 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Cognitive behavioural therapy (CBT) can effectively treat depression in the general population, but there is a lack of studies evaluating CBT tailored to specific cognitive and communication needs of individuals with post-stroke aphasia. We aimed to evaluate the feasibility and preliminary efficacy of a modified CBT intervention to ameliorate depressive symptoms. An ABA withdrawal/reversal single case design with concurrent multiple baselines (2.5, 4.5, or 6.5 weeks) was repeated across 10 participants (six male, four female) with post-stroke aphasia and self-reported depression. Participants completed 10 individual intervention sessions with a clinical neuropsychologist and a 4-week follow-up. The primary outcome was self-rated depression, and secondary outcomes included observer-rated symptoms of depression and anxiety. Data were analysed visually and statistically controlling for baseline trend. Feasibility was addressed by analysing recruitment and retention rates, treatment adaptations, and fidelity ratings. Three participants self-reported decreased depression levels during the intervention phase, which was sustained for two participants. Four additional participants improved during the follow-up phase. Close others reported sustained improvements in depressive symptoms (six participants) and anxiety symptoms (seven participants). Modified CBT appears feasible and potentially efficacious in reducing depressive symptoms in post-stroke aphasia. A randomized controlled trial is warranted, and should consider additional treatment sessions.
Introduction
Depression affects approximately one-third of stroke survivors and is directly associated with reduced health-related quality of life and social functioning (Ayerbe et al., Citation2013; Guajardo et al., Citation2011; Hackett & Pickles, Citation2014; Schmid et al., Citation2012). Caregivers rate symptoms of depression and anxiety, which are highly comorbid, as among the most stress-inducing consequences of stroke (Haley et al., Citation2009; Lincoln et al., Citation2013). While both pharmacological and psychological interventions are used to treat these symptoms, antidepressants may be associated with side effects, especially in the presence of multiple comorbidities and medications (Allida et al., Citation2020; Hackett et al., Citation2005; Paolucci, Citation2008). Evidence suggests that psychological interventions in conjunction with pharmacotherapy may be more effective than either treatment alone (Karyotaki et al., Citation2016; Mitchell et al., Citation2009).
Stroke survivors may be particularly vulnerable to depression due to physical impairments and cognitive dysfunction (Kutlubaev & Hackett, Citation2014), factors which can also impact their ability to engage with psychological intervention. For instance, cognitive limitations may hinder capacity for self-reflection and abstract thought, as required in traditional cognitive behavioural therapy (CBT) (Lincoln & Flannaghan, Citation2003). Furthermore, approximately one-third of stroke survivors experience aphasia, communication difficulties resulting from damage to language networks of the brain (Flowers et al., Citation2016). Post-stroke depression may be more prevalent and severe in people with aphasia (Kauhanen et al., Citation2000; Shehata et al., Citation2015), yet the majority of studies on post-stroke depression have excluded people with aphasia, largely due to a lack of suitable screening tools and the assumption that talk-based interventions cannot be provided to those with impaired communication (Ahrens et al., Citation2022; Townend et al., Citation2007). As a result, there is a notable lack of research investigating interventions that may effectively treat depression in people with aphasia, despite optimizing mental health and wellbeing in this population becoming a top research priority (Ali et al., Citation2022).
There is increasing recognition of the potential to modify traditional psychological interventions to accommodate cognitive and communication impairments (Kneebone, Citation2016; Kootker et al., Citation2015; Rasquin et al., Citation2009). Small-scale feasibility studies indicate that talk-based therapies (e.g., motivational interviewing, solution-focused brief therapy) can be tailored for use in people with aphasia using supported conversation techniques (Holland et al., Citation2018; Northcott et al., Citation2016), and a modified behavioural therapy has been shown to successfully improve mood and self-esteem (S. A. Thomas et al., Citation2013). However, while a systematic review identified psychosocial interventions that may improve mood in people with aphasia without depression or with mild depression, they found no studies for moderate to severe depression (Baker et al., Citation2018).
CBT is an established treatment for depression in the general population (Cuijpers et al., Citation2023) and has been successfully adapted for use in post-stroke depression, showing positive effects in reducing overall symptoms and maintaining improvement (Ahrens et al., Citation2022; Wang et al., Citation2018). Additionally, psychotherapy aimed at treating depression may also alleviate symptoms of anxiety (Weitz et al., Citation2018). CBT’s orientation to the “here and now” and its focus on optimizing skills and problem-solving makes it well-suited for treating the psychological needs and concerns of stroke survivors (Broomfield et al., Citation2011). However, there is a lack of research evaluating the use of CBT tailored to the specific cognitive and communication needs of stroke survivors with aphasia. The aim of this study was to investigate the feasibility and preliminary efficacy of a modified and individually tailored CBT programme in treating depressive symptoms in stroke survivors with aphasia.
Methods
Design
An ABA withdrawal/reversal single-case experimental design using concurrent multiple baselines and a four-week follow-up period was replicated across ten participants. The research design was developed in accordance with the Risk of Bias in N-of-1 Trials (RoBiNT) Scale (Tate et al., Citation2013; Supplementary Material 1). Ethics approvals were obtained from the Monash University Human Research Ethics Committee (MUHREC/7888) and the University of Technology Sydney Human Research Ethics Committee (ETH20-5000). The ADaPT protocol was registered (09/11/2020) with the Australian and New Zealand Clinical Trials Registry (ACTRN12620001174976). Preparation of the manuscript was guided by the Single-Case Reporting guideline in Behavioural interventions (SCRIBE) Statement checklist (Tate et al., Citation2016; Supplementary Material 2).
Participants
Ten stroke survivors with aphasia and depressive symptoms were recruited via community referrals between December 2020 and June 2022 through nationwide advertising to community and stroke support groups, as well as health professional mailing lists. Inclusion criteria were: aged 18 years or older; ischaemic or haemorrhagic stroke; scoring below the cut-off (≤ 93.7; Ross & Wertz, Citation2003) on the Western Aphasia Battery (WAB-R; Kertesz, Citation2006); self-reported low mood (scoring ≥2 on the Depression Intensity Scale Circles (DISCs); Turner-Stokes et al., Citation2005); no previous history or concurrent major neurological or psychiatric diagnosis other than depression and stroke; capacity to provide informed written consent (with assistance) to research participation; capacity and availability to engage with a multi-session therapeutic programme; not concurrently receiving other psychological interventions; and maintaining a stable course of mood medications (i.e., not changing type or dosage) if any. The participants were labelled AA through to JJ to support confidentiality. They did not receive financial compensation, but received treatment free of charge.
Intervention
The CBT intervention followed a manualised treatment programme (S. Thomas, Citation2020). This was developed by a senior clinical neuropsychologist (ST) with over 20 years of experience in the fields of neuropsychological rehabilitation, psychological interventions, and supported communication techniques, in consultation with a team including an experienced clinical psychologist (IK), clinical neuropsychologist (RS), and speech pathologist (BR). Overall, the intervention aimed to reduce depressive symptoms by using behavioural techniques such as activity scheduling and relaxation, as well as cognitive techniques such as challenging automatic negative thoughts and problem-solving. Each session followed a structured approach, which included reviewing homework and experiences from the previous week, setting an agenda and goals for the session, covering session content (outlined in ), and ending with summarizing the session and setting homework tasks. The intervention also incorporated cognitive rehabilitation techniques using individually tailored strategies to increase participation, drawing on key strategies and techniques from previous studies (Kootker et al., Citation2015; S. A. Thomas et al., Citation2013; Wong et al., Citation2018). For instance, utilizing a therapy journal to record/review summaries of each session to assist with memory difficulties, and/or incorporating session plans to provide structure and help participants stay on track.
Table 1. Structure of the treatment protocol.
Where appropriate, close others were engaged to assist in identifying key issues, completing homework tasks, and supporting communication during therapy. Supported Conversation for Adults with Aphasia (SCA; Kagan, Citation1998) techniques were tailored to the type and severity of each participant’s communication impairment. Techniques included encouraging the use of a photo diary, providing written answers or pictorial representations of words, using closed and semi-closed questions, keeping sentences short with plain language, recording key content words, using visual aids, and summarizing content at regular intervals.
Changes in response to the COVID-19 pandemic. Sessions were initially planned to be delivered in person at a private practice in Melbourne, Australia. However, pandemic-related restrictions were introduced as the intervention was initiated for the third and fourth participants. This also interrupted intervention sessions for the first two participants – see details in the Results section below. Rather than suspend the study, the research team decided (with Ethics approval) to offer the intervention over telehealth via a videoconferencing platform. This also allowed us to recruit participants from other Australian states. Eight of the 10 participants had telehealth sessions as part of their intervention, either due to travel barriers or for pandemic-related safety reasons. Therapy tools were consolidated into electronic forms to allow online sharing during and after sessions, via email or cloud storage services. A second camera was used to demonstrate the use of smartphone applications.
Materials
Baseline characteristics. To characterize our sample, at the start of baseline participants were assessed using the EQ-5D-3L and the Assessment for Living with Aphasia (ALA). The EQ-5D-3L contains 3-point ordinal scales assessing subjective quality of life across five domains, and a visual analogue scale assessing self-rated health state (from worst at 0 to best at 100). We used an interview administered version supported by a preliminary pictorial version (Whitehurst et al., Citation2018). The ALA is a pictographic, self-reported assessment of aphasia-related quality of life, with higher scores indicating better quality of life (maximum score 148). A validation study yielded an average score of 135.8 (SD = 20.6) across individuals with mild, moderate, and severe aphasia (Simmons-Mackie et al., Citation2014).
Outcome measures. Participants were asked to complete the DISCs, a 6-point ordinal graphic rating scale which depicts six circles with an increasing proportion of dark shading that represents severity of depression (Turner-Stokes et al., Citation2005). The measure has been demonstrated as sensitive to change and a cut-off score of 2 or higher to have adequate sensitivity and specificity (Turner-Stokes et al., Citation2005). Each close other was asked to complete the Stroke Aphasic Depression Questionnaire – Community 10 (SADQ; Sutcliffe & Lincoln, Citation1998), rating how often (often, sometimes, rarely, never) the participant had exhibited 10 different specific behaviours over the past week. A cut off score of 15 or higher has demonstrated adequate sensitivity and specificity (Leeds et al., Citation2004). Close others were also asked to complete the Behavioural Outcomes of Anxiety (BOA; Kneebone et al., Citation2012), a 10-item questionnaire that has been validated on a group of stroke patients with aphasia and demonstrated adequate sensitivity and specificity, with a cut-off of 17 or higher for significant anxiety (Eccles et al., Citation2017).
Treatment monitoring form. A tool was designed to monitor treatment content (based on components outlined in the manual) and to qualitatively record modifications made to cater to the communication and cognitive profile of each individual (Supplementary Material 3). This was completed by the clinician after each session for all participants.
Treatment fidelity rating form. A pre-existing tool was adapted to specifically assess treatment fidelity in the context of this study (Ymer et al., Citation2021). Treatment fidelity was rated against three parameters: (i) overall adherence to elements common to a CBT approach; (ii) session-specific adherence to treatment manual; and (iii) therapist competency in CBT delivery for a person with aphasia (Supplementary Material 4). Each parameter was rated on a 7-point Likert scale ranging from “unacceptable” to “excellent.”
Procedure
Data was collected between March 2021 and January 2023. Participants were screened in person or via a videoconferencing platform and provided with information about the research project before giving verbal and written consent. Those who met eligibility criteria were randomly allocated to a baseline phase and scheduled for initial baseline assessment. Prior to commencing treatment, participants were paired and randomly assigned to baseline durations of 2.5, 4.5, or 6.5 weeks. Following the baseline phase, participants attended 10 intervention sessions. Upon treatment completion, there was a 4-week follow-up phase. Outcome measures were administered twice per week across all study phases via a text message reminder system to the participant and/or their close other. Responses could be submitted through an online form or via text message, aided by hard copies of measures. Participants with reading and writing difficulties were assisted by their close others in completing outcome measures. Outcome measures were documented by a researcher independent of the therapist. Intervention sessions were delivered by a clinical neuropsychologist (ST), on a weekly basis progressing to fortnightly (individually tailored), with homework undertaken between sessions. ST received monthly peer supervision from clinical neuropsychology colleagues, as mandated by professional registration requirements. Sessions were audio and video recorded to capture verbal and non-verbal communication. At the conclusion of the study, participants were provided with the opportunity to review their case vignettes (as reported in the Results section) for accuracy and to confirm sufficient preservation of anonymity, facilitated by the researcher or their close other.
Data analysis
The primary analysis included both visual and statistical inspection of the outcomes. The raw data record of the outcome measures were graphed using GraphPad Prism 9 (Citation2023) to allow for visual inspection, separately for all ten participants, and separately for the three outcome measures: DISCs (primary outcome), SADQ and BOA (secondary outcomes). Structured visual analyses were conducted within and between phases, in accordance with established guidelines (Lane & Gast, Citation2014), and focus on level (magnitude), trend/slope (progress over time), variability (stability), immediacy of phase effect, and phase overlap. Stability was defined as 80% of data points being within an envelope of 25% of the phase median. To further aid visual inspection, a freely accessible R syntax was utilized to estimate the split-middle trend line of baseline data and project it onto the intervention and follow-up phases as a stability envelope around the trend (Manolov et al., Citation2016; Supplementary Material 5).
Quantitative statistical analysis across phases was conducted using Tau-U, a non-overlap method which is robust in managing small data sets and outliers in data, and can control for effects of trend in the baseline (Parker et al., Citation2011, Citation2014). Planned comparisons between adjacent conditions assessed the efficacy of adapted CBT to treat depressive symptoms in stroke survivors with aphasia. Baseline correction was applied when Tau-U values for baseline exceeded .20 and the trend occurred in the same direction as the aims of the intervention (Vannest & Ninci, Citation2015). With respect to effect size, Tau-U values below .20 were considered small, .20 to .60 medium, .60 to .80 large, and greater than .80 very large (Vannest et al., Citation2018). Analysis was conducted using an online calculator (Vannest et al., Citation2016).
Feasibility. To address the feasibility of conducting a similar study at a larger scale (e.g., randomized controlled trial) and collecting research data from this population, we analysed recruitment and retention rates, as well as participants’ ability to complete outcome measures. To address the feasibility of delivering a modified CBT intervention, adaptation and fidelity were assessed. Other subsets of feasibility, including acceptability and practicality, will be addressed in later publications, using pilot measures and interview data. To assess feasibility of adaptation, the clinician’s qualitative observations on the treatment monitoring form were reviewed. We analysed which aspects of the content were able to be delivered consistently, and unmodified, modified, or not at all (e.g., whether modifications limited the intervention to behavioural components and excluded cognitive components). To assess treatment fidelity, two participants were randomly selected and all 10 of their session recordings evaluated (20% of total intervention sessions) using the treatment fidelity rating form by an independent clinical psychologist with CBT experience and training in SCA and cognitive rehabilitation techniques.
Results
details recruitment and flow of participants over the course of the study period. The ten participants (6 male, 4 female) varied in age (39–74 years), aphasia severity (mild to very severe), and time since stroke (0.4–5 years). The majority completed the treatment via videoconferencing, with only two participants (AA and BB) attending sessions in person. Participant EE withdrew during the treatment phase due to extenuating medical circumstances unrelated to the study that impacted her capacity to attend treatment sessions. All other participants completed the study in its entirety. Participant demographic and baseline characteristics are presented in . No adverse events were recorded for any participant across the duration of the study.
Figure 1. Recruitment and flow of participants throughout the study. Notes: *An attempt was made to balance the range of aphasia severity among participants concurrently receiving intervention to ensure a manageable caseload for the clinician.
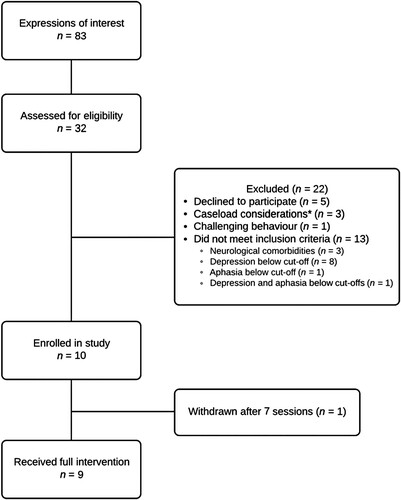
Table 2. Participant demographic and baseline characteristics.
The preliminary efficacy of the intervention was evaluated primarily at the individual level. The results are presented as vignettes for each participant, which consist of their demographic information, case formulation by the treating therapist (including relevant background history and contributing factors to depressive symptoms), and barriers and facilitators to treatment progress based on the therapist’s clinical impressions. Following this, we present their response to the intervention (i.e., self-reported depression levels) and generalization to secondary outcome measures (i.e., close other ratings of observable symptoms of depression and anxiety). provides a summary of each participant’s results across the three outcome measures.
Table 3. Participant outcome summary: interpretation of results.
Participant AA
AA, a 64-year-old separated man, sustained a left MCA ischaemic stroke one year prior to enrolment in the study. Before his stroke, he was employed in a management role and previously participated in performing arts. He did not work after his stroke. As a consequence of stroke, AA experienced hemiparesis in his right upper and lower limbs, requiring use of a wheelchair. He had also developed seizures. AA had very severe Broca’s aphasia. He was living in his own home with his wife periodically present.
AA’s depressive symptoms were precipitated by the impacts of aphasia post-stroke. It was perpetuated by his limited recovery of expressive language and perception of complete dependence on others. He was unable to verbally express his needs or thoughts and felt worthless when relying on others to set-up appointments and activities for him. He was predisposed to depression due to marital separation and obsessive-compulsive personality factors, such as being self-critical and preoccupied with mental and interpersonal control at the expense of flexibility, openness, and efficiency. He also had dominant demand and dichotomous thinking styles. A protective factor was supportive friends. Prior to his stroke, AA had undergone marital counselling with two different psychologists. They noted hoarding behaviour and narcissistic tendencies, but no formal diagnoses were made. AA refused mood medication.
Establishing a way for AA to complete homework was challenging due to the severity of his communication impairment. His wife however did assist with written aspects. Over time, AA became more engaged and made progress in activity scheduling and cognitive restructuring. Unfortunately, pandemic-related restrictions put sessions on hold at a critical juncture when he was beginning to identify unhelpful thoughts. As a result, he had to independently manage for an extended period of time (5 weeks) without having developed cognitive restructuring skills, which increased risk of further rumination. The potential effectiveness of activity scheduling was also reduced due to pandemic-related restrictions on travel and participation in activities. Identifying unhelpful thoughts was challenging because AA was unable to produce words, therefore it took multiple sessions for the therapist to generate approximations that he endorsed, leaving limited sessions for cognitive restructuring.
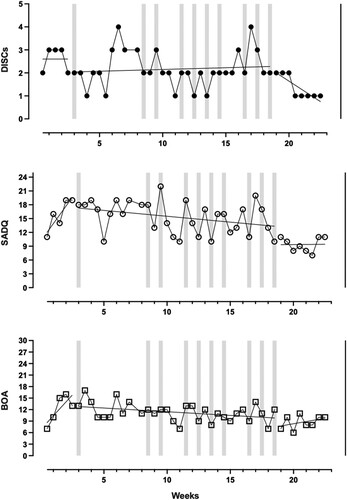
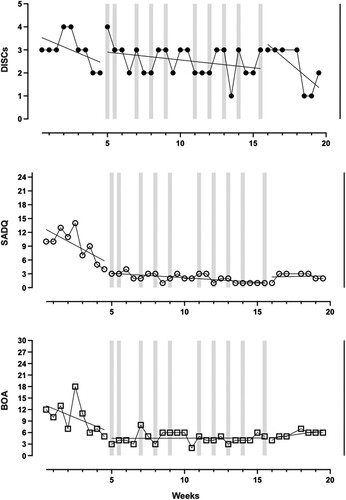
Response to intervention. The application of a stability envelope suggested a stable baseline phase (). With respect to between phase change, the introduction of treatment was associated with a median level improvement in subjective mood rating, which was statistically significant with a medium effect size (see ). While AA showed a slow improving trend following the introduction of the intervention, after the gap in treatment sessions he returned to his baseline level of depression. A deteriorating trend was observed in the follow-up phase.
Figure 2. Participant AA’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
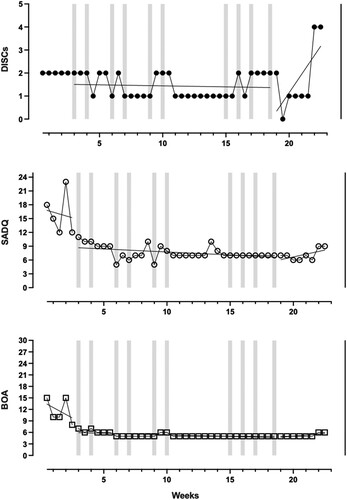
Table 4. Tau-U analyses for subjective depressive symptoms, and depressive and anxiety symptoms as observed by close other.
Generalization measures. AA’s close other (wife) reported decreases in observable symptoms of depression and anxiety following introduction of the treatment. These were statistically significant with very large effect sizes despite the trend towards improvement evident during baseline (see ). While scores on the SADQ and BOA remained low, his wife qualitatively remarked that she perceived significant deterioration in depression during the follow-up phase.
Participant BB
BB, a 64-year-old married man, sustained a left ICA occlusion 5 months prior to enrolment in the study. He had previously worked in construction however he was unemployed following his stroke. He lived at home with his wife and two adult children. As a consequence of stroke, BB had balance problems and some cognitive difficulties, including poor planning and organization. He had mild anomic aphasia. BB struggled to read even simple information, although he self-reported premorbid literacy difficulties.
BB’s depressive symptoms were precipitated by the impacts of aphasia and cognitive impairments post-stroke. It was perpetuated by loneliness and the stress associated with living in a complex family dynamic and with cognitive difficulties (e.g., forgetting appointments). He was predisposed to depression due to longstanding marital difficulties and social isolation. He also had a dominant internal critic and thinking styles that included demand thinking overgeneralizations. Protective factors included a supportive child, independent mobility, and having a driver’s licence. He had completed 12 weeks of fortnightly post-stroke counselling prior to commencing this programme.
BB struggled to understand the concept of cognitive restructuring and to apply it independently, suspected due to cognitive limitations. Pandemic-related restrictions limited the options for activity scheduling outside the home. Participating in pleasant activities, particularly community activities, also required planning and scheduling, which was difficult for BB. While BB was able to engage with and apply techniques during sessions with the therapist’s facilitation, he appeared to lack sufficient support to apply them consistently outside of sessions. This meant he obtained clarity about the triggers for his depressive symptoms without developing the skills to address or modify them. Memory issues were determined to be a barrier to treatment progress, and memory rehabilitation strategies were insufficiently established due to time constraints.
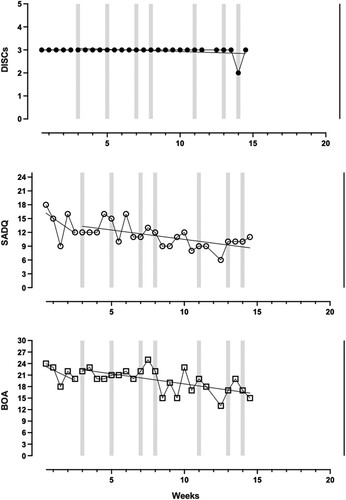
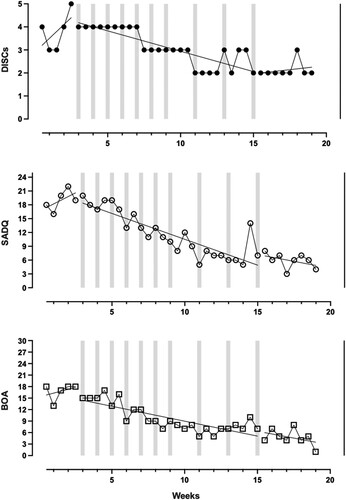
Response to intervention. BB demonstrated a deteriorating trend in subjective depressive symptoms during baseline (). This trend was continued throughout the intervention and follow-up phases, notably exacerbated during and after the gap in treatment sessions. The decline in mood rating from baseline to intervention was statistically significant (see ).
Figure 3. Participant BB’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. BB’s close other (wife) reported a statistically significant deterioration in observable depressive symptoms when the intervention was introduced, which persisted throughout follow-up (see ). However, there was no notable change in observable symptoms of anxiety following treatment introduction, throughout the intervention and follow-up phases.
Participant CC
CC, a 39-year-old single-woman, sustained a left ischaemic stroke two years prior to enrolment in the study. She formerly taught foreign languages at the secondary level and was unemployed following her stroke. At the time of her stroke, she was living outside of Australia and planning to pursue postgraduate studies. As a consequence of stroke, she had hemiparesis in her right lower limb, and spasticity in her right upper and lower limbs. She had mild transcortical motor aphasia. CC lived alone in her own apartment.
CC’s depressive symptoms were precipitated by the impacts of aphasia post-stroke. CC reported experiencing symptoms of anxiety and depression prior to her stroke, which she managed with exercise. However, this coping strategy was no longer viable after her stroke. Her post-stroke depressive symptoms were perpetuated by loneliness and the stress associated with living alone during pandemic-related restrictions, and a sense of inadequacy regarding her communication. She was predisposed to depression due to longstanding migraines and perfectionistic personality traits, most notably expressed in high expectations of herself. Her dominant thinking styles were demand thinking, dichotomous thinking, and negative forecasting. A protective factor was supportive family. CC had previously seen a psychologist 18 months prior to starting intervention, but found it frustrating due to communication barriers. CC was being prescribed a low dose of antidepressants, and was sensitive to its effects (i.e., a higher dose had previously triggered an episode of mania).
CC’s perfectionism and high expectations were noted by the therapist as barriers to treatment progress. While relaxation techniques were beneficial, she would feel guilty when not implementing them. Her family and friends mostly lived far away, which limited her social interactions. She initially struggled with the thought record form because writing was very effortful for her, but this was resolved when she pivoted to using a thought diary mobile application (i.e., Clarity). Towards the end of the intervention, she decided she felt better and ceased taking her antidepressant medication. This was associated with her mood declining significantly during follow-up.
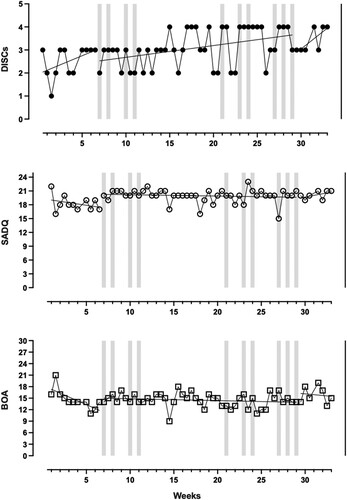
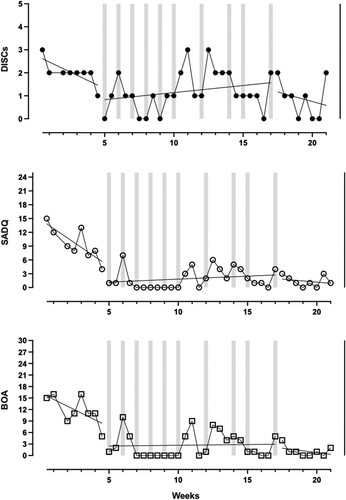
Response to intervention. CC demonstrated a deteriorating trend in subjective mood ratings during the baseline phase, and a slightly improving trend in the therapeutic direction following introduction of the intervention (). However, there was a statistically significant deterioration (large effect size) from intervention to follow up (see ), with a median level decline and a deteriorating trend in the follow-up phase.
Figure 4. Participant CC’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. Upon visual inspection, CC’s close other’s (sister) reports suggested no apparent change in observable symptoms of depression and anxiety following introduction of treatment. However, Tau-U analyses indicated statistically significant improvements with large and very large effect sizes, respectively (see ). CC’s symptoms deteriorated during the follow-up period.
Participant DD
DD, a 59-year-old separated man, sustained a left ischaemic stroke two years prior to enrolment in the study. Before his stroke, he worked in two manual jobs. He stopped working after his stroke. DD spoke English as a second language, with fair proficiency. The main consequence of his stroke was mild anomic aphasia. DD lived alone in a rented house.
DD’s depressive symptoms were precipitated by the impacts of the stroke on his employment and a marital breakdown. They were perpetuated by stress from not being able to access or maintain the family home, and having limited interests. He was predisposed to depression as he had a limited social network and was not close to his family, due to working long hours previously. He also had a longstanding black-and-white thinking style and a dominant negative forecasting thinking style. Protective factors included a strong relationship with a bilingual support worker. DD was not taking any mood medications and had never engaged in psychological intervention.
DD's bilingual support worker attended the sessions with him, which facilitated engagement, as she encouraged his participation when his motivation was low and helped with translation when necessary. Issues with cross-cultural communication and cognitive rigidity presented additional challenges for DD to understand CBT concepts, including the notion of enjoyable activities. For DD, being happy meant working hard, providing for his family, and being with his wife. Activity scheduling was not established due to lockdown restrictions and DD’s fear of contracting COVID-19 in the community. DD struggled to understand the relationship between thoughts and emotions. He could identify his thoughts but had difficulty identifying the most unhelpful or trigger thought for his emotion. Cognitive restructuring was attempted, but DD misperceived it as indicating he should not be thinking about this at all. He was unable to learn cognitive restructuring skills.
Response to intervention. DD’s baseline data, while not meeting stability criteria, showed a flat trend (). While the introduction of treatment was associated with a median level improvement in mood ratings, DD demonstrated a variable and marginally deteriorating trend throughout the intervention phase. However, there was a statistically significant improvement of medium effect size from intervention to follow-up (see ), with a median level improvement and an improving trend in the therapeutic direction during the follow-up phase. This suggests delayed therapeutic gains.
Figure 5. Participant DD’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. DD’s close other (support worker) reports indicated worsening of observable symptoms of depression and anxiety during baseline. Slight improvements were noted across both domains following introduction of treatment, with a notable change in the directions of trends. These therapeutic gains were maintained throughout the follow-up phase, with Tau-U analyses indicating statistically significant improvements of medium and large effect size (see ).
Participant EE
EE, a 74-year-old widowed woman, sustained a left ischaemic stroke with haemorrhagic complications two years prior to enrolment in the study. She lived at home with her daughter’s family. She was a retired administration worker who was actively volunteering in an administrative role prior to her stroke. EE experienced fatigue, vertigo, and memory difficulties as a result of her stroke, and had a number of medical comorbidities that existed pre-stroke. She had moderate Wernicke’s aphasia.
EE’s depressive symptoms were precipitated by pain and aphasia post-stroke. They were perpetuated by the stress of undiagnosed and poorly treated medical issues. She was predisposed to depression due to personality factors, such as high expectations of herself due to perfectionistic traits with a dominant negative forecasting thinking style. Protective factors included supportive family and friends. EE was on antidepressant medication for the period of this study but had not engaged in any psychological intervention beforehand.
Throughout the intervention, EE was observed as very conscientious and determined to put in the work. However, she was often physically unwell, which hindered progress. Her granddaughter was supportive and would assist with homework (e.g., completing thought record forms). The therapist tried to establish progressive muscle relaxation techniques, but EE had difficulty accessing the recording on a cloud storage service. EE was not able to learn cognitive restructuring before intervention had to be ceased after seven sessions due to medical reasons.
Response to intervention. EE’s self-reported mood ratings were stable throughout baseline (). There was no median level change following introduction of the intervention, and EE demonstrated a flat trend throughout. As EE did not complete intervention in full, there was no follow-up data to analyse.
Figure 6. Participant EE’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. Based on EE’s close other (daughter) reports, introduction of treatment did not lead to noticeable improvements in observable symptoms of depression and anxiety. Changes in median level and trend towards the therapeutic direction during the intervention phase were only slight, and did not appear distinct from baseline phase on visual inspection.
Participant FF
FF, a 71-year-old divorced woman, sustained a subdural haematoma one year prior to enrolment in the study. She was a retired healthcare professional, and lived alone in her own home. As a result of stroke, she experienced right-sided weakness and hyperacusis (i.e., increased sensitivity to high pitched noises). She also developed seizures, which were well-controlled on medication. FF had moderate conduction aphasia.
FF’s depressive symptoms were precipitated by the impact of aphasia post-stroke. It was perpetuated by stress from family relationships and the increased difficulty of independently managing her personal affairs. She was predisposed to depression due to personality factors, such as high expectations of herself due to perfectionistic tendencies, and both demand and negative forecasting thinking styles. Protective factors included good friends, financial security, and physical capability. Pre-stroke, FF was prescribed a low dose of antidepressants for anxiety relating to her medical conditions. She stopped taking them post-stroke. She had previously seen a psychologist for 10 sessions.
FF engaged well with therapy. A major stressor, in addition to the stroke itself, was returning to driving and having to complete driving assessments. She found relaxation techniques useful, and activity scheduling enabled her to resume enjoyable activities that she had previously avoided due to lack of confidence in communication (e.g., social lunches, attending concerts and ballets). There were some challenges in engaging with cognitive restructuring homework, due to difficulties with writing and time prioritization. However, FF understood the concept and found it helpful when the therapist demonstrated the technique.
Response to intervention. FF demonstrated improvement in subjective mood ratings during the baseline period (). The introduction of treatment was associated with a statistically significant improvement of large effect size (see ). There was median level improvement and an improving trend in the therapeutic direction throughout the intervention phase. Therapeutic gains were maintained throughout the follow-up period, with Tau-U analyses indicating another statistically significant improvement of medium effect size from intervention to follow-up.
Figure 7. Participant FF’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
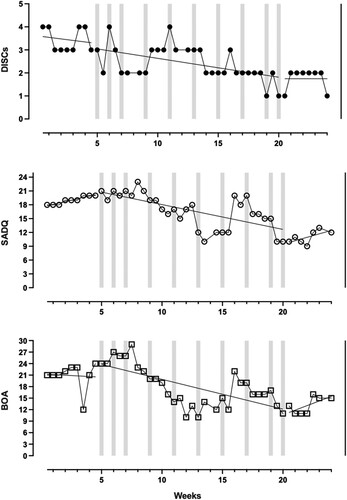
Generalization measures. FF’s close other (daughter) reported improvements in observable symptoms of depression and anxiety following introduction of treatment. There were improving trends in the therapeutic direction during the intervention phase. Therapeutic gains were maintained throughout the follow-up period, and Tau-U analyses indicated statistically significant improvements from intervention to follow-up, with large and medium effect sizes (see ).
Participant GG
GG, a 58-year-old married man, sustained a left ICA dissection with haemorrhagic transformation three years prior to enrolment in the study. He was working as a sales manager and ceased working after his stroke. As a consequence of stroke, he experienced hemiparesis in his right arm, weakness in his right leg, tics on the right side of his body, balance issues, and swallowing difficulties. He developed impulsiveness and cognitive rigidity, which resulted in a tendency to lose his temper quickly. GG had severe Wernicke’s aphasia. He lived at home with his wife and two adult children.
GG’s depressive symptoms were precipitated by the impacts of aphasia post-stroke. After his stroke, GG reportedly experienced anxiety attacks in crowded areas, but this improved over time. His post-stroke depressive symptoms were perpetuated by stress associated with his child’s mental health issues and his wife’s neurological condition, and the loss of agency from his severe communication difficulties. GG’s irritable bowel syndrome also caused him frustration and anger. He was predisposed to depression due to personality factors, such as high expectations of himself and a dominant demand thinking style. Protective factors included a supportive family and financial security. GG had no prior experience with psychological intervention. He was taking antidepressant medication for the duration of the study.
With regards to the intervention, GG’s expressive language difficulties posed a challenge, but his wife was present for most sessions to support conversation. GG struggled to read even simple language, which made it difficult for him to review therapy content between sessions. Activity scheduling was implemented, with support from his wife. He was able to engage in some cognitive restructuring, but not independently. Due to the severity of his language impairment GG struggled to dispute his own thoughts and required modelling and facilitation from the therapist in doing this.
Response to intervention. There were improvements in GG’s subjective mood ratings throughout the baseline period (). A deteriorating trend was observed throughout the intervention phase. However, there was an improving trend in the therapeutic direction during the follow-up phase, accompanied by a median level improvement, which was suggestive of delayed onset of therapeutic gains.
Figure 8. Participant GG’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. Visual inspection of GG’s close other’s (wife) reports suggested a slight improvement in observable depressive symptoms following introduction of treatment, and Tau-U analyses indicated statistical significance with a large effect size (see ). Therapeutic gains were maintained throughout intervention and follow-up, with a further statistically significant improvement of very large effect size from intervention to follow-up. On the other hand, there was no change in observable anxiety symptoms throughout the intervention and follow-up phases.
Participant HH
HH, a 70-year-old married man, sustained a left MCA ischaemic stroke one year prior to enrolment in the study. He formerly worked in animal care, and was working in the criminal justice system with no plans to retire. Following his stroke, HH took sick leave and subsequently stopped working. HH was fluent in two languages including English. He lived at home with his wife. The stroke resulted in weakness in his right leg and hand, which impacted his fine motor skills. He had mild anomic aphasia. HH appeared to also have difficulties with memory, planning and organization.
HH’s depressive symptoms were precipitated by the impacts of aphasia post-stroke. It was perpetuated by stress associated with marital strain, cognitive impairment, and a sense of inadequacy. He was predisposed to depression due to personality factors, such as high expectations of himself and both dichotomous and negative forecasting thinking styles. HH had low mood prior to his stroke. Protective factors included a supportive family, financial security, and physical capability. HH was prescribed antidepressants throughout the duration of this study but had had no prior experience with psychological interventions.
Although HH was very engaged and had a good working relationship with the therapist, he had difficulties getting his message across, which slowed progress. HH was an active person and responded well to activity scheduling, but had difficulties completing the thought record homework, possibly due to memory and/or writing difficulties. While HH would have benefitted from cognitive rehabilitation for memory and planning, there was limited time to cover this in ten sessions.
Response to intervention. There were substantial improvements in HH’s subjective depression ratings throughout baseline (), which was corrected for in the statistical analysis. Following introduction of the intervention, there was no noticeable change during the intervention phase. However, a slight improving trend was observed during the follow-up phase, suggesting a delayed onset of therapeutic gains.
Figure 9. Participant HH’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. HH’s close other (wife) also reported improving trends throughout baseline, for observable symptoms of depression and anxiety. Despite this, introduction of treatment was associated with statistically significant improvements of very large and large effect sizes for depressive and anxiety symptoms respectively (see ), and median level improvements. This could be attributed to the consistency of low depression and anxiety ratings, which distinguished the intervention phase from the baseline phase. Therapeutic gains were maintained throughout the follow-up period.
Participant II
II, a 46-year-old married man, sustained a left MCA ischaemic stroke two years prior to enrolment in the study. At that time, he was working in aviation and legal services. After his stroke, he moved to Australia from overseas and lived at home with his wife and two young children. II was physically fit, but experienced some cognitive changes including slowed processing speed and poor divided attention. He had moderate Wernicke’s aphasia, including difficulty with numbers.
II’s depressive symptoms were precipitated by the impact of aphasia post-stroke. It was perpetuated by stress, as a result of full-time parenting two young children, and the isolation of being unable to effectively express himself. He was predisposed to depression due to his high expectations of recovery given the time since stroke, and moving away from his friends and family. He also had a tendency to overgeneralize and had dichotomous and demand thinking styles. Protective factors included a supportive wife, financial security, and physical capability.
Prior to his stroke, II had a history of post-traumatic stress disorder following military postings. He also experienced depression after the breakdown of his first marriage some time prior to his stroke. He had had no psychological treatment pre-stroke. After his stroke, he completed six sessions of psychotherapy over six months in his home country. He was prescribed antidepressants throughout the duration of this study.
II was able to schedule physical and social activities, adding to these throughout the intervention. He was also able to fundamentally understand how modifying his thoughts could change his emotions. His wife assisted him initially to record unhelpful thoughts in a thought record. He was then able to independently use the thought record and develop short phrases to restructure unhelpful thoughts between sessions. The therapist was also able to organize an education session with his wife to facilitate her understanding of his recovery, his perspective regarding their swapped roles (i.e., breadwinner versus childcare duties), and how she could support his CBT journey.
Response to intervention. II’s self-reported mood ratings were stable throughout baseline (). There was median level improvement from baseline to intervention, with an improving trend in the therapeutic direction throughout the intervention phase. Therapeutic gains were maintained, with Tau-U indicating a statistically significant improvement of large effect size from intervention to follow-up (see ), also reflected in median level improvement between the two phases.
Figure 10. Participant II’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. Visual inspection of II’s close other’s (wife) reports suggested continuous improving trends in observable symptoms of depression and anxiety throughout intervention and follow-up, with statistically significant improvements of very large effect sizes from baseline phase to intervention phase (see ). Therapeutic gains were maintained throughout the follow-up period, and Tau-U analyses indicated further statistically significant improvements of large and very large effect sizes.
Participant JJ
JJ, a 69-year-old left-handed married woman, sustained a left haemorrhagic stroke five years prior to enrolment in the study. She was a retired mental health professional and lived at home with her husband. She initially suffered from right-sided facial paresis and hemiplegia (for two weeks), but by the time she started intervention she had recovered physically, apart for intermittent challenges from fatigue. She acquired mild anomic aphasia as a result of stroke and had difficulties with numbers and mathematics. JJ also reported struggling to concentrate when multiple conversations were co-occurring and having lost the ability to touch-type.
JJ’s most recent depressive episode was precipitated by aphasia post-stroke. JJ has had depressive episodes for most of her life, including postnatal depression. She had taken antidepressant medication intermittently throughout her life and was on a consistent dose for the duration of this study. Her post-stroke depressive symptoms were perpetuated by avoidance of situations that challenged her communication and a sense of disempowerment due to her communication difficulties. She was predisposed to depression due to her low self-esteem and sense of inadequacy. She also had a dominant internal critic and a demand thinking style. Protective factors included a supportive husband, family and friends, as well as financial security and physical capability. JJ had seen a psychologist post-stroke and completed 10 sessions of Acceptance and Commitment Therapy four years prior to commencing our programme. In the year prior to her enrolment, she had also participated in a co-design study of a behavioural activation intervention for people with aphasia.
Identifying unhelpful thoughts was a confronting process to JJ, as she had held them for most of her life. Facilitators to treatment progress were that JJ was highly psychologically minded and had prior experience with behavioural activation, which the therapist could expand on. JJ had many interests, and activity scheduling worked very well for her. JJ received a lot of social support from her family and small-town community. A barrier to progress was that JJ struggled with being assertive with her husband, who tended to not give her the time she needed in conversation.
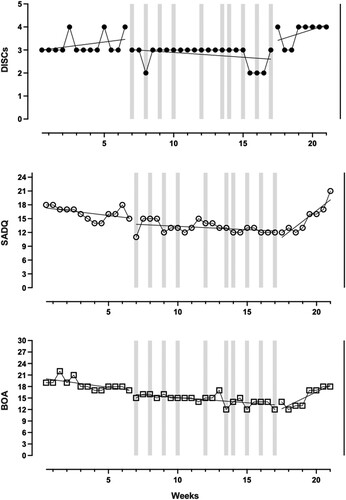
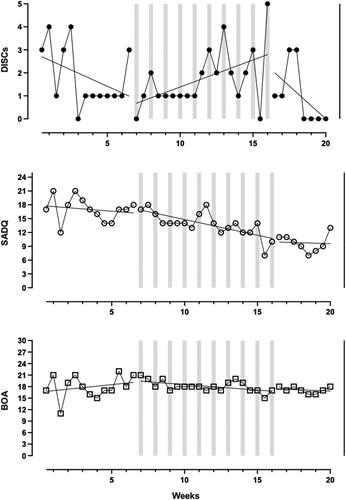
Response to intervention. There were substantial improvements in JJ’s subjective depression ratings throughout baseline (), which were corrected for in the statistical analysis. Based on visual inspection, JJ demonstrated a variable and marginally deteriorating trend throughout the intervention phase. Despite the statistically significant improvement of medium effect size indicated by Tau-U analyses (see ), visually there was no noticeable overall change throughout the intervention period. However, JJ showed a slight improving trend in the therapeutic direction during the follow-up phase, suggestive of delayed onset of therapeutic gains.
Figure 11. Participant JJ’s self-reported depression levels (DISCs) and observer-rated symptoms of depression (SADQ) and anxiety (BOA) across baseline, intervention, and follow-up phases. DISCs: Depression Intensity Scale Circles; SADQ: Stroke Aphasic Depression Questionnaire; BOA: Behavioural Outcomes of Anxiety. Notes: Higher scores denote worse depressive/anxiety symptoms. Dotted lines demarcate the different phases; grey shadings indicate treatment sessions; trend lines calculated using ordinary least squares estimation are superimposed on the raw data.
Generalization measures. Based on JJ’s close other (husband) reports, introduction of treatment was associated with median level improvements in observable symptoms of depression and anxiety, which were statistically significant with very large effect sizes (see ). Therapeutic gains were maintained throughout the intervention and follow-up phases.
Feasibility
It took 20 months to achieve our recruitment target, with the first 9 months limited to those residing in Melbourne, Australia. A total of 83 expressions of interest were received, of which 32 were appropriate referrals and screened for eligibility. lists reasons for exclusion, including 5 individuals declining participation and 9 individuals not meeting the depressed mood criteria based on DISCs scores. Most potential participants were referred by their clinicians (e.g., speech pathologist, clinical neuropsychologist) who learned about the study from advertisements on mailing lists (e.g., Neuropsychology in Australia (NPinOz), Brain Impairment Clinician and Researcher Peer Network (BRAINSPaN)) or community groups (e.g., Centre for Research Excellence in Aphasia). Some people referred themselves or their family members after seeing an advertisement on community groups (e.g., Stroke Foundation’s EnableMe website, Australia Aphasia Association). Nine out of the 10 participants completed all 10 intervention sessions, and one withdrew after 7 sessions due to medical reasons. All participants were able to complete all outcome measures, although those who had difficulties with written communication needed assistance from their close others.
Adaptation. The most and least frequently implemented CBT components (as outlined in the treatment manual) were quantified based on the therapist’s self-report using the treatment monitoring form (Supplementary Material 3). summarizes this information, along with the most frequently used supported conversation techniques. Raw data can be found in Supplementary Material 6. The results indicated that core CBT techniques, such as thought modification and activity scheduling, were implemented most frequently. Homework was regularly assigned and reviewed. Treatment components that were only relevant to certain participants, such as assessing energy levels and relaxation techniques, were less frequently utilized. The discussion of core beliefs and values, as well as cognitive rehabilitation techniques, were also identified as less frequently implemented. Nevertheless, it should be noted that cognitive rehabilitation was integrated throughout the treatment protocol, suggesting that its implementation may have been implicit rather than explicit. Supported conversation techniques commonly employed included the use of support materials such as visual aids, slowing down the pace of the conversation, simplifying language, and employing repetition to enhance understanding.
Table 5. Intervention elements and supported conversation techniques: frequency analysis.
Additional qualitative observations detailed on the treatment monitoring forms across all participants and sessions revealed a range of therapy adaptations were employed to deliver the intervention, with some techniques more feasible to implement than others. Visual aids were extensively utilized to educate participants on the foundations of CBT and to facilitate the implementation of CBT techniques, including to illustrate how thoughts can influence feelings, present an emotion list, and demonstrate potential enjoyable activities. For participants who struggled to express unhelpful thoughts due to communication limitations, the therapist generated possible unhelpful thoughts for the participants to endorse. Simplified resources were used, such as a 3-column form for thought modification comprising “unhelpful thought,” “question to modify thought,” and “modified thought.” While thought modification could be successfully demonstrated during sessions, some participants struggled and needed more time to acquire the skill and implement it independently. Activity scheduling was attempted with all participants, but some struggled with identifying enjoyable activities or planning and executing them. The therapist provided scaffolding by arranging prompts (e.g., daily notification asking what positive thing happened today) and making specific suggestions (e.g., asking participant to identify parks/gardens where they could go for a walk). Homework was consistently assigned, but not always completed by participants, sometimes due to difficulties with writing or cognition. Some modifications included using smartphone applications or cutting and pasting pictures. Close others were often involved to provide background information during sessions and to assist with homework. However, this was not always feasible or appropriate. Cognitive rehabilitation strategies were not addressed as a standalone component, but integrated into the CBT intervention, such as by sending written summaries and reminders via email to support memory. Though therapeutically indicated, discussion of core beliefs and values was often not feasible due to communication limitations and time restrictions (i.e., 10 sessions).
Fidelity. Independent fidelity assessment of treatment delivery on a sample of 20 sessions across two participants indicated “acceptable” to “excellent” ratings. The average rating score for overall delivery (from 0-“unacceptable” to 6-“excellent”) was 5.5 (SD = 0.61; range, 4–6). For session adherence it was 4.55 (SD = 0.89; range, 3–6), and for competency it was 4.75 (SD = 0.79; range, 3–6). We note that the recording of the final portion (10 min) of one session was missing, therefore the rating for that session was guided by a discussion with the therapist to identify session content, with supporting documents provided.
Discussion
The purpose of this study was to investigate the feasibility and preliminary efficacy of a modified CBT programme for treating depressive symptoms in individuals with post-stroke aphasia. Overall, the intervention appeared to be largely feasible and could be implemented with most participants across varying degrees of aphasia severity and time since stroke. Three participants reported improvement in mood during the intervention period and an additional four participants exhibited a delayed treatment response. Three participants did not appear to benefit throughout the study period, one of whom did not complete the intervention in its entirety.
Fidelity ratings indicated that overall, the intervention programme was delivered with adequate treatment adherence, suggesting the feasibility of implementing CBT for stroke survivors with different levels and types of aphasia, provided that appropriate modifications are made. Successful and consistent delivery was observed for various components of the intervention, including activity scheduling and thought modification. Our study is among the few to assess treatment adherence and confirm the feasibility of modified CBT for individuals with acquired brain injury (Gallagher et al., Citation2019). However, treatment monitoring also highlighted that some intervention components were less consistently applied. Non-core components of CBT, such as relaxation techniques and general rehabilitation techniques, were not consistently covered, particularly for participants with significant communication and cognitive limitations where extra time is required to effectively work through the intervention content. Given the maximum number of ten sessions available within the intervention protocol, it appears that the therapist prioritized delivering core CBT techniques over other components. This aligns with previous research suggesting that individuals with complex mental health needs may benefit from additional sessions (Pirkis et al., Citation2022). It is suggested that future iterations of this intervention allow flexibility with regards to number of treatment sessions based on client need. Despite significant intervention modifications and supported conversation techniques, certain aspects of the intervention, such as discussions of core beliefs and values, were challenging to deliver to participants with more severe aphasia and, therefore, were not consistently delivered. Finally, certain components of the intervention, such as addressing energy levels and fatigue, were not consistently delivered as they were not identified as issues for some clients.
With regards to treatment efficacy, the treatment response rate in this study, although based on a different methodological design, aligns with previous findings. Studies comparing CBT against control groups, pharmacotherapy, and other psychotherapies to treat depression in the general adult population typically report a number needed to treat ranging between 2.60–5 (Cuijpers et al., Citation2023; Guidi et al., Citation2016). Number needed to treat is a metric used to quantify the number of patients who would need to undergo CBT instead of a comparison intervention to generate one additional positive outcome. These findings suggest that not all participants can be expected to respond positively to treatment, even in standard practice. Our preliminary findings are also consistent with emerging research demonstrating the efficacy of CBT in individuals with acquired brain injury, including stroke, particularly when the intervention is adapted to address cognitive limitations (Ahrens et al., Citation2022; Gallagher et al., Citation2019). Additionally, our results suggest that this modified intervention could also ameliorate anxiety symptoms. This is consistent with previous research suggesting that psychotherapy targeting depression may also reduce anxiety symptoms (Weitz et al., Citation2018), and indicates further promise in the treatment of mood disorders in those with post-stroke aphasia.
This study highlighted a number of potential facilitators and barriers to treatment response, in light of the observed variations across participants, which may guide further refinement of the intervention. With regards to facilitators, at least four participants (AA, EE, GG, II) were assisted by close others in completing homework. Carer and family involvement has been shown to facilitate of implementation of treatment strategies and has previously been recommended for inclusion in modified CBT for individuals with cognitive impairment due to brain injury (Gallagher et al., Citation2019; Tate et al., Citation2020). Further, a range of mobile applications (e.g., Clarity Thought Diary) were successfully used in the current intervention, particularly in the context of scaffolding homework completion. This is consistent with previous research suggesting the use of smartphones to boost independence in people with acquired brain injury (Wong et al., Citation2017). Further development in this area may lead to assistive technology that specifically enhances CBT implementation, incorporating features such as personalized feedback to engage and motivate users (Tang & Kreindler, Citation2017). With regards to barriers, implementation and generalization of strategies acquired during therapy sessions, facilitated by homework completion, were impacted by external and internal factors. For instance, pandemic-related lockdowns limited opportunities for activity participation, particularly for the first four participants (AA, BB, CC, DD), who overall showed less benefit from the intervention. Further, cognitive impairments presented as challenges to the execution of activity scheduling and thought modification (Taylor et al., Citation2011). This was particularly apparent for participants BB, GG, and HH.
Due to pandemic-related restrictions, the intervention had to transition to telehealth delivery, necessitating further adaptations. Therapy tools were digitized and shared with participants during and after sessions via email or cloud storage services. Existing studies support the effectiveness of telehealth delivery of CBT in treating depressive and anxiety disorders (Bashshur et al., Citation2016). Our results suggest the applicability of this approach to individuals with post-stroke aphasia, with tailored support. This provides an alternative for individuals who are unable to attend in-person sessions. It is important to recognize, however, that when designing telehealth interventions for individuals with aphasia, it is beneficial to perform a formal task analysis to ensure that the technology chosen to deliver the intervention matches the remote needs of users and clinicians (e.g., video and audio features, communication options) (Pitt et al., Citation2019). Our study lacked this structured process due to the rapid translation required during the COVID-19 pandemic. Future development of telehealth interventions for people with aphasia should consider this aspect in their design. It is also important to recognize that while receptivity towards telehealth may have increased following the COVID-19 pandemic (Bunnell et al., Citation2020; Tse et al., Citation2021), this shift is not universal. Reluctance towards telehealth can arise from the clinician or the client (McClellan et al., Citation2020; Swinton et al., Citation2009). It may be beneficial to promote the option of establishing initial rapport through face-to-face appointments prior to transitioning to telehealth (Swinton et al., Citation2009).
An interesting and unexpected observation within this study was that close others tended to report reductions in participants’ symptoms of depression more often than the participants themselves. This occurred in five cases during the intervention period, and the underlying reason remains unclear. It is possible that close others observed increased engagement in activities or that an expectancy effect influenced their perceptions. Further investigation is necessary to gain a deeper understanding of this phenomenon. Previous studies have frequently noted discrepancies between self-report measures and proxy ratings of mood, mental health, and quality of life (Ashaie & Cherney, Citation2021; Kozlowski et al., Citation2015; Lapin et al., Citation2021; Rand & Caiels, Citation2015). Rating agreement may be influenced by the nature and closeness of the relationship between the proxy and the individual, with higher agreement observed when the individual has more severe depression and the proxy experiences lower caregiving burden (Rand & Caiels, Citation2015; Williams et al., Citation2006). Additionally, in our study, some close others were present during therapy sessions, which could have influenced their ratings. Both perspectives remain valuable, as mood symptoms affect not only the individual but also their close others (Dou et al., Citation2018; Lincoln et al., Citation2013). Close others may also provide important insight into changes in the participant’s mood and behaviour that the participants themselves may miss.
In addressing research feasibility, we note that recruitment and treatment delivery for this study were conducted during the COVID-19 pandemic. Clinicians and community groups were major avenues for recruitment, and our rate of recruitment was affected by limited access to health services for non-COVID-19 and non-acute conditions, as well as suspension of community groups (Harper et al., Citation2020; Rosenbaum, Citation2020). Nonetheless, this study revealed challenges in recruiting participants who met the rigorous inclusion criteria. We excluded many potential participants with neurological and psychiatric comorbidities (e.g., cerebral vasculitis, cerebral amyloid angiopathy, chronic substance use, history of epilepsy and traumatic brain injury), which are commonly experienced by stroke survivors (Nuyen et al., Citation2006). Further, some individuals referred by family members or clinicians did not meet the threshold for depressed mood upon screening. While it is possible that some individuals may lack awareness or insight into their own mood problems (Rose et al., Citation2023), in some cases, scores provided by close others also did not indicate depression. Upon questioning, these individuals appeared to experience more general psychological distress and adjustment issues as opposed to a specific depressive disorder (White et al., Citation2012). Additionally, some prospective participants were reluctant to engage in psychological treatment, aligning with previous research suggesting the tendency to prioritize addressing physical impairments especially during the early stages of stroke recovery (Baker et al., Citation2021; Ryan et al., Citation2019). Future research should explore alternative approaches to address the wide range of mental health challenges after stroke, beyond the conventional focus on mood disorders. Including a range of mental health presentations within studies of psychological therapies and exploring the efficacy of informal supports such as stroke-support groups and self-management techniques are promising future research directions (Kotov et al., Citation2022; Tjokrowijoto et al., Citation2023). Despite challenges with recruitment, the study demonstrated high rates of retention and outcome measure completion, albeit with some participants requiring assistance from close others. This underscores the feasibility of conducting future research with a similar protocol.
This study achieved good methodological rigour, scoring 22/30 on the RoBiNT critical appraisal scale (Supplementary Material 1). While external validity was a strength (15/16), internal validity (7/14) could have been improved with an additional tier on the multiple baseline design. However, blinding of participants and therapist was not possible due to the nature of the intervention, and blinding of assessors and use of interrater agreement were not possible due to utilization of self-report outcomes. Assessing baseline stability for self-rated depression was challenging due to the nature of a 6-point scale, where even minor fluctuations would be deemed unstable within the 80% stability envelope. Consequently, it is necessary to identify alternative primary outcome measures that provide a broader range of scores, with good sensitivity to change. This study lacked diagnostic certainty regarding participants’ mood problems – no structured diagnostic interviews were conducted and the intervention targeted depression and anxiety at the symptom level. As most of our participants came from high functioning backgrounds in terms of education and employment, future studies may benefit from recruiting a more diverse sample to investigate this impact on treatment response. Finally, it is important to acknowledge that this study employed a single-case design with a limited sample size of 10 participants, signifying the need for larger-scale research (i.e., a Phase II randomized controlled trial) to further validate these findings and enhance their generalisability.
Assuming future studies support these preliminary findings, it is suggested a modified CBT programme could potentially provide a basis for interventions that cater to individuals who are currently often excluded from treatment access. Future studies could investigate the optimal duration and frequency of this intervention, as well as the potential further integration of cognitive rehabilitation techniques for those requiring more intensive support due to cognitive impairments. Utilizing longer follow-up periods may offer insights into the maintenance of treatment effects. Challenges encountered during recruitment suggest the potential value of incorporating psychoeducation or motivational interviewing to enhance participant engagement in clinical practice. It is also essential to investigate client acceptability of this modified CBT intervention. To accomplish this, semi-structured interviews were conducted by an independent researcher, exploring the experience of stroke survivors who participated in this programme. These results will be reported in subsequent publications. Additionally, future studies may wish to explore the experience of close others.
This study addresses a gap in existing research by being among the first to develop and evaluate a tailored CBT intervention for individuals with post-stroke aphasia. The findings underscore the complexity of treating mood symptoms in this population and identify potential facilitators of treatment response. It also highlights challenges in implementation and suggested modifications. Our results underscore the importance of tailoring the intervention to individual circumstances. Different adaptations were suitable for different individuals, and allowed for independent participation in therapy. Close others can be involved in various capacities, depending on individualized therapy content and clinical need. Despite the obstacles encountered, this study demonstrates good feasibility and preliminary efficacy in improving mood in people with post-stroke aphasia and depression, which will help inform and guide future research and clinical practice in this field.
Supplementary Materials.docx
Download MS Word (1.1 MB)Supplementary Material 6.xlsx
Download MS Excel (21.9 KB)Acknowledgements
We acknowledge the contributions of Dr Caroline Baker in administering the WAB-R for participant screening and Elizabeth Walters in evaluating treatment adherence.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahrens, J., Shao, R., Blackport, D., Macaluso, S., Viana, R., Teasell, R., & Mehta, S. (2022). Cognitive-behavioral therapy for managing depressive and anxiety symptoms after stroke: A systematic review and meta-analysis. Topics in Stroke Rehabilitation, 30(4), 368–383. https://doi.org/10.1080/10749357.2022.2049505
- Ali, M., Soroli, E., Jesus, L. M. T., Cruice, M., Isaksen, J., Visch-Brink, E., Grohmann, K. K., Jagoe, C., Kukkonen, T., Varlokosta, S., Hernandez-Sacristan, C., Rosell-Clari, V., Palmer, R., Martinez-Ferreiro, S., Godecke, E., Wallace, S. J., McMenamin, R., Copland, D., Breitenstein, C., … Brady, M. C. (2022). An aphasia research agenda – A consensus statement from the collaboration of aphasia trialists. Aphasiology, 36(4), 555–574. https://doi.org/10.1080/02687038.2021.1957081
- Allida, S., Cox, K. L., Hsieh, C. F., Lang, H., House, A., & Hackett, M. L. (2020). Pharmacological, psychological, and non-invasive brain stimulation interventions for treating depression after stroke. Cochrane Database of Systematic Reviews, 1(1), CD003437. https://doi.org/10.1002/14651858.CD003437.pub4
- Ashaie, S. A., & Cherney, L. R. (2021). Internal consistency and convergent validity of self-report and by-proxy measures of depression in persons with aphasia. Journal of Speech, Language, and Hearing Research, 64(6), 2047–2052. https://doi.org/10.1044/2021_JSLHR-20-00621
- Ayerbe, L., Ayis, S., Wolfe, C. D. A., & Rudd, A. G. (2013). Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. British Journal of Psychiatry, 202(1), 14–21. https://doi.org/10.1192/bjp.bp.111.107664
- Baker, C., Worrall, L., Rose, M., Hudson, K., Ryan, B., & O’Byrne, L. (2018). A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia. Disability and Rehabilitation, 40(16), 1870–1892. https://doi.org/10.1080/09638288.2017.1315181
- Baker, C., Worrall, L., Rose, M., & Ryan, B. (2021). Stroke health professionals’ management of depression after post-stroke aphasia: A qualitative study. Disability and Rehabilitation, 43(2), 217–228. https://doi.org/10.1080/09638288.2019.1621394
- Bashshur, R. L., Shannon, G. W., Bashshur, N., & Yellowlees, P. M. (2016). The empirical evidence for telemedicine interventions in mental disorders. Telemedicine and e-Health, 22(2), 87–113. https://doi.org/10.1089/tmj.2015.0206
- Broomfield, N., Laidlaw, K., Hickabottom, E., Murray, M., Pendrey, R., Whittick, J., & Gillespie, D. (2011). Post-stroke depression: The case for augmented, individually tailored cognitive behavioural therapy. Clinical Psychology & Psychotherapy, 18(3), 202. https://doi.org/10.1002/cpp.711
- Bunnell, B. E., Barrera, J. F., Paige, S. R., Turner, D., & Welch, B. M. (2020). Acceptability of telemedicine features to promote its uptake in practice: A survey of community telemental health providers. International Journal of Environmental Research and Public Health, 17(22), Article 22. https://doi.org/10.3390/ijerph17228525
- Cuijpers, P., Miguel, C., Harrer, M., Plessen, C. Y., Ciharova, M., Ebert, D., & Karyotaki, E. (2023). Cognitive behavior therapy vs. control conditions, other psychotherapies, pharmacotherapies and combined treatment for depression: A comprehensive meta-analysis including 409 trials with 52,702 patients. World Psychiatry, 22(1), 105–115. https://doi.org/10.1002/wps.21069
- Dou, D.-M., Huang, L.-L., Dou, J., Wang, X.-X., & Wang, P.-X. (2018). Post-stroke depression as a predictor of caregivers burden of acute ischemic stroke patients in China. Psychology, Health & Medicine, 23(5), 541–547. https://doi.org/10.1080/13548506.2017.1371778
- Eccles, A., Morris, R., & Kneebone, I. (2017). Psychometric properties of the Behavioural Outcomes of Anxiety questionnaire in stroke patients with aphasia. Clinical Rehabilitation, 31(3), 369–378. https://doi.org/10.1177/0269215516644311
- Flowers, H. L., Skoretz, S. A., Silver, F. L., Rochon, E., Fang, J., Flamand-Roze, C., & Martino, R. (2016). Poststroke aphasia frequency, recovery, and outcomes: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation, 97(12), 2188–2201.e8. https://doi.org/10.1016/j.apmr.2016.03.006
- Gallagher, M., McLeod, H. J., & McMillan, T. M. (2019). A systematic review of recommended modifications of CBT for people with cognitive impairments following brain injury. Neuropsychological Rehabilitation, 29(1), 1–21. https://doi.org/10.1080/09602011.2016.1258367
- GraphPad Software, L. L. C. (2023). GraphPad Prism 9 [Computer software].
- Guajardo, V. D., Souza, B. P., Henriques, S. G., Lucia, M. C., Menezes, P. R., Martins, M. A., Tardivo, L. S., Gattaz, W. F., & Fráguas, R. (2011). Loss of interest, depressed mood and impact on the quality of life: Cross-sectional survey. BMC Public Health, 11(1), 826. https://doi.org/10.1186/1471-2458-11-826
- Guidi, J., Tomba, E., & Fava, G. A. (2016). The sequential integration of pharmacotherapy and psychotherapy in the treatment of major depressive disorder: A meta-analysis of the sequential model and a critical review of the literature. American Journal of Psychiatry, 173(2), 128–137. https://doi.org/10.1176/appi.ajp.2015.15040476
- Hackett, M. L., Anderson, C. S., & House, O. A. (2005). Management of depression after stroke: A systematic review of pharmacological therapies. Stroke, 36(5), 1092–1097. https://doi.org/10.1161/01.STR.0000162391.27991.9d
- Hackett, M. L., & Pickles, K. (2014). Part I: Frequency of depression after stroke: An updated systematic review and meta-analysis of observational studies. International Journal of Stroke, 9(8), 1017–1025. https://doi.org/10.1111/ijs.12357
- Haley, W. E., Allen, J. Y., Grant, J. S., Clay, O. J., Perkins, M., & Roth, D. L. (2009). Problems and benefits reported by stroke family caregivers. Stroke, 40(6), 2129–2133. https://doi.org/10.1161/STROKEAHA.108.545269
- Harper, L., Kalfa, N., Beckers, G. M. A., Kaefer, M., Nieuwhof-Leppink, A. J., Fossum, M., Herbst, K. W., & Bagli, D. (2020). The impact of COVID-19 on research. Journal of Pediatric Urology, 16(5), 715–716. https://doi.org/10.1016/j.jpurol.2020.07.002
- Holland, E.-J., Watkins, C. L., Boaden, E., & Lightbody, C. E. (2018). Fidelity to a motivational interviewing intervention for those with post-stroke aphasia: A small-scale feasibility study. Topics in Stroke Rehabilitation, 25(1), 54–60. https://doi.org/10.1080/10749357.2017.1376916
- Kagan, A. (1998). Supported conversation for adults with aphasia: Methods and resources for training conversation partners. Aphasiology, 12(9), 816–830. https://doi.org/10.1080/02687039808249575
- Karyotaki, E., Smit, Y., Holdt Henningsen, K., Huibers, M. J. H., Robays, J., de Beurs, D., & Cuijpers, P. (2016). Combining pharmacotherapy and psychotherapy or monotherapy for major depression? A meta-analysis on the long-term effects. Journal of Affective Disorders, 194, 144–152. https://doi.org/10.1016/j.jad.2016.01.036
- Kauhanen, M. L., Korpelainen, J. T., Hiltunen, P., Määttä, R., Mononen, H., Brusin, E., Sotaniemi, K. A., & Myllylä, V. V. (2000). Aphasia, depression, and non-verbal cognitive impairment in ischaemic stroke. Cerebrovascular Diseases, 10(6), 455–461. https://doi.org/10.1159/000016107
- Kertesz, A. (2006). Western-Aphasia battery-revised (WAB-R). Pearson.
- Kneebone, I. I. (2016). A framework to support cognitive behavior therapy for emotional disorder after stroke. Cognitive and Behavioral Practice, 23(1), 99–109. https://doi.org/10.1016/j.cbpra.2015.02.001
- Kneebone, I. I., Neffgen, L. M., & Pettyfer, S. L. (2012). Screening for depression and anxiety after stroke: Developing protocols for use in the community. Disability and Rehabilitation, 34(13), 1114–1120. https://doi.org/10.3109/09638288.2011.636137
- Kootker, J. A., Rasquin, S. M. C., Smits, P., Geurts, A. C., van Heugten, C. M., & Fasotti, L. (2015). An augmented cognitive behavioural therapy for treating post-stroke depression: Description of a treatment protocol. Clinical Rehabilitation, 29(9), 833–843. https://doi.org/10.1177/0269215514559987
- Kotov, R., Cicero, D. C., Conway, C. C., DeYoung, C. G., Dombrovski, A., Eaton, N. R., First, M. B., Forbes, M. K., Hyman, S. E., Jonas, K. G., Krueger, R. F., Latzman, R. D., Li, J. J., Nelson, B. D., Regier, D. A., Rodriguez-Seijas, C., Ruggero, C. J., Simms, L. J., Skodol, A. E., … Wright, A. G. C. (2022). The hierarchical taxonomy of psychopathology (HiTOP) in psychiatric practice and research. Psychological Medicine, 52(9), 1666–1678. https://doi.org/10.1017/S0033291722001301
- Kozlowski, A. J., Singh, R., Victorson, D., Miskovic, A., Lai, J.-S., Harvey, R. L., Cella, D., & Heinemann, A. W. (2015). Agreement between responses from community-dwelling persons with stroke and their proxies on the NIH Neurological Quality of Life (Neuro-QoL) Short Forms. Archives of Physical Medicine and Rehabilitation, 96(11), 1986–1992.e14. https://doi.org/10.1016/j.apmr.2015.07.005
- Kutlubaev, M. A., & Hackett, M. L. (2014). Part II: Predictors of depression after stroke and impact of depression on stroke outcome: An updated systematic review of observational studies. International Journal of Stroke, 9(8), 1026–1036. https://doi.org/10.1111/ijs.12356
- Lane, J. D., & Gast, D. L. (2014). Visual analysis in single case experimental design studies: Brief review and guidelines. Neuropsychological Rehabilitation, 24(3–4), 445–463. https://doi.org/10.1080/09602011.2013.815636
- Lapin, B. R., Thompson, N. R., Schuster, A., Ryan, H., & Katzan, I. L. (2021). The validity of proxy responses on patient-reported outcome measures: Are proxies a reliable alternative to stroke patients’ self-report? Quality of Life Research, 30(6), 1735–1745. https://doi.org/10.1007/s11136-021-02758-9
- Leeds, L., Meara, R. J., & Hobson, J. P. (2004). The utility of the Stroke Aphasia Depression Questionnaire (SADQ) in a stroke rehabilitation unit. Clinical Rehabilitation, 18(2), 228–231. https://doi.org/10.1191/0269215504cr685oa
- Lincoln, N. B., Brinkmann, N., Cunningham, S., Dejaeger, E., De Weerdt, W., Jenni, W., Mahdzir, A., Putman, K., Schupp, W., Schuback, B., & De Wit, L. (2013). Anxiety and depression after stroke: A 5 year follow-up. Disability and Rehabilitation, 35(2), 140–145. https://doi.org/10.3109/09638288.2012.691939
- Lincoln, N. B., & Flannaghan, T. (2003). Cognitive behavioral psychotherapy for depression following stroke. Stroke, 34(1), 111–115. https://doi.org/10.1161/01.STR.0000044167.44670.55
- Manolov, R., Losada, J. L., Chacón-Moscoso, S., & Sanduvete-Chaves, S. (2016). Analyzing two-phase single-case data with non-overlap and mean difference indices: Illustration, software tools, and alternatives. Frontiers in Psychology, 7, 32. https://doi.org/10.3389/fpsyg.2016.00032
- McClellan, M. J., Florell, D., Palmer, J., & Kidder, C. (2020). Clinician telehealth attitudes in a rural community mental health center setting. Journal of Rural Mental Health, 44(1), 62–73. https://doi.org/10.1037/rmh0000127
- Mitchell, H. P., Veith, C. R., Becker, J. K., Buzaitis, C. A., Cain, C. K., Fruin, C. M., Tirschwell, C. D., & Teri, C. L. (2009). Brief psychosocial–behavioral intervention with antidepressant reduces poststroke depression significantly more than usual care With antidepressant. Stroke, 40(9), 3073–3078. https://doi.org/10.1161/STROKEAHA.109.549808
- Northcott, S., Burns, K., Simpson, A., & Hilari, K. (2016). ‘Living with aphasia the best Way I can': A feasibility study exploring solution-focused brief therapy for people with aphasia. Folia Phoniatrica et Logopaedica, 67(3), 156–167. https://doi.org/10.1159/000439217
- Nuyen, J., Schellevis, F. G., Satariano, W. A., Spreeuwenberg, P. M., Birkner, M. D., van den Bos, G. A. M., & Groenewegen, P. P. (2006). Comorbidity was associated with neurologic and psychiatric diseases: A general practice-based controlled study. Journal of Clinical Epidemiology, 59(12), 1274–1284. https://doi.org/10.1016/j.jclinepi.2006.01.005
- Paolucci, S. (2008). Epidemiology and treatment of post-stroke depression. Neuropsychiatric Disease and Treatment, 4(1), 145–154. https://doi.org/10.2147/NDT.S2017
- Parker, R. I., Vannest, K. J., & Davis, J. L. (2014). Non-overlap analysis for single-case research. In T. R. Kratochwill, & J. R. Levin (Eds.), Single-case research design and analysis: Methodological and statistical advances (pp. 127–151). Erlbaum.
- Parker, R. I., Vannest, K. J., Davis, J. L., & Sauber, S. B. (2011). Combining nonoverlap and trend for single-case research: Tau-U. Behavior Therapy, 42(2), 284–299. https://doi.org/10.1016/j.beth.2010.08.006
- Pirkis, J., Currier, D., Harris, M., Mihalopoulos, C., Arya, V., Banfield, M., Bassilios, B., Buchanan, B., Butterworth, P., Brophy, L., Burgess, P., Chatterton, M. L., Chilver, M., Eagar, K., Faller, J., Fossey, E., Ftanou, M., Gunn, J., Kruger, A., … Williamson, M. (2022). Evaluation of better access initiative. Australian Government Department of Health and Aged Care. https://www.health.gov.au/resources/collections/evaluation-of-the-better-access-initiative-final-report.
- Pitt, R., Theodoros, D., Hill, A. J., & Russell, T. (2019). The development and feasibility of an online aphasia group intervention and networking program – TeleGAIN. International Journal of Speech-Language Pathology, 21(1), 23–36. https://doi.org/10.1080/17549507.2017.1369567
- Rand, S., & Caiels, J. (2015). Using proxies to assess quality of life: A review of the issues and challenges. Quality and Outcomes of Person-centred Care Policy Research Unit.
- Rasquin, S. M. C., van de Sande, P., Praamstra, A. J., & van Heugten, C. M. (2009). Cognitive-behavioural intervention for depression after stroke: Five single case studies on effects and feasibility. Neuropsychological Rehabilitation, 19(2), 208–222. https://doi.org/10.1080/09602010802091159
- Rose, A. E., Cullen, B., Crawford, S., & Evans, J. J. (2023). A systematic review of mood and depression measures in people with severe cognitive and communication impairments following acquired brain injury. Clinical Rehabilitation, 37(5), 679–700. https://doi.org/10.1177/02692155221139023
- Rosenbaum, L. (2020). The untold toll — The pandemic’s effects on patients without COVID-19. New England Journal of Medicine, 382(24), 2368–2371. https://doi.org/10.1056/NEJMms2009984
- Ross, K. B., & Wertz, R. T. (2003). Discriminative validity of selected measures for differentiating normal from aphasic performance. American Journal of Speech-Language Pathology, 12(3), 312–319. https://doi.org/10.1044/1058-0360(2003/077)
- Ryan, B., Bohan, J., & Kneebone, I. (2019). Help-seeking and people with aphasia who have mood problems after stroke: perspectives of speech–language pathologists. International Journal of Language & Communication Disorders, 54(5), 779–793. https://doi.org/10.1111/1460-6984.12476
- Schmid, A. A., Damush, T., Tu, W., Bakas, T., Kroenke, K., Hendrie, H. C., & Williams, L. S. (2012). Depression improvement is related to social role functioning after stroke. Archives of Physical Medicine and Rehabilitation, 93(6), 978–982. https://doi.org/10.1016/j.apmr.2011.12.012
- Shehata, G. A., Mistikawi, T. E., Risha, A. S. K., & Hassan, H. S. (2015). The effect of aphasia upon personality traits, depression and anxiety among stroke patients. Journal of Affective Disorders, 172, 312–314. https://doi.org/10.1016/j.jad.2014.10.027
- Simmons-Mackie, N., Kagan, A., Victor, J. C., Carling-Rowland, A., Mok, A., Hoch, J. S., Huijbregts, M., & Streiner, D. L. (2014). The assessment for living with aphasia: Reliability and construct validity. International Journal of Speech-Language Pathology, 16(1), 82–94. https://doi.org/10.3109/17549507.2013.831484
- Sutcliffe, L. M., & Lincoln, N. B. (1998). The assessment of depression in aphasic stroke patients: The development of the Stroke Aphasic Depression Questionnaire. Clinical Rehabilitation, 12(6), 506–513. https://doi.org/10.1191/026921598672167702
- Swinton, J., Robinson, W., & Bischoff, R. (2009). Telehealth and rural depression: Physician and patient perspectives. Families, Systems, & Health, 27(2), 172–182. https://doi.org/10.1037/a0016014
- Tang, W., & Kreindler, D. (2017). Supporting homework compliance in cognitive behavioural therapy: Essential features of mobile apps. JMIR Mental Health, 4(2), e20. https://doi.org/10.2196/mental.5283
- Tate, R. L., Perdices, M., Rosenkoetter, U., Shadish, W., Vohra, S., Barlow, D. H., Horner, R., Kazdin, A., Kratochwill, T., McDonald, S., Sampson, M., Shamseer, L., Togher, L., Albin, R., Backman, C., Douglas, J., Evans, J. J., Gast, D., Manolov, R., … Wilson, B. (2016). The single-case reporting guideline in behavioural interventions (SCRIBE) 2016 statement. Canadian Journal of Occupational Therapy, 83(3), 184–195. https://doi.org/10.1177/0008417416648124
- Tate, R. L., Perdices, M., Rosenkoetter, U., Wakim, D., Godbee, K., Togher, L., & McDonald, S. (2013). Revision of a method quality rating scale for single-case experimental designs and n-of-1 trials: The 15-item Risk of Bias in N-of-1 Trials (RoBiNT) Scale. Neuropsychological Rehabilitation, 23(5), 619–638. https://doi.org/10.1080/09602011.2013.824383
- Tate, R. L., Wakim, D., Sigmundsdottir, L., & Longley, W. (2020). Evaluating an intervention to increase meaningful activity after severe traumatic brain injury: A single-case experimental design with direct inter-subject and systematic replications. Neuropsychological Rehabilitation, 30(4), 641–672. https://doi.org/10.1080/09602011.2018.1488746
- Taylor, G. H., Todman, J., & Broomfield, N. M. (2011). Post-stroke emotional adjustment: A modified social cognitive transition model. Neuropsychological Rehabilitation, 21(6), 808–824. https://doi.org/10.1080/09602011.2011.598403
- Thomas, S. (2020). Aphasia, depression, and psychological therapy (ADaPT): A CBT manual to treat depression in people with aphasia. Thinking Matters.
- Thomas, S. A., Walker, M. F., Macniven, J. A., Haworth, H., & Lincoln, N. B. (2013). Communication and low mood (CALM): A randomized controlled trial of behavioural therapy for stroke patients with aphasia. Clinical Rehabilitation, 27(5), 398–408. https://doi.org/10.1177/0269215512462227
- Tjokrowijoto, P., Kneebone, I., Baker, C., Andrew, N. E., & Stolwyk, R. J. (2023). Mental health support after stroke: A qualitative exploration of lived experience. Rehabilitation Psychology, https://doi.org/10.1037/rep0000527
- Townend, E., Brady, M., & McLaughlan, K. (2007). A systematic evaluation of the adaptation of depression diagnostic methods for stroke survivors who have aphasia. Stroke, 38(11), 3076–3083. https://doi.org/10.1161/STROKEAHA.107.484238
- Tse, J., LaStella, D., Chow, E., Kingman, E., Pearlman, S., Valeri, L., Wang, H., & Dixon, L. B. (2021). Telehealth acceptability and feasibility among people served in a community behavioral health system during the COVID-19 pandemic. Psychiatric Services, 72(6), 654–660. https://doi.org/10.1176/appi.ps.202000623
- Turner-Stokes, L., Kalmus, M., Hirani, D., & Clegg, F. (2005). The Depression Intensity Scale Circles (DISCs): A first evaluation of a simple assessment tool for depression in the context of brain injury. Journal of Neurology, Neurosurgery & Psychiatry, 76(9), 1273. https://doi.org/10.1136/jnnp.2004.050096
- Vannest, K. J., & Ninci, J. (2015). Evaluating intervention effects in single-case research designs. Journal of Counseling & Development, 93(4), 403–411. https://doi.org/10.1002/jcad.12038
- Vannest, K. J., Parker, R. I., Gonen, O., & Adiguzel, T. (2016). Single Case Research: Web based calculators for SCR analysis. (Version 2.0) [Web-based application]. http://singlecaseresearch.org/calculators/tau-u.
- Vannest, K. J., Peltier, C., & Haas, A. (2018). Results reporting in single case experiments and single case meta-analysis. Research in Developmental Disabilities, 79, 10–18. https://doi.org/10.1016/j.ridd.2018.04.029
- Wang, S.-B., Wang, Y.-Y., Zhang, Q.-E., Wu, S.-L., Ng, C. H., Ungvari, G. S., Chen, L., Wang, C.-X., Jia, F.-J., & Xiang, Y.-T. (2018). Cognitive behavioral therapy for post-stroke depression: A meta-analysis. Journal of Affective Disorders, 235, 589–596. https://doi.org/10.1016/j.jad.2018.04.011
- Weitz, E., Kleiboer, A., van Straten, A., & Cuijpers, P. (2018). The effects of psychotherapy for depression on anxiety symptoms: A meta-analysis. Psychological Medicine, 48(13), 2140–2152. https://doi.org/10.1017/S0033291717003622
- White, J. H., Magin, P., Attia, J., Sturm, J., Carter, G., & Pollack, M. (2012). Trajectories of psychological distress after stroke. The Annals of Family Medicine, 10(5), 435–442. https://doi.org/10.1370/afm.1374
- Whitehurst, D. G. T., Latimer, N. R., Kagan, A., Palmer, R., Simmons-Mackie, N., Victor, J. C., & Hoch, J. S. (2018). Developing accessible, pictorial versions of health-related quality-of-life instruments suitable for economic evaluation: A report of preliminary studies conducted in Canada and the United Kingdom. PharmacoEconomics - Open, 2(3), 225–231. https://doi.org/10.1007/s41669-018-0083-2
- Williams, L. S., Bakas, T., Brizendine, E., Plue, L., Tu, W., Hendrie, H., & Kroenke, K. (2006). How valid Are family proxy assessments of stroke patients’ health-related quality of life? Stroke, 37(8), 2081–2085. https://doi.org/10.1161/01.STR.0000230583.10311.9f
- Wong, D., Hsieh, M.-Y., McKay, A., Haines, K., O’Donnell, M., & Ponsford, J. (2018). Cognitive behaviour therapy for anxiety and depression—Adapted for brain injury (CBT-ABI): A treatment manual. ASSBI Resources.
- Wong, D., Sinclair, K., Seabrook, E., McKay, A., & Ponsford, J. (2017). Smartphones as assistive technology following traumatic brain injury: A preliminary study of what helps and what hinders. Disability and Rehabilitation, 39(23), 2387–2394. https://doi.org/10.1080/09638288.2016.1226434
- Ymer, L., McKay, A., Wong, D., Frencham, K., Grima, N., Tran, J., Nguyen, S., Junge, M., Murray, J., Spitz, G., & Ponsford, J. (2021). Cognitive behavioural therapy versus health education for sleep disturbance and fatigue after acquired brain injury: A pilot randomised trial. Annals of Physical and Rehabilitation Medicine, 64(5), 101560. https://doi.org/10.1016/j.rehab.2021.101560
