an intervention promoting proactive coping competencies in middle and late adulthood. The Gerontologist, 47(1), 42–51. https://doi.org/10.1093/geront/47.1.42
- Cameron, J. I., Cheung, A. M., Streiner, D. L., Coyte, P. C., & Stewart, D. E. (2011). Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years poststroke. Stroke, 42(2), 302–306. https://doi.org/10.1161/STROKEAHA.110.597963
- Carlsson, G. E., Forsberg-Wärleby, G., Möller, A., & Blomstrand, C. (2007). Comparison of life satisfaction within couples one year after a partner’s stroke. Journal of Rehabilitation Medicine, 39(3), 219–224. https://doi.org/10.2340/16501977-0048
- Chun, H.-Y. Y., Whiteley, W. N., Dennis, M. S., Mead, G. E., & Carson, A. J. (2018). Anxiety after stroke: The importance of subtyping. Stroke, 49(3), 556–564. https://doi.org/10.1161/STROKEAHA.117.020078
- Chung, M. L., Bakas, T., Plue, L. D., & Williams, L. S. (2016). Effects of self-esteem, optimism, and perceived control on depressive symptoms in stroke survivor-spouse dyads. The Journal of Cardiovascular Nursing, 31(2), E8–E16. https://doi.org/10.1097/JCN.0000000000000232
- Cook, W. L., & Kenny, D. A. (2005). The actor-partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. https://doi.org/10.1080/01650250444000405
- De Wit, L., Putman, K., Baert, I., Lincoln, N., Angst, F., & Beyens, H. (2008). Anxiety and depression in the first six months after stroke. A longitudinal multicentre study. Disability and Rehabilitation, 30(24), 1858–1866. https://doi.org/10.1080/09638280701708736
- Donnellan, C., Hickey, A., Hevey, D., & O’Neill, D. (2010). Effect of mood symptoms on recovery one year after stroke. International Journal of Geriatric Psychiatry, 25(12), 1288–1295. https://doi.org/10.1002/gps.2482
- Eriksson, G., Tham, K., & Fugl-Meyer, A. R. (2005). Couples’ happiness and its relationship to functioning in everyday life after brain injury. Scandinavian Journal of Occupational Therapy, 12(1), 40–48. https://doi.org/10.1080/11038120510027630
- Folkman, S., Lazarus, R. S., Gruen, R. J., & DeLongis, A. (1986). Appraisal, coping, health status, and psychological symptoms. Journal of Personality and Social Psychology, 50(3), 571–579. https://doi.org/10.1037//0022-3514.50.3.571
- Gellert, P., Häusler, A., Gholami, M., Rapp, M., Kuhlmey, A., & Nordheim, J. (2018). Own and partners’ dyadic coping and depressive symptoms in individuals with early-stage dementia and their caregiving partners. Aging & Mental Health, 22(8), 1008–1016. https://doi.org/10.1080/13607863.2017.1334759
- Godwin, K. M., Swank, P. R., Vaeth, P., & Ostwald, S. K. (2013). The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging & Mental Health, 17(4), 423–431. https://doi.org/10.1080/13607863.2012.756457
- Gregorio, W., Ponds, G., Smeets, R. W. H. M., Jonker, S. M. J., Pouwels, F., Verhey, C. G. J. G., R, F., & van Heugten, C. M. (2015). Associations between executive functioning, coping, and psychosocial functioning after acquired brain injury. The British Journal of Clinical Psychology, 54(3), 291–306. https://doi.org/10.1111/bjc.12074
- Gregório, W., Visser-Meily, G., Tan, J. M. A., Post, F. E. S., M, M. W., & van Heugten, C. M. (2011). Changes in the coping styles of spouses and the influence of these changes on their psychosocial functioning the first year after a patient’s stroke. Journal of Psychosomatic Research, 71(3), 188–193. https://doi.org/10.1016/j.jpsychores.2011.01.013
- Hackett, M. L., & Pickles, K. (2014). Part I: Frequency of depression after stroke: An updated systematic review and meta-analysis of observational studies. International Journal of Stroke: Official Journal of the International Stroke Society, 9(8), 1017–1025. https://doi.org/10.1111/ijs.12357
- Haley, W. E., Roth, D. L., Hovater, M., & Clay, O. J. (2015). Long-term impact of stroke on family caregiver well-being: A population-based case-control study. Neurology, 84(13), 1323–1329. https://doi.org/10.1212/WNL.0000000000001418
- Knapp, P., Dunn-Roberts, A., Sahib, N., Cook, L., Astin, F., Kontou, E., & Thomas, S. A. (2020). Frequency of anxiety after stroke: An updated systematic review and meta-analysis of observational studies. International Journal of Stroke: Official Journal of the International Stroke Society, 15(3), 244–255. https://doi.org/10.1177/1747493019896958
- Kruithof, W., Post, M., van Mierlo, M., Van den Bos, G., de Man-van Ginkel, J., & Visser-Meily, J. (2016). Caregiver burden and emotional problems in partners of stroke patients at two months and one year post-stroke: Determinants and prediction. Patient Education and Counseling, 99(10), 1632–1940. https://doi.org/10.1016/j.pec.2016.04.007
- Kutlubaev, M. A., & Hackett, M. L. (2014). Part II: Predictors of depression after stroke and impact of depression on stroke outcome: An updated systematic review of observational studies. International Journal of Stroke: Official Journal of the International Stroke Society, 9(8), 1026–1036. https://doi.org/10.1111/ijs.12356
- Lingler, J. H., Terhorst, L., Schulz, R., Gentry, A., & Lopez, O. (2016). Dyadic analysis of illness perceptions among persons with mild cognitive impairment and their family members. The Gerontologist, 56(5), 886–895. https://doi.org/10.1093/geront/gnv029
- Loh, A. Z., Tan, J. S., Zhang, M. W., & Ho, R. C. (2017). The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. Journal of the American Medical Directors Association, 18(2), 111–116. https://doi.org/10.1016/j.jamda.2016.08.014
- Meijer, R., van Limbeek, J., & de Haan, R. (2006). Development of the stroke-unit discharge guideline: Choice of assessment instruments for prediction in the subacute phase post-stroke. International Journal of Rehabilitation Research, 29(1), 1–8. https://doi.org/10.1097/01.mrr.0000175269.59788.41
- Mitchell, A. J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., & Meader, N. (2017). Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. General Hospital Psychiatry, 47, 48–60. https://doi.org/10.1016/j.genhosppsych.2017.04.001
- Mou, H., Wong, M. S., & Chien, W. T. P. (2021). Effectiveness of dyadic psychoeducational intervention for stroke survivors and family caregivers on functional and psychosocial health: A systematic review and meta-analysis. International Journal of Nursing Studies, 120, 103969. https://doi.org/10.1016/j.ijnurstu.2021.103969
- Oosterveer, D. M., Mishre, R. R., van Oort, A., Bodde, K., & Aerden, L. (2017). Depression is an independent determinant of life satisfaction. Journal of Rehabilitation Medicine, 49(3), 223–227. https://doi.org/10.2340/16501977-2199
- Panicker, A. S., & Ramesh, S. (2019). Psychological status and coping styles of caregivers of individuals with intellectual disability and psychiatric illness. Journal of Applied Research in Intellectual Disabilities: JARID, 32(1), 1–14. https://doi.org/10.1111/jar.12496
- Post, M. W., van Leeuwen, C. M., van Koppenhagen, C. F., & de Groot, S. (2012). Validity of the life satisfaction questions, the Life Satisfaction Questionnaire, and the Satisfaction With Life Scale in persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 93(10), 1832–1837. https://doi.org/10.1016/j.apmr.2012.03.025
- Rafsten, L., Danielsson, A., & Sunnerhagen, K. S. (2018). Anxiety after stroke: A systematic review and meta-analysis. Journal of Rehabilitation Medicine, 50(9), 769–778. https://doi.org/10.2340/16501977-2384
- Rippon, I., Quinn, C., Martyr, A., Morris, R., Nelis, S. M., Jones, I. R., Victor, C. R., & Clare, L. (2020). The impact of relationship quality on life satisfaction and well-being in dementia caregiving dyads: Findings from the IDEAL study. Aging & Mental Health, 24(9), 1411–1420. https://doi.org/10.1080/13607863.2019.1617238.
- Robinson, R. G., & Jorge, R. E. (2016). Post-stroke depression: A review. The American Journal of Psychiatry, 173(3), 221–231. https://doi.org/10.1176/appi.ajp.2015.15030363
- Röding, J., Glader, E.-L., Malm, J., & Lindström, B. (2010). Life satisfaction in younger individuals after stroke: Different predisposing factors among men and women. Journal of Rehabilitation Medicine, 42(2), 155–161. https://doi.org/10.2340/16501977-0497
- Sagen, U., Vik, T. G., Moum, T., Mørland, T., Finset, A., & Dammen, T. (2009). Screening for anxiety and depression after stroke: Comparison of the hospital anxiety and depression scale and the Montgomery and Asberg depression rating scale. Journal of Psychosomatic Research, 67(4), 325–332. https://doi.org/10.1016/j.jpsychores.2009.03.007
- Scholten, E. W. M., Ketelaar, M., Visser-Meily, J. M. A., Roels, E. H., Kouwenhoven, M., & Post, M. W. M. (2020). Prediction of psychological distress among persons with spinal cord injury or acquired brain injury and their significant others. Archives of Physical Medicine and Rehabilitation, 101(12), 2093–2102. https://doi.org/10.1016/j.apmr.2020.05.023
- Scholz, U., Doña, B., Sud, S., & Schwarzer, R. (2002). Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment, 18(3), 242–251. https://doi.org/10.1027//1015-5759.18.3.242
- Schöttke, H., & Giabbiconi, C.-M. (2015). Post-stroke depression and post-stroke anxiety: Prevalence and predictors. International Psychogeriatrics, 27(11), 1805–1812. https://doi.org/10.1017/S1041610215000988
- Snaith, R., & Zigmond, A. (1986). The hospital anxiety and depression scale. British Medical Journal (Clinical Research Ed.), 292, https://doi.org/10.1136/bmj.292.6516.344
- Spinhoven, P., Ormel, J., Sloekers, P., Kempen, G., Speckens, A., & van Hemert, A. (1997). A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine, 27(2), 363–370. https://doi.org/10.1017/s0033291796004382
- Tielemans, N., Schepers, V., Visser-Meily, J., Post, M., & van Heugten, C. (2015). Associations of proactive coping and self-efficacy with psychosocial outcomes in individuals after stroke. Archives of Physical Medicine and Rehabilitation, 96(8), 1484–1491. https://doi.org/10.1016/j.apmr.2015.04.009
- Tielemans, N. S., Visser-Meily, J. M., Schepers, V. P., Post, M. W., & van Heugten, C. M. (2014). Proactive coping poststroke: Psychometric properties of the Utrecht Proactive Coping Competence Scale. Archives of Physical Medicine and Rehabilitation, 95(4), 670–675. https://doi.org/10.1016/j.apmr.2013.11.010
- Twiddy, M., House, A., & Jones, F. (2012). The association between discrepancy in illness representations on distress in stroke patients and carers. Journal of Psychosomatic Research, 72(3), 220–225. https://doi.org/10.1016/j.jpsychores.2011.12.004
- van Mierlo, M. L., van Heugten, C. M., Post, M. W., de Kort, P. L., & Visser-Meily, J. M. (2015). Psychological factors determine depressive symptomatology after stroke. Archives of Physical Medicine and Rehabilitation, 96(6), 1064–1070. https://doi.org/10.1016/j.apmr.2015.01.022
- van Mierlo, M. L., van Heugten, C. M., Post, M. W. M., Lindeman, E., de Kort, P. L. M., & Visser-Meily, J. M. A. (2014). A longitudinal cohort study on quality of life in stroke patients and their partners: Restore4Stroke Cohort. International Journal of Stroke: Official Journal of the International Stroke Society, 9(1), 148–154. https://doi.org/10.1111/j.1747-4949.2012.00882.x
- Visser, M., Heijenbrok-Kal, M., Spijker, A., Oostra, K., Busschbach, J., & Ribbers, G. (2015). Coping, problem solving, depression, and health-related quality of life in patients receiving outpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation, 96(8), 1492–1498. https://doi.org/10.1016/j.apmr.2015.04.007
- Visser-Meily, A., Post, M., Schepers, V., & Lindeman, E. (2005). Spouses’ quality of life 1 year after stroke: Prediction at the start of clinical rehabilitation. Cerebrovascular Diseases, 20(6), 443–448. https://doi.org/10.1159/000088983
- Visser-Meily, A., Post, M., van de Port, I., Maas, C., Forstberg-Warleby, G., & Lindeman, E. (2009). Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke: Course and relations with coping strategies. Stroke, 40(4), 1399–1404. https://doi.org/10.1161/STROKEAHA.108.516682
- Wan-Fei, K., Hassan, S. T. S., Sann, L. M., Ismail, S. I. F., Raman, R. A., & Ibrahim, F. (2017). Depression, anxiety and quality of life in stroke survivors and their family caregivers: A pilot study using an actor/partner interdependence model. Electronic Physician, 9(8), 4924–4933. https://doi.org/10.19082/4924
- Wilz, G., & Kalytta, T. (2008). Anxiety symptoms in spouses of stroke patients. Cerebrovascular Diseases, 25(4), 311–315. https://doi.org/10.1159/000118375
- Wong, J. S., & Hsieh, N. (2019). Functional status, cognition, and social relationships in dyadic perspective. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 74(4), 703–714. https://doi.org/10.1093/geronb/gbx024